Back to Journals » Clinical and Experimental Gastroenterology » Volume 13
Peroral Endoscopic Myotomy as a Novel Treatment for Achalasia: Patient Selection and Perspectives
Authors Chadalavada P, Thota PN, Raja S, Sanaka MR
Received 30 July 2020
Accepted for publication 19 October 2020
Published 3 November 2020 Volume 2020:13 Pages 485—495
DOI https://doi.org/10.2147/CEG.S230436
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Andreas M. Kaiser
Pravallika Chadalavada,1 Prashanthi N Thota,2 Siva Raja,3 Madhusudhan R Sanaka2
1Department of Internal Medicine, Cleveland Clinic, Cleveland, OH, USA; 2Department of Gastroenterology and Hepatology, Digestive Disease and Surgery Institute, Cleveland Clinic, Cleveland, OH, USA; 3Department of Cardiothoracic Surgery, Cleveland Clinic, Cleveland, OH, USA
Correspondence: Madhusudhan R Sanaka
Department of Gastroenterology and Hepatology, Digestive Disease and Surgery Institute, Cleveland Clinic, 9500 Euclid Avenue, Cleveland, OH 44195, USA
Tel +1 (216)-444-3423
Fax +1 216-444-6284
Email [email protected]
Abstract: Achalasia is a rare esophageal motility disorder characterized by esophageal aperistalsis and impaired relaxation of lower esophageal sphincter. There is no cure for achalasia and all the current treatments are aimed at palliation of symptoms by reducing the lower esophageal sphincter pressure. Currently, laparoscopic Heller myotomy (LHM) with partial fundoplication is considered the most effective and durable treatment option owing to its superiority over other treatments such as pneumatic dilation. Advancements in interventional endoscopy led to a novel minimally invasive endoscopic alternative to LHM, namely peroral endoscopic myotomy (POEM). In the last decade since its inception, POEM expanded rapidly throughout the world due to excellent safety profile and its efficacy comparable to LHM. The main drawback of POEM is gastroesophageal reflux disease since it is not combined with an anti-reflux procedure. The current review focuses on the indications, contraindications, technique, outcomes of POEM in various patient populations, and complications along with its effectiveness in comparison to LHM and pneumatic dilation.
Keywords: achalasia, peroral endoscopic myotomy, Eckardt score, POEM
Background
Achalasia is a chronic esophageal motility disorder characterized by impaired LES relaxation and esophageal aperistalsis. Classic symptoms include progressive dysphagia to solids and liquids, regurgitation of undigested food, chest pain and weight loss. It is a rare disease with an estimated prevalence of 10.82 and incidence of 0.3–1.63 per 100,000 adults per year.1 It has an equal predisposition with regard to race and gender with a reported mean age at diagnosis of 50 years.1 All the available treatments for achalasia are palliative and are directed towards lowering the high LES pressure. The conventional treatments for achalasia include botulinum toxin injection (BTI) to LES, pneumatic dilation (PD), and LHM along with partial fundoplication. Peroral endoscopic myotomy (POEM) is a recently emerging treatment modality.2 Medications such as calcium channel blockers and nitrates are ineffective and rarely used.3
PD involves a forceful endoscopic dilation of the LES using a large diameter hydrostatic balloon varying in diameter from 30 mm to 40 mm. PD provides excellent symptom relief in 90% of the patients but the effect declines in 1/3rd of these patients over a span of 4–6 years.4 Thus, many patients who undergo PD require repeated graded dilations with larger balloons, thus increasing the risk of perforation. BTI to LES is easy to administer and has a good safety profile.5 However, the durability of this treatment is limited to few months requiring repeat injections. Repeated BTI also causes fibrosis of the LES, making it challenging to perform a subsequent myotomy. Hence, it is mainly considered a salvage therapy for the frail and elderly. LHM with partial fundoplication has demonstrated superior efficacy over BTI and PD in various studies and became the time-honored treatment of choice in achalasia patients.6 LHM provides long-standing relief of dysphagia in up to 90% (range 76–100%) of the patients with low complication rate.7 Owing to the progressive nature of achalasia, the success rates of LHM have also been noted to decrease to 65–85% at a follow-up of 5 years.8 An endoscopic alternative to surgical myotomy, namely peroral endoscopic myotomy (POEM) was first reported in 2008.9 POEM has is emerging as a preferred treatment of choice for achalasia with proven success in patients of all age groups, in all subtypes and stages of achalasia.10
Evolution of Peroral Endoscopic Myotomy (POEM)
The concept of endoscopic myotomy was initially proposed by Ortega et al11 where an electrosurgical knife was used to dissect the lower esophageal rosette without manipulation of the distal anti-reflux zone. However, direct endoscopic myotomy was associated with severe complications and it never made into widespread practice and was eventually abandoned. POEM was first described by Pasricha et al12 in 2007 in a porcine model, using a submucosal tunnel to perform LES myotomy. Inoue et al13 improvised this technique and performed the first-ever POEM in humans and reported 100% technical success in a series of 17 patients with achalasia in 2010. Ever since, POEM has rapidly gained widespread adoption across the world as a safe and effective treatment for achalasia patients.
Patient Selection and Considerations for POEM
Work-Up in Patients with Suspected Achalasia
Definitive diagnosis of achalasia requires a careful clinical history, esophagogastroduodenoscopy (EGD), barium swallow and a high-resolution esophageal manometry (HREM).14 Presenting symptoms include dysphagia to solids and liquids over several years, regurgitation, chest pain, weight loss and sometimes atypical symptoms such as cough and aspiration. Eckardt score is a standardized, validated scoring system used for symptom assessment in achalasia. It scores the four symptoms of achalasia (dysphagia, regurgitation, chest pain, and weight loss) based on their severity on a point scale of 0–3. The total score ranges from 0 to 12 with a higher score suggesting more severe symptoms and a score less than 3 used to define remission or successful palliation of symptoms.
Esophagogastroduodenoscopy (EGD)
All patients with suspected achalasia should undergo an EGD to rule out any mechanical obstruction such as esophageal cancer2 or pseudoachalasia,15 as both these diseases can mimic achalasia. Patients presenting at an older age with rapidly progressive symptoms or significant weight loss should be evaluated for pseudoachalasia by an endoscopic ultrasound or computed tomography (CT) scan of the chest. EGD findings such as retained saliva, undigested food, or liquid in the esophagus, in the absence of any underlying mechanical obstruction (mass or stricture), are supportive of diagnosis of achalasia and may be present in up to one-third of the affected patients (Figure 1A and B).16 A characteristic “pop” is felt when endoscope passes through LES.
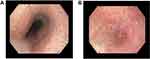 |
Figure 1 (A) Frothy secretion seen in mid esophagus, and (B) food debris in lower esophagus and tight GEJ. |
Barium Esophagram
Visualization of a dilated proximal esophagus with a narrow gastroesophageal junction giving the characteristic “bird beak” appearance on the barium esophagram is highly suggestive of achalasia (Figure 2). Both EGD and barium esophagram are only complementary to esophageal manometry and lack sensitivity for accurately diagnosing achalasia.17,18 While a barium swallow is used for the structural evaluation of the esophagus, a timed barium esophagram (TBE) is performed to specifically evaluate the degree of esophageal emptying. Radiographic images of the esophagus are taken at timed intervals after the patients are instructed to drink the maximum volume of dilute barium sulfate contrast that they could tolerate (mostly between 100 and 250 mL) over a period of 30 to 45 seconds.19 Height and width of the barium column are then measured using a calibrated ruler with the patient in upright position. Barium column height >2 cm at 5 minutes can be used as a cut off for diagnosing achalasia due to a sensitivity of 85% and specificity of 86% in differentiating untreated achalasia from esophagogastric junction outflow obstruction (EGJOO) and non-achalasia.20
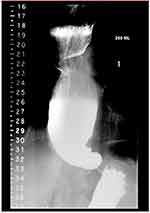 |
Figure 2 Dilated esophagus with retained barium and tapered bird beak appearance at GEJ. |
High-Resolution Esophageal Manometry (HREM)
HREM is the gold standard test for confirming the diagnosis of achalasia and defining the type of achalasia.21 The presence of inadequate relaxation of LES (mean 4-second integrated relaxation pressures (IRP) >15 mmHg) and aperistalsis of the esophageal body in the absence of a mechanical obstruction confirms the diagnosis of achalasia.2,21 Based on Chicago classification, achalasia is classified into: Type I – Absent peristalsis with minimal or no esophageal pressurization; Type II – Absent peristalsis with pan esophageal pressurization in ≥20% of swallows; and Type III – Absent peristalsis with premature contractions in ≥20% of swallows. Thus, HREM not only confirms the diagnosis of achalasia but also enables recognition of subtypes of achalasia with different treatment-outcome implications.14
Indications for POEM
POEM is indicated in all patients with Type I and II achalasia as an alternative to PD and LHM14 and preferred treatment of choice in type III achalasia. Patients who underwent prior therapy for achalasia such as PD,22 BTI,23 LHM,24 or even previous POEM are all suitable candidates for POEM. Several series have also reported excellent technical success of POEM even in pediatric patients. Of note, POEM is also being used for the treatment of other esophageal motility disorders such as distal esophageal spasm (DES) and jackhammer esophagus refractory to conventional treatments.25–30 A systematic review of 8 studies including 179 patients by Khan et al31 reported a clinical success of 88% for DES and 72% for Jackhammer esophagus. Another study by Khashab et al25 reported a 93.3% clinical success in 15 patients with esophago-gastric outflow obstruction (EGJOO) who underwent POEM.
Contraindications of POEM
The widely accepted consensus on the absolute contraindications to POEM include severe coagulopathy or bleeding diathesis, severe reflux esophagitis, presence of decompensated liver cirrhosis with portal hypertension, and severe lung disease.14 Patients who underwent prior endoscopic mucosal resection, radiation or radiofrequency ablation are also not suitable candidates as these procedures cause fibrosis and obliteration of submucosal plane. Large mouthed esophageal diverticula are considered a relative contraindication depending on their size and location.
Pre-Operative Care
Patients are advised to be on a clear liquid diet for two days before the procedure and are kept nil per os (NPO) past midnight on the day prior to the procedure. It is prudent to remove any food residue in the esophagus via endoscopy prior to POEM, especially in patients with sigmoid esophagus. All patients are given intravenous broad-spectrum antibiotics on the day of POEM. Due to the high risk of bleeding, anticoagulant and antiplatelet medications should be withheld prior to POEM with the exception of aspirin when medically indicated.
POEM Technique
POEM requires a thorough understanding of the surgical anatomy and technical expertise in the field of interventional endoscopy. After an initial training on animal and cadaveric models followed by observation of several live human cases, structured proctoring of at least 15 POEMS in the porcine esophagus is recommended.32 All POEM procedures at our institution are performed under general anesthesia in an operating room using the standard steps as proposed by Inoue et al.13 The sequence of steps in POEM as illustrated in Figure 3 include (1) creation of a submucosal tunnel starting approximately 10–12 cm proximal to the LES and extending distally to about 2–4 cm into the stomach side (A and B); (2) Myotomy of the circular muscle fibers starting 3–4 cm distal to the entry site and extending 2–4 cm into the stomach wall (C); and (3) Closure of the entry site of the submucosal tunnel by using endoscopic clips (D).
Post-Operative Care and Follow-Up
Patients are kept NPO till, a water-soluble contrast esophagram is obtained to identify any esophageal leak on the first post-operative day. In the absence of a leak, patients are started on a liquid diet and advanced to a soft diet and subsequently transition to a regular diet over the next few weeks. Post-procedure pain is usually controlled with non-opioid analgesics or modest doses of opioids, if required.33 Patients are started on proton pump inhibitors in the post-operative period. A chest X-ray or a CT scan can be considered to evaluate for compression atelectasis, pleural effusion, or pneumothorax in patients with persistent hypoxia during the post-operative period. Patients with uneventful recovery are typically discharged home on first postoperative day. In our institution, approximately 2 months after POEM, patients undergo clinical assessment for improvement in Eckardt scores, and objective assessment with EGD for reflux esophagitis, pH study for abnormal esophageal acid exposure, barium esophagram for esophageal emptying and HREM for reduction in LES-IRP. Thereafter, they have routine annual follow-ups.
POEM Outcomes
The clinical success is defined as reduction of post-procedure Eckardt score to ≤3 or a decrease in LES residual pressure by >50%.10 Other commonly measured outcomes include barium esophagram and quality of life with patient-reported outcomes. In a review of 841 patients who underwent POEM, 82–100% of the patients had a post treatment Eckardt score of ≤3 and a decrease in LES-IRP of >50%. Many studies also demonstrated improvement in the TBE parameters with >90% emptying of the barium column in 93% patients after POEM.34–36 In a study of 143 achalasia patients during a 3-year follow-up after POEM, there was a remarkable improvement in all dimensions of short- and long-term health-related quality of life (HRQOL) as measured by the SF-36 survey.37 There appears to be a strong association between the Eckardt score and the HRQOL mental and physical component scores following POEM.38 As such, major societies such as the American Society for Gastrointestinal Endoscopy (ASGE) and the Japan Gastroenterological Endoscopy Society (JGES) now recommend POEM as one of the primary treatment options for achalasia.9,14 Despite the efficacy of POEM being well established in the short to mid-term management of achalasia, data is sparse on the long-term durability of this novel therapy. Li et al39 estimated that the clinical success decreased from 94.2% at 1 year to 87.1% at 5 years. A multivariate cox regression analysis revealed a long disease duration (>10 years) and a history of prior interventions to be major risk factors for disease recurrence. In a Japanese study of 500 achalasia patients, clinical success had decreased to 88% at a 3-year follow-up compared to 91% at 1–2 years after POEM.40 Another German study reported symptom recurrence in 17.7% of the treated patients during the long term follow up, suggesting an overall decrease in success rate to 78% at 24–49 months.41
Achalasia with Failed Prior Therapy
Almost 40% of the patients referred for POEM had prior failed therapy for achalasia according to a global POEM experience survey.42 The high success and low complication rate of POEM, now make it a go-to treatment for patients with recurrent symptoms after LHM. In a meta-analysis.43 POEM was successful in 98% of patients with prior failed LHM. Another study suggested that POEM had lower operative time and shorter length of stay over redo-LHM in patients with failed prior LHM.44 In patients with prior LHM, a posterior myotomy is preferred. A posterior myotomy is equally effective as anterior myotomy and could be performed in 100% of patients with failed LHM.45 Recently, a prospective study by Nabi et al46 demonstrated that the clinical success was achieved in 96.8% of previously treated patients when compared to 97.3% of treatment-naïve patients at one year follow up after POEM (p = 0.795). Hence, POEM is very safe and efficacious in treating patients who failed prior treatments such as BTI, PD or LHM.
Advanced Achalasia
Patients with end-stage achalasia and sigmoid esophagus often have poor response to conventional treatments such as LHM or PD and may require esophagectomy for palliation of symptoms.38 Emerging data indicate that POEM achieves promising results even in advanced end-stage achalasia.47,48 Hu et al49 reported that POEM achieved long-term dysphagia relief in 96% of the patients with sigmoid esophagus at a 2-year follow-up with minimal complications. Of note, the sigmoid configuration might make creation of submucosal tunneling technically challenging and time consuming.
Special Situations
Obese Patients
In obese patients, LHM is associated with suboptimal clinical outcomes or high rate of postoperative GERD.50 A growing body of research has proposed POEM as an exciting option for management of achalasia before or after a Roux-en-Y gastric bypass (RYGB). A recent review by Aiolfi et al51 including 12 studies with 28 patients summarized the current treatments for achalasia after RYGB. In that review, 61% of patients had LHM, and 39% had a POEM. The overall complication rate and disease recurrence requiring retreatment was not significantly different between LHM and POEM. Bashir et al52 and a few others53,54 performed POEM before or after RYGB and reported excellent symptomatic resolution and clinical success. Despite obesity being an independent risk factor for GERD in comparison to the general population, it certainly does not bestow a higher superimposed risk of reflux esophagitis following POEM.54 Hence, it is believed that obese patients might achieve better outcomes with POEM over LHM due to the lower reported risk of iatrogenic reflux with the former.
High Surgical Risk Patients
It is well known that an increasing American Society of Anesthesiologists (ASA) physical class is associated with higher perioperative morbidity and mortality.56 The minimally invasive alternative to the surgical myotomy, POEM, seems to be an appealing option for these high-risk patients with achalasia. We compared the outcomes of POEM in achalasia patients with lower ASA class (combined ASA I and II) versus higher ASA class (combined ASA class III and IV) at our institution. Treatment success was similar in both groups and was achieved in 92% of the patients in higher ASA class group with a remarkable improvement in HREM and TBE parameters. There was no significant difference in the post-operative GERD between patients belonging to the two groups, and none of our patients had a prolonged length of stay or admission to an intensive care unit.
Geriatric Patients
POEM is emerging as a safe and effective therapy for older patients with achalasia. Recent studies have reported a high safety and success rates of POEM in geriatric patients.57,58 An international multicenter retrospective study, including eight centers (4 US, 3 European, and 1 Asian), reported a clinical success of 96% with a significant post POEM LES IRP reduction by 12.4 mmHg at a median follow-up duration of 256 days in octogenarians.59
Pediatric Patients
Achalasia is extremely rare in children. Nabi et al60 performed POEM on 15 children with achalasia and reported a 100% resolution of symptoms at a 1-year follow-up. A prospective study by Chen et al61 also reported a 100% clinical success in 26 children at a mean follow-up of 24 months. However, about 20% of patients developed mild esophagitis which responded to PPIs.59,60 Possible sequelae of POEM, several decades later in this population remains unknown and requires careful observation.
Complications and Safety Profile of POEM
POEM has a relatively low incidence of perioperative complications when performed by operators after adequate training.62 As described by Nabi et al63 the most common adverse events (AEs) that occur during POEM include CO2 insufflation-related events such as subcutaneous emphysema (7.5%), mediastinal emphysema (1.1%), pneumoperitoneum (6.8%) and pneumothorax (1.2%). Most of these gas-related side effects have no clinical significance and only 6% require an active intervention.64 The other intraoperative AEs include mucosal injury or perforation (4.8%), which can be managed simultaneously and usually do not lead to any unforeseen consequences. While intraprocedural bleeding can occur during any of the steps in POEM, most of these episodes are minor, and significant bleeding requiring interventions is rare (0.2%; 95% confidence interval, 0–1.4%).65 The delayed post-procedural complications, such as delayed mucosal perforation or bleeding are rare, and generally troublesome and challenging to manage.66
In a comprehensive analysis of 1826 patients who underwent POEM by Haito et al67 the incidence of adverse events (AEs) was as low as 7.5% with the most common complication being an inadvertent mucosostomy (2.8%) followed by symptomatic capnoperitoneum (1.2%), and esophageal leak (0.7%). On multivariate analysis, the significant factors associated with a high risk of perioperative complications were advanced achalasia with sigmoid configuration, inexperienced operator, and usage of a triangular tipped knife. Serious adverse events such as pneumonia, empyema and esophageal leak occurred in less than 0.5% of the studied patients.
Another study of 1912 achalasia patients by Wang et al68 suggested that the overall frequency of intraoperative complications from POEM was 17.1%. Prior LHM or POEM, presence of submucosal fibrosis, longer submucosal tunnel length (≥13 cm) and mucosal edema were associated with a higher occurrence of mucosal injury. Having a POEM technical experience of more than a year was a strong protective factor against any degree of mucosal injuries.
GERD After POEM
GERD is an important drawback of POEM. In an international multicenter study of 282 patients followed for 10–24 months after POEM with careful reflux testing, 58% had abnormal pH study, 25% had reflux esophagitis on EGD and 40% were taking PPI.69 GERD rates are significantly higher after POEM compared to LHM with fundoplication. A systematic review and meta-analysis showed pooled rates of abnormal esophageal acid exposure and esophagitis were 39% and 29.4% after POEM compared to 16.8% and 7.6% after LHM.70 Another meta-analysis reported that compared to LHM with fundoplication, POEM patients were more likely to develop GERD symptoms (OR 1.69, 95% CI 1.33–2.14, P < 0.0001), GERD evidenced by erosive esophagitis (OR 9.31, 95% CI 4.71–18.85, P < 0.0001), and GERD evidenced by pH monitoring (OR 4.30, 95% CI 2.96–6.27, P < 0.0001).71 In our institution's experience, rates of abnormal acid exposure were 48.4% after POEM compared to 13.6% after LHM (p < 0.001).72
Although numerous studies have reported a relatively high incidence of iatrogenic acid reflux after POEM, extensive heterogeneity exists among their results due to the variable metrics used to indicate GERD and the duration of follow up. Assessments usually include symptom questionnaires, use of proton pump inhibitors, 24-hr pH abnormalities and endoscopic evaluation of reflux esophagitis. As such, it is essential to acknowledge that the variability in the evaluation of GERD among various studies including large meta-analyses, may account for wide range of incidence reported in literature thus far. Interestingly, the most sensitive measure of GERD, acid exposure time (AET), appears to be the least reported metric after POEM.65,71 A meta-analysis by Repici et al70 suggested that the geographic location and patient sex also seem to be associated with variable incidence of GERD after POEM. The occurrence of post-POEM GERD was noted to be lower in studies conducted in Asian population when compared to the Non-Asian studies with a reported incidence of 16% and 22.8%, respectively. This observed difference was postulated to be secondary to lower prevalence of GERD and factors involved in the pathogenesis of GERD such as lifestyle, dietary habits, prevalence of H. pylori and chronic atrophic gastritis in the Asian population. Lastly, selection bias may occur when only symptomatic patients undergo testing, further obscuring the available data.
Moreover, little is known about the intraoperative or other patient-related factors that might influence the occurrence of GERD following POEM. An Italian study by Familari et al73 reported that patient demographics such as age, previous therapies, type of achalasia, esophageal shape, LES pressure, and length of myotomy, correlated only minimally with the occurrence of GERD after POEM. Notably, despite the high incidence of clinically relevant GERD after POEM, many studies have reported complete resolution of this reflux with PPI therapy.74 Additionally, the long-term consequences of this pathologic acid reflux are not known. More extensive studies with long-term follow-up are needed to assess if these patients would eventually develop long-standing complications from GERD such as peptic strictures or Barrett’s esophagus. In fact, some experts recommend that prior to POEM, patients should be informed of the high risk of GERD and the need for long-term PPI therapy and/or surveillance endoscopy.75
Comparison of POEM Outcomes with LHM
POEM appears to be equally or more effective compared to LHM in treatment of achalasia. In a randomized control trial (RCT), clinical success was achieved in 83% of the patients in the POEM group and 81.7% in the LHM group with a significantly lower risk of serious adverse events (SAEs) with the former at a 2-year follow up.76 In a meta-analysis of about 7000 patients, POEM was more efficacious than LHM in relieving dysphagia during a serial follow up from 1 year to 5 years. When averaged across 74 studies, the improvement of dysphagia was reported by 93.2% of the patients who underwent POEM and 87.7% of patients after LHM. The probabilities for improvement in dysphagia at 12 months were 93.5% for POEM and 91.0% for LHM (p = 0.01), and at 24 months were 92.7% for POEM and 90.0% for LHM (p = 0.01).71 They also found that POEM seemed to have a significant benefit over LHM in patients with Type III achalasia. Another meta-analysis, including 486 patients, reported an identical improvement in the post-treatment Eckardt score after POEM and LHM.77 The only notable disadvantage of POEM is the lack of anti-reflux procedure as compared to LHM, which is always combined with a partial fundoplication. Hence, GERD has been reported in 57% of patients after POEM compared to 20% after LHM.76
Comparison of POEM Outcomes with PD
POEM provides superior and long-lasting symptom relief compared to PD in patients with achalasia. A multicenter RCT78 demonstrated a significantly higher treatment success of POEM when compared to PD (92% vs 54%) in patients with treatment-naïve achalasia and zero serious adverse events. At a 2-year follow-up, 46% of the patients in the PD group had recurrence of symptoms requiring retreatments in contrast to only 8% in the POEM group. Furthermore, 1.5% in the PD group incurred a perforation despite the usage of the smallest 30-mm balloon. In a metanalysis,79 including 4407 achalasia patients POEM achieved higher rates of dysphagia remission when compared to PD (RR = 1.40; 95% CIs = 1.14–1.79). Another study by Zheng et al80 reported a success rate of 92.3% for POEM in contrast to 57.5% for PD at a follow-up of 12 months. Interestingly, the patients who underwent POEM had a greater improvement in Eckardt scores and LES-IRP than those who underwent PD at 1 month, 3 months, and even at 1 year after treatment.
Cost-Effectiveness
Miller et al81 concluded that POEM is more cost-effective than BTI due to the high failure rate of BTI. The cost per cure of POEM has decreased from $12,120 to $3030 over time, while the cost per cure for BTI gradually increased from $7862 at 1 year to $14,986 after 4 years. The cost per cure for PD had a trend from $7175 at 1 year to $ 2392 at 4 years. Although PD appeared to be more cost-effective at 1 year due to the high initial cost of POEM, the cost per cure of POEM began to equalize with PD at 4 years. Furthermore, BTI and PD are associated with additional costs as a vast majority of these patients would need retreatment with POEM within two years of initial therapy. As such, it might be ideal to reserve these therapies for patients with a life expectancy of <3 years or those who cannot tolerate general anesthesia.81 Additionally, Greenleaf et al82 conducted a cost-utility analysis of POEM and LHM and suggested that POEM appeared to more cost-effective relative to LHM, depending on one’s willingness to pay for additional quality-adjusted life-years gained by using POEM. Thus, POEM seems to be equivalent to LHM from an economic standpoint.
Criteria for Selection of Achalasia Patients for POEM Procedure
Based on the available data in literature as discussed above and our experience, we follow certain criteria for selection of patients for POEM procedure at our center. POEM is offered as first line of therapy for all type 3 achalasia patients. Type 1 achalasia patients with significantly dilated or sigmoidal esophagus are preferably treated with POEM. All achalasia patients with significant obesity are also preferentially treated with POEM, since partial fundoplication is not durable in these patients. Patients with recurrent symptoms after prior LHM are preferentially treated with posterior POEM, since repeat LHM is very difficult in these patients. POEM is also preferred treatment in patients with prior upper abdominal surgeries due to potential scarring making LHM technically challenging. POEM is also offered to patients with other esophageal motility disorders such as distal esophageal spasm, jackhammer esophagus and EGJ out flow obstruction, if other conventional treatments have failed to relieve the symptoms.
Conclusion
POEM is a novel procedure utilizing endoscopic approach to myotomy and a less invasive alternative to traditional LHM. There is rapid proliferation of POEM throughout the world since it was first reported in 2010. POEM is a very safe and highly effective treatment option for achalasia. POEM is indicated to treat all types of achalasia along with PD and LHM and is considered the preferred approach for type 3 achalasia. POEM has shown excellent short and intermediate term outcomes and the long-term outcome data are emerging. POEM is also indicated to treat other esophageal motility disorders refractory to conventional treatment options. The main disadvantage with POEM is the substantial increased risk of GERD since it is not combined with anti-reflux fundoplication as compared to LHM. The main disadvantage with POEM is the substantial increased risk of GERD since it is not combined with an anti-reflux fundoplication as compared to LHM. As such, patients selected for POEM should undergo careful consideration of long-term effects including complications prior to treatment. Further prospective studies are needed to shed light on the consequences of GERD in these patients.
Disclosure
All the authors declare that this review was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. The authors report no conflicts of interest for this work.
References
1. Sadowski DC, Ackah F, Jiang B, Svenson LW. Achalasia: incidence, prevalence and survival. A population-based study. Neurogastroenterol Motil. 2010;22(9):e256–e261. doi:10.1111/j.1365-2982.2010.01511.x
2. Vaezi MF, Pandolfino JE, Vela MF. ACG clinical guideline: diagnosis and management of achalasia. Am J Gastroenterol. 2013;108(8):1238–1249. doi:10.1038/ajg.2013.196
3. Zaninotto G, Bennett C, Boeckxstaens G, et al. The 2018 ISDE achalasia guidelines. Dis Esophagus off J Int Soc Dis Esophagus. 2018;31(9). doi:10.1093/dote/doy071
4. Richter JE. Update on the management of achalasia: balloons, surgery and drugs. Expert Rev Gastroenterol Hepatol. 2008;2(3):435–445. doi:10.1586/17474124.2.3.435
5. Yamaguchi D, Tsuruoka N, Sakata Y, Shimoda R, Fujimoto K, Iwakiri R. Safety and efficacy of botulinum toxin injection therapy for esophageal Achalasia in Japan. J Clin Biochem Nutr. 2015;57(3):239–243. doi:10.3164/jcbn.15-47
6. Von Rahden BHA. Current treatment of achalasia 2019. Zentralblatt fur Chir - Zeitschrift fur Allg Visz und Gefasschirurgie. 2019;144(2):163–170. doi:10.1055/a-0863-4917
7. Costantino CL, Geller AD, Visenio MR, Morse CR, Rattner DW. Outcomes of laparoscopic Heller myotomy for achalasia: 22-year experience. J Gastrointest Surg. 2020;24(6):1411–1416. doi:10.1007/s11605-020-04586-7
8. Vaezi MF, Felix VN, Penagini R, et al. Achalasia: from diagnosis to management. Ann N Y Acad Sci. 2016;1381(1):34–44. doi:10.1111/nyas.13176
9. Khashab MA, Vela MF, Thosani N, et al. ASGE guideline on the management of achalasia. Gastrointest Endosc. 2020;91(2):213–227.e6. doi:10.1016/j.gie.2019.04.231
10. Stavropoulos SN, Desilets DJ, Fuchs K-H; NOSCAR POEM White Paper Committee, et al. Per-oral endoscopic myotomy white paper summary. Gastrointest Endosc. 2014;80(1):1–15. doi:10.1016/j.gie.2014.04.014.
11. Ortega JA, Madureri V, Perez L. Endoscopic myotomy in the treatment of achalasia. Gastrointest Endosc. 1980;26(1):8–10. doi:10.1016/s0016-5107(80)73249-2
12. Pasricha PJ, Hawarl R, Ahmed I, et al. Submucosal endoscopic esophageal myotomy: a novel experimental approach for the treatment of achalasia. Endoscopy. 2007;39(9):761–764. doi:10.1055/s-2007-966764
13. Inoue H, Minami H, Kobayashi Y, et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42(4):265–271. doi:10.1055/s-0029-1244080
14. Inoue H, Shiwaku H, Iwakiri K, et al. Clinical practice guidelines for peroral endoscopic myotomy. Dig Endosc. 2018;30(5):563–579. doi:10.1111/den.13239
15. Roushan N, Zolfaghari A, Asadi M, Taslimi R. Pseudoachalasia: a diagnostic challenge. Med J Islam Repub Iran. 2014;28:54.
16. Howard PJ, Maher L, Pryde A, Cameron EW, Heading RC, Howard J. Five year prospective study of the incidence, clinical features, and diagnosis of achalasia in Edinburgh. Gut. 1992;33(8):1011–1015. doi:10.1136/gut.33.8.1011
17. Boeckxstaens GE, Zaninotto G, Richter JE. Achalasia. Lancet. 2014;383(9911):83–93. doi:10.1016/S0140-6736(13)60651-0
18. Francis DL, Katzka DA. Achalasia: update on the disease and its treatment. Gastroenterology. 2010;139(2):369–374.e2. doi:10.1053/j.gastro.2010.06.024
19. Neyaz Z, Gupta M, Ghoshal UC. How to perform and interpret timed barium esophagogram. J Neurogastroenterol Motil. 2013;19(2):251–256. doi:10.5056/jnm.2013.19.2.251
20. Blonski W, Kumar A, Feldman J, Richter JE. Timed barium swallow: diagnostic role and predictive value in untreated Achalasia, esophagogastric junction outflow obstruction, and non-Achalasia dysphagia. Am J Gastroenterol. 2018;113(2):196–203. doi:10.1038/ajg.2017.370
21. Kahrilas PJ, Bredenoord AJ, Carlson DA, Pandolfino JE. Advances in management of esophageal motility disorders. Clin Gastroenterol Hepatol. 2018;16(11):1692–1700. doi:10.1016/j.cgh.2018.04.026
22. Ponsky JL. Per-oral endoscopic myotomy after previous interventions for achalasia. J Xiangya Med. 2019;4:5. doi:10.21037/jxym.2018.12.03
23. Sharata A, Kurian AA, Dunst CM, Bhayani NH, Reavis KM, Swanström LL. Peroral Endoscopic Myotomy (POEM) is safe and effective in the setting of prior endoscopic intervention. J Gastrointest Surg. 2013;17(7):1188–1192. doi:10.1007/s11605-013-2193-6
24. Zhou PH, Li QL, Yao LQ, et al. Peroral endoscopic remyotomy for failed Heller myotomy: a prospective single-center study. Endoscopy. 2013;45(3):161–166. doi:10.1055/s-0032-1326203
25. Khashab M, Familiari P, Draganov P, et al. Peroral endoscopic myotomy is effective and safe in non-achalasia esophageal motility disorders: an international multicenter study. Endosc Int Open. 2018;06(08):E1031–E1036. doi:10.1055/a-0625-6288
26. Feng J, Ali RW, Hao JY, Kong GX, Yang LH, Huang XJ. Peroral endoscopic myotomy for esophageal motility disorders. Esophagus. 2020;17(1):11–18. doi:10.1007/s10388-019-00693-w
27. Bechara R, Ikeda H, Inoue H. Peroral endoscopic myotomy for Jackhammer esophagus: to cut or not to cut the lower esophageal sphincter. Endosc Int Open. 2016;04(05):E585–E588. doi:10.1055/s-0042-105204
28. Khashab MA, Messallam AA, Onimaru M, et al. International multicenter experience with peroral endoscopic myotomy for the treatment of spastic esophageal disorders refractory to medical therapy (with video). Gastrointest Endosc. 2015;81(5):1170–1177. doi:10.1016/j.gie.2014.10.011
29. Minami H, Isomoto H, Yamaguchi N, et al. Peroral endoscopic myotomy (POEM) for diffuse esophageal spasm. Endoscopy. 2014;46(SUPPL 1):E79–81. doi:10.1055/s-0032-1309922
30. Shiwaku H, Inoue H, Beppu R, et al. Successful treatment of diffuse esophageal spasm by peroral endoscopic myotomy. Gastrointest Endosc. 2013;77(1):149–150. doi:10.1016/j.gie.2012.02.008
31. Khan MA, Kumbhari V, Ngamruengphong S, et al. Is POEM the answer for management of spastic esophageal disorders? A systematic review and meta-analysis. Dig Dis Sci. 2017;62(1):35–44. doi:10.1007/s10620-016-4373-1
32. Eleftheriadis N, Inoue H, Ikeda H, et al. Training in peroral endoscopic myotomy (POEM) for esophageal achalasia. Ther Clin Risk Manag. 2012;8:329–342. doi:10.2147/TCRM.S32666
33. Misra L, Fukami N, Nikolic K, Trentman TL. Peroral endoscopic myotomy: procedural complications and pain management for the perioperative clinician. Med Devices Evid Res. 2017;10:53–59. doi:10.2147/MDER.S115632
34. Verlaan T, Rohof WO, Bredenoord AJ, Eberl S, Rösch T, Fockens P. Effect of peroral endoscopic myotomy on esophagogastric junction physiology in patients with achalasia. Gastrointest Endosc. 2013;78(1):39–44. doi:10.1016/j.gie.2013.01.006
35. Swanstrom LL, Kurian A, Dunst CM, Sharata A, Bhayani N, Rieder E. Long-term outcomes of an endoscopic myotomy for achalasia: the POEM procedure. Ann Surg. 2012;256:659–667. doi:10.1097/SLA.0b013e31826b5212
36. Hungness ES, Teitelbaum EN, Santos BF, et al. Comparison of perioperative outcomes between Peroral Esophageal Myotomy (POEM) and laparoscopic Heller myotomy. J Gastrointest Surg. 2013;17(2):228–235. doi:10.1007/s11605-012-2030-3
37. Perbtani YB, Mramba LK, Yang D, Suarez J, Draganov PV. Life after per-oral endoscopic myotomy: long-term outcomes of quality of life and their association with Eckardt scores. Gastrointest Endosc. 2018;87(6):1415–1420.e1. doi:10.1016/j.gie.2018.01.019
38. Patti MG, Schlottmann F, Herbella FA. The treatment of esophageal achalasia: at the intersection between innovation and patient’s care. J Laparoendosc Adv Surg Tech. 2020;30(3):233–235. doi:10.1089/lap.2019.0718
39. Li QL, Wu QN, Zhang XC, et al. Outcomes of per-oral endoscopic myotomy for treatment of esophageal achalasia with a median follow-up of 49 months. Gastrointest Endosc. 2018;87(6):1405–1412.e3. doi:10.1016/j.gie.2017.10.031
40. Inoue H, Sato H, Ikeda H, et al. Per-oral endoscopic myotomy: a series of 500 patients. J Am Coll Surg. 2015;221(2):256–264. doi:10.1016/j.jamcollsurg.2015.03.057
41. Werner YB, Costamagna G, Swanström LL, et al. Clinical response to peroral endoscopic myotomy in patients with idiopathic achalasia at a minimum follow-up of 2 years. Gut. 2016;65(6):899–906. doi:10.1136/gutjnl-2014-308649
42. Stavropoulos SN, Modayil RJ, Friedel D, Savides T. The international per oral endoscopic myotomy survey (IPOEMS): a snapshot of the global POEM experience. Surg Endosc. 2013;27(9):3322–3338. doi:10.1007/s00464-013-2913-8
43. Fernandez-Ananin S, Fernández AF, Balagué C, Sacoto D, Targarona EM. What to do when Heller’s myotomy fails? Pneumatic dilatation, laparoscopic remyotomy or peroral endoscopic myotomy: a systematic review. J Minim Access Surg. 2018;14(3):177–184. doi:10.4103/jmas.JMAS_94_17
44. Fumagalli U, Rosati R, De Pascale S, et al. Repeated surgical or endoscopic myotomy for recurrent dysphagia in patients after previous myotomy for achalasia. J Gastrointest Surg. 2016;20(3):494–499. doi:10.1007/s11605-015-3031-9
45. Ramchandani M, Nabi Z, Reddy D, et al. Outcomes of anterior myotomy versus posterior myotomy during POEM: a randomized pilot study. Endosc Int Open. 2018;06(02):E190–E198. doi:10.1055/s-0043-121877
46. Nabi Z, Ramchandani M, Chavan R, et al. Per-oral endoscopic myotomy for achalasia cardia: outcomes in over 400 consecutive patients. Endosc Int Open. 2017;05(05):E331–E339. doi:10.1055/s-0043-105517
47. Maruyama S, Taniyama Y, Sakurai T, et al. Per-oral endoscopic myotomy (POEM) for a sigmoid type of achalasia: short-term outcomes and changes in the esophageal angle. Surg Endosc. 2019. doi:10.1007/s00464-019-07180-4
48. Lv L, Liu J, Tan Y, Liu D. Peroral endoscopic full-thickness myotomy for the treatment of sigmoid-type Achalasia: outcomes with a minimum follow-up of 12 months. Eur J Gastroenterol Hepatol. 2016;28(1):30–36. doi:10.1097/MEG.0000000000000491
49. Hu JW, Li QL, Zhou PH, et al. Peroral endoscopic myotomy for advanced achalasia with sigmoid-shaped esophagus: long-term outcomes from a prospective, single-center study. Surg Endosc. 2015;29(9):2841–2850. doi:10.1007/s00464-014-4013-9
50. Nguyen D, Dip F, Lo Menzo E, Szomstein S, Rosenthal R. Heller oesophagomyotomy as treatment for achalasia after gastric bypass for morbid obesity. Ann R Coll Surg Engl. 2016;98(1):e3–e5. doi:10.1308/rcsann.2016.0006
51. Aiolfi A, Tornese S, Bonitta G, Rausa E, Micheletto G, Bona D. Management of esophageal achalasia after Roux-en-Y gastric bypass: narrative review of the literature. Obes Surg. 2019;29(5):1632–1637. doi:10.1007/s11695-019-03774-y
52. Bashir U, El Abiad R, Gerke H, Keech J, Parekh K, Nau P. Peroral endoscopic myotomy is feasible and safe in a gastric bypass population. Obes Surg. 2019;29(11):3523–3526. doi:10.1007/s11695-019-04026-9
53. Casas MA, Schlottmann F, Herbella FAM, Buxhoeveden R, Patti MG. Esophageal achalasia after Roux-en-Y gastric bypass for morbid obesity. Updates Surg. 2019;71(4):631–635. doi:10.1007/s13304-019-00688-3
54. Sanaei O, Draganov P, Kunda R, Yang D, Khashab MA. Peroral endoscopic myotomy for the treatment of achalasia patients with Roux-en-Y gastric bypass anatomy. Endoscopy. 2019;51(4):342–345. doi:10.1055/a-0656-5530
55. Sanaka MR, Parikh MP, Thota PN, et al. Tu1157 comparison of outcomes of Peroral Endoscopic Myotomy (POEM) in achalasia patients with or without prior Laproscopic Heller’s Myotomy (LHM). Gastrointest Endosc. 2018;87(6):AB546. doi:10.1016/j.gie.2018.04.2187
56. Doyle DJ, Garmon EH American Society of Anesthesiologists Classification (ASA Class). StatPearls Publishing; 2018. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28722969.
57. Chen Y-I, Inoue H, Ujiki M, et al. An international multicenter study evaluating the clinical efficacy and safety of per-oral endoscopic myotomy in octogenarians. Gastrointest Endosc. 2018;87(4):956–961. doi:10.1016/j.gie.2017.02.007
58. Li CJ, Tan YY, Wang XH, Liu DL. Peroral endoscopic myotomy for achalasia in patients aged ≥ 65 years. World J Gastroenterol. 2015. doi:10.3748/wjg.v21.i30.9175
59. Tang X, Ren Y, Gao Q, et al. Peroral endoscopic myotomy is safe and effective in achalasia patients aged older than 60 years compared with younger patients. Geriatr Gerontol Int. 2017;17(12):2407–2413. doi:10.1111/ggi.13083
60. Nabi Z, Ramchandani M, Nageshwar Reddy D, et al. Per oral endoscopic myotomy in children with Achalasia cardia. J Neurogastroenterol Motil. 2016;22(4):613–619. doi:10.5056/jnm15172
61. Chen WF, Li QL, Zhou PH, et al. Long-term outcomes of peroral endoscopic myotomy for achalasia in pediatric patients: a prospective, single-center study. Gastrointest Endosc. 2015;81(1):91–100. doi:10.1016/j.gie.2014.06.035
62. Barbieri LA, Hassan C, Rosati R, Romario UF, Correale L, Repici A. Systematic review and meta-analysis: efficacy and safety of POEM for achalasia. United European Gastroenterology Journal. 2015;3(4):325–334. doi:10.1177/2050640615581732
63. Nabi Z, Reddy DN, Ramchandani M. Adverse events during and after per-oral endoscopic myotomy: prevention, diagnosis, and management. Gastrointest Endosc. 2018;87(1):4–17. doi:10.1016/j.gie.2017.09.029
64. Pannu D, Yang D, Abbitt PL, Draganov PV. Prospective evaluation of CT esophagram findings after peroral endoscopic myotomy. Gastrointest Endosc. 2016;84(3):408–415. doi:10.1016/j.gie.2016.02.022
65. Akintoye E, Kumar N, Obaitan I, Alayo QA, Thompson CC. Peroral endoscopic myotomy: a meta-analysis. Endoscopy. 2016. doi:10.1055/s-0042-114426
66. Werner Y. TN-G, 2017 undefined. early adverse events of per-oral endoscopic myotomy. Elsevier; 2017. Available from: https://www.sciencedirect.com/science/article/pii/S0016510716305399.
67. Haito-Chavez Y, Inoue H, Beard KW, et al. Comprehensive analysis of adverse events associated with per oral endoscopic myotomy in 1826 patients: an international multicenter study. Am J Gastroenterol. 2017;112(8):1267–1276. doi:10.1038/ajg.2017.139
68. Wang Y, Liu ZQ, Xu MD, et al. Clinical and endoscopic predictors for intraprocedural mucosal injury during per-oral endoscopic myotomy. Gastrointest Endosc. 2019;89(4):769–778. doi:10.1016/j.gie.2018.09.003
69. Kumbhari V, Familiari P, Bjerregaard NC, et al. Gastroesophageal reflux after peroral endoscopic myotomy: a multicenter case-control study. Endoscopy. 2017;49(7):634–642. doi:10.1055/s-0043-105485
70. Repici A, Fuccio L, Maselli R, et al. GERD after per-oral endoscopic myotomy as compared with Heller’s myotomy with fundoplication: a systematic review with meta-analysis. Gastrointest Endosc. 2018;87(4):934–943.e18. doi:10.1016/j.gie.2017.10.022
71. Schlottmann F, Luckett DJ, Fine J, Shaheen NJ, Patti MG. Laparoscopic Heller Myotomy Versus Peroral Endoscopic Myotomy (POEM) for achalasia: a systematic review and meta-analysis. Ann Surg. 2018;267(3):451–460. doi:10.1097/SLA.0000000000002311
72. Sanaka MR, Thota PN, Parikh MP, et al. Peroral endoscopic myotomy leads to higher rates of abnormal esophageal acid exposure than laparoscopic Heller myotomy in achalasia. Surg Endosc. 2019;33(7):2284–2292. doi:10.1007/s00464-018-6522-4
73. Familiari P, Greco S, Gigante G, et al. Gastroesophageal reflux disease after peroral endoscopic myotomy: analysis of clinical, procedural and functional factors, associated with gastroesophageal reflux disease and esophagitis. Dig Endosc. 2016;28(1):33–41. doi:10.1111/den.12511
74. Shiwaku H, Inoue H, Sasaki T, et al. A prospective analysis of GERD after POEM on anterior myotomy. Surg Endosc. 2016;30(6):2496–2504. doi:10.1007/s00464-015-4507-0
75. Kahrilas PJ, Katzka D, Richter JE. Clinical practice update: the use of per-oral endoscopic myotomy in achalasia: expert review and best practice advice from the AGA institute. Gastroenterology. 2017;153(5):1205–1211. doi:10.1053/j.gastro.2017.10.001
76. Werner YB, Hakanson B, Martinek J, et al. Endoscopic or surgical myotomy in patients with idiopathic Achalasia. N Engl J Med. 2019;381(23):2219–2229. doi:10.1056/NEJMoa1905380
77. Marano L, Pallabazzer G, Solito B, et al. Surgery or peroral esophageal myotomy for Achalasia: a systematic review and meta-analysis. Med (United States). 2016;95(10). doi:10.1097/MD.0000000000003001
78. Ponds FA, Fockens P, Lei A, et al. Effect of peroral endoscopic myotomy vs pneumatic dilation on symptom severity and treatment outcomes among treatment-naive patients with achalasia: a randomized clinical trial. JAMA. 2019;322(2):134–144. doi:10.1001/jama.2019.8859
79. Aiolfi A, Bona D, Riva CG, et al. Systematic review and Bayesian network meta-analysis comparing laparoscopic Heller myotomy, pneumatic dilatation, and peroral endoscopic myotomy for esophageal Achalasia. J Laparoendosc Adv Surg Tech. 2020;30(2):1–9. doi:10.1089/lap.2019.0432
80. Zheng Z, Zhao C, Su S, et al. Peroral endoscopic myotomy versus pneumatic dilation - Result from a retrospective study with 1-year follow-up. Z Gastroenterol. 2019;57(3):304–311. doi:10.1055/a-0821-7232
81. Miller HJ, Neupane R, Fayezizadeh M, Majumder A, Marks JM. POEM is a cost-effective procedure: cost-utility analysis of endoscopic and surgical treatment options in the management of achalasia. Surg Endosc. 2017;31(4):1636–1642. doi:10.1007/s00464-016-5151-z
82. Greenleaf EK, Winder JS, Hollenbeak CS, Haluck RS, Mathew A, Pauli EM. Cost-effectiveness of per oral endoscopic myotomy relative to laparoscopic Heller myotomy for the treatment of achalasia. Surg Endosc. 2018;32(1):39–45. doi:10.1007/s00464-017-5629-3
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

