Back to Journals » Drug Design, Development and Therapy » Volume 11
Pharmacokinetic and pharmacodynamic interaction between ezetimibe and rosuvastatin in healthy male subjects
Authors Kim CH, An H, Kim SH, Shin D
Received 20 July 2017
Accepted for publication 7 November 2017
Published 5 December 2017 Volume 2017:11 Pages 3461—3469
DOI https://doi.org/10.2147/DDDT.S146863
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Tuo Deng
Chang Hee Kim,1 Hyungmi An,2 Sung Hye Kim,3 Dongseong Shin4
1Department of Urology, Gachon University Gil Medical Center, Incheon, 2Department of Statistics, Seoul National University, Seoul, 3Clinical Development, Navipharm Co., Ltd., Suwon, 4Clinical Trials Center, Gachon University Gil Medical Center, Incheon, South Korea
Background and objective: Rosuvastatin and ezetimibe are commonly applied in lipid-lowering pharmacotherapy. However, the pharmacokinetic (PK) interaction was not clear by the coadministration of rosuvastatin and ezetimibe. This study investigated the pharmacodynamic (PD) and PK interactions between rosuvastatin and ezetimibe through a crossover clinical trial.
Subjects and methods: A randomized, open-label, multiple-dose, two-treatment, two-period, two-sequence crossover study with two treatment parts was conducted in healthy male subjects. Study part A involved rosuvastatin, and study part B involved ezetimibe. A total of 25 subjects in both parts completed the PK and PD evaluations. Rosuvastatin (20 mg) or ezetimibe (10 mg) was administered once daily for 7 days as monotherapy or co-therapy. The plasma concentrations of rosuvastatin, total ezetimibe and free ezetimibe were measured for 72 h after day 7. Low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C) and total cholesterol (TC) were investigated for the PD assessments on day 1 (pretreatment) and day 8.
Results: Rosuvastatin and ezetimibe presented multiple peaks. The 90% confidence intervals (CIs) of the geometric mean ratios for the peak plasma concentration at steady state (Cmax,ss) and area under the plasma concentration–time curve during the dosing interval at steady state (AUCt,ss) of rosuvastatin and total ezetimibe were within the range 0.8–1.25. However, the coadministration increased the systemic exposure of free ezetimibe. In the PD assessments, rosuvastatin and ezetimibe monotherapy reduced the LDL-C and TC levels effectively. In addition, the lipid-lowering effects of the coadministration corresponded to an approximate summation of the effects of rosuvastatin and ezetimibe monotherapy. However, no significant changes in HDL-C were observed with rosuvastatin or ezetimibe treatment. No significant safety issue was noted.
Conclusion: The coadministration of rosuvastatin and ezetimibe revealed a bioequivalent PK interaction. Additional lipid-lowering effects, including decreased LDL-C and TC, were observed as expected in combination therapy without significant safety concern.
Keywords: pharmacokinetics, pharmacodynamics, drug interaction, rosuvastatin, ezetimibe
Introduction
Statins are used as a first-choice treatment in lipid-lowering pharmacotherapy.1 However, approximately one-third of statin-treated patients experience difficulty in reaching their low-density lipoprotein cholesterol (LDL-C) goals because of poor compliance, variability in drug response, inadequate titration of applied doses and safety issues associated with higher doses.2,3 Among statins, rosuvastatin is the most efficacious and is relatively safe, with low rates of severe myopathy, rhabdomyolysis and renal failure.1,4 Because of its high hydrophilicity, hepatoselectivity and low systemic bioavailability, rosuvastatin is minimally metabolized via the cytochrome P450 system and is likely excreted mainly by organic anion transporter protein 1B1 (OATP 1B1).4
Ezetimibe is a cholesterol absorption inhibitor that blocks the transport of dietary and biliary cholesterol from the small intestine.3 After oral intake, ezetimibe is biotransformed to ezetimibe glucuronide, which is an active metabolite in the intestinal mucosa and liver.3 Regarding the pharmacological activity in the blockade of cholesterol absorption, ezetimibe glucuronide is more potent than the parent drug.5
The beneficial effects of ezetimibe combination therapy with statins have been demonstrated in patients with a high risk of cardiovascular disease or a severely high LDL-C level.6,7 Furthermore, one report demonstrated that when rosuvastatin was coadministered with ezetimibe in healthy hypercholesterolemic subjects, an additional LDL-C-lowering effect could be expected compared to that with rosuvastatin monotherapy and ezetimibe monotherapy, without a significant pharmacokinetic (PK) interaction.8 However, since this result was obtained in a small, parallel-group study, the PK interaction did not meet the bioequivalence acceptance criteria.8 The aim of the current study was to evaluate the PK and pharmacodynamic (PD) interactions between rosuvastatin and ezetimibe in healthy Korean male subjects after multiple oral administrations through a crossover clinical study.
Subjects and methods
Study population and design
Healthy male subjects between 19 and 45 years of age and within ±20% of their ideal body weight were eligible if they did not have clinically significant medical histories, physical examination findings, 12-lead electrocardiogram (ECG) readings or clinical laboratory testing results. Volunteers who showed creatinine clearance under 80 mL/min by the Cockcroft-Gault equation were also excluded from this study. The institutional review board of Gachon University Gil Medical Center approved this protocol and provided informed consent for this study. Written informed consent forms were obtained before enrollment.
This drug interaction study consisted of two parts: study part A evaluated rosuvastatin, and study part B evaluated ezetimibe (Figure 1). Both study part A and study part B were randomized, open-label, multiple-dose, two-treatment, two-sequence crossover studies and were conducted in accordance with the recommendations of the Korean Good Clinical Practice and the Declaration of Helsinki (ClinicalTrials.gov registry number: NCT02289430). In total, 56 subjects were randomly assigned to one of the two sequences (28 in each). In study part A, rosuvastatin (20 mg) or rosuvastatin (20 mg) and ezetimibe (10 mg) were administered once daily for 7 days. In study part B, ezetimibe (10 mg) or rosuvastatin (20 mg) and ezetimibe (10 mg) were administered once daily for 7 days. A 14-day washout period was required between the dosing periods. The subjects received the study drug during outpatient visits for 6 days. The last dose was given during a 2-day hospitalization period, and the PK assessment was then conducted. The subjects were given the study drugs with 240 mL of water while in a fasting state.
PK assessment
Blood samples at steady state (day 7) were collected prior to dosing (0 h) and at 0.5, 1, 1.5, 2, 2.5, 3, 3.5, 4, 5, 6, 8, 12, 24, 48 and 72 h post-dosing to evaluate the plasma concentrations of rosuvastatin, free ezetimibe and total ezetimibe (free ezetimibe and ezetimibe glucuronide). Blood samples were obtained in K2-ethylenediaminetetraacetic acid (EDTA) tubes and centrifuged at 3,000 rpm at 4°C for 10 min. The separated plasma was frozen and stored at −70°C until analysis.
For the analysis of rosuvastatin, 300 μL of plasma sample was mixed with 100 μL of sodium acetate trihydrate (pH 4.0, 0.2 M). After the addition of 20 μL of internal standard (rosuvastatin-d6 sodium salt) solution (200 ng/mL) into 200 μL of this mixture, the mixture was extracted with 1.2 mL of methyl tert-butyl ether for 20 min and centrifuged at 3,000 rpm for 5 min. The organic phase was dried with nitrogen gas, and the residue was dissolved in 150 μL of mobile phase and centrifuged at 13,000 rpm for 5 min. High-performance liquid chromatography (HPLC, Shiseido Nanospace SI-2 system; Shiseido, Tokyo, Japan) and triple-quadrupole mass spectrometry (MS, TSQ Quantum Discovery MAX; Thermo Fisher Scientific, Waltham, MA, USA) in positive ionization mode were used for the quantitative analysis of rosuvastatin with an internal standard. Chromatographic separation was performed at 40°C using a Unison UK-C18 column (75×2.0 mm, 3 μm; Imtakt, Kyoto, Japan) with a mobile phase of acetonitrile:deionized water:formic acid (45:55:0.1, v/v/v). The detection range for rosuvastatin was 0.5–300 ng/mL. The intrabatch precision and accuracy of the quality control samples were less than 15.7% and 93.7%–107.5%, respectively. The corresponding interbatch values were less than 10.5% and 94.2%–105.4%, respectively.
For the analysis of free ezetimibe, 100 μL of plasma sample and 20 μL of internal standard (ezetimibe-d4) solution (100 ng/mL) were mixed and extracted with 1 mL of methyl tert-butyl ether for 20 min. After centrifugation at 3,000 rpm for 5 min, the separated organic phase was dried with nitrogen gas. The residue was dissolved in 500 μL acetonitrile and centrifuged at 13,000 rpm for 5 min, and then 5 μL of supernatant was injected into liquid chromatography–MS/MS system. For total ezetimibe, 100 μL of plasma sample and 10 μL of internal standard (ezetimibe-d4) solution (5,000 ng/mL) were transferred to a polypropylene tube. Then, 75 μL of sodium acetate buffer (0.5 M, pH 5.0 with acetic acid) and 15 μL of β-glucuronidase were added. After vortexing for 15 s, the mixture was incubated at 50°C for 30 min. In addition, 75 μL of sodium borate solution (0.1 M) was added into the tube. The solution was extracted with 1 mL of methyl tert-butyl ether for 5 min and centrifuged at 13,000 rpm for 5 min. The organic phase was dried with nitrogen gas. The residue was dissolved in 500 μL acetonitrile and centrifuged at 13,000 rpm for 5 min.
The plasma concentrations of total ezetimibe were measured with an HPLC–MS system, which consisted of a Nanospace 5200A spectrometer (Nasca; Shiseido) and a triple-quadrupole linear ion trap MS system (6500 Q-Trap; AB Sciex, Foster City, CA, USA).
The detection range for total ezetimibe was 0.5–500 ng/mL. The intrabatch precision and accuracy of the quality control samples were less than 9.4% and 90.8%–100.4%, respectively. The corresponding interbatch values were less than 6.9% and 94.1%–95.2%, respectively.
The plasma concentrations of free ezetimibe were measured with an HPLC–MS system consisting of a Shimadzu Prominence instrument (Shimadzu Corporation, Kyoto, Japan) and a triple-quadrupole linear ion trap MS system (API5000; AB Sciex). The detection range for total ezetimibe was 0.2–200 ng/mL. The intrabatch precision and accuracy of the quality control samples were less than 5.3% and 95.0%–105.9%, respectively, and the corresponding interbatch values were less than 5.0% and 95.6%–103.7%, respectively. The chromatographic separations of both ezetimibe and total ezetimibe were performed at 40°C using a Unison UK-C18 column (75×2.0 mm, 3 μm; Imtakt) with a mobile phase of 5 mM ammonium acetate:acetonitrile (35:65, v/v). The accuracy of short-term stability at room temperature and long-term stability at −70°C for plasma rosuvastatin, ezetimibe and total ezetimibe was within 85%–115%. The precision of short-term stability and long-term stability for these three analytes were under 15%.
PD assessment
Blood samples for the measurement of LDL-C, high-density lipoprotein cholesterol (HDL-C) and total cholesterol (TC) were obtained pre-dose (day 1) and at steady state (day 8). Blood (5 mL) was collected in serum separator tubes and centrifuged at 2,000 g for 10 min. The serum levels of LDL-C, HDL-C and TC were determined by the Department of Laboratory Medicine of Gachon University Gil Medical Center using an ADVIA® Chemistry XPT System (Global Siemens Headquarters, Munich, Germany). The detection ranges for LDL-C, HDL-C and TC were 0–1,000 mg/dL, 5–115 mg/dL and 10–675 mg/dL, and the intra-assay coefficients of variation were 0.5%–0.6%, 1.1%–1.5% and 0.5%–0.6%, respectively.
PK and PD analyses
The primary PK parameters (peak plasma concentration at steady state [Cmax,ss] and area under the plasma concentration–time curve during the dosing interval at steady state [AUCτ,ss]) for rosuvastatin, ezetimibe and total ezetimibe were estimated based on the non-compartmental method of WinNonlin® 6.4 (Pharsight Co., Cary, NC, USA). Cmax,ss was directly obtained from the plasma concentration–time profiles. AUCτ,ss was calculated using the linear-up/log-down trapezoidal method. The slope of the terminal log-linear phase in the plasma concentration–time profile was used as the elimination rate constant (λz), which was estimated by a least-squares linear regression. The terminal elimination half-life at steady state (t1/2,ss) was determined as ln(2)/λz. Log-transformed Cmax,ss and AUCτ,ss were analyzed to evaluate the PK interaction. The mean difference between treatments was back-transformed to calculate the geometric mean ratios (GMRs) and 90% confidence intervals (CIs) for the GMRs. The GMRs of Cmax,ss and AUCτ,ss between the treatments were estimated with a linear mixed-effects model that included sequence, period and treatment as fixed effects and subject nested within sequence as a random effect. If the two-sided 90% CIs for the GMRs between mono- and co-therapy were within the range 0.80–1.25, the drug interaction was considered insignificant.
The lipid-lowering effects of rosuvastatin or ezetimibe monotherapy and co-therapy on LDL-C, HDL-C and TC were also compared in a mixed-effect model based on the percent changes in the lipid profiles from baseline (pre-dose) to steady state. Statistical significance was considered at P<0.05. SPSS 22.0 (IBM Corporation, Armonk, NY, USA) was applied for these evaluations.
Safety and tolerability
Safety and tolerability were investigated via spontaneous reporting and inquiries regarding adverse events (AEs). Physical examinations, vital sign measurements, 12-lead ECG and laboratory tests, such as hematology, serum chemistry and urinalysis, were also performed for tolerability monitoring.
Results
Demographics and baseline characteristics
In each part of the study, 28 subjects were randomly assigned to one of the two sequences. Six subjects discontinued due to consent withdrawal. Ultimately, 50 subjects (25 in study part A and 25 in study part B) completed the study, and the PK conclusion was based on the results of these subjects. Mean ± standard deviation (SD) values for age, weight, height and body mass index (BMI) in study part A and study part B were 25±4 and 27±7 years, 71.5±10.9 and 69.0±8.3 kg, 174.9±6.9 and 174.6±6.3 cm and 23.3±2.4 and 22.6±2.1 kg/m2, respectively. Except for their heights, the participants’ demographic characteristics did not differ significantly between the sequences and parts.
PK characteristics
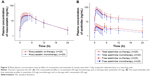
After the 7-day administration of rosuvastatin monotherapy and co-therapy with ezetimibe, the median times to reach the maximum plasma concentration at steady state (Tmax,ss) were 5 and 3 h, with t1/2,ss values of 12.2 and 10.4 h, respectively. Tmax,ss and t1/2,ss did not differ between co-therapy and monotherapy (P=0.126 and P=0.467, respectively). The Cmax,ss and AUCτ,ss of rosuvastatin were equivalent between co-therapy and monotherapy. The GMRs of Cmax,ss and AUCτ,ss were 1.037 and 1.037, with 90% CIs of 0.945–1.137 and 0.977–1.101, respectively (Table 1 and Figure 2A).
For ezetimibe monotherapy and co-therapy with rosuvastatin, the median Tmax of total ezetimibe was 1 h, after which the concentration decreased, with mean t1/2,ss values of 17.3 and 20.7 h, respectively. Free ezetimibe reached a peak plasma level at ~2 h after administration in both treatments. The GMRs of Cmax,ss and AUCτ,ss for total ezetimibe were 1.069 and 1.130, respectively, and the 90% CIs were 0.976–1.171 and 1.022–1.249, respectively, which were within the range 0.8–1.25. However, the PK profiles of free ezetimibe were higher for co-therapy with rosuvastatin than for ezetimibe monotherapy. The GMRs (90% CIs) of Cmax,ss and AUCτ,ss were 1.130 (0.994–1.285) and 1.211 (1.094–1.341), respectively. The Tmax,ss and t1/2,ss for total ezetimibe did not differ from the drug interaction perspective (P=0.395 and P=0.270, respectively; Table 1 and Figure 2B).
In both rosuvastatin and ezetimibe concentration–time profiles, the secondary peaks were observed after initial absorption peaks. Especially, in free ezetimibe, this phenomenon was remarkable and t1/2,ss could not be presented.
PD characteristics
The baseline LDL-C levels in study part A were 87.2±25.9 and 89.1±21.0 mg/dL in rosuvastatin monotherapy and co-therapy with ezetimibe, respectively, and were not significantly different (P=0.829). In study part B, the pretreatment LDL-C levels were similar between the two treatment groups: 99.4±22.5 mg/dL in ezetimibe monotherapy and 99.9±29.6 mg/dL in co-therapy with rosuvastatin (P=0.942). The other lipid profiles, including HDL-C and TC at pretreatment, did not differ between the treatment periods (P=0.852 and P=0.399 for HDL-C and P=0.922 and P=0.674 for TC in study part A and study part B, respectively; Table 2). The lipid profiles were not influenced by the previous treatment during the washout period.
After co-therapy with rosuvastatin and ezetimibe, cholesterol levels decreased to a greater degree than after rosuvastatin or ezetimibe monotherapy (Figure 3). Co-therapy reduced LDL-C by 65.3% and 64.6% in study part A and study part B, respectively, and the resulting values were 19.4% (95% CI: 14.0%–24.8%) and 41.3% (95% CI: 35.5%–47.1%) lower than those achieved with rosuvastatin and ezetimibe alone, respectively. In addition, co-therapy reduced the TC by 10.3% (95% CI: 6.4%–14.1%) and 26.4% (95% CI: 22.0%–30.7%) more than rosuvastatin or ezetimibe monotherapy, respectively. However, the co-therapy did not result in changes in the HDL-C, which were not significantly different compared to those achieved with monotherapies (P=0.219 for rosuvastatin and P=0.251 for ezetimibe).
Safety and tolerability
In study part A, three of the 27 participants (11.1%) in the rosuvastatin monotherapy group and one of the 26 participants (3.8%) in the co-therapy group reported drug-related AEs. The most commonly reported AEs were myalgia in monotherapy and myalgia and dizziness in co-therapy. In study part B, three of the 28 participants (10.7%) in the ezetimibe monotherapy group and 0 of the 26 participants (0%) in the co-therapy group reported drug-related AEs. Commonly reported drug-related AEs included eye pruritus, toothache, myalgia, cough and rhinorrhea in the ezetimibe monotherapy group. All AEs were mild, and no other abnormal findings, including vital signs, 12-lead ECG, physical examination and clinical laboratory tests, were reported. None of the subjects withdrew from this clinical study due to AEs.
Discussion
Statin combination therapies with ezetimibe are commonly considered to control blood cholesterol for the successful management of cardiovascular risk.9 Indeed, in a previous study, the coadministration of rosuvastatin and ezetimibe was effectively reported to reduce LDL-C and TC levels without a significant PK interaction in a small number of patients with primary hypercholesterolemia.8 However, the primary PK parameters, including Cmax and AUCτ, did not satisfy the bioequivalence criteria.8 This multiple-dose, crossover clinical study presented quantitative information about the PK and PD interactions between rosuvastatin and ezetimibe at steady state in healthy Korean subjects with sufficient power.
In the current study, a once-daily dose of rosuvastatin administered for 7 days resulted in multiple peaks of plasma concentration, with a terminal half-life of 10.4–12.2 h and a mean accumulation ratio at steady state of 1.3–1.4. These PK results of rosuvastatin in healthy Korean subjects were comparable to those found in other Asians, including Japanese and Chinese subjects.10 Coadministration with ezetimibe had limited effects on the systemic exposure of rosuvastatin, consistent with the results found for combinations of other statins and ezetimibe.11
At steady state after 7-day dosing, the plasma concentration–time profiles of total ezetimibe revealed that the terminal half-life was 17.2–20.7 h and that the mean accumulation ratio was 1.6–1.8. Since the multiple peaks of free ezetimibe caused by enterohepatic recirculation were more remarkable than those found for total ezetimibe, the terminal half-life and accumulation ratio of free ezetimibe could not be determined.3,8 The mean systemic exposure of free ezetimibe based on the AUCτ,ss was 13.6%–14.5% of total ezetimibe. When ezetimibe was administered in combination with rosuvastatin, rosuvastatin increased the systemic exposure of free ezetimibe. However, the 90% CIs of the GMRs for both the Cmax,ss and AUCτ,ss of total ezetimibe were within the range 0.8–1.25 (ie, the bioequivalence limits). In terms of pharmacological activity, total ezetimibe was considered the primary end point to evaluate the drug interaction instead of free ezetimibe because ezetimibe glucuronide, the metabolite of ezetimibe, is as potent as the unchanged form in the inhibition of intestinal cholesterol absorption.3,5 Consequently, the PK interaction between rosuvastatin and ezetimibe was not significant and satisfied the bioequivalence criteria.
Rosuvastatin is mainly eliminated unchanged in feces, and ~10% of the oral dose undergoes hepatic metabolism via cytochrome P450 (CYP) 2C9 and 2C19.12 Because the major metabolite, N-desmethyl rosuvastatin, which is produced primarily by CYP 2C9, exhibits one-sixth to one-half of the 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase inhibition of rosuvastatin, the drug interactions of the metabolically mediated drug may be clinically insignificant.12
In contrast, more than 80% of ezetimibe is metabolized to pharmacologically active ezetimibe glucuronide in the intestine and liver.3 UDP glycosyltransferase (UGT) 1A1, 1A3 and 2B15 are responsible for the glucuronidation of ezetimibe.3 In the metabolic pathway of rosuvastatin, glucuronidation was found to be partially involved in the metabolism of statins, possibly resulting in PK interactions between rosuvastatin and the glucuronidation-metabolized drug.13–15 However, the competitive inhibition of glucuronidation, which is a common metabolic pathway, may contribute to the increased exposure of free ezetimibe. The overall PK interaction between ezetimibe and rosuvastatin was not significant due to either the existence of multiple clearance pathways or the extensive capacity of UGT enzymes.16
PD effects were investigated through changes in LDL-C, HDL-C and TC according to the PK interaction. At steady state, the coadministration of rosuvastatin and ezetimibe exerted significant lipid-lowering effects on LDL-C and TC. The coadministration led to reductions in LDL-C that were 19.4% and 41.3% greater than those achieved with rosuvastatin and ezetimibe monotherapies, respectively. For TC, co-therapy led to reductions that were 10.3% and 26.4% greater than those observed for rosuvastatin and ezetimibe monotherapies, respectively. These enhanced effects observed for co-therapy were similar to the summed effects of the corresponding monotherapies studied in the opposite part of the clinical trial. Rosuvastatin exerts lipid-lowering effects through the competitive inhibition of HMG-CoA reductase, which catalyzes the rate-limiting step in cholesterol biosynthesis.14 Ezetimibe inhibits cholesterol uptake by binding to a specific transport protein, including Niemann-Pick C1-Like 1 (NPC1L1) protein, in the wall of the small intestine.3,14 These lipid-lowering mechanisms were independent between rosuvastatin and ezetimibe, and thus, the coadministration of these drugs can produce additive effects in the reduction of LDL-C and TC.8 Regarding HDL-C, it did not show a significant change at steady state after either co-therapy or monotherapy and no difference was found between the individual monotherapies and co-therapy. Although a modest increase in HDL-C in patients with hypercholesterolemia was reported in some previous studies of ezetimibe and rosuvastatin, meaningful effects on HDL-C were not detected in this study of healthy subjects.17,18
Conclusion
At steady state, rosuvastatin and ezetimibe showed no significant interaction in terms of tolerability or PK and PD profiles. The extents of LDL-C and TC reduction were additive with the coadministration of rosuvastatin and ezetimibe. Therefore, in our crossover clinical trial, combination therapy with rosuvastatin and ezetimibe resulted in additive lipid-lowering effects with PK bioequivalence, as expected.
Acknowledgments
This study was sponsored by Navipharm Co., Ltd, Suwon, Korea, supported by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI) and funded by the Ministry of Health & Welfare, Republic of Korea (grant numbers: HI17C1919 and HI14C2750). The investigation was conducted at the Clinical Trials Center, Gachon University Gil Medical Center.
Disclosure
Sung Hye Kim is an employee of Navipharm Co., Ltd. The other authors report no conflicts of interest in this work.
References
Brault M, Ray J, Gomez YH, Mantzoros CS, Daskalopoulou SS. Statin treatment and new-onset diabetes: a review of proposed mechanisms. Metabolism. 2014;63(6):735–745. | ||
Waters DD, Brotons C, Chiang CW, et al; Lipid Treatment Assessment Project 2 Investigators. Lipid treatment assessment project 2: a multinational survey to evaluate the proportion of patients achieving low-density lipoprotein cholesterol goals. Circulation. 2009;120(1):28–34. | ||
Kosoglou T, Statkevich P, Johnson-Levonas AO, Paolini JF, Bergman AJ, Alton KB. Ezetimibe: a review of its metabolism, pharmacokinetics and drug interactions. Clin Pharmacokinet. 2005;44(5):467–494. | ||
Kostapanos MS, Milionis HJ, Elisaf MS. Rosuvastatin-associated adverse effects and drug-drug interactions in the clinical setting of dyslipidemia. Am J Cardiovasc Drugs. 2010;10(1):11–28. | ||
van Heek M, Farley C, Compton DS, et al. Comparison of the activity and disposition of the novel cholesterol absorption inhibitor, SCH58235, and its glucuronide, SCH60663. Br J Pharmacol. 2000;129(8):1748–1754. | ||
Stone NJ, Robinson JG, Lichtenstein AH, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 pt B):2889–2934. | ||
Authors/Task Force M, Catapano AL, Graham I, et al. 2016 ESC/EAS guidelines for the management of dyslipidaemias: the task force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS) Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Atherosclerosis. 2016;253:281–344. | ||
Kosoglou T, Statkevich P, Yang B, et al. Pharmacodynamic interaction between ezetimibe and rosuvastatin. Curr Med Res Opin. 2004;20(8):1185–1195. | ||
Catapano AL, Graham I, De Backer G, et al; Authors/Task Force Members; Additional Contributor. 2016 ESC/EAS guidelines for the management of dyslipidaemias. Eur Heart J. 2016;37(39):2999–3058. | ||
Lee E, Ryan S, Birmingham B, et al. Rosuvastatin pharmacokinetics and pharmacogenetics in white and Asian subjects residing in the same environment. Clin Pharmacol Ther. 2005;78(4):330–341. | ||
Gagne C, Bays HE, Weiss SR, et al; Ezetimibe Study Group. Efficacy and safety of ezetimibe added to ongoing statin therapy for treatment of patients with primary hypercholesterolemia. Am J Cardiol. 2002;90(10):1084–1091. | ||
Olsson AG, McTaggart F, Raza A. Rosuvastatin: a highly effective new HMG-CoA reductase inhibitor. Cardiovasc Drug Rev. 2002;20(4):303–328. | ||
Prueksaritanont T, Tang C, Qiu Y, Mu L, Subramanian R, Lin JH. Effects of fibrates on metabolism of statins in human hepatocytes. Drug Metab Dispos. 2002;30(11):1280–1287. | ||
Rosenson RS. Rosuvastatin: a new inhibitor of HMG-coA reductase for the treatment of dyslipidemia. Expert Rev Cardiovasc Ther. 2003;1(4):495–505. | ||
Prueksaritanont T, Subramanian R, Fang X, et al. Glucuronidation of statins in animals and humans: a novel mechanism of statin lactonization. Drug Metab Dispos. 2002;30(5):505–512. | ||
Kosoglou T, Statkevich P, Fruchart JC, et al. Pharmacodynamic and pharmacokinetic interaction between fenofibrate and ezetimibe. Curr Med Res Opin. 2004;20(8):1197–1207. | ||
Bays HE, Moore PB, Drehobl MA, et al; Ezetimibe Study Group. Effectiveness and tolerability of ezetimibe in patients with primary hypercholesterolemia: pooled analysis of two phase II studies. Clin Ther. 2001;23(8):1209–1230. | ||
Blasetto JW, Stein EA, Brown WV, Chitra R, Raza A. Efficacy of rosuvastatin compared with other statins at selected starting doses in hypercholesterolemic patients and in special population groups. Am J Cardiol. 2003;91(5A):3C–10C; discussion 10C. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.