Back to Journals » Patient Preference and Adherence » Volume 10
Persistence and compliance with newly initiated antihypertensive drug treatment in patients with chronic kidney disease
Authors Truong VT, Moisan J, Kröger E, Langlois S, Gregoire J
Received 18 March 2016
Accepted for publication 29 April 2016
Published 21 June 2016 Volume 2016:10 Pages 1121—1129
DOI https://doi.org/10.2147/PPA.S108757
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Viet Thanh Truong,1,2 Jocelyne Moisan,1,2 Edeltraut Kröger,1–3 Serge Langlois,4 Jean-Pierre Grégoire1,2
1Faculty of Pharmacy, Laval University, 2Chair on Adherence to Treatments, Population Health and Optimal Practices in Health Research Unit, CHU de Québec Research Center, 3Center of Excellence on Aging of Québec, 4Faculty of Medicine, Laval University, Quebec, Canada
Background: Patients with chronic kidney disease initiating an antihypertensive drug (AH) treatment must persist and comply with it to slow disease progression and benefit from the reduction of cardiovascular morbidity and mortality.
Objectives: This study evaluates the persistence and compliance with AH treatment and identifies the associated factors among chronic kidney disease patients who initiated AH treatment.
Methods: A population-based cohort study using Quebec administrative data was conducted. Patients who still take any AH 1 year after initiation were considered persistent. Of these patients, those who had ≥80% of days covered with an AH in the year after initiation were considered compliant. Factors associated with persistence and compliance were identified using a modified Poisson regression.
Results: Of the 7,119 eligible patients, 78.8% were persistent, 87.7% of whom were compliant with their AH treatment. Compared with patients on diuretic monotherapy, those who initially used angiotensin-converting enzyme inhibitor monotherapy, angiotensin II receptor blocker monotherapy, calcium channel blocker monotherapy, β-blocker monotherapy, or multidrug therapy were more likely to be persistent. In contrast, individuals who visited their physicians ≥17 times were less likely to be persistent than those who visited between 0 and 8 times. The patients who were more likely to be compliant had initially used an angiotensin-converting enzyme inhibitor, β-blocker, calcium channel blocker, or multitherapy as opposed to a diuretic.
Conclusion: A year after initiating AH treatment, nearly a third of chronic kidney disease patients were either not taking an AH or had not been compliant. Factors associated with persistence and compliance could help identify patients who need help in managing their AH treatment.
Keywords: chronic kidney disease, adherence, factors, antihypertensive drug
Introduction
Chronic kidney disease (CKD) is a group of disorders that affect structure and function of kidney.1 As CKD progresses, the risk of cardiovascular disease increases.2 CKD patients who suffer from high blood pressure require antihypertensive drug (AH) treatment to reduce their risk of high blood pressure-related cardiovascular complications, such as stroke, coronary artery disease, and heart failure.1,3 To fully benefit from AH treatment, patients must adhere to it. Good adherence to AH treatment has been associated with a lower risk of acute cardiovascular events,4 a reduction in the risk of chronic heart failure events5 and end-stage renal disease,5,6 and with lower health care costs.7
For patients who initiate a drug treatment, adherence to treatment is composed of two main constructs: persistence and compliance.8 Patients are persistent with their drug treatment if they take it for the recommended duration.9 In addition to persisting with the treatment, patients also need to comply, that is, take the medication as recommended in terms of dosage and schedule.
To our knowledge, persistence with AH treatment among individuals suffering from CKD in clinical practice has never been assessed. However, four studies have assessed the compliance with AH treatment in CKD patients.10–13 The results of the first study10 are difficult to interpret because compliance was measured by pill counts, a measure that lacks validity.14 In addition, the results cannot be extrapolated to the general population of CKD patients, because it was conducted under the specific conditions of a clinical trial in which the patients received counseling based on their pill count results. The three other studies11–13 were observational with a cross-sectional design and therefore included only patients who were current AH users at the time when those studies were conducted. The results are therefore difficult to interpret, as current users typically do not include patients who have discontinued their treatment early. The factors associated with AH compliance were assessed in two11,13 of those studies. Because the studies had a cross-sectional design, the temporal relationship between the associated factors and compliance cannot be determined. Consequently, little is known about the factors associated with persistence and compliance with AH treatment among individuals suffering from CKD.
A study of Quebecers aged ≥18 years with CKD who were new users of AH drugs was conducted. The objectives were to estimate the proportion of patients persistent with AH treatment 1 year after treatment initiation and the proportion of the persistent patients who were compliant with AH treatment in the year following treatment initiation and identify the factors associated with persistence and compliance.
Methods
Data sources
We conducted a population-based cohort study using data from the Quebec Health Insurance Board (RAMQ), the Quebec registry of hospitalizations, and the Quebec Institute of Statistics. All Quebec permanent residents are covered by RAMQ for both medical services and hospitalizations. Regarding drug reimbursement, the RAMQ public drug plan covers 97% of individuals aged ≥65 years, 100% of those who receive guaranteed income supplement (GIS) and those who are not covered by a private drug insurance group plan.
The RAMQ databases provide information on the following demographic characteristics: socioeconomic status, outpatient medical services (diagnostic code for the main diagnosis, date of diagnosis, and physician specialty) and use of drugs (drug’s identity, date of drug claim, quantity, number of days’ supply, and prescriber’s specialty). RAMQ data on the prescribed drugs are accurate.15 The hospitalization registry provides information on hospitalizations, including admission date, duration of stay, and principal and secondary diagnoses. The Institute of Statistics database provides the exact date of death and the first and secondary causes of death.
Study population
The RAMQ provided us with data on all individuals aged ≥18 years who were beneficiaries of RAMQ and had their first CKD diagnosis between January 1, 2000, and December 31, 2011, inclusively. Individuals were considered to have CKD if they had ≥1 CKD diagnosis unless the recorded diagnosis was made in a hospital. If the first recorded CKD diagnosis was in an outpatient setting, it had to be followed within a year by a second recorded diagnosis from either source. This definition of a CKD case maximizes specificity.16 To ensure that only individuals who were newly diagnosed with CKD (waiting period of 365 days) were included, we excluded patients who were not continuously eligible for RAMQ in the 365 days prior to the date of CKD diagnosis.
From this initial study population, we identified a cohort of new AH users. Individuals with a claim for any AH (Anatomical Therapeutic Chemical Classification System code: C02, C03, C07, C08, C09A, C09B, C09D, C09X) in the year before their CKD diagnosis were excluded. Of the remaining eligible individuals, those with a claim for any AH on the day of their CKD diagnosis or after were included. To ensure that there were complete data for all patients for 365 days following treatment initiation, individuals who had a follow-up period of less than 365 days or who were not eligible for the RAMQ drug plan in the 365-day period before and after the date of AH treatment initiation were also excluded.
Variables
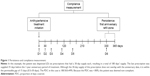
Persistence and compliance were assessed using RAMQ prescription claim data. Persistence was defined as filling out at least one prescription for any AH within a period of the 1-year anniversary of treatment initiation (Figure 1). A prescription was considered filled in the anniversary period if, at the most recent refill prior to the 1-year anniversary, the individual was supplied with enough days of medication to reach the 1-year anniversary date. A permissible gap of 0.5 times the days’ supply was allowed. We assessed compliance with AH among the patients who were persistent with AH treatment using the proportion of days covered (PDC). The PDC was calculated by dividing the number of days covered by at least one AH during the year after treatment initiation by 365 days. As information about the in-hospital use of drugs was not captured in the hospitalization registry, the number of days hospitalized was removed from both the numerator and the denominator. Patients were considered to be compliant if they had a PDC ≥80%.
In addition to the initial AH treatment modalities, we examined an array of variables that were potentially associated with AH treatment persistence and compliance. The following variables were assessed on the date of CKD diagnosis: age (categorized by quintiles), sex, and socioeconomic status (low = maximum GIS or welfare, medium = partial GIS, and high = no GIS).
The following variables were determined for the year prior to the initiation of AH treatment: number of physician visits (categorized by tertiles), previous hospitalization, time from the diagnosis of CKD to initial AH treatment (days, categorized by quintiles), number of distinct drugs as a measure of comorbidity (categorized by tertiles), and comorbidities of CKD including diabetes, dyslipidemia, stroke, coronary disease, and anemia. We also determined the specialty of the physicians who prescribed the initial AH treatment (general practitioner, nephrologist, internist, or other).
Statistical analysis
Patient characteristics were assessed using descriptive statistics. We calculated the proportion of patients who persisted with any AH 1 year after treatment initiation and the proportion of the patients who persisted who were also compliant.
We identified factors that were potentially associated with persistence and compliance using a multivariate modified Poisson regression model. This method enables the calculation of prevalence ratios when the prevalence is >5%.17 We calculated adjusted prevalence ratios with 95% confidence intervals.
The sensitivity of our results regarding the factors associated with both persistence and compliance were tested by changing the duration of the permissible gap allowed while defining persistence and the PDC threshold used to define compliance. The persistence analysis was therefore repeated using a permissible gap of one time the day’s supply to define persistence, and the compliance analysis was repeated using ≥70% and ≥90% as PDC thresholds for defining compliance. The statistical analyses were conducted using SAS 9.4 (SAS Institute Inc., Cary, NC, USA).
The Quebec Commission on access to personal information provided approval to RAMQ to send us the data. The research ethics committee of the CHU de Québec approved the study.
Results
Of the 7,119 patients included in this study, 5,609 (78.8%) were persistent with AH treatment. One factor associated with persistence was the number of physician visits made; individuals who visited their physicians ≥17 times were less likely to be persistent than those who made between 0 and 8 visits. In addition, individuals whose AH treatment was not initiated on the date of CKD diagnosis were less likely to be persistent. In contrast, compared with individuals whose initial treatment was diuretic monotherapy, those initiated on an angiotensin-converting enzyme inhibitor, an angiotensin II receptor blocker, a β-blocker, a calcium channel blocker, or a multidrug therapy were more likely to be persistent. Similarly, individuals who had a diagnosis of dyslipidemia, stroke, or coronary disease were also more likely to be persistent (Table 1).
Of the 5,609 patients who persisted with AH treatment, the mean PDC was 91.2% (median: 96.4%), and 4,920 (87.7%) of them were deemed compliant. Individuals aged ≥60 years, those with a low socioeconomic status, and women were more likely to be compliant. Similar to the findings for persistence, individuals who initiated an angiotensin-converting enzyme inhibitor, a β-blocker, a calcium channel blocker, or a multidrug therapy were more likely to be compliant than individuals whose initial treatment was diuretic monotherapy. Moreover, patients whose AH was initiated between 7 and 448 days after being diagnosed with CKD were less likely to be compliant than those who initiated the AH on the date of diagnosis. Patients who had CKD comorbidities such as dyslipidemia and stroke were also more likely to be compliant (Table 2).
There was no variation in the factors associated with persistence when the duration of the permissible gap used for defining persistence was changed. Similarly, the factors associated with compliance were not sensitive to changes in the PDC threshold that was used to define compliance (the results are not shown).
Discussion
In this study, we found that in 1 year after initiating AH treatment, approximately 21% of CKD patients were no longer persistent with AH treatment. Of the persistent individuals, approximately 12% were noncompliant. Overall, 31% of the study population was either not persistent or not compliant.
Although conducted on patients using AH but not necessarily suffering from CKD, previous studies have also reported suboptimal levels of persistence with AH treatment.18–21 In a study of patients from Pennsylvania (USA), British Columbia (Canada), and the Netherlands, researchers observed that irrespective of the country, approximately 24% of the patients did not persist (defined as having at least 180 consecutive days without AH in the year following treatment initiation).18 Qvarnstrom et al19 also observed that in the first year following AH initiation, ~26% of patients had been more than 30 days late refilling their prescriptions at least once and were therefore considered nonpersistent. The results of the two aforementioned studies18,19 are similar to our results, although the criteria for defining persistence in those studies differed from ours. However, in a recent study conducted in Ontario (Canada), Tu et al20 observed that in the year following treatment initiation, 35.4% of new AH users were not persistent with AH treatment. In a study using the French National Public Health Insurance Scheme database, researchers observed that 35% of the patients initiating AH treatment were no longer taking an AH at the end of the year following initiation.21 The higher proportion of nonpersistent patients observed in these two latter studies20,21 compared with our results could be explained by differences in the definitions of persistence or in the study populations. For example, in the study by Tu et al,20 nonpersistence was not assessed at the end of the 1-year period following treatment initiation. Nonpersistent individuals were those who had failed to refill their treatment within a 1.5 days’ supply window of a previous prescription anytime in the year following treatment initiation. In the study by Midy et al,21 individuals whose last refill before their 1-year anniversary of treatment initiation contained enough days’ supply to pass the 1-year anniversary mark were considered persistent. Although this method was similar to ours, it is unclear how persistence was calculated, as the number of days’ supply is not captured in the French National Public Health Insurance Scheme database.
The percentage of noncompliant patients (12.3%) that we observed is lower than that observed in the two studies conducted among CKD patients.12,13 In one analysis of administrative data on patients with CKD treated with AH in a Veterans Affairs Clinic in the Unites States, Schmitt et al13 observed that 33% of the patients had a PDC <80%. In another study, Muntner et al12 measured compliance with AH in patients treated for hypertension. They observed that among patients with CKD, 30% self-reported noncompliance. The lower proportion of noncompliant patients that we observed is likely because we assessed compliance only among patients who were persistent with treatment. The proportion of noncompliance would have been greater if we had included nonpersistent patients, as their PDC would be more likely to be low. The difference between our results and those observed by Muntner et al12 may also be due to the differences in how compliance was measured. Self-reported measures of compliance are known to exhibit poor agreement with those based on pharmacy dispensing data, which was the method that we used.22 However, our results are consistent with those observed in a study in which patients with CKD who were treated with an AH were interviewed during a visit to an ambulatory nephrology clinic.11 In that study, 17.7% of the patients self-reported noncompliance with AH. Comparing our results with those reported in the aforementioned studies is challenging because all of those studies included current users of AH, as opposed to only including new users as we did in ours. Indeed, the population of current users of AH includes fewer patients who discontinue their treatment early.
To our knowledge, this study is the first to identify factors associated with both constructs of adherence – persistence and compliance – with AH in a population of patients with CKD who initiated their AH treatment after CKD diagnosis. We found three factors to be associated with both persistence and compliance: choice of initial AH treatment, history of dyslipidemia and stroke, and time between date of CKD diagnosis and AH treatment initiation.
Compared with patients initiated on diuretics, those initiated on an angiotensin-converting enzyme inhibitor, angiotensin II receptor blocker, β-blocker, calcium channel blocker, and multiple AH were all more likely to be persistent. Other authors have also observed that patients initiating an AH treatment with diuretics are more likely to discontinue their treatment than those whose initial treatment is from another AH class.23,24 Regarding the increased likelihood of compliance among individuals who persisted, we observed similar associations (with the exception of those initiated on an angiotensin II receptor blocker). Our findings on the effect of the choice of initial drug treatment are consistent with the findings observed in studies on persistence with AH regardless of whether the patients had CKD.18,20,23,25,26 In addition, our results add to previous evidence18,25 that the likelihood of persistence is higher for those initiated on a multiple drug therapy. The association between the initial AH treatment and compliance is also observed to be consistent with the results observed in one study27 on new AH users that investigated the factors associated with compliance among patients who were persistent with the AH treatment. In that study, those initiated on an angiotensin-converting enzyme inhibitor were more likely to self-report compliant behavior.27 However, the clinical impact of our results regarding the role of the initial AH is unclear, as the effect size as measured by prevalence ratios was low and indicated an increased likelihood of compliance of no more than 15%.
Patients suffering from comorbidities of CKD such as dyslipidemia and stroke were also more likely to be persistent and to be compliant with the AH treatment compared with patients without those comorbidities. Similar results have been observed in the multicountry study mentioned earlier,18 in which hypercholesterolemia was identified as a predictor of persistence in all the settings and stroke a significant predictor in British Columbia. In a recent study including new users of AH, Mancia et al25 observed that those who had a cardiovascular disease at baseline were more likely to be persistent with AH treatment. Suffering from a CKD-related comorbidity such as dyslipidemia or stroke may highlight the importance of taking the AH treatment to patients and thus improve their persistence and compliance with AH treatment.
Patients who initiated AH treatment more than 7 days after CKD diagnosis were less likely to be persistent. Of those who persisted, these patients were also less likely to be compliant. These results could be explained by the fact that those groups might include patients who have failed to fill their initial AH prescription (primary nonadherence). Those patients may also be less likely to persist with treatment once started. A study suggests that the proportion of patients not filling a first AH prescription could be as high as 28%.28
In this study, some factors were associated with either AH treatment persistence or compliance but not with both. For example, we observed that patients who visited a physician more than 17 times in the year prior to AH initiation were less likely to be persistent compared with those who had made between zero and eight visits. A similar association was not found with compliance among those who persisted. In contrast, we observed that increasing age (71 years and above vs aged between 18 and 60 years old), low socioeconomic status (vs high), and being female were factors associated with an increased likelihood of compliance but not of persistence. Other studies on hypertension27 and schizophrenia29 have similarly found factors that are associated with persistence and not with compliance and vice versa. Our results add further support to the need to separately study persistence and compliance. This is particularly important because for interventions to be efficient, those aiming to optimize persistence may need to target different patient factors than those aiming to optimize compliance.
There are some limitations in our study. First, we assumed that the drugs claimed were taken. Therefore, we may have overestimated the extent of persistence and compliance. However, as we did not count the leftover days’ supply when patients had overlapping consecutive refills, both persistence and compliance may have been underestimated. Second, in our models, we included all patient-related, disease-related, and treatment-related factors likely to be associated with persistence and compliance that were available in the RAMQ databases. However, many more factors can contribute to medication persistence and compliance but are not captured in these databases. For example, we were unable to consider some potential factors that had been previously identified in prior studies on hypertension, such as stage of CKD,13 perceived side effects,26 and the belief that hypertension is a risk factor for other diseases.27 In addition, we were unable to separate the patients who discontinued the AH from those whose physicians discontinued the treatment.
Despite these limitations, we were able to study a large population of CKD patients in a real-life practice setting. We longitudinally assessed persistence and compliance as two different constructs of adherence over a 1-year period.
Conclusion
CKD is a debilitating chronic condition that requires long-term and continuous treatment of risk factors to slow down its progression. This is particularly true for patients who require AH treatment. Persistence and compliance with the AH treatment are important to achieve blood pressure control, preventing the progression of CKD and minimizing cardiovascular risk. Our results suggest that nearly a third of CKD patients who undergo an AH treatment may not fully benefit from it.
In this study, we identified several factors associated with persistence and with compliance. This knowledge may help target at-risk patients while developing interventions to prevent nonpersistence and noncompliance.
Acknowledgments
The authors thank Éric Demers for his assistance in the data analyses. This study was funded by the Laval University’s Chair on Adherence to Treatments. The Chair was funded by the Laval University Foundation and by unrestricted grants from AstraZeneca Canada and Sanofi Canada.
Disclosure
The authors declare no conflicts of interest in this work.
References
Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int Suppl. 2013;3:1–150. | ||
Collins AJ, Foley RN, Chavers B, et al. United States Renal Data System 2011 Annual Data Report: Atlas of chronic kidney disease & end-stage renal disease in the United States. Am J Kidney Dis. 2012;59(Suppl 1):e1–e420. | ||
Levin A, Hemmelgarn B, Culleton B, et al. Guidelines for the management of chronic kidney disease. CMAJ. 2008;179(11):1154–1162. | ||
Mazzaglia G, Ambrosioni E, Alacqua M, et al. Adherence to antihypertensive medications and cardiovascular morbidity among newly diagnosed hypertensive patients. Circulation. 2009;120(16):1598–1605. | ||
Perreault S, Dragomir A, White M, Lalonde L, Blais L, Berard A. Better adherence to antihypertensive agents and risk reduction of chronic heart failure. J Intern Med. 2009;266(2):207–218. | ||
Roy L, White-Guay B, Dorais M, Dragomir A, Lessard M, Perreault S. Adherence to antihypertensive agents improves risk reduction of end-stage renal disease. Kidney Int. 2013;84(3):570–577. | ||
Nasseh K, Frazee S, Visaria J, Vlahiotis A, Tian Y. Cost of medication nonadherence associated with diabetes, hypertension and dyslipidemia. Am J Pharm Benefits. 2012;4(2):e41–e47. | ||
Wahl C, Grégoire JP, Teo K, et al. Concordance, compliance and adherence in healthcare: closing gaps and improving outcomes. Healthc Q. 2005;8(1):65–70. | ||
Cramer JA, Roy A, Burrell A, et al. Medication compliance and persistence: terminology and definitions. Value Health. 2008;11(1):44–47. | ||
Lee JY, Kusek JW, Greene PG, et al. Assessing medication adherence by pill count and electronic monitoring in the African American Study of Kidney Disease and Hypertension (AASK) Pilot Study. Am J Hypertens. 1996;9(8):719–725. | ||
Moreira LB, Fernandes PF, Mota RS, et al. Medication noncompliance in chronic kidney disease. J Nephrol. 2008;21(3):354–362. | ||
Muntner P, Judd SE, Krousel-Wood M, McClellan WM, Safford MM. Low medication adherence and hypertension control among adults with CKD: data from the REGARDS (reasons for geographic and racial differences in stroke) Study. Am J Kidney Dis. 2010;56(3): 447–457. | ||
Schmitt KE, Edie CF, Laflam P, Simbartl LA, Thakar CV. Adherence to antihypertensive agents and blood pressure control in chronic kidney disease. Am J Nephrol. 2010;32(6):541–548. | ||
Vick SA, Maxwell CJ, Hogan DB, Patten SB, Johnson JA, Romoko-Slack L. Assessing medication adherence among older persons in community settings. Can J Clin Phamacol. 2005;12:e152–e164. | ||
Tamblyn R, Lavoie G, Petrella L, Monette J. The use of prescription claims databases in pharmacoepidemiological research: the accuracy and comprehensiveness of the prescription claims database in Quebec. J Clin Epidemiol. 1995;48(8):999–1009. | ||
Ronksley PE, Tonelli M, Quan H, et al. Validating a case definition for chronic kidney disease using administrative data. Nephrol Dial Transplant. 2012;27(5):1826–1831. | ||
Zou GY, Donner A. Extension of the modified Poisson regression model to prospective studies with correlated binary data. Stat Methods Med Res. 2013;22(6):661–670. | ||
van Wijk BL, Shrank WH, Klungel OH, Schneeweiss S, Brookhart MA, Avorn J. A cross-national study of the persistence of antihypertensive medication use in the elderly. J Hypertens. 2008;26(1):145–153. | ||
Qvarnstrom M, Kahan T, Kieler H, et al. Persistence to antihypertensive drug treatment in Swedish primary healthcare. Eur J Clin Pharmacol. 2013;69(11):1955–1964. | ||
Tu K, Anderson LN, Butt DA, et al. Antihypertensive drug prescribing and persistence among new elderly users: implications for persistence improvement interventions. Can J Cardiol. 2014;30(6):647–652. | ||
Midy F, Rudnichi A. The impact of cardiovascular profile on persistence associated with antihypertensive medications. Int J Clin Pract. 2013;67(12):1334–1341. | ||
Guénette L, Moisan J, Preville M, Boyer R. Measures of adherence based on self-report exhibited poor agreement with those based on pharmacy records. J Clin Epidemiol. 2005;58(9):924–933. | ||
Bourgault C, Sénécal M, Brisson M, Marentette MA, Grégoire JP. Persistence and discontinuation patterns of antihypertensive therapy among newly treated patients: a population-based study. J Hum Hypertens. 2005;19(8):607–613. | ||
Patel BV, Remigio-Baker RA, Mehta D, Thiebaud P, Frech-Tamas F, Preblick R. Effects of initial antihypertensive drug class on patient persistence and compliance in a usual-care setting in the United States. J Clin Hypertens. 2007;9(9):692–700. | ||
Mancia G, Zambon A, Soranna D, Merlino L, Corrao G. Factors involved in the discontinuation of antihypertensive drug therapy: an analysis from real life data. J Hypertens. 2014;32(8):1708–1715. | ||
Grégoire JP, Moisan J, Guibert R, et al. Determinants of discontinuation of new courses of antihypertensive medications. J Clin Epidemiol. 2002;55(7):728–735. | ||
Grégoire JP, Moisan J, Guibert R, Ciampi A, Milot A. Predictors of self-reported noncompliance with antihypertensive drug treatment: a prospective cohort study. Can J Cardiol. 2006;22(4):323–329. | ||
Fischer MA, Stedman MR, Lii J, et al. Primary medication non-adherence: analysis of 195,930 electronic prescriptions. J Gen Intern Med. 2010;25(4):284–290. | ||
Cooper D, Moisan J, Grégoire JP. Adherence to atypical antipsychotic treatment among newly treated patients: a population-based study in schizophrenia. J Clin Psychiatry. 2007;68(6):818–825. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.