Back to Journals » Neuropsychiatric Disease and Treatment » Volume 15
Personality associated with depressive status in individuals with type 2 diabetes mellitus
Authors Yasui-Furukori N, Murakami H, Otaka H, Nakayama H, Murabayashi M, Mizushiri S, Matsumura K, Tanabe J, Matsuhashi Y, Yanagimachi M, Nakamura K, Daimon M , Sugawara N
Received 31 December 2018
Accepted for publication 1 April 2019
Published 3 May 2019 Volume 2019:15 Pages 1133—1139
DOI https://doi.org/10.2147/NDT.S200012
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Taro Kishi
Norio Yasui-Furukori,1,2 Hiroshi Murakami,3 Hideyuki Otaka,3 Hirofumi Nakayama,3 Masaya Murabayashi,3 Satoru Mizushiri,3 Koki Matsumura,3 Jutaro Tanabe,3 Yuki Matsuhashi,3 Miyuki Yanagimachi,3 Kazuhiko Nakamura,2 Makoto Daimon,3 Norio Sugawara1,4
1Department of Psychiatry, Dokkyo Medical University School of Medicine, Tochigi, Japan; 2Department of Neuropsychiatry, Hirosaki University Graduate School of Medicine, Hirosaki, Japan; 3Department of Endocrinology and Metabolism, Hirosaki University Graduate School of Medicine, Hirosaki, Japan; 4Department of Clinical Epidemiology, Translational Medical Center, National Center of Neurology and Psychiatry, Kodaira, Tokyo, Japan
Objective: Type 2 diabetes mellitus (T2DM) is associated with a high prevalence of depression, and depression is influenced by personality traits; however, these psychological factors have not been well studied in individuals with T2DM. The association between the use of a 5-factor model of personality and depressive symptoms was examined in individuals with T2DM.
Methods: The subjects were 435 T2DM patients (mean age 63.1±12.6 years). Depressive status and personality traits were assessed using the Center for Epidemiologic Studies Depression Scale and the Ten-Item Personality Inventory, Japanese version, respectively. Lifestyle factors and glycated hemoglobin A1c levels in the patients were also included in the analyses.
Results: Among the 435 subjects with T2DM, 130 (29.9%) exhibited possible depression, and 68 (15.6%) exhibited probable depression. After adjustment for confounders, Extraversion, Agreeableness and Neuroticism were found to be significantly associated with the presence of depression. No relationships were found between depression and HbA1c.
Conclusion: These findings indicate that Extraversion and Agreeableness are protective factors, and Neuroticism is a risk factor for depression in T2DM patients. Psychological therapy focusing on personality may reduce depressive symptoms. Additional studies are needed to examine the relationships between psychological factors and depressive symptoms using a longitudinal study design.
Keywords: cross-sectional studies, depressive symptoms, Japanese, personality, type 2 diabetes
Introduction
The high prevalence of type 2 diabetes mellitus (T2DM) as a lifestyle-related disease has become a burden, and T2DM can increase the risk of both serious physical and mental health issues. Depression is two times more common in patients with diabetes than in the general population, with differing rates in patients with type 1 diabetes (21.3%) and T2DM (27.0%).1 A recent meta-analysis suggests that the pooled relative risk for T2DM is 1.41–1.43 for depression.2,3 Because cerebral small vessel lesions are associated with depressive symptoms due to damage to deep and frontal brain structures that regulate mood, the vascular depression hypothesis may be potentially relevant in T2DM.4,5 In addition, the inflammatory pathway may involve oxidative stress as well as endothelial dysfunction, and markers of these processes are associated with depression6–9 and are known risk markers for T2DM.10,11 Prolonged hyperglycemia or hypoglycemia can lead to negative emotion in T2DM patients.12
Personality variability determines individual stress reactivity and the psychological adjustment to diabetes. Previous studies have found that individuals with T2DM and depressive and anxious temperaments adjusted differently to diabetes and have worse self-management and metabolic control than subjects without a predominant affective temperament.13–15 In addition, previous studies have suggested that personality is associated with the onset of depressive symptoms in T2DM patients.16,17 These studies used the Temperament Evaluation of Memphis, Pisa, Paris and San Diego (TEMPS-A) as a measurement tool for personality. In recent decades, however, the Five-Factor Model has been widely accepted in both clinical practice and scientific research to conceptualize personality.18 Higher levels of Neuroticism and lower levels of Extraversion and Conscientiousness have been associated with depression in individuals without T2DM.19–23 No studies, however, have examined the potential link between the Five-Factor Model and depressive symptoms among individuals with T2DM.
In the present study, we aimed to investigate the relationship between the Five-Factor Model-based personality traits and depressive symptoms among individuals with T2DM. We hypothesized that three personality strategies (Neuroticism, Extraversion and Conscientiousness) would be associated with depressive symptoms even in individuals with T2DM.
Methods
Participants
This study was conducted in accordance with the Declaration of Helsinki. This study was approved by the ethics committee of the Graduate school of Medicine, Hirosaki University, and written informed consent was obtained from each subject before they could participate in this study.
The subjects were 728 individuals with T2DM who received treatment for at least 1 year at the Department of Endocrinology and Metabolism at the Hirosaki University Hospital. We collected 945 patients, and 728 agreed to take part in the study. The remaining 217 patients were excluded because of declining to participate (41 patients), moderate to severe dementia (85 patients), blindness (23 patients), and moderate to severe psychiatric diseases (eg, schizophrenia and bipolar disorder; 68 patients). A total of 611 patients out of 728 returned the questionnaires, and 435 had complete questionnaires. Thus, in total, 435 patients were included in the study. The final sample included 435 participants for an overall response rate of 59.7%.
Blood laboratory examinations from these patients were conducted routinely for glycated hemoglobin A1c (HbA1c) analysis at least 4 times per year. Among the subjects, 385 were receiving an oral hypoglycemic agent, and 215 were receiving insulin therapy. The demographic data (age, sex, alcohol consumption, smoking, marital status, solitary living, and exercise habits) and medical histories of the patients were obtained from questionnaires and medical records.
The Japanese version of the Center for Epidemiologic Studies Depression Scale (CES-D) was administered to all of the participants to measure their depressive symptoms.24 The CES-D is a 20-item self-reported measure that focuses on the depressive symptoms the patient experienced during the week prior to completing the questionnaire. The maximum score is 60, with higher scores indicating more severe depressive symptoms. The standard cut-off score of −16 for the CES-D had excellent sensitivity (91.3%) but low specificity (60.8%). A cut-off score of −21 on the CES-D yielded an optimal balance between sensitivity (78.3%) and specificity (74.3%), with a positive predictive value (PPV) of 48.6% and a negative predictive value (NPV) of 91.7%.25 In addition, our previous study indicated that the stratum-specific likelihood ratios (SSLRs) were 0.13 (95% CI 0.04–0.40), 3.68 (95% CI 1.37–9.89)and 24.77 (95% CI 14.97–40.98) for CES-D scores of 0–16, 17–20, and above 21, respectively.26 Therefore, possible depression was considered to be present when a subject reported a CES-D score of −16, while probable depression was considered to be present when a subject reported a CES-D score of −21 based on our previous study.
We used the Japanese version of the Ten-Item Personality Inventory (TIPI-J) to measure personality traits. The TIPI-J is a measure of the Big-Five personality dimensions: Extraversion, Conscientiousness, Agreeableness, Neuroticism, and Openness to experience.27 Each item was scored from 1 to 7 points, and the scores were summed for each 3 dimensions. The tests of validation and reliability for TIPI-J have been established in Japan.28
Statistical analysis
In the present study, comparisons of several factors between patients with and without depression were performed using Student’s t-tests and chi-square tests. The data are presented as the means±standard deviations. A p-value <0.05 indicated statistical significance. The factors associated with depression were examined using logistic regression analyses with forced entry; they included age, sex, body mass index (BMI), HbA1c, presence/absence of smoking, habitual alcohol consumption, living alone, and exercise habits, each score for the 5 personality dimensions. In addition, linear regression analyses with forced entry were performed to examine the correlation between the severity of depression (total CES-D scores) and several factors. The dummy variables were as follows: male =1, female =2, living with family =0, living alone =1, presence of spouse =1, absence of spouse =2, presence of smoking =1, absence of smoking =2, presence of alcohol consumption =1, absence of alcohol consumption =2, no exercise =1, exercise once a week =2, exercise 2–3 days per week =3, exercise 4–5 days per week =4, and exercise almost every day =5. When α =0.05 and β =0.2 with a two-sided test, the estimated sample size is 133. A p-value <0.05 indicated statistical significance. The SPSS Statistics software program for Windows, version 25.0, was used for all analyses.
Results
A total of 130 (29.9%) of the 435 patients had possible depression based on the standard CES-D cut-off value of 15.5; however, we regarded 21.5 as the solid CES-D cut-off value, as previously described. Thus, 64 (14.7%) patients exhibited probable depression.
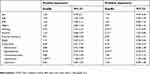
There were significant differences in all the personality traits (Extraversion, Agreeableness, Conscientiousness, Neuroticism and Openness) between the patients with and without possible depression; however, there were no differences in HbA1c, lifestyle or marital status (Table 1). There were significant differences in BMI, smoking habits, Extraversion, Agreeableness, Conscientiousness, and Neuroticism between the patients with and without probable depression, but there were no differences in age, HbA1c, major lifestyle factors or marital status (Table 1).
 | Table 1 Characteristics of subjects with and without possible or probaple depression |
The logistic regression analysis determined the factors associated with possible depression, which included Extraversion, Agreeableness and Neuroticism (Table 2). In addition, the logistic regression analysis that included patients with probable depression revealed associations with smoking habits, alcohol consumption habits, Extraversion, Agreeableness and Neuroticism (Table 2). Multiple regression analysis indicated that BMI, smoking habits, alcohol consumption habits, marital status, Agreeableness and Neuroticism, but not Extraversion, were correlated with the severity of depression as measured by the total CES-D score (Table 3).
 | Table 2 Logistic regression results for factors associated with depression among T2DM patients |
 | Table 3 Simple and multiple regression results for factors associated with severity of depression among T2DM patients |
Discussion
The results of this study indicated that after adjustment for confounders, Agreeableness was inversely associated with depression, and Neuroticism was significantly associated with depression in logistic regression analyses and linear regression analysis. This study is the first to investigate the relationship between personality profile and depression in T2DM. These findings indicate that Agreeableness is a protective factor and that Neuroticism is a risk factor for depression in T2DM patients.
We sought to replicate and extend previous research showing that the personality traits of Neuroticism, Extraversion, and Conscientiousness moderate one another to predict depression (Table 2).29,30 Depression, however, was associated with Neuroticism and Agreeableness and possibly Extraversion, but not with Conscientiousness, although the scores for Conscientiousness differed between depressed and non-depressed patients with T2DM (Table 1) and the total score of CES-D was correlated with Extraversion or Conscientiousness only in the crude regression analysis (Table 3). These discrepancies in the associations of personality factors other than Neuroticism and Extraversion between our study and previous studies may be due to population differences between individuals with T2DM and the general population and to the use of different personality measurement tools, such as the NEO, FFM and TIPI-J, the correlations of which were significant but not perfect.28 In addition, we did not evaluate depression subtypes or symptom dimensions of depression, although a previous study reported that Agreeableness was negatively associated with the mood symptom dimension in late-life depression.31
In the present study, the prevalence of possible and probable untreated depression among individuals with T2DM were 29.9% and 15.6%, respectively. The prevalence of depression in our study was within the range of previous results (15–43%).32–36 Untreated depression is associated with a greater quantity and severity of physical and mental health comorbidities.37 Compared to the normal population in the same area, the prevalence of depression in the study population was high. Depression is frequently combined with sleep problems,36 anxiety,38 and cardiovascular disease39 and is often associated with risky health behaviors, such as poor diet, sedentariness and smoking, which can result in obesity and diabetes.40 Therefore, the early detection of potential depression in individuals with T2DM is clinically important.
This study has several notable limitations. First, the assessment of depressive symptoms was based on the CES-D rather than clinician-administered structured diagnostic interviews based on established criteria, such as the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV). The second limitation of this study was the recruitment strategy, which involved the recruitment of individuals with T2DM from the clinical setting of only one institute and excluded patients with severe mental illness, including major depressive disorders. These untreated individuals may not be representative of patients with clinical depression. The severity of depressive symptoms among our participants might be lower than that among clinical T2DM patients. Third, data for several potential confounding factors were not obtained because of strict ethical considerations and a reluctance to share medical information. This limitation is important because interpersonal relationships among family members and the severity of T2DM complications may have influenced the results of this study. Finally, this study is limited by its cross-sectional design; thus, we could not determine a causal relationship between personality and the onset of depressive symptoms among the patients in our study population. A follow-up survey is needed to investigate these associations.
Conclusion
Extraversion, Agreeableness and Neuroticism were significantly associated with depressive symptoms. These findings indicate that personality may affect depressive symptoms among individuals with T2DM. Furthermore, T2DM patients might benefit from psycho-educational interventions, such as supportive psychotherapy or cognitive behavior therapy, which are designed to help patients change their personalities when coping with the symptoms of their illness. Additional studies using a longitudinal study design are needed to examine the relationships between personality and depressive symptoms among T2DM patients.
Acknowledgments
This study was funded by a Grant-in-Aid for Scientific Research (KAKENHI) from the Japan Society for the Promotion of Research JSPS, 15H04754 (Principal Investigator Norio Yasui-Furukori) and 15K01643 (Principal Investigator Hiroshi Murakami). The funders had no role in the study design, data collection and analysis, the decision to publish, or the preparation of the manuscript.
Author contributions
Norio Yasui-Furukori, Hideyuki Otaka and Hiroshi Murakami designed the study and wrote the initial draft of the manuscript. Hirofumi Nakayama, Masaya Murabayashi, Satoru Mizushiri, Koki Matsumura, Jutaro Tanabe, Yuki Matsuhashi, and Miyuki Yanagimachi took samples and obtained patients’ informed consents. Kazuhiko Nakamura and Makoto Daimon contributed to analysis and interpretation of data, and Norio Sugawara assisted in the preparation of the manuscript. All other authors have contributed to data collection and interpretation, and critically reviewed the manuscript. All authors approved the final version of the manuscript and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Disclosure
Norio Yasui-Furukori has been a speaker for Dainippon-Sumitomo Pharmaceutical, Mochida Pharmaceutical, MSD and Otsuka Pharmaceutical. The authors report no other conflicts of interest in this work.
References
1. Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care. 2001;24:1069–1078.
2. Yu M, Zhang X, Lu F, Fang L. Depression and risk for diabetes: a meta-analysis. Can J Diabetes. 2015;39:266–272. doi:10.1016/j.jcjd.2014.11.006
3. Vancampfort D, Correll CU, Galling B, et al. Diabetes mellitus in people with schizophrenia, bipolar disorder and major depressive disorder: a systematic review and large scale meta-analysis. World Psychiatry. 2016;15:166–174. doi:10.1002/wps.20309
4. Alexopoulos GS, Meyers BS, Young RC, Campbell S, Silbersweig D, Charlson M. ‘Vascular depression’ hypothesis. Arch Gen Psychiatry. 1997;54:915–922.
5. Krishnan KR, Hays JC, Blazer DG. MRI-defined vascular depression. Am J Psychiatry. 1997;154:497–501. doi:10.1176/ajp.154.4.497
6. Sherwood A, Hinderliter AL, Watkins LL, Waugh RA, Blumenthal JA. Impaired endothelial function in coronary heart disease patients with depressive symptomatology. J Am Coll Cardiol. 2005;46:656–659. doi:10.1016/j.jacc.2005.05.041
7. Hemingway H, Shipley M, Mullen MJ, et al. Social and psychosocial influences on inflammatory markers and vascular function in civil servants (the Whitehall II study). Am J Cardiol. 2003;92:984–987.
8. Harris KF, Matthews KA, Sutton-Tyrrell K, Kuller LH. Associations between psychological traits and endothelial function in postmenopausal women. Psychosom Med. 2003;65:402–409.
9. Lesperance F, Frasure-Smith N, Theroux P, Irwin M. The association between major depression and levels of soluble intercellular adhesion molecule 1, interleukin-6, and C-reactive protein in patients with recent acute coronary syndromes. Am J Psychiatry. 2004;161:271–277. doi:10.1176/appi.ajp.161.2.271
10. Wang X, Bao W, Liu J, et al. Inflammatory markers and risk of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care. 2013;36:166–175. doi:10.2337/dc12-0702
11. Muris DM, Houben AJ, Schram MT, Stehouwer CD. Microvascular dysfunction is associated with a higher incidence of type 2 diabetes mellitus: a systematic review and meta-analysis. Arterioscler Thromb Vasc Biol. 2012;32:3082–3094. doi:10.1161/ATVBAHA.112.300291
12. Bot M, Pouwer F, de Jonge P, Tack CJ, Geelhoed-Duijvestijn PH, Snoek FJ. Differential associations between depressive symptoms and glycaemic control in outpatients with diabetes. Diabet Med. 2013;30:e115–e122. doi:10.1111/dme.12082
13. Gois C, Barbosa A, Ferro A, et al. The role of affective temperaments in metabolic control in patients with type 2 diabetes. J Affect Disord. 2011;134:52–58. doi:10.1016/j.jad.2011.05.021
14. Hall PA, Rodin GM, Vallis TM, Perkins BA. The consequences of anxious temperament for disease detection, self-management behavior, and quality of life in type 2 diabetes mellitus. J Psychosom Res. 2009;67:297–305. doi:10.1016/j.jpsychores.2009.05.015
15. Shamsi A, Khodaifar F, Arzaghi SM, Sarvghadi F, Ghazi A. Is there any relationship between medication compliance and affective temperaments in patients with type 2 diabetes? J Diabetes Metab Disord. 2014;13:96. doi:10.1186/s40200-014-0096-z
16. Gois C, Akiskal H, Akiskal K, Figueira ML. Depressive temperament, distress, psychological adjustment and depressive symptoms in type 2 diabetes. J Affect Disord. 2012;143:1–4. doi:10.1016/j.jad.2012.05.028
17. Gois C, Akiskal H, Akiskal K, Figueira ML. The relationship between temperament, diabetes and depression. J Affect Disord. 2012;142(Suppl):S67–S71. doi:10.1016/S0165-0327(12)70010-1
18. McCrae R, Costa PT
19. Kotov R, Gamez W, Schmidt F, Watson D. Linking “big” personality traits to anxiety, depressive, and substance use disorders: a meta-analysis. Psychol Bull. 2010;136:768–821. doi:10.1037/a0020327
20. Malouff JM, Thorsteinsson EB, Schutte NS. The relationship between the five factor model of personality and symptoms of clinic disorders: a meta-analysis. J Psychopathol Behav. 2005;27:101–114. doi:10.1007/s10862-005-5384-y
21. Hayward RD, Taylor WD, Smoski MJ, Steffens DC, Payne ME. Association of five-factor model personality domains and facets with presence, onset, and treatment outcomes of major depression in older adults. Am J Geriatr Psychiatry. 2013;21:88–96. doi:10.1016/j.jagp.2012.11.012
22. Koorevaar AML, Comijs HC, Dhondt ADF, van der Mast RC, Stek ML, Comijs HC. Big five personality and depression diagnosis, severity and age of onset in older adults. J Affect Disord. 2013;51:178–185. doi:10.1016/j.jad.2013.05.075
23. Weber K, Giannakopoulos P, Delaloye C, et al. Volumetric MRI changes, cognition and personality traits in old age depression. J Affect Disord. 2010;124:275–282. doi:10.1016/j.jad.2009.11.016
24. Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1997;1:385–401. doi:10.1177/014662167700100306
25. Zhang Y, Ting RZ, Lam MH, et al. Measuring depression with CES-D in Chinese patients with type 2 diabetes: the validity and its comparison to PHQ-9. BMC Psychiatry. 2015;15:198. doi:10.1186/s12888-015-0580-0
26. Sugawara N, Kaneda A, Takahashi I, Nakaji S, Yasui-Furukori N. Application of a stratum-specific likelihood ratio analysis in a screen for depression among a community-dwelling population in Japan. Neuropsychiatr Dis Treat. 2017;13:2369–2374. doi:10.2147/NDT.S142517
27. Gosling SD, Rentfrow PJ, Swann WB
28. Oshio A, Abe S, Cutrone P. Development, reliability, and validity of the Japanese version of Ten item personality inventory (TIPI-J). Jpn J Pers. 2012;21:40–52.
29. Dinovo SA, Vasey MW. Reactive and self-regulatory dimensions of temperament: interactive relations with symptoms of general distress and anhedonia. J Res Pers. 2011;45:430–440. doi:10.1016/j.jrp.2011.05.002
30. Vasey MW, Harbaugh CN, Lonigan CJ, et al. Dimensions of temperament and depressive symptoms: replicating a three-way interaction. J Res Pers. 2013;47:908–921. doi:10.1016/j.jrp.2013.09.001
31. Koorevaar AML, Hegeman JM, Lamers F, et al. Big five personality characteristics are associated with depression subtypes and symptom dimensions of depression in older adults. Int J Geriatr Psychiatry. 2017;32:e132–e140. doi:10.1002/gps.4670
32. Allen TA, Carey BE, McBride C, Bagby RM, DeYoung CG, Quilty LC. Big five aspects of personality interact to predict depression. J Pers. 2018;86(4):714–725.
33. Gavard JA, Lustman PJ, Clouse RE. Prevalence of depression in adults with diabetes. An epidemiological evaluation. Diabetes Care. 1993;16:1167–1178.
34. Stahl D, Sum CF, Lum SS, et al. Screening for depressive symptoms: validation of the center for epidemiologic studies depression scale (CES-D) in a multiethnic group of patients with diabetes in Singapore. Diabetes Care. 2008;31:1118–1119. doi:10.2337/dc07-2019
35. Roy T, Lloyd CE. Epidemiology of depression and diabetes: a systematic review. J Affect Disord. 2012;142(Suppl):S8–S21. doi:10.1016/S0165-0327(12)70004-6
36. Zhang P, Lou P, Chang G, et al. Combined effects of sleep quality and depression on quality of life in patients with type 2 diabetes. BMC Fam Pract. 2016;17:40. doi:10.1186/s12875-016-0435-x
37. Ghio L, Gotelli S, Cervetti A, et al. Duration of untreated depression influences clinical outcomes and disability. J Affect Disord. 2015;175:224–228. doi:10.1016/j.jad.2015.01.014
38. Tiller JW. Depression and anxiety. Med J Aust. 2013;199(6 Suppl):S28–S31.
39. Joynt KE, Whellan DJ, O‘Connor CM. Depression and cardiovascular disease: mechanisms of interaction. Biol Psychiatry. 2003;54:248–261.
40. Holt RI, de Groot M, Golden SH. Diabetes and depression. Curr Diab Rep. 2014;14:491. doi:10.1007/s11892-014-0475-3
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
