Back to Journals » Patient Preference and Adherence » Volume 9
Physical activity in patients with heart failure: barriers and motivations with special focus on sex differences
Authors Klompstra L , Jaarsma T , Strömberg A
Received 22 June 2015
Accepted for publication 20 August 2015
Published 9 November 2015 Volume 2015:9 Pages 1603—1610
DOI https://doi.org/10.2147/PPA.S90942
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Johnny Chen
Leonie Klompstra,1 Tiny Jaarsma,1 Anna Strömberg2,3
1Department of Social and Welfare Studies, Faculty of Health Sciences, 2Department of Medical and Health Sciences, Division of Nursing, 3Department of Cardiology, Linköping University, Linköping, Sweden
Background: Adherence to recommendations for physical activity is low in both male and female patients with heart failure (HF). Men are more physically active than women. In order to successfully promote physical activity, it is therefore essential to explore how much and why HF patients are physically active and if this is related to sex. The aim of this study was therefore to evaluate physical activity in HF patients, to describe the factors related to physical activity, and to examine potential barriers and motivations to physical activity with special focus on sex differences.
Methods: The study had a cross-sectional survey design. HF patients living at home received a questionnaire during May–July 2014, with questions on physical activity (from the Short Form-International Physical Activity Questionnaire), and potential barriers and motivations to physical activity.
Results: A total of 154 HF patients, 27% women, with a mean age of 70±10 were included. In total, 23% of the patients reported a high level of physical activity, 46% a moderate level, and 34% a low level. Higher education, self-efficacy, and motivation were significantly associated with a higher amount of physical activity. Symptoms or severity of the disease were not related to physical activity. All the potential barriers to exercise were reported to be of importance. Psychological motivations were most frequently rated as being the most important motivation (41%) to be physically active. Physical motivations (33%) and social motivations were rated as the least important ones (22%). Women had significantly higher total motivation to be physically active. These differences were found in social, physical, and psychological motivations.
Discussion: One-third of the HF patients had a low level of physical activity in their daily life. Severity of the disease or symptoms were not related, whereas level of education, exercise self-efficacy, and motivation were important factors to take into account when advising a HF patient about physical activity. Women reported higher motivation to be physically active than men, but there was no difference in the reported level of physical activity.
Keywords: barriers, sex differences, heart failure, motivation, physical activity, self-efficacy
Background
Heart failure (HF) is known to lead to poor health-related quality of life as well as high morbidity and mortality rates. It is also the most common reason for hospitalization in older adults.1,2 Physical activity in HF patients is known to have positive outcomes such as improved physical capacity and quality of life, and reduced health care utilization.3 However, adherence to physical activity is less than 50% in HF patients;4,5 it even seems more difficult to achieve than dietary modification and medication regimes.6
Predictors of regular participation in physical activity in healthy adults have been well documented. Lower age positively correlates with physical activity as well as better self-efficacy, greater social support, better knowledge of perceived benefits, and a positive attitude toward physical activity.7,8 Compared with men, women are less physically active.9 Engaging in regular physical activity or having an early history of physical activity has also been described as a predictor of future physical activity, as have higher education and income level, support from a health care provider, and support from surrounding people.10 Being single or having an inactive partner has been negatively correlated with physical activity levels in older adults.11 Depression has been identified as being negatively correlated with physical activity levels.12
Barriers and motivations to participation in regular physical activity have been well studied in the adult population. Barriers to physical activity include internal barriers, such as lack of time, fear of injury, lack of knowledge, lack of self-discipline or motivation, and ill health or changing health status.13–16 External barriers to physical activity include environmental considerations (eg, no facilities nearby), safety, cost, friends/partner not interested, and barriers related to the weather.15–18
Motivations toward physical activity in adults include advice by health care providers, family influences, improvement in physical or motor competence, health benefits, and psychosocial reasons such as enjoying group interaction and meeting with friends.16 Chronic health conditions have been identified both as a barrier and as motivations toward physical activity in the older adult population; individuals may exercise to prevent further physical decline, but their ability to participate in physical activity could be limited by the same conditions.16
Data on rehabilitation in cardiac patients have shown that lower adherence to physical activity is associated with older age, lower social and economic status, lack of motivation, and financial and medical concerns.19 Data on HF-specific barriers to physical activity have shown that experiencing symptoms and lack of energy is associated with lower adherence to physical activity.5,6,20
Patients with HF have been described as being less physically active in daily life compared with healthy adults,21 but a few studies have described the level of physical activity in HF patients living at home. To our knowledge, there has been only one study where the amount of physical activity in 68 HF patients has been examined, using an accelerometer. The authors found that 44% of the patients were sedentary, 35% were moderately physically active, and 15% were physically active on a low level.8 The variance in daily activity in that study could be partly explained by the patients’ symptoms and self-efficacy.8 In order to promote physical activity in HF patients, it is essential to know how physically active they are and to understand the barriers and motivation they experience for being more physically active. Motivation not only affects exercise participation, but is also a critical factor in exercise adherence.22,23
There are sex differences in physical activity that could be explained by a number of factors. Research has indicated that older women’s personal backgrounds are less favorable for physical activity than those of men (for instance, reported lower levels of education and income, fewer women were married, and a greater number lived alone).24,25 In addition, women perceive their health as poorer, are more likely to experience barriers to physical activity, and indicate lower self-efficacy for physical activity than men.24,25 Motivation and barriers to exercise are important to consider when promoting physical activity in HF patients.
Therefore, this study aimed to, first, evaluate physical activity in HF patients and describe the factors related to physical activity, and, second, to examine potential barriers and motivations to physical activity, and possible sex differences related to them in HF patients.
Methods
Design and subjects
This study has a cross-sectional design. Patients diagnosed with HF (regardless of ejection fraction) and older than 18 years of age were eligible for participation. Exclusion criteria were inability to understand Swedish and/or a cognitive impairment that would make it impossible to fill in the questionnaires.
Definition of physical activity, exercise, and physical fitness
In this study, physical activity is defined as any bodily movement produced by skeletal muscles that results in energy expenditure. Exercise is a subset of physical activity that is planned, structured, and repetitive, and has as a final or intermediate objective to improve or maintain physical fitness.26
Procedures
This study complies with the Declaration of Helsinki and was approved by the Regional Ethics Committee (Regionala etikprövningsnämnden i Linköping; Dnr 2014/292-32). All patients provided written informed consent.
Patients with HF were selected through the diagnosis registry from a HF clinic (diagnose codes: I50.0 and I50.9) in a county hospital in Sweden. Three hundred patients were invited to participate during May–July 2014. Patients received the invitation by post together with the informed consent form and the questionnaire. They were asked to return everything in a prepaid envelope.
Pedhazur’s and Schmelkin’s27 rule of thumb that states that good power requires 50 patients for each factor was used. In this study, three factors were measured (physical activity, self-efficacy, and motivation), which means that 150 patients needed to be included.27 We chose to approach 300 patients, as previous surveys have shown the response rate of HF patients in Sweden to be 33%–65%.28–30
Measurement
Physical activity was measured by the Short Form-International Physical Activity Questionnaire (s-IPAQ). The s-IPAQ contains seven items for identifying the frequency and duration of light, moderate, and vigorous physical activity as well as inactivity during the past week. The questions focus on four activity types: “vigorous activity” periods of at least 10 minutes, “moderate activity” periods of at least 10 minutes, “walking” periods of at least 10 minutes, and times spent “sitting” on weekdays. Frequency of activity is measured in days, and duration in hours and minutes. The answers to the questions were transformed into metabolic equivalent of task (MET), or simply metabolic equivalent, a physiological measure expressing the energy cost of physical activities defined as the ratio of metabolic rate and therefore the rate of energy consumption. The total physical activity score is the sum of vigorous, moderate, and walking physical activity scores. The patients were classified into three physical activity categories: low, moderate, and high. Typical s-IPAQ correlations with an accelerometer were 0.80 for reliability.31,32
Potential barriers to physical activity were measured with the Exercise Self-Efficacy Questionnaire, which assesses self-efficacy beliefs specifically related to confidence to exercise in relation to potential barriers: work schedule, physical fatigue, boredom related to exercise, minor injuries, other time demands, and family and home responsibilities. The questionnaire consists of nine situations that might affect participation in exercise. For each situation, the subjects use a scale ranging from 1 (not confident) to 10 (very confident) to describe their current confidence of being able to exercise for 20 minutes three times a week. The instrument is reliable and valid,33 and Cronbach’s alpha in this sample was 0.931. Based on the literature, four additional potential HF-specific barriers were added; in spite of poor weather, in spite of experiencing HF symptoms, in spite of experiencing side effects of the medications, afraid of getting hurt through exercise.
Participation motives were measured with the Exercise Motivation Index. The questionnaire consists of 15 statements followed by a five-point rating scale for each statement, ranging from 0 (not important) to 4 (extremely important). Although the authors found that the index was valid and reliable, they advise that further validation be made. Three subscores (0–4) were calculated by summing the scores for physical, psychological, and social motivation and dividing them by the number of statements for each area.34 Cronbach’s alpha was 0.889.34
Data were collected on demographic questions relating to sex, education, marital status, smoking habits, alcohol consumption, and symptoms (fatigue and shortness of breath).
Additional data concerning New York Heart Association (NYHA) Classification, which is a measure for symptom severity, HF medications, and comorbidity, were collected from the patients’ medical charts.
Statistical analysis
SPSS version 22 (IBM, Armonk, NY, USA) was used to analyze the data. Means and standard deviation were calculated for continuous data, and absolute numbers and percentages were computed for nominal variables.
Because the s-IPAQ is validated for people in the 18–69 age range, an additional analysis was performed to see whether there were significant differences in the total score of the scale between HF patients younger than 69 years and those older than 69.
For presentation reasons, we dichotomized the response alternatives in the Exercise Self-Efficacy and the added potential HF-specific barriers. The response alternatives 1 (not confident)–5 were combined to a potential barrier, whereas the response alternatives 6–10 (very confident) were combined as no potential barrier. The response alternatives in the Exercise Motivation Index were also dichotomized. Response alternatives 0 (not at all important)–2 (important) were combined as no or little motivation, and response alternatives 3 (very important) and 4 (enormously important) were combined as a motivation. Possible differences between patients with a high physical activity level and patients with a low physical activity level with regard to sex, education, marital status, NYHA classification, smoking habits, alcohol consumption, and comorbidity were analyzed with Mann–Whitney U-tests. Associations with age, time after diagnosis, body mass index, exercise self-efficacy, and exercise motivation were analyzed using independent sample t-tests.
Results
Sample characteristics
Overall, 154 HF patients responded to the questionnaire (response rate, 51%). There was no significant difference concerning sex among the nonresponders (n=146, 26% female, P-value =0.27), but there was a significant difference in age, with nonresponders being younger (67±13) than the responders (P-value =0.04).
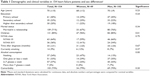
The mean age of the sample was 70 (±10) years, and 27% of the HF patients were women (Table 1).
In total, 20% of the patients were educated beyond high school, and 71% were married or in a relationship. Most of the patients were in NYHA class I or II (64%). Almost half of the patients (46%) were overweight or obese.
Physical activity in HF patients
Of the HF patients, 56% were older than the IPAQ target age range (15–69 years), but no differences were found in the amount of total METs (P-value =0.71), METs vigorous (P-value =0.94), METs moderate (P-value =0.34), and METs walking (P-value =0.71) between patients younger or older than 69.
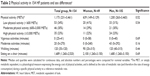
Of the 154 HF patients, 23% reported high physical activity (≥3,000 METs) (at least 1 h/d of moderate-intensity activity or half an hour of vigorous-intensity activity). Thirty percent reported moderate physical activity (600–3,000 METs) (at least 30 minutes of moderate-intensity physical activity on most days), and 34% of the patients reported low physical activity (<600 METs) (Tables 2 and 3).
Patients reported performing only a small amount of vigorous activities (median =0, quartiles 25–41) (lifting, digging, aerobics, or fast cycling), a median of 20 min/wk (quartiles 0–270) moderate activities (carrying light loads, cycling at a regular pace, or doubles tennis), and walking for a median 120 min/wk (quartiles 35–120) (walking at work and at home, walking from place to place, and any other walking that might be done solely for recreation, sport, exercise, or leisure). Patients reported spending a median of 1,680 min/wk (4 h/d at rest) sitting on a chair (quartiles 1,260–2,520).
Factors related to physical activity
The level of education was significantly associated with levels of physical activity (Table 3). There were more patients who were educated to just primary school level (n=29, 55%) in the low physical activity level group compared to patients with a high physical activity level (9 patients completed just primary school, 26%, P-value =0.04).
Patients with high physical activity had higher exercise self-efficacy (mean 2±1) and higher exercise motivation (mean 4±2) compared to patients with a low physical activity level (mean 3±2 and mean 1±1, P-value <0.01).
No differences were found between patients with a high physical activity level and patients with a low physical activity level with regard to sex (P-value =0.54), NYHA (P-value =0.13), or comorbidity (P-value =0.26).
Potential barriers to exercise
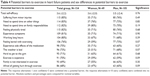
Most of the patients (68%–85%) reported all the potential barriers to exercise in the Exercise Self-Efficacy Scale to be relevant. The potential barriers that were experienced by more than 80% of the patients were: “suffering from minor injuries” (85%), “need to spend time on other things” (83%), “need to spend time on family responsibilities” (82%), “feeling physically tired” (82%), and “working long hours” (80%) (Table 4).
The potential barriers “family is not interested in exercise” (69%) and “being afraid of getting hurt through exercise” (68%) were the ones least experienced. No differences were found in potential barriers between men and women.
Motivations
Only two out of the 15 motivations in the questionnaire were experienced by more than 50% of the HF patients. The motivations “I want to be healthier and perhaps live longer” and “I want a slower aging process and feel younger” were reported as relevant by more than half of the patients (66% vs 57%) (Table 5). The motivations that were experienced by less than 20% of the patients were: “People who are fit are admired, I want to be admired too” (13%); “I want to look good” (16%); and “Everyone else exercises, I want to do that too” (17%).
When considering the different subscales of motivations (physical, psychological, and social motivations), the social motivations to exercise were rated the least important (22%), the physical motivations were expressed to be important by 33%, and the psychological motivations were rated as the most frequent motivations for being physically active (41%).
We found differences between men and women in the total amount of motivation and the subscales of motivation (social motivation, physical motivation, and psychological motivation). Women had higher total motivation than men (mean 2.1±2.4 vs mean 1.7±2.0, P-value <0.01), higher social motivation than men (mean 1.7±1.0 vs mean 1.2±0.9, P-value =0.02), higher physical motivation than men (mean 2.5±1.0 vs 2.1±1.0, P-value =0.04), and higher psychological motivation than men (mean 2.2±1.0 vs 1.8±1.1, P-value =0.02).
Two motivations were significantly more often expressed by women as being a motivation to exercise compared with men: “I am proud of myself when I take regular exercise” (53% vs 31%, P-value <0.01), and “I feel more successful when I am in good shape” (39% vs 24%, P-value <0.05).
Discussion
This is the first study that examines sex differences in physical activity in HF patients in relation to their barriers and motivation in physical activity. The aim of this study was chosen because having HF is identified as both a barrier and a motivation to physical activity in the older adult population.16 Furthermore, women tend to be less physically active compared with men,9 and experience different barriers and motivations to physical activity. Identifying factors associated with HF patients’ physical activity is important because it will help future research and may guide the implementation of interventions aimed at promoting physical activity. It is particularly important to identify and promote those factors that lead to sustained physical activity in the long term.
Despite the fact that most of the patients were in NYHA class I or II (64%), reflecting that they had no or few symptoms of HF, one-third of them had a low physical activity level in their daily life. Since there is evidence of the beneficial effects of physical activity on quality of life, morbidity, and hospitalization,35,36 these findings might inspire health care providers to address this issue further.
Since a higher level of education, exercise self-efficacy, and motivation were associated with a higher physical activity level, these factors might be important to take into account when advising a HF patient on how to become more physically active. The majority of the patients in this study experienced all potential barriers in becoming physically active. All barriers were reported as being high (including environmental barriers such as “It is hard to get to the gym” and interpersonal barriers such as “Family is not interested in exercise”). Social motivation was only important for 22% of the patients, and physical motivation was only important for one-third of the patients. In this study, we did not find differences in potential barriers to physical activity between men and women, which have been found in other research.24 Psychological motivation was viewed as the most important motivation and expressed by 41% of the patients. By far the most important single item that motivated patients was “I want to be healthier and perhaps live longer”, which motivated two-thirds of the patients. Sex differences in motivations were found. Women had higher total motivation to physical activity and also scored higher on the subscale motivation (physical, social, and psychological).
From this study, it is not clear why women with HF had higher motivation but similar physical activity levels compared with men. An explanation for this result could be that women have more difficulties in dealing with their barriers toward physical activity compared with men. In this research, we only measured whether the HF patients had certain barriers, but not how these specific barriers affected the physical activity and motivation.
Looking at the self-determination theory,37 intrinsic motivations (engaging in an activity for pleasure and inherent satisfaction) were more often expressed as motivators than extrinsic motivations (engaging in an activity for instrumental reasons). Intrinsic motivation could be the key for maintaining physical activity in HF patients22,37 and important motivators to take into consideration when developing promotion or intervention strategies. Promotion and intervention strategies should therefore include motivation as important factors in maintaining physical activity, and health care professionals should look at the specific needs of HF patients in order to reduce their barriers and enhance motivation to physical activity. In order to promote physical activity in HF patients, it is essential for health care professionals to know how physically active they are and to understand the barriers and motivation they experience for being more physically active. Also, it is important to understand sex differences in relation to physical activity in order to be able to advise patients on physical activity. Based on the results of this study, future research regarding physical activity in HF patients should assess intrinsic motivations and focus on differences in motivations between men and women.
This study was limited by physical activity levels being based on self-reports. Furthermore, the cross-sectional design was a limitation in implying causal relationships between physical activity and health indicators. Another limitation is that there are fewer women in this research compared with the general population of HF patients in Sweden who were mostly over 70 years old. It is therefore difficult to generalize the findings to women with HF. Older women more often have diastolic dysfunction. The myocardial structural and primary functional derangements are distinctive in these two syndromes, although hemodynamic consequences, clinical presentations, signs and symptoms, and prognosis are similar.38
The generalizability of these findings may be limited to relatively healthy HF patients living at home. Therefore, the disease itself could be of little influence on the barriers and motivation, although we found different outcomes compared with research done in older adults.21 The population was also younger and comprised fewer women than the general HF population in Sweden.2 This could be because the research included only HF patients living at home.
The results help to understand that barriers and motivation for physical activity in HF patients do not always relate to their disease. However they are important to keep in mind to tailor rehabilitation or exercise programs to individual patients.
Disclosure
The authors report no conflicts of interest in this work.
References
Dickstein K, Cohen-Solal A, Filippatos G, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the diagnosis and treatment of acute and chronic heart failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur J Heart Fail. 2008;10(10):933–989. | ||
Zarrinkoub R, Wettermark B, Wändell P, et al. The epidemiology of heart failure, based on data for 2.1 million inhabitants in Sweden. Eur J Heart Fail. 2013;15(9):995–1002. | ||
Piepoli MF, Conraads V, Corrà U, et al. Exercise training in heart failure: from theory to practice. A consensus document of the Heart Failure Association and the European Association for Cardiovascular Prevention and Rehabilitation. Eur J Heart Fail. 2011;13(4):347–357. | ||
Keteyian SJ, Brawner CA, Ehrman JK, et al. Reproducibility of peak oxygen uptake and other cardiopulmonary exercise parameters: implications for clinical trials and clinical practice. Chest. 2010;138(4):950–955. | ||
van der Wal MH, van Veldhuisen DJ, Veeger NJ, Rutten FH, Jaarsma T. Compliance with non-pharmacological recommendations and outcome in heart failure patients. Eur Heart J. 2010;31(12):1486–1493. | ||
Evangelista LS, Berg J, Dracup K. Relationship between psychosocial variables and compliance in patients with heart failure. Heart Lung. 2001;30(4):294–301. | ||
Crombie IK, Irvine L, Williams B, et al. Why older people do not participate in leisure time physical activity: a survey of activity levels, beliefs and deterrents. Age Ageing. 2004;33(3):287–292. | ||
Dontje ML, van der Wal MH, Stolk RP, et al. Daily physical activity in stable heart failure patients. J Cardiovasc Nurs. 2014;29(3):218–226. | ||
CDC. Facts About Physical Activity. Available from: http://www.cdc.gov/physicalactivity/data/facts.htm [cited 2015]. Accessed September 3, 2015. | ||
Thompson AM, Humbert ML, Mirwald RL. A longitudinal study of the impact of childhood and adolescent physical activity experiences on adult physical activity perceptions and behaviors. Qual Health Res. 2003;13(3):358–377. | ||
Pettee KK, Brach JS, Kriska AM, et al. Influence of marital status on physical activity levels among older adults. Med Sci Sports Exerc. 2006;38(3):541–546. | ||
Lindwall M, Rennemark M, Halling A, Berglund J, Hassmén P. Depression and exercise in elderly men and women: findings from the Swedish national study on aging and care. J Aging Phys Act. 2007;15(1):41. | ||
Tak E, van Uffelen J, Paw M, van Mechelen W, Hopman-Rock M. Adherence to exercise programs and determinants of maintenance in older adults with mild cognitive impairment. J Aging Phys Act. 2012;20(1):32–46. | ||
Moschny A, Platen P, Klaaβen-Mielke R, Trampisch U, Hinrichs T. Barriers to physical activity in older adults in Germany: a cross-sectional study. Int J Behav Nutr Phys Act. 2011;8(1):121–131. | ||
Bauman AE, Reis RS, Sallis JF, et al. Correlates of physical activity: why are some people physically active and others not? Lancet. 2012;380(9838):258–271. | ||
Costello E, Kafchinski M, Vrazel J, Sullivan P. Motivators, barriers, and beliefs regarding physical activity in an older adult population. J Geriatr Phys Ther. 2011;34(3):138–147. | ||
Rosenberg DE, Huang DL, Simonovich SD, Belza B. Outdoor built environment barriers and facilitators to activity among midlife and older adults with mobility disabilities. Gerontologist. 2013;53(2):268–279. | ||
Van Cauwenberg J, De Bourdeaudhuij I, De Meester F, et al. Relationship between the physical environment and physical activity in older adults: a systematic review. Health Place. 2011;17(2):458–469. | ||
Barbour KA, Miller NH. Adherence to exercise training in heart failure: a review. Heart Fail Rev. 2008;13(1):81–89. | ||
Yates BC, Price-Fowlkes T, Agrawal S. Barriers and facilitators of self-reported physical activity in cardiac patients. Res Nurs Health. 2003;26(6):459–469. | ||
Jehn M, Schmidt-Trucksass A, Schuster T, et al. Daily walking performance as an independent predictor of advanced heart failure: Prediction of exercise capacity in chronic heart failure. Am Heart J. 2009;157(2):292–298. | ||
Andre N, Dishman RK. Evidence for the construct validity of self-motivation as a correlate of exercise adherence in French older adults. J Aging Phys Act. 2012;20(2):231–245. | ||
Aaltonen S, Leskinen T, Morris T, et al. Motives for and barriers to physical activity in twin pairs discordant for leisure time physical activity for 30 years. Int J Sports Med. 2012;33(2):157–163. | ||
Lee YS. Gender differences in physical activity and walking among older adults. J Women Aging. 2005;17(1–2):55–70. | ||
Sjögren K, Stjernberg L. A gender perspective on factors that influence outdoor recreational physical activity among the elderly. BMC Geriatr. 2010;10(1):34. | ||
Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100(2):126–131. | ||
Pedhazur EJ, Schmelkin LP. Measurement, Design, and Analysis: An Integrated Approach. Hillsdale, NJ: Erlbaum; 1991. | ||
Theander K, Hasselgren M, Luhr K, Eckerblad J, Unosson M, Karlsson I. Symptoms and impact of symptoms on function and health in patients with chronic obstructive pulmonary disease and chronic heart failure in primary health care. Int J Chron Obstruct Pulmon Dis. 2014;9:785–794. | ||
Nordgren L, Soderlund A. Being on sick leave due to heart failure: encounters with social insurance officers and associations with sociodemographic factors and self-estimated ability to return to work. Eur J Cardiovasc Nurs. Epub February 3, 2015. | ||
Niklasson O, Boman K, Stenberg B. The prevalence and characteristics of pruritus in patients with heart failure. Br J Dermatol. 2015;172(6):1541–1546. | ||
Hurtig-Wennlöf A, Hagströmer M, Olsson LA. The International Physical Activity Questionnaire modified for the elderly: aspects of validity and feasibility. Public Health Nutr. 2010;13(11):1847–1854. | ||
Craig CL, Marshall AL, Sjostrom M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–1395. | ||
Dzewaltowski D. Toward a model of exercise motivation. J Sport Exerc Psychol. 1989;11:251–269. | ||
Stenström CH, Boestad C, Carlsson M, Edström M, Reuterhäll A. Why exercise?: a preliminary investigation of an exercise motivation index among individuals with rheumatic conditions and healthy individuals. Physiother Res Int. 1997;2(1):7–16. | ||
Lewinter C, Doherty P, Gale CP, et al. Exercise-based cardiac rehabilitation in patients with heart failure: a meta-analysis of randomised controlled trials between 1999 and 2013. Eur J Prev Cardiol. Epub November 14, 2014. | ||
Piepoli MF, Davos C, Francis DP, Coats AJ; Collaborative E. Exercise training meta-analysis of trials in patients with chronic heart failure (ExTraMATCH). BMJ. 2004;328(7433):189. | ||
Hagger MS, Chatzisarantis NL. Integrating the theory of planned behaviour and self-determination theory in health behaviour: a meta-analysis. Br J Health Psychol. 2009;14(Pt 2):275–302. | ||
Chatterjee K, Massie B. Systolic and diastolic heart failure: differences and similarities. J Card Fail. 2007;13(7):569–576. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.