Back to Journals » Drug Design, Development and Therapy » Volume 12
Pharmacokinetic interactions and tolerability of rosuvastatin and ezetimibe: an open-label, randomized, multiple-dose, crossover study in healthy male volunteers
Authors Kim H , Choi HY, Kim YH, Bae KS , Jung J , Son H, Lim HS
Received 29 November 2017
Accepted for publication 3 February 2018
Published 11 April 2018 Volume 2018:12 Pages 815—821
DOI https://doi.org/10.2147/DDDT.S158408
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Qiongyu Guo
Hyungsub Kim,1 Hee Youn Choi,1 Yo-Han Kim,1 Kyun-Seop Bae,1 Jina Jung,2 Hankil Son,2 Hyeong-Seok Lim1
1Department of Clinical Pharmacology and Therapeutics, Asan Medical Center, University of Ulsan, Seoul, Republic of Korea; 2Clinical Research Team, Hanmi Pharmaceutical Co. Ltd., Seoul, Republic of Korea
Purpose: Rosuvastatin is a synthetic 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitor that effectively reduces low-density lipoprotein cholesterol levels. However, statin monotherapy does not always achieve acceptable low-density lipoprotein cholesterol levels in patients with severe hypercholesterolemia. Ezetimibe, a selective cholesterol-absorption inhibitor, is approved for use as a monotherapy or combination therapy with 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors for patients with hypercholesterolemia. The aim of this study was to examine the pharmacokinetics (PKs) of drug interactions between rosuvastatin and ezetimibe, and the tolerability of combined administration in healthy Korean male volunteers.
Subjects and methods: Healthy subjects (n=24) were randomly allocated to 3 treatment groups: rosuvastatin (20 mg) alone, ezetimibe (10 mg) alone, and rosuvastatin (20 mg) plus ezetimibe (10 mg). The drugs were taken once every 24 hours over a period of 10 days. Blood samples were collected to analyze steady-state PKs.
Results: All adverse events observed during the study were mild, and the frequency was no higher for combined administration than for mono administration. For rosuvastatin, the steady-state mean ratios (90% CI) of the combined over the single dose were 1.076 (1.019–1.136) for AUCτ,ss and 1.099 (1.003–1.204) for concentration at steady-state, respectively. In the case of free and total ezetimibe, the steady-state ratios of AUCτ,ss and concentration at steady-state were 1.131 (1.051–1.218) and 1.182 (1.038–1.346), and 1.055 (0.969–1.148) and 0.996 (0.873–1.135), respectively.
Conclusion: Combined administration of rosuvastatin and ezetimibe was well tolerated. No clinically significant PK interactions between rosuvastatin and ezetimibe were observed when the 2 drugs were administered concomitantly.
Keywords: rosuvastatin, ezetimibe, pharmacokinetics, DDI, tolerability
Introduction
Globally, cardiovascular disease (CAD) is a major cause of morbidity and death. Dyslipidemia, hypertension, diabetes mellitus (DM), and obesity are important risk factors for CAD.1,2 Among them, dyslipidemia due to elevated total and low-density lipoprotein cholesterol (LDL-C) and reduced high-density lipoprotein cholesterol is closely associated with coronary artery disease, atherosclerosis, and cerebrovascular disease.
Cholesterol-lowering drugs, such as 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitors (statins) reduce the risk of CAD. Rosuvastatin is a fully synthetic HMG-CoA reductase inhibitor that is more effective at reducing LDL-C levels than other statins when used at a low dose; thus, it is the most potent drug for reducing cardiovascular risk.3 However, statin monotherapy does not always reduce LDL-C levels to acceptable levels in patients with severe hypercholesterolemia, particularly those at high cardiovascular risk.4 Therefore, to meet the target LDL-C levels, it may be necessary to combine stains with an additional drug that acts via a different mechanism.
Ezetimibe is a selective cholesterol and phytosterol absorption inhibitor that targets gastrointestinal cholesterol in the small intestine; this drug reduces plasma cholesterol in humans by 15%–20%.5 Ezetimibe administration is effective for both mono- and combination therapy with HMG-CoA reductase inhibitors in patients with hypercholesterolemia.6 Ezetimibe monotherapy is the recommended treatment for primary hypercholesterolemia in patients in whom statin therapy is contraindicated or in those that cannot tolerate statins. A previous study shows that a fixed-dose combination of ezetimibe and rosuvastatin is significantly better than rosuvastatin alone in terms of reducing LDL-C and triglyceride levels, and that the rate of reduction is even greater in patients with DM or metabolic syndrome.7 An early trial demonstrated additional reductions in LDL-C levels (by 12%–19%) when ezetimibe was administered with atorvastatin.8 Daily combined administration of ezetimibe plus rosuvastatin led to a significant fall in LDL-C when compared with rosuvastatin alone.9
The potential therapeutic interaction between ezetimibe and HMG-CoA reductase inhibitors offers significant clinical benefits provided that this drug combination is both safe and well tolerated.10,11 The primary purpose of this study was to examine the pharmacokinetic (PK) interactions and tolerability of rosuvastatin and ezetimibe when taken orally over 10 consecutive days by healthy Korean volunteers.
Subjects and methods
Subjects
Healthy male volunteers aged 19–45 years with a body mass index of 19–28 kg/m2 were eligible for the study. All subjects were considered to be in good health based on medical history, physical examinations, vital signs (blood pressure, heart rate, and body temperature), 12-lead ECG, clinical laboratory tests (hematology, blood chemistry, and urinalysis), serology (hepatitis B surface antigen, hepatitis C virus antibodies, and HIV antigen/antibodies), and urine drug screening (amphetamines, methamphetamines, barbiturates, cocaine, opiates, benzodiazepine, cannabinoids, and methadone) within 4 weeks before the first administration of the study drug. Subjects with a known allergy or hypersensitivity to rosuvastatin or ezetimibe, or with a history of drug abuse, were excluded.
Study design
The study was designed as an open-label, randomized, multiple-dose, 3-treatment, 3-period, 6-sequence, and crossover clinical trial (Figure 1). All subjects were randomly assigned to 1 of 6 sequences and received 1 of 3 different treatments every 24 hours over 10 days: rosuvastatin 20 mg (Treatment A), ezetimibe 10 mg (Treatment B), or rosuvastatin 20 mg plus ezetimibe 10 mg (Treatment C). All treatments were given under fasted conditions along with 240 mL of water. After administration of the study drug(s), subjects were required to fast for 4 hours. Following a 2-week washout interval, subjects received one of the other treatment regimen. This was repeated until they had received all 3. Subjects were admitted in the Clinical Trial Center (CTC) at Asan Medical Center (AMC) from Days 9 to 11 (24 hours after the last dose) during each treatment period. On Days 12 and 13, all subjects visited the CTC to assess the tolerability and PK of rosuvastatin or ezetimibe. The schedule for the second and third treatment periods was the same as that for the first period. Follow-up visits were performed within 11 days after the last treatment.
For PK analysis, sequential blood samples were collected prior to (Days 1 and 9) and 0, 0.25, 0.5, 1, 1.5, 2, 3, 4, 6, 8, 12, 24, 48, and 72 hours after the Day-10 dose. All blood samples used to determine the concentration of rosuvastatin, total ezetimibe, and free ezetimibe were drawn into EDTA tubes and separated by centrifugation at 1,800 g for 8 minutes at 4°C. Samples were then stored at −70°C until analysis.
Tolerability was assessed throughout the study by: 1) measuring vital signs, 2) 12-lead ECG, 3) clinical laboratory tests (hematology, blood chemistry, and urinalysis), 4) physical examinations, and 5) monitoring of adverse events (AEs). AEs were recorded in terms of symptoms and signs, duration, intensity, relationship to the study drug, action taken, outcome, and seriousness.
The study protocol was approved by the Korean Ministry of Food and Drug Safety and the Institutional Review Board of the AMC, Seoul, Republic of Korea. The study was conducted at the CTC of the AMC from June to September 2014. All subjects provided written informed consent before undergoing screening tests. The trial was registered at ClinicalTrials.gov (identifier number NCT02127320).
Analytical methods
Measurement of rosuvastatin concentrations
The plasma concentration of rosuvastatin was measured using a validated liquid chromatography method with tandem mass spectrometric detection (LC-MS/MS) (Thermo Fisher Scientific, Waltham, MA, USA). The analytical column was Nanospace SI-2 C18 column (75×2.1 mm × 3.0 μm, Shiseido, Tokyo, Japan), and the mobile phase comprised acetonitrile (A), deionized water (B), and formic acid (C) (A:B:C=45:55:0.1, v/v/v). The flow rate was 0.2 mL/minute. For rosuvastatin and the internal standard (rosuvastatin-d6), the precursor-to-production reactions monitored were m/z 482.18 → 258.16 and 488.20 → 264.20, respectively. This assay had a lower limit of quantitation (LLOQ) of 0.5 ng/mL (signal to noise ratio >5), and calibration curves covered the concentration range of 0.5–300 ng/mL (R2 >0.995).
Measurement of ezetimibe and total ezetimibe concentrations
The plasma concentration of free and total ezetimibe (free ezetimibe plus ezetimibe glucuronide) was measured using a validated LC-MS/MS (Sciex API 4000 LC-MS/MS system, Framingham, MA, USA). The analytical column was ACQUITY UPLC C18 column (75×2.0 mm × 3.0 μm, Milford, MA, USA), the mobile phase comprised acetonitrile (A) and 5 mM ammonium acetate (B) [A:B=65:35, v/v]. The flow rate was 0.2 mL/minute. For ezetimibe and the internal standard (ezetimibe-d4), the precursor-to-production reactions monitored were m/z 408.3 → 271.1 and 412.3 → 275.1, respectively. The LLOQ was 0.2 and 0.5 ng/mL for free and total ezetimibe (signal to noise ratio >5), respectively. The calibration curves of free and total ezetimibe covered the concentration range 0.2–200 ng/mL and 0.5–500 ng/mL, respectively (R2 >0.995). All plasma analyses were performed at BioCore Co., Seoul, Republic of Korea.
PK assessment and statistical analysis
The PK of rosuvastatin, free and total ezetimibe in each subject was analyzed using a non-compartmental method with WinNonlin® software 6.3 (Pharsight Co., Princeton, NJ, USA). All analyses were based on actual sampling times. The peak plasma concentration at steady-state (Cmax,ss) and the time taken to reach Cmax,ss (Tmax,ss) were determined from observed values. The terminal elimination rate constant (λz) was estimated by linear regression of the terminal log-linear portion of the plasma concentration-time curves. The t1/2β for each participant was calculated as ln(2)/λz.
All statistical analyses were performed using SAS® software (v 9.3; SAS Institute Inc., Cary, NC, USA) and Phoenix® WinNonlin 6.3. Demographic data and PK parameters were summarized using descriptive statistics. For the comparison of PK characteristics between rosuvastatin or ezetimibe alone with combined administration of rosuvastatin and ezetimibe, Cmax,ss and (AUCτ,ss) were log-transformed and tested by analysis of variance. The mean differences and 90% CIs were back-transformed to obtain geometric mean ratios and CIs for those ratios. Fisher’s exact test was used to compare the frequency of AEs between 2 drugs. A P-value <0.05 was deemed significant.12
Result
Study participants
Of the 24 healthy Korean male volunteers enrolled, 21 completed the study. Three subjects withdrew informed consent for personal reasons. One was before first hospitalization and 2 after second hospitalization. All subjects were included in the tolerability assessment, whereas only the subjects who completed blood sampling as scheduled were included in PK analysis. Participant demographics, including age, height, weight, and body mass index are summarized in Table 1.
  | Table 1 Demographic characteristics of the study participants (n=24) |
PK analysis
To evaluate the PK drug–drug interactions between rosuvastatin and ezetimibe, the PK profiles of rosuvastatin, total and free ezetimibe were separately assessed (Figure 2).
  | Figure 2 Mean (SD) plasma concentration-time curves for rosuvastatin (A), total ezetimibe (B), and free ezetimibe (C). |
Of the 24 subjects who were administered the study drugs, 1 was excluded from all PK analyses due to delay in administering ezetimibe. Finally, 23 subjects were included in the PK analysis of rosuvastatin, and 20 were included in the PK analysis of ezetimibe.
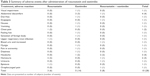
The PK parameters of rosuvastatin in the absence and presence of ezetimibe are shown in Table 2. For rosuvastatin, the steady-state mean ratios of single versus combination doses (90% CI) for AUCτ,ss and Cmax,ss were 1.076 (1.019–1.136) and 1.099 (1.003–1.204), respectively.
For total ezetimibe, the steady-state mean ratios (90% CI) of AUCτ,ss and Cmax,ss were 1.055 (0.969–1.148) and 0.996 (0.873–1.135), respectively, while those for free ezetimibe were 1.131 (1.051–1.218) and 1.182 (1.038–1.346), respectively.
Tolerability
Ten subjects experienced a total of 28 AEs; of these, 23 were considered to be “possibly related” and 2 “probably related” to the study drug. Among the 25 events considered to be related to the study drug, the most common in the ezetimibe alone and ezetimibe plus rosuvastatin group were abdominal pain (4 subjects, 4 events) and headache (3 subjects, 4 events; Table 3). No significant changes in hepatic and renal function test, such as ALT, AST, creatine kinase, serum creatinine, and BUN were observed (data not shown). Laboratory tests revealed microscopic hematuria (occult blood) in 2 subjects: in 1 during the second period after rosuvastatin-only treatment and in the other one at the follow-up visit. No clinically significant abnormalities were found with respect to vital signs, ECGs, and physical examinations. No volunteers dropped out due to AEs and no serious AE occurred during the entire course of the study. All AEs were mild in severity, and resolved without any sequelae.
  | Table 3 Summary of adverse events after administration of rosuvastatin and ezetimibe |
Discussion
The present study examined the potential PK interaction between rosuvastatin and ezetimibe, and their tolerability by healthy male subjects taking multiple oral doses over a 10-day period.
Once absorbed, ezetimibe is extensively metabolized in the intestine to yield its glucuronide conjugate; therefore, it exists mainly as ezetimibe glucuronide in the body. Cholesterol absorption inhibiting activity assays in a rat model demonstrate that both ezetimibe and ezetimibe glucuronide are pharmacologically active and that ezetimibe glucuronide is more potent than ezetimibe of the 2.13 Here, we show that the 90% CIs for the geometric mean ratios of single versus combination treatment for Cmax,ss and AUCmax,ss were 0.80–1.25; the exception was Cmax,ss of free ezetimibe (90% CI, 1.038–1.346). Recently, a PK study in healthy subjects using rosuvastatin (study part A) and ezetimibe (study part B) was reported; however, the study design was 7 day-dosing, 2-treatment, 2-period, 2-sequence crossover study with 2 treatment parts.14 Although the study design was different from the present study, the coadministration increased both Cmax,ss and AUCmax,ss of free ezetimibe (90% CI of Cmax,ss and AUCmax,ss, 0.994–1.285 and 1.094–1.341, respectively). These results suggest that we might need larger sample size when comparing a fixed-dose combination product with separate tablets.
A previous single-dose study of 20 mg ezetimibe reported that the Cmax,ss of free ezetimibe was higher (5.2 ng/mL) than that reported herein (5.0 ng/mL; combination treatment, Table 2); however, no AEs or clinically significant changes were noted on physical examinations.15 As the pharmacological effect of the ezetimibe conjugate is more potent than that of the parent drug, and there is a small amount of free ezetimibe (<8%) in the body, the increase in the Cmax,ss value of free ezetimibe may have no impact on treatment effects or on toxicity.
Kosoglou et al reported that the Tmax of free ezetimibe was 6.0 hours in individuals administered 10 mg rosuvastatin plus 10 mg ezetimibe, and 10 mg of ezetimibe alone for 14 consecutive days; the subjects were mainly Caucasian (87%) with LDL-C levels ≥130 mg/dL.9 These data are consistent with the results presented herein (5.4 and 7.3 hours, respectively). When we compared the Tmax,ss value of free ezetimibe with the time of AE onset, we found no clear association between them, suggesting that AEs were not related to the Cmax,ss. Taken together, rosuvastatin and ezetimibe were well tolerated when administered either alone or concomitantly. We found that the LDL-C level significantly decreased in rosuvastatin-only and combination (rosuvastatin plus ezetimibe) groups (by 43.7% and 56.9%, respectively), but not significantly (9.7%) in the group taking ezetimibe alone, after the 10-day multiple dosing regimen (Table 4). In all treatment groups, the LDL-C levels returned to baseline after a 2-week washout. Although administration of 10 mg of ezetimibe reduced LDL-C levels significantly in volunteers (n=8) with hypercholesterolemia, 1 of 8 subjects in the ezetimibe-only group achieved a 35%–50% reduction compared with half (4/8) of those in the combination group (ezetimibe and fluvastatin).10 This suggests that ezetimibe alone has limited efficacy to control hypercholesterolemia. A recent population pharmacodynamic model of Japanese patients supported the beneficial effects of ezetimibe when combined with rosuvastatin.16 Therefore, ezetimibe is expected to have synergistic effects in patients with hypercholesterolemia.
Previous reports demonstrated multiple peaks in the plasma concentration-time profiles of total and free ezetimibe; this was due to enterohepatic recycling after an oral dose of ezetimibe.17,18 Here, we also observed multiple peaks in PK plots for total and free ezetimibe; these peaks coincided with mealtimes and are thought to be due to enterohepatic recycling (Figure 2). This suggests that food intake triggers the enterohepatic recycling of total ezetimibe by emptying the gallbladder. Further studies based on population PK modeling would help to elucidate the impact of enterohepatic circulation on PK and its inter-individual variation quantitatively. Finally, this study would be important evidence to develop fixed-dose combination tablet to increase patient compliance.19,20
Conclusion
Rosuvastatin (20 mg) and ezetimibe (10 mg) showed no clinically significant PK interactions. Concomitant administration of these 2 drugs was well tolerated by healthy male subjects taking multiple doses over 10 days.
Acknowledgments
This research was sponsored by Hanmi Pharm. Co., Ltd., Seoul, Republic of Korea. We thank Dr Joon Seo Lim from the Scientific Publications Team at AMC for his editorial assistance in preparing this manuscript.
Disclosure
Dr Jung and Dr Son are employees of Hanmi Pharmaceutical Co., Ltd. The other authors report no conflicts of interest in this work.
References
Sytkowski PA, Kannel WB, D’Agostino RB. Changes in risk factors and the decline in mortality from cardiovascular disease. The Framingham Heart Study. N Engl J Med. 1990;322(23):1635–1641. | ||
Lewis SJ, Moye LA, Sacks FM, et al. Effect of pravastatin on cardiovascular events in older patients with myocardial infarction and cholesterol levels in the average range, Results of Cholesterol and Recurrent Events (CARE) trial. Ann Intern Med. 1988;129(9):681–689. | ||
Cortese F, Gesualdo M, Cortese A, et al. Rosuvastatin: beyond the cholesterol-lowering effect. Pharmacol Res. 2016;107:1–18. | ||
Tikkanen MJ. Statin: within-group comparisons, statin escape and combination therapy. Curr Opin Lipidol. 1996;7(6):385–388. | ||
Hammersley D, Signy M. Ezetimibe: an update on its clinical usefulness in specific patient groups. Ther Adv Chronic Dis. 2017;8(1):4–11. | ||
Farnier M. Ezetimibe in hypercholesterolemia. Int J Clin Pract. 2002;56(8):611–614. | ||
Kim KJ, Kim SH, Yoon YW, et al. Effect of fixed-dose combinations of ezetimibe plus rosuvastatin in patients with primary hypercholesterolemia: MRS-ROSE (Multicenter Randomized Study of ROsuvastatin and eZEtimibe). Cardiovasc Ther. 2016;34(5):371–382. | ||
Ballantyne CM, Houri J, Notarbartolo A, et al. Effect of ezetimibe coadministered with atorvastatin in 628 patients with primary hypercholesterolemia. Circulation. 2003;107(19):2409–2415. | ||
Kosoglou T, Statkevich P, Yang B, et al. Pharmacodynamic interaction between ezetimibe and rosuvastatin. Curr Med Res Opin. 2004;20(8):1185–1195. | ||
Reyderman L, Kosoglou T, Cutler DL, Maxwell S, Statkevich P. The effect of fluvastatin on the pharmacokinetics and pharmacodynamics of ezetimibe. Curr Med Res Opin. 2005;21(8):1171–1179. | ||
Sweeney ME, Johnson RR. Ezetimibe: an update on the mechanism of action, pharmacokinetics and recent clinical trials. Expert Opin Drug Metab Toxicol. 2007;3(3):441–450. | ||
Kim YH, Choi HY, Lee SH, et al. Single and multiple dose pharmacokinetics and tolerability of HX-1171, a novel antioxidant, in healthy volunteers. Drug Des Devel Ther. 2015;9:1735–1742. | ||
van Heek M, Farley C, Compton DS, et al. Comparison of the activity and disposition of the novel cholesterol absorption inhibitor, SCH58235, and its glucuronide, SCH60663. Br J Pharmacol. 2000;129(8):1748–1754. | ||
Kim CH, An H, Kim SH, Shin D. Pharmacokinetic and pharmacodynamics interaction between ezetimibe and rosuvastatin in healthy male subjects. Drug Des Devel Ther. 2017;11:3461–3469. | ||
Patrick JE, Kosoglou T, Stauber KL, et al. Disposition of the selective cholesterol absorption inhibitor ezetimibe in healthy male subjects. Drug Metab Dispos. 2002;30(4):430–437. | ||
Kakara M, Nomura H, Fukae M, et al. Population pharmacodynamic analysis of LDL-cholesterol lowering effects by statins and co-medications based on electronic medical records. Br J Clin Pharmacol. 2014;78(4):824–835. | ||
Chu NN, Chen WL, Xu HR, Li XN. Pharmacokinetics and safety of ezetimibe/simvastatin combination tablet. Clin Drug Investig. 2012;32(12):791–798. | ||
Ezzet F, Krishna G, Wexler B, Statkevich P, Kosoglou T, Batra VK. A population pharmacokinetic model that describes multiple peaks due to enterohepatic recirculation of ezetimibe. Clin Ther. 2001;23(6):871–885. | ||
Min KL, Park MS, Jung J, Chang MJ, Kim CO. Comparison of pharmacokinetics and safety of a fixed-dose combination of rosuvastatin and ezetimibe versus separate tablets in healthy subjects. Clin Ther. 2017;39(9):1799–1810. | ||
Kang WY, Seong SJ, Ohk B, et al. Pharmacokimetics and bioequivalence of a rosuvastatin/ezetimibe fixed-dose combination tablet versus single agents in healthy male subjects. Int J Clin Pharmacol Ther. 2018;56(1):43–52. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



