Back to Journals » Neuropsychiatric Disease and Treatment » Volume 19
Personal and Social Functioning and Health-Related Quality of Life in Patients with Schizophrenia Treated with the Long-Acting Injectable Antipsychotic Risperidone ISM
Authors Litman R, Naber D, Anta L , Martínez J , Filts Y , Correll CU
Received 15 November 2022
Accepted for publication 13 January 2023
Published 25 January 2023 Volume 2023:19 Pages 219—232
DOI https://doi.org/10.2147/NDT.S392351
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Robert Litman,1,2 Dieter Naber,3 Lourdes Anta,4 Javier Martínez,4 Yuriy Filts,5 Christoph U Correll6– 8
1CBH Health LLC, Gaithersburg, MD, USA; 2Department of Psychiatry, Georgetown University Medical School, Washington, DC, USA; 3Department of Psychiatry and Psychotherapy, Hamburg-Eppendorf University, Hamburg, Germany; 4Medical Department, Laboratorios Farmacéuticos ROVI, S.A., Madrid, Spain; 5Communal Noncommercial Enterprise of Lviv Regional Council, Lviv Regional Clinical Psychiatric Hospital, Lviv, Ukraine; 6Department of Psychiatry Research, The Zucker Hillside Hospital, Glen Oaks, NY, USA; 7Department of Psychiatry and Molecular Medicine, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Hempstead, NY, USA; 8Department of Child and Adolescent Psychiatry, Charité Universitätsmedizin Berlin, Berlin, Germany
Correspondence: Javier Martínez, Laboratorios Farmacéuticos ROVI, S.A., Calle Alfonso Gómez, 45A, Madrid, 28037, Spain, Tel +34 91 375 63 36, Fax +34 91 304 78 81, Email [email protected]
Objective: To analyze the effect of Risperidone ISM on social functioning and health-related quality of life (HR-QoL) in both short- and long-term treatment of patients with schizophrenia.
Patients and Methods: This analysis was based on data from both phases of the PRISMA-3 study, including 433 relapsed patients from the double-blind (DB) phase of the PRISMA-3 trial who were treated for 12-weeks with once-monthly (every 28 days) intramuscular Risperidone ISM 75 mg or 100 mg (n = 288), or placebo (n = 145), as well as 174 patients transitioning from the DB to an open-label 52-week extension (OLE) phase, plus 41 de novo patients treated on a stable maintenance dose of oral risperidone. The clinician-administered Personal and Social Performance (PSP) scale and the patient-reported 20-item Subjective Well-being under Neuroleptics scale (SWN-20) were used to measure social functioning and HR-QoL outcomes, respectively.
Results: Risperidone ISM significantly improved PSP total score from baseline to endpoint (Day 85) versus placebo in the DB phase with mean change total score (95% CI) of 10.7 (9; 12) compared to 4.8 (3; 7) for placebo (p < 0.0001). The statistically significant improvement was present from the first measurement time point (Day 29). SWN-20-measured HR-QoL increased on average in patients treated with Risperidone ISM in the DB phase. A significant improvement was also observed for PSP and SWN-20 scores from the OLE baseline to week 52 for patients transitioning from the DB phase. Stable de novo patients maintained similar PSP and SWN-20 scores during the whole OLE phase.
Conclusion: Risperidone ISM provided a rapid and sustained improvement in personal and social functioning, and HR-QOL without need of oral risperidone supplementation or loading doses. These findings, along with a fast onset of efficacy, could contribute to reinforcing the therapeutic alliance and possibly an earlier discharge. Moreover, patient functioning continued improving or was maintained with long-term treatment.
Keywords: risperidone, long-acting injectable, antipsychotics, schizophrenia, social functioning, quality of life
Introduction
Schizophrenia is a complex chronic disorder that is associated with significant disability and high personal and social costs.1 It is burdened by a high rate of comorbidities2,3 and a progressive decline in social functioning,1 which can lead to social isolation and poor health outcomes.4,5 The evaluation of health-related quality of life (HR-QoL) is relevant since the illness interacts with contextual factors (social and environmental), and since social functioning is considered an integral outcome parameter to evaluate the success of the treatment of schizophrenia.6 Hence, improving social functioning and HR-QoL in schizophrenia is a cornerstone for shifting toward a person-centered and recovery-oriented care.7 Minimizing schizophrenia symptomatology is crucial for achieving adequate functioning and satisfactory HR-QoL.8 Therefore, long-term treatment with antipsychotics is recommended by clinical practice guidelines, which also provides additional benefits, such as reducing the risk of relapse, rehospitalization and mortality.9–13 Antipsychotics are efficacious in improving symptoms in patients with acute schizophrenia,14 in preventing relapses,15,16 as well as in improving QoL and social functioning.17 Moreover, the treatment with long-acting injectable antipsychotics (LAIs) has been superior to oral antipsychotics for persistence of antipsychotic treatment, prevention of relapse and hospitalizations as well as other efficacy and functionality-related outcomes.18 Furthermore, use of LAIs in the earlier course of illness has been associated with preventing hospitalization or relapse, greater reduction of symptoms and improved functionality.19–22
Risperidone ISM is a new intramuscular (IM) LAI formulation of risperidone for monthly (every 28 days) administration without the need for using oral risperidone supplementation or loading doses, as opposed to recommendations for other LAIs.23–27 The specific technology used in this new formulation is based on an in situ forming of a solid polymeric matrix system that contains risperidone, which can explain, from a pharmacokinetic perspective, why therapeutic plasma concentration levels can be rapidly and smoothly achieved and maintained over the interval between administrations.28–30 The efficacy and safety of Risperidone ISM were demonstrated in the pivotal PRISMA-3 study, which consisted in a 12-week, randomized, double-blind (DB), placebo-controlled Phase 3 clinical trial31 followed by a 52-week open-label extension (OLE) phase.32
The aim of the present analysis was to assess the short- and long-term effects of Risperidone ISM on clinician-administered personal and social functioning and patient-reported subjective well-being, a major component of HR-QoL, in patients with schizophrenia.
Methods
This analysis was based on data from both phases of the PRISMA-3 study, ie, the DB (NCT03160521) and OLE (NCT03870880) phase, which was conducted at 26 centers in the United States and Ukraine between June 2017 and January 2020, in accordance with the Declaration of Helsinki, and Good Clinical Practice principles outlined in the International Conference on Harmonization. The protocol, amendments, and informed consent were approved by an Ethics Committee at each site, and written informed consent was obtained from all patients before study participation.
Full details of the study design, methods and eligibility criteria have been reported elsewhere.31,32 Briefly, participants were aged 18–65 years, with a diagnosis of schizophrenia, according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) criteria.33
The study was designed in two phases, a 12-week DB phase and a 52-week OLE phase. During the DB phase, patients with an acute exacerbation of schizophrenia (n = 438) were randomly assigned (1:1:1) to receiving 3 monthly intramuscular injections (every 28 days) of Risperidone ISM 75 mg (n = 145) or 100 mg (n = 146) or placebo (n = 147). Those patients who completed the DB phase according to the protocol were invited to enter an OLE phase along with other newly enrolled patients (de novo) to determine the efficacy, safety and tolerability of the long-term use of Risperidone ISM. Overall, 215 patients were included in the OLE phase and divided into three groups according to the following: stable patients (clinically stable – de novo – patients with a Positive and Negative Syndrome Scale [PANSS] total score of <70, a Clinical Global Impression-Severity [CGI-S] score of ≤3 [mild], without significant symptom exacerbation or hospitalizations due to relapses in the 3 months prior to OLE screening, and were previously treated with stable maintenance doses of oral risperidone 4–6 mg/day for at least the last 4 weeks; n = 41), unstable patients (rolled over from the placebo group of the DB phase: those who completed the DB phase of the PRISMA-3 study according to the protocol31 and had been receiving placebo in the DB phase and then Risperidone ISM at a dose of either 75 or 100 mg in the OLE phase; n = 55) and stabilized patients (rolled over from Risperidone ISM of the DB phase: patients treated with Risperidone ISM in the DB phase who continued to receive monthly Risperidone ISM in the OLE study at the same dose, 75 or 100 mg, as during the DB phase; n = 119).
Assessments
Social functioning was assessed by the clinician-administered Personal and Social Performance scale (PSP).34 The PSP is a 100-point single-item rating scale that is based on 4 areas: personal and social relationships; self-care; work and socially useful activities; and disturbing and aggressive behaviors.34 Each of the 4 domains is rated in 6 degrees of severity (absent, mild, manifest, marked, severe, very severe). Higher PSP scores indicate a better social functioning. The PSP was administered at several scheduled time points throughout the whole study duration (Supplementary Figure 1).
HR-QoL was assessed through the patient-reported 20-item Subjective Well-Being Under Neuroleptics Treatment (SWN-20) scale.35 The SWN-20 contains 5 different subscales: mental functioning, self-control, emotional regulation, physical functioning, social integration, with each subscale score ranging from 4 to 24, and with a total score range from 20 (poor) to 120 (excellent). To rate this scale, patients were asked to score identified well-being items as related to antipsychotic treatment on a 6-point scale from “Not at all” to “Very much”, with higher scores indicating better HR-QoL. This scale has been validated as a reliable measure for subjective well-being in patients with schizophrenia.36 The SWN-20 was also performed at several scheduled time points throughout the whole study duration (Supplementary Figure 1).
Baseline assessment of PSP and SWN-20 occurred before the administration of Risperidone ISM on acute study Day 1 (DB phase) or extension study Day 1 (OLE phase). For those patients who rolled over from the DB phase, PSP and SWN-20 total score at Day 85 of the DB phase were used as their baseline for the OLE phase. Both scales were administered at 4, 8 and 12 weeks after treatment initiation in the DB phase and at 12, 24 and 52 weeks after baseline of the OLE phase (Supplementary Figure 1).
Statistical Analysis
All statistical analyses were performed using SAS® statistical software version 9.3 or higher (SAS Institute, Inc., Cary, North Carolina).
The analysis in the DB phase was conducted on the intent-to-treat (ITT) population containing all randomized patients who had a baseline measurement, received ≥1 dose of study drug, and had ≥1 postbaseline evaluation of the PANSS.37 The analysis in the OLE phase was undertaken on the population of patients who received ≥1 dose of study drug during this phase. Two subgroups were used to analyze data from the DB phase, ie placebo vs pooled Risperidone ISM 75 mg and 100 mg,31 whereas data from the OLE phase were analyzed according to the three aforementioned subgroups (stable, unstable and stabilized patients) pooling also both Risperidone ISM dosages.32
At baseline, statistical difference between the treatment groups of the summary scores was estimated with a general linear model (GLM) with the summary score as dependent and treatment allocation as independent variables. The GLM has an identity or log link, and a normal distribution and gamma distribution were fitted. The best-fitting model parameterization was determined by the Akaike information criterion C statistic.38 In a second step, the values of these summary scores were summarized (means, 95% confidence interval [CI]) by treatment group over time. P-values for differences between treatment groups over time were estimated with a repeated measurement model, which took the inter-patient as well as the intra-patient correlation into account. A repeated measurement regression framework considered the repeated measures structure of the data and, if appropriate, additionally allowed regression coefficients to vary across specified subgroups.
Results
A total of 565 participants were screened and 438 were randomized in the DB phase but one of them withdrew consent before receiving the study treatment; therefore, 437 received the allocated intervention. Of them, 433 participants were included in the social functioning and HR-QoL analyses for the DB phase (4 patients did not have any postbaseline PANSS measurement). After completion of DB phase, 55 participants from the placebo group and 119 participants from the Risperidone ISM group rolled over into the OLE phase. Forty-one additional de novo stable patients were also enrolled to make up a total of 215 participants followed prospectively in the OLE phase and included in the OLE social functioning and HR-QoL analyses.
The baseline sociodemographic and clinical characteristics of patients are shown in Table 1. Patients from the DB phase had a mean age of 42 years, over two-thirds were male (67.2%), and black and white races were equally represented (49.4% vs 49.0%, respectively). In the OLE phase, most patients were male (60.9%) and white (84.7%) with a mean age of 39.3 years.
 |
Table 1 Patient Characteristics at Baseline in the Double Blind (DB) and Open-Label Extension (OLE) Phases |
Personal and Social Performance (PSP) Scores
At baseline of the DB phase, the mean PSP total score was 49.9 (95% CI = 49; 51) for the Risperidone ISM group, and 50.5 (95% CI = 49; 52) for the placebo group (Table 1). Throughout the DB phase, participants in the Risperidone ISM group consistently showed statistically significant greater improvements in the PSP total score than in the placebo group at every follow-up visit (Figure 1). This improvement was shown from the first measurement time point (Day 29) and at the end of the DB phase (Day 85), with the mean PSP total score for the Risperidone ISM group improving by 10.7 points compared to 4.8 points for the placebo group (p < 0.0001) (Supplementary Table 1).
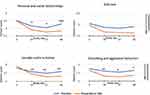
The Risperidone ISM group also showed significantly greater improvement (p < 0.05) than the placebo group in all domains of the PSP (except for “Self Care”) based on clinicians’ assessment (Figure 2). In addition, according to the severity classification for each PSP domain at the endpoint (Day 85) compared to baseline, a greater proportion of patients treated with Risperidone ISM showed a decrease in the “marked” and “severe” rating in two domains, “personal and social relationship” and “socially useful activities including work and study”. In addition, the proportion of patients with “absent” rating in “self-care” and “disturbing and aggressive behaviors” increased in the Risperidone ISM group compared with the placebo one (Supplementary Figure 2).
Over the 12-month OLE phase, the unstable and stabilized participants obtained further statistically significant improvement in the PSP total score at all time points (week 12, 24 and 52) from baseline (Figure 3), achieving a mean (95% CI) score of 66.9 (64; 70) and 68.2 (66; 70) at week 52, respectively, while stable patients maintained a steady PSP total score throughout the 12-month extension phase (Supplementary Table 2), obtaining a mean (95% CI) PSP total score of 73.31 (71; 76) at week 52. The unstable group also showed significant improvement at each time point from baseline in all domains of PSP (Figure 4).
Subjective Well-Being Under Neuroleptic Treatment (SWN-20) Scores
At baseline of the DB phase, mean SWN-20 total score was 80.3 (95% CI = 78; 83) for the placebo group, and 80.9 (95% CI = 79; 82) for the Risperidone ISM group (Table 1). Both Risperidone ISM and placebo groups increased the mean SWN-20 scores compared to baseline, with the mean (95% CI) change being slightly higher in the Risperidone ISM group than in the placebo group at the end of the DB phase (8.6 [7; 10] vs 5.6 [3; 8]; p = 0.0771) (Supplementary Table 3). Statistically significant differences versus placebo in mean change from baseline were observed at Day 29 (p = 0.0060) and Day 85 (p = 0.0357) for the “Social integration” domain, and at Day 85 (p = 0.0184) for the “Mental functioning” domain (Supplementary Table 3).
Over the 12-month OLE phase, a mean improvement from baseline to week 52 in the SWN-20 total score was observed for all 3 groups (unstable, stabilized and stable patients), with a mean (95% CI) change at 52 weeks in SWN-20 total score of 8.08 (4; 12), 4.16 (2; 7) and 1.94 (−1; 5) in the unstable, stabilized and stable patients, respectively, and reaching statistical significance in unstable and stabilized groups (Supplementary Table 4). The largest improvement was observed in the unstable patients in whom statistically significant improvements in SWN-20 total score were seen at all time points (week 12, 24 and 52) from baseline (Figure 5). Furthermore, stabilized and stable patients showed a mild improvement or maintained SWN-20 total score throughout the 12-month extension (Figure 5).
In addition, unstable patients showed an improvement in all SWN-20 domains compared to baseline, with statistically significant differences at all time points in “Social integration” and at two time points in “Mental functioning”, “Self-control” and “Physical functioning” (Supplementary Table 4). Furthermore, stabilized patients also showed statistically significant improvements from baseline at week 52 in “Physical functioning”, while stable patients maintained consistent SWN-20 total scores throughout the follow-up time (Supplementary Table 4).
Discussion
In this study, patients with schizophrenia who were treated with the long-acting injectable Risperidone ISM experienced a significant improvement in their level of functioning over time and showed a similar trend regarding HR-QoL, as measured through two widely used and validated scales, ie the PSP and SWN-20.34,35 The PSP has shown sufficient reliability and validity in different countries and settings for patients with schizophrenia,39–41 as well as substantial internal responsiveness (sensitivity to change) for in-patients with acute schizophrenia.42 In our study, the functional improvement was significantly greater for the Risperidone ISM group compared to placebo in the DB phase, which was observed as early as 4 weeks after starting the treatment and achieving a statistically and clinically significant43 10.7-point improvement from baseline to endpoint in the PSP score compared to placebo (with 4.8 points of improvement). Although indirect comparisons should be interpreted with caution due to potential heterogeneity of the study population and setting, the short-term results look better than those observed in two placebo-controlled 13-week studies of acutely patients with schizophrenia treated with another LAI (ie, monthly paliperidone palmitate), which evaluated a similar population with comparable PSP baseline values and showed improvements in the total PSP score of 4.2 and 4.8 points (for 50 mg eq and 100 mg eq, respectively) or 2.9, 6.1 and 8.3 points (for 25 mg eq, 100 mg eq and 150 mg eq, respectively), from baseline to endpoint.44,45
The individual domain data show what the PSP is measuring and what aspects of personal and social functioning are improving.46 Importantly, in our study results, three of the four PSP domains (personal and social relationships, social useful activities, and disturbing and aggressive behaviors) showed significant improvements with Risperidone ISM and were observed from week 4 post-treatment (the first follow-up time point) and beyond, which is important for the rapid treatment of aggressive behavioral symptoms and prevention of potential harm to the patient or others. Additionally, the persistence of aggressive behavior can prolong hospital stays and constitute an important barrier to appropriate community placement.47,48 Indeed, these domains are key components of the functioning of patients with schizophrenia,34 where progress in psychosocial functioning can contribute to personal, social, and occupational improvement and successful reintegration.4 In this sense, it has been reported that patients hospitalized with low function scores in PSP were less than half as likely to be discharged compared with those with the highest functioning (PSP 71 to 100), and, similarly, patients with high total PANSS scores were less than half as likely to be discharged at any time than the patients with the total PANSS scores <75.49 This finding suggests that enhancing social relationships and activities influences other improvements in clinical symptoms and facilitates hospital discharge and the return of the patient into their normal life.
Regarding the HR-QoL, SWN-20 total scores increased in both the placebo and Risperidone ISM groups, with a non-statistically significant trend of higher scores in the Risperidone ISM group. A period of 12 weeks could have been too short to produce definitive results about the possible effects of Risperidone ISM on HR-QoL, among others, because such parameters may require longer time to change.50 Nevertheless, statistically significant improvements in two relevant domains of the SWN-20 (mental functioning and social integration) were shown in the Risperidone ISM group, which may also indicate an improvement in patients’ quality of life, since SWN-20 scores appear to be correlated with objective evaluation of the psychopathology, quality of life, and mood control domains.35
We have already shown long-term efficacy of Risperidone ISM, which was observed in the OLE phase.32 The analysis of the 12-month OLE phase also provided the opportunity to further demonstrate long-term benefits of Risperidone ISM, particularly on domains of personal and social functioning and perception of well-being. Moreover, significant intra-group improvements, occurred at all time points in PSP and SWN-20 scores in the unstable rollover participants from the DB phase. For stabilized patients, significant intra-group improvements were observed at all time points in the PSP, and at end point (week 52) in the SWN-20.
Finally, the inclusion of de novo patients in the OLE phase allowed us to study the impact of Risperidone ISM on schizophrenia in patients who were clinically stable with oral risperidone at the time of entering the study. The maintenance of the same level of functioning and perception of well-being throughout the 12-months OLE phase highlights the value of Risperidone ISM administration as a simple and effective treatment option in case of switching from oral risperidone. Although the 12-month extension phase of the study was not designed to make comparisons among the groups differentiated based on level of stability at study baseline, and differences in baseline characteristics (eg, age, PANSS total score at baseline, time since diagnosis indicating greater illness severity/chronicity in the stabilized vs stable patient group) could have influenced the results, the mean 52-week [95% CI] PSP score in the stabilized patients (68.2 [66; 70]) was only slightly lower than the mean [95% CI] baseline PSP score in the stable patients (72.03 [70; 74]).
Antipsychotic medications, in particular LAI formulations, may improve rehabilitation and reentry into society of the patient, facilitating the ongoing relationship and therapeutic alliance that is essential for a reliable monitoring of the patient’s progress and compliance.51 Indeed, the therapeutic alliance and the patient’s level of functioning can significantly impact on their drug attitude since lower levels of positive and depressive symptoms, as well as a higher level of functioning have been associated with better drug attitudes.52 In contrast, nonadherence has been associated with poorer functional outcomes.53 Therefore, treatment with Risperidone ISM of patients with schizophrenia may also be an effective way to reinforce the therapeutic alliance between patient and clinician,54 resulting in improved adherence and acceptance of a LAI formulation55,56 that avoids the need of additional boosting injections or oral risperidone supplementation, thereby providing a rapid effect on positive and negative symptoms, as well as a meaningful impact on the functioning and HR-QoL outcomes.
However, the current findings need to be evaluated in the context of the study limitations. First, this was an analysis of secondary endpoints of the PRISMA-3 study, and therefore the results should be interpreted with caution. Nevertheless, this was a priori analysis, and pooling of the two Risperidone ISM arms increases the sample size and therefore the precision around estimates. Moreover, the analysis of primary and key secondary efficacy endpoints (PANSS total score and CGI-S score mean change from baseline to endpoint, respectively) also demonstrated superiority of Risperidone ISM over placebo.31 Second, as with other randomized, placebo-controlled clinical trials in schizophrenia, the placebo effect bias could have had an impact on the results.57 However, such a placebo effect would have created a conservative bias minimizing potential differences between Risperidone ISM and placebo. Third, higher adherence rates, which are common among patients enrolled in clinical trials, as well as the highly select clinical trial population, may be different from what is observed in real-world settings.58 Fourth, the 12-week trial only captured short-term results. Despite our positive results clearly showing statistically significant differences between Risperidone ISM and placebo in the PSP scores, it is possible that a 12-week treatment period may not be long enough to detect clinically meaningful differences in the SWN-20 total score.50 Therefore, our short-term HR-QoL results should be interpreted with caution. Finally, we did not assess patient- or clinician-reported treatment alliance in this study, outcomes that should be explored in future studies of rapidly acting LAIs.
Nevertheless, despite these limitations, this study with its positive outcomes on functioning and HR-QoL corroborates the value of Risperidone ISM, not only regarding its rapid onset of efficacy,31 but also as a long-term treatment that is able to reduce symptoms and relapses.32
Conclusion
In conclusion, the results from this study demonstrate that patients with a relapse of schizophrenia treated with the long-acting injectable antipsychotic Risperidone ISM experience a significant improvement in their level of functioning over time, as well as a positive change on HR-QoL. These findings, along with Risperidone ISM’s rapid onset of efficacy, combined with the lack of the need for loading doses or oral supplementations to rapidly achieve plasma therapeutic levels, can contribute to reinforce the therapeutic alliance and provide earlier hospital discharge. Finally, positive findings with the long-term treatment with Risperidone ISM provide further evidence that functioning continues to improve in unstable and stabilized patients and is maintained in stable patients previously treated with oral risperidone. Taken together, these data reinforce that Risperidone ISM can be a valuable treatment for the acute and maintenance management of patients with schizophrenia.
Data Sharing Statement
Any Risperidone ISM’s data besides what is included in the manuscript may not be available for research reason. Data supporting the results of this study are available from ROVI, but restrictions apply to the availability of them, which were used under license for the present study and are therefore not publicly available. However, the data may be provided by authors upon reasonable request and with the permission of ROVI.
Ethics Approval and Informed Consent
The Ethics approval and the informed consent form were approved by Ethics Committee for each site in Ukraine:
Ethics Committee of Kyiv City
Psychoneurological Hospital No. 2
vul. Myropilska, 8
Kyiv, 02192
Ukraine
Ethics Committee of Communal Institution of Lviv Regional Council
Lviv Regional Clinical Psychiatric Hospital
vul. Kulparkivska, 95
Lviv, 79021
Ukraine
Ethics Committee of Communal Non-profit Enterprise of Kharkiv Regional Council
Regional Clinical Psychiatric Hospital #3
vul. Ac. Pavlova 46
Kharkiv, 61068
Ukraine
Ethics Committee of Communal Non-profit Enterprise of Kharkiv Regional Council
Regional Clinical Psychiatric Hospital #3
vul. Ac. Pavlova 46
Kharkiv, 61068
Ukraine
Ethics Committee of Communal Establishment
Kherson Regional Psychiatric Hospital of Kherson Regional Council
vul Dzhona Hovarda 65
Stepanivka village
Kherson, 73488
Ukraine
Ethics Committee of Communal Establishment
Acad. O.I. Iushchenko Vinnytsia Regional Psychoneurological Hospital
vul. Pyrohova, 109
Vinnytsia, 21005
Ukraine
Ethics Committee of Communal Enterprise
Poltava Regional Clinical Psychiatric Hospital named after O. F. Maltsev of Poltava Regional Council
vul. Medychna 1
Poltava, 36013
Ukraine
Ethics Committee of Communal Non-profit Enterprise
Odesa Regional Medical Centre of Mental Health
Odesa Regional Council
9, Vorobyova Street
Odesa, 65006
Ukraine
Ethics Committee of Kyiv Regional Medical Association
Psykhiatriya in Kyiv
103, Kyrylivska street
Kyiv, 04080
Ukraine
Ethics Committee of Communal Institution
Dnipropetrovsk Regional Clinical Hospital named after I.I., ploshcha Soborna, 14
Dnipro, 49005
Ukraine
Ethics Committee of Communal Institution of Lviv Regional Council
Lviv Regional Clinical Psychiatric Hospital
vul. Kulparkivska, 95
Lviv, 79021
Ukraine
The Ethics approval and the informed consent form were approved in US by the Copernicus Group Independent Review Board on behalf of each participant site: Copernicus Group Independent Review Board 5000 Centre, Green Way, Suite 200 Cary, North Carolina, 27513, United States of America.
Acknowledgments
The authors would like to acknowledge to Jordi Llaudó, Begoña Gorostidi, Laura Vallejo, Ibon Gutierro, Ignacio Ayani, Ana Belén López-Yélamos and Mateo Fernández-Varela for their contribution to the study. All of them are employees of Laboratorios Farmacéuticos ROVI, S.A. The authors also thank the study participants, their families and caregivers, and the investigators for their participation.
Author Contributions
Robert Litman was involved in the design and interpretation, as well as in the recruitment of the patients; Dieter Naber was involved in the data analysis; Lourdes Anta was involved in the data analysis, interpretation as well as in the manuscript development; Javier Martínez was involved in the data analysis, in the design and interpretation, as well as in the manuscript development; Yuriy Filts was involved in the design and interpretation, as well as in the recruitment of the patients; Christoph U. Correll was involved in the data analysis, interpretation as well as in the manuscript development. All the authors have made substantial contributions, took part in revising or critically reviewing the article; agreed to submit to the current journal; gave final approval of the version to be published; and agreed to be accountable for all aspects of the work.
Funding
This study was funded by Laboratorios Farmacéuticos Rovi, S.A. Madrid, Spain. It was supported also in part by Centro para el Desarrollo Tecnológico Industrial (Expedient No. IDI-20160109).
Disclosure
Robert Litman, is a Member, Speakers Bureau, for JNJ and for Allergan, Member, Scientific Advisory Board, Terran BioSciences. He participated as Investigator Coordinator in The United States of America and as Principal Investigator in the study PRISMA-3. Dieter Naber, has received consulting fees from Laboratorios Farmacéuticos Rovi, S.A. He served on the Data Monitoring Committee for Rovi at the present study. Lourdes Anta and Javier Martínez are employees of Laboratorios Farmacéuticos Rovi, S.A., the sole developer of Risperidone ISM. Yuriy Filts has participated as Investigator Coordinator in Ukraine and Principal Investigator in the study PRISMA-3. He also received fees from ROVI for his advice in some previous tasks related to PRISMA-3 study. Dr Yuriy Filts also reports personal fees from Suvion, Otsuka, Arkermes, ROVI, Intracellular Therapies, Janssen, Minerva Neurosciences, Gedeon Richter as principal investigator in clinical study, outside the submitted work. He also received fees for lecturing from Laboratorios Farmacéuticos Rovi, S.A., and Lundbeck. Christoph U. Correll, has been a consultant and/or advisor to or have received honoraria from: AbbVie, Acadia, Alkermes, Allergan, Angelini, Aristo, Boehringer-Ingelheim, Cardio Diagnostics, Cerevel, CNX Therapeutics, Compass Pathways, Darnitsa, Gedeon Richter, Hikma, Holmusk, IntraCellular Therapies, Janssen/J&J, Karuna, LB Pharma, Lundbeck, MedAvante-ProPhase, MedInCell, Merck, Mindpax, Mitsubishi Tanabe Pharma, Mylan, Neurocrine, Newron, Noven, Otsuka, Pharmabrain, PPD Biotech, Recordati, Relmada, Reviva, Rovi, Seqirus, SK Life Science, Sunovion, Sun Pharma, Supernus, Takeda, Teva, and Viatris. He provided expert testimony for Janssen and Otsuka. He served on a Data Safety Monitoring Board for Lundbeck, Relmada, Reviva, Rovi, Supernus, and Teva. He has received grant support from Janssen and Takeda. He received royalties from UpToDate and is also a stock option holder of Cardio Diagnostics, Mindpax, LB Pharma and Quantic. The authors report no other conflicts of interest in this work.
References
1. Kahn RS, Sommer IE, Murray RM, et al. Schizophrenia. Nat Rev Dis Primers. 2015;1:15067.
2. Charlson FJ, Ferrari AJ, Santomauro DF, et al. Global epidemiology and burden of schizophrenia: findings from the global burden of disease study 2016. Schizophr Bull. 2018;44(6):1195–1203. doi:10.1093/schbul/sby058
3. Laursen TM, Nordentoft M, Mortensen PB. Excess early mortality in schizophrenia. Annu Rev Clin Psychol. 2014;10:425–448. doi:10.1146/annurev-clinpsy-032813-153657
4. Bellack AS, Green MF, Cook JA, et al. Assessment of community functioning in people with schizophrenia and other severe mental illnesses: a white paper based on an NIMH-sponsored workshop. Schizophr Bull. 2007;33(3):805–822. doi:10.1093/schbul/sbl035
5. Correll CU, Stanford AD, Claxton A, Du Y, Weiden PJ. Social and functional outcomes with two doses of aripiprazole lauroxil vs placebo in patients with schizophrenia: a post-hoc analysis of a 12-week phase 3 efficacy study. Psychiatry Res. 2019;274:176–181. doi:10.1016/j.psychres.2019.02.021
6. Peters-Strickland T, Baker RA, Such P, Zhang P, Madera JJ. The effect of aripiprazole once-monthly on personal and social functioning: post hoc analyses of acute and long-term studies. Neuropsychiatr Dis Treat. 2019;15:1659–1669. doi:10.2147/NDT.S198241
7. Harvey P, Bellack AS. Toward a terminology for functional recovery in schizophrenia: is functional remission a viable concept? Schizophr Bull. 2009;35(2):300–306. doi:10.1093/schbul/sbn171
8. Lambert M, Naber D, Schacht A, et al. Rates and predictors of remission and recovery during 3 years in 392 never-treated patients with schizophrenia. Acta Psychiatr Scand. 2008;118(3):220–229. doi:10.1111/j.1600-0447.2008.01213.x
9. The American Psychiatric Association (APA). Practice Guideline for the Treatment of Patients with Schizophrenia. The American Psychiatric Association (APA); 2019.
10. National Institute for Health and Care Excellence (NICE). Psychosis and Schizophrenia in Adults: Prevention and Management. National Institute for Health and Care Excellence (NICE); 2014.
11. Correll CU, Martin A, Patel C, et al. Systematic literature review of schizophrenia clinical practice guidelines on acute and maintenance management with antipsychotics. Schizophrenia. 2022;8(1):5. doi:10.1038/s41537-021-00192-x
12. Solmi M, Correll CU. The antipsychotic paradox: lessons regarding determinants of premature mortality. Eur Neuropsychopharmacol. 2022;62:1–3. doi:10.1016/j.euroneuro.2022.05.014
13. Correll CU, Solmi M, Croatto G, et al. Mortality in people with schizophrenia: a systematic review and meta-analysis of relative risk and aggravating or attenuating factors. World Psychiatry. 2022;21(2):248–271. doi:10.1002/wps.20994
14. Huhn M, Nikolakopoulou A, Schneider-Thoma J, et al. Comparative efficacy and tolerability of 32 oral antipsychotics for the acute treatment of adults with multi-episode schizophrenia: a systematic review and network meta-analysis. Lancet. 2019;394(10202):939–951. doi:10.1016/S0140-6736(19)31135-3
15. Schneider-Thoma J, Chalkou K, Dörries C, et al. Comparative efficacy and tolerability of 32 oral and long-acting injectable antipsychotics for the maintenance treatment of adults with schizophrenia: a systematic review and network meta-analysis. Lancet. 2022;399(10327):824–836. doi:10.1016/S0140-6736(21)01997-8
16. Ostuzzi G, Bertolini F, Tedeschi F, et al. Oral and long-acting antipsychotics for relapse prevention in schizophrenia-spectrum disorders: a network meta-analysis of 92 randomized trials including 22,645 participants. World Psychiatry. 2022;21(2):295–307. doi:10.1002/wps.20972
17. Leucht S, Leucht C, Huhn M, et al. Sixty years of placebo-controlled antipsychotic drug trials in acute schizophrenia: systematic review, Bayesian meta-analysis, and meta-regression of efficacy predictors. Am J Psychiatry. 2017;174(10):927–942. doi:10.1176/appi.ajp.2017.16121358
18. Kishimoto T, Hagi K, Kurokawa S, Kane JM, Correll CU. Long-acting injectable versus oral antipsychotics for the maintenance treatment of schizophrenia: a systematic review and comparative meta-analysis of randomised, cohort, and pre-post studies. Lancet Psychiatry. 2021;8:387–404. doi:10.1016/S2215-0366(21)00039-0
19. Rubio JM, Taipale H, Tanskanen A, Correll CU, Kane JM, Tiihonen J. Long-term continuity of antipsychotic treatment for schizophrenia: a nationwide study. Schizophr Bull. 2021;47(6):1611–1620. doi:10.1093/schbul/sbab063
20. Hargarter L, Bergmans P, Cherubin P, et al. Once-monthly paliperidone palmitate in recently diagnosed and chronic non-acute patients with schizophrenia. Expert Opin Pharmacother. 2016;17(8):1043–1053. doi:10.1080/14656566.2016.1174692
21. Brown B, Turkoz I, Mancevski B, Mathews M. Evaluation of paliperidone palmitate long-acting injectable antipsychotic therapy as an early treatment option in patients with schizophrenia. Early Interv Psychiatry. 2020;14(4):428–438. doi:10.1111/eip.12868
22. Kim S, Kim S, Koh M, et al. Effects of long-acting injectable paliperidone palmitate on clinical and functional outcomes in patients with schizophrenia based on illness duration. J Clin Psychiatry. 2021;82(1):20m13446. doi:10.4088/JCP.20m13446
23. Risperdal Consta® (risperidone) US [package insert]. Beerse, BE: Janssen pharmaceuticals Inc; 2003. Available from: https://wwwaccessdata.fda.gov/drugsatfda_docs/label/2010/021346_s31_s35_s38_s39lbl.pdf.
24. Abilify Maintena® (aripiprazole) US [package insert]. Chiyoda, JP: Otsuka Pharmaceutical Co; 2002. Available from: https://wwwaccessdata.fda.gov/drugsatfda_docs/label/2016/202971s008lbl.pdf.
25. Aristada® (aripiprazole lauroxil) [US package insert]. Dublin, IR: Alkermes; 2015. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/207533s000lbl.pdf.
26. Invega Sustena® (paliperidone) US [package insert]. Beerse, BE: Janssen pharmaceuticals Inc; 2006. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/022264s023lbl.pdf.
27. Correll CU, Citrome L, Haddad PM, et al. The use of long-acting injectable antipsychotics in schizophrenia: evaluating the evidence. J Clin Psychiatry. 2016;77(suppl 3):1–24. doi:10.4088/JCP.15032su1
28. Anta L, Llaudó J, Ayani I, Martínez J, Litman RE, Gutierro I. A Phase II study to evaluate the pharmacokinetics, safety, and tolerability of Risperidone ISM multiple intramuscular injections once every 4 weeks in patients with schizophrenia. Int Clin Psychopharmacol. 2018;33(2):79–87. doi:10.1097/YIC.0000000000000203
29. Llaudó J, Anta L, Ayani I, et al. Phase I, open-label, randomized, parallel study to evaluate the pharmacokinetics, safety, and tolerability of one intramuscular injection of risperidone ISM at different dose strengths in patients with schizophrenia or schizoaffective disorder (PRISMA-1). Int Clin Psychopharmacol. 2016;31(6):323–331. doi:10.1097/YIC.0000000000000139
30. Walling DP, Hassman HA, Anta L, et al. The steady-state comparative bioavailability of intramuscular Risperidone ISM and oral risperidone: an open-label, one-sequence study. Drug Des Devel Ther. 2021;15:4371–4382. doi:10.2147/DDDT.S332026
31. Correll CU, Litman RE, Filts Y, et al. Efficacy and safety of once-monthly Risperidone ISM® in schizophrenic patients with an acute exacerbation. NPJ Schizophr. 2020;6(1):37. doi:10.1038/s41537-020-00127-y
32. Filts Y, Litman RE, Martínez J, Anta L, Naber D, Correll CU. Long-term efficacy and safety of once-monthly Risperidone ISM® in the treatment of schizophrenia: results from a 12-month open-label extension study. Schizophr Res. 2022;239:83–91. doi:10.1016/j.schres.2021.11.030
33. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders.
34. Morosini PL, Magliano L, Brambilla L, Ugolini S, Pioli R. Development, reliability and acceptability of a new version of the DSM-IV Social and Occupational Functioning Scale (SOFAS) to assess routine social functioning. Acta Psychiatr Scand. 2000;101(4):323–329. doi:10.1034/j.1600-0447.2000.101004323.x
35. Naber D, Moritz S, Lambert M, et al. Improvement of schizophrenic patients’ subjective well-being under atypical antipsychotic drugs. Schizophr Res. 2001;50(1–2):79–88. doi:10.1016/S0920-9964(00)00166-3
36. Vothknecht S, Meijer C, Zwinderman A, et al; for Genetic Risk and Outcome of Psychosis (GROUP). Psychometric evaluation of the Subjective Well-being Under Neuroleptic Treatment Scale (SWN) in patients with schizophrenia, their relatives and controls. Psychiatry Res. 2013;206(1):62–67. doi:10.1016/j.psychres.2012.09.004
37. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261–276. doi:10.1093/schbul/13.2.261
38. Akaike H. Information theory and an extension of the maximum likelihood principle. In: Petrov B, Csáki F, editors. Second International Symposium on Information Theory. Budapest: Akadémiai Kiadó; 1998:199–213.
39. Brissos S, Palhava F, Marques JG, et al. The Portuguese version of the Personal and Social Performance Scale (PSP): reliability, validity, and relationship with cognitive measures in hospitalized and community schizophrenia patients. Soc Psychiatry Psychiatr Epidemiol. 2012;47(7):1077–1086. doi:10.1007/s00127-011-0412-6
40. Garcia-Portilla MP, Saiz PA, Bousoño M, Bascaran MT, Guzmán-Quilo C, Bobes J. Validation of the Spanish Personal and Social Performance scale (PSP) in outpatients with stable and unstable schizophrenia. Rev Psiquiatr Salud Ment. 2011;4(1):9–18. doi:10.1016/j.rpsm.2010.11.003
41. Kawata AK, Revicki DA. Psychometric properties of the Personal and Social Performance scale (PSP) among individuals with schizophrenia living in the community. Qual Life Res. 2008;17(10):1247–1256. doi:10.1007/s11136-008-9400-z
42. Chiu EC, Hung TM, Huang CM, Lee SC, Hsieh CL. Responsiveness of the Personal and Social Performance scale in patients with schizophrenia. Psychiatry Res. 2018;260:338–342. doi:10.1016/j.psychres.2017.11.053
43. Nicholl D, Nasrallah H, Nuamah I, Akhras K, Gagnon D, Gopal S. Personal and social functioning in schizophrenia: defining a clinically meaningful measure of maintenance in relapse prevention. Curr Med Res Opin. 2010;26(6):1471–1484. doi:10.1185/03007991003798927
44. Gopal S, Hough DW, Xu H, et al. Efficacy and safety of paliperidone palmitate in adult patients with acutely symptomatic schizophrenia: a randomized, double-blind, placebo-controlled, dose-response study. Int Clin Psychopharmacol. 2010;25(5):247–256. doi:10.1097/YIC.0b013e32833948fa
45. Pandina G, Lindenmayer JP, Lull J, et al. A randomized, placebo-controlled study to assess the efficacy and safety of 3 doses of paliperidone palmitate in adults with acutely exacerbated schizophrenia. J Clin Psychopharmacol. 2010;30(3):235–244. doi:10.1097/JCP.0b013e3181dd3103
46. Fleischhacker WW, Baker RA, Eramo A, et al. Effects of aripiprazole once-monthly on domains of personal and social performance: results from 2 multicenter, randomized, double-blind studies. Schizophr Res. 2014;159(2–3):415–420. doi:10.1016/j.schres.2014.09.019
47. Bigelow DA, Cutler DL, Moore LJ, McComb P, Leung P. Characteristics of state hospital patients who are hard to place. Hosp Community Psychiatry. 1988;39:181–185. doi:10.1176/ps.39.2.181
48. Greenfield TK, McNiel DE, Binder RL. Violent behavior and length of psychiatric hospitalization. Hosp Community Psychiatry. 1989;40:809–814. doi:10.1176/ps.40.8.809
49. Kozma CM, Dirani RG, Canuso CM, Mao L. Predicting hospital admission and discharge with symptom or function scores in patients with schizophrenia: pooled analysis of a clinical trial extension. Ann Gen Psychiatry. 2010;9:24. doi:10.1186/1744-859X-9-24
50. Montemagni C, Frieri T, Rocca P. Second-generation long-acting injectable antipsychotics in schizophrenia: patient functioning and quality of life. Neuropsychiatr Dis Treat. 2016;12:917–929. doi:10.2147/NDT.S88632
51. Bozzatello P, Bellino S, Mancini I, Sandei L, Zanalda E, Rocca P. Effects on satisfaction and service engagement of paliperidone palmitate compared with oral paliperidone in patients with schizophrenia: an open label randomized controlled trial. Clin Drug Investig. 2019;39(2):169–178. doi:10.1007/s40261-018-0734-1
52. Lim M, Li Z, Xie H, Tan BL, Lee J. The effect of therapeutic alliance on attitudes toward psychiatric medications in schizophrenia. J Clin Psychopharmacol. 2021;41(5):551–560. doi:10.1097/JCP.0000000000001449
53. Ascher-Svanum H, Faries DE, Zhu B, Ernst FR, Swartz MS, Swanson JW. Medication adherence and long-term functional outcomes in the treatment of schizophrenia in usual care. J Clin Psychiatry. 2006;67(3):453–460. doi:10.4088/JCP.v67n0317
54. Álamo C. Risperidone ISM as a new option in the clinical management of schizophrenia: a narrative review. Adv Ther. 2022;39(11):4875–4891. doi:10.1007/s12325-022-02299-8
55. Citrome L, Belcher E, Stacy S, Suett M, Mychaskiw M, Salinas GD. Management of schizophrenia with long-acting injectable antipsychotic medications: an assessment of the educational needs of clinicians. Neuropsychiatr Dis Treat. 2022;18:111–123. doi:10.2147/NDT.S326299
56. Potkin S, Bera R, Zubek D, Lau G. Patient and prescriber perspectives on long-acting injectable (LAI) antipsychotics and analysis of in-office discussion regarding LAI treatment for schizophrenia. BMC Psychiatry. 2013;13:261. doi:10.1186/1471-244X-13-261
57. Kubo K, Fleischhacker W, Suzuki T, Yasui-Furukori N, Mimura M, Uchida H. Placebo effects in adult and adolescent patients with schizophrenia: combined analysis of nine RCTs. Acta Psychiatr Scand. 2019;139:108–116. doi:10.1111/acps.12960
58. Kane JM, Kishimoto T, Correll CU. Assessing the comparative effectiveness of long-acting injectable versus oral antipsychotic medications in the prevention of relapse provides a case study in comparative effectiveness research in psychiatry. J Clin Epidemiol. 2013;66(8 Suppl):S37–S41. doi:10.1016/j.jclinepi.2013.01.012
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.