Back to Journals » Nature and Science of Sleep » Volume 14
Peripheral Iron Metabolism is Associated with Leg Movements on Polysomnography but Not with the Severity of Restless Legs Syndrome or Its Impact on Patients
Authors Wang T, Xu J, Xu Q, Zhao R, Pan L, Zhu D, Pan Y, Chen L, Lou G, Xu X , Wang J , Zhang L
Received 2 July 2022
Accepted for publication 23 September 2022
Published 13 October 2022 Volume 2022:14 Pages 1829—1842
DOI https://doi.org/10.2147/NSS.S378970
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Ahmed BaHammam
Tiantian Wang,1– 3 Jiahui Xu,2,4 Qinglin Xu,2,4 Rui Zhao,5 Liuqing Pan,2 Danyan Zhu,3 Yu Pan,2 Lehui Chen,6 Guodong Lou,2,5 Xiaoye Xu,7 Jin Wang,4 Lisan Zhang2,4
1Department of Pharmacy, Xiasha Campus, Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University, Hangzhou, People’s Republic of China; 2Department of Neurology/Center for Sleep Medicine, Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University, Hangzhou, People’s Republic of China; 3Institute of Pharmacology and Toxicology, College of Pharmaceutical Science, Zhejiang University, Hangzhou, People’s Republic of China; 4Department of Neurology, Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University, Hangzhou, People’s Republic of China; 5Department of Pharmacy, Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University, Hangzhou, People’s Republic of China; 6Department of Internal Medicine, Hangzhou Wuyunshan Hospital, Hangzhou, People’s Republic of China; 7Department of Nursing, Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University, Hangzhou, People’s Republic of China
Correspondence: Jin Wang, Department of Neurology, Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University, 3 Qingchundong Road, Hangzhou, Zhejiang Province, 310016, People’s Republic of China, Tel +86-135-1681-8933, Email [email protected] Lisan Zhang, Department of Neurology/Center for Sleep Medicine, Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University, 3 Qingchundong Road, Hangzhou, Zhejiang Province, 310016, People’s Republic of China, Tel +86-138-0575-2614, Email [email protected]
Purpose: This study investigated the associations of peripheral iron status with different manifestations of restless legs syndrome (RLS), including leg movements (LMs) on polysomnography (PSG), disease severity, and impact on patients.
Patients and Methods: In this cross-sectional study, 108 patients with RLS were enrolled at Sir Run Run Shaw Hospital’s Center for Sleep Medicine. Demographic information, disease characteristics, RLS severity, and impact on patients were assessed through a semi-structured questionnaire. Peripheral iron indicators [serum ferritin, iron, and transferrin concentrations; unsaturated iron-binding capacity (UIBC) and total iron-binding capacity (TIBC); transferrin saturation (TSAT)] were measured following PSG to assess sleep stages, respiratory events, microarousals and LM parameters. Data from patients with and without ferritin concentration < 50 μg/L were compared in crude analyses, and Spearman correlations of other iron indicators with RLS data were examined. An ordinal logistic regression model was used to adjust for age, sex, body mass index, years of education, age at the time of RLS onset, prior treatment (yes/no), C-reactive protein (CRP)/hemoglobin level, total sleep time and apnea-hypopnea index.
Results: Multivariate analysis showed that periodic LMs during sleep (PLMS) and other LM parameters were significantly associated with a ferritin concentration < 50 μg/L, UIBC, TIBC, and serum transferrin concentration, but not serum iron or TSAT. By contrast, the severity and impact of RLS were not associated with a ferritin concentration < 50 μg/L or other peripheral iron indicators in the multivariate model.
Conclusion: In this study, peripheral iron status was associated mainly with motor components (LMs on PSG) rather than sensory components (severity and impact of RLS) after adequately controlling for potential confounders, such as CRP and hemoglobin levels. Commonly used peripheral iron metabolism indicators may therefore not be ideal biomarkers of RLS severity or impact on patients.
Keywords: restless legs syndrome, peripheral iron metabolism, polysomnography, leg movements, severity, impact
Statement of Significance
Although iron deficiency contributes to RLS, the relationship between peripheral iron metabolism and RLS is controversial. The present study investigated the associations of peripheral iron status with different manifestations of RLS and observed the following. In patients with RLS, commonly used peripheral iron metabolism indicators were mainly related to motor rather than sensory components of RLS, suggesting that abnormal peripheral iron metabolism is not a risk factor for RLS severity or a negative impact on patients, and that the two clinical presentations of RLS are likely independent of each other. Leg movement parameters were associated with a ferritin concentration < 50 µg/L, UIBC, TIBC and the serum transferrin concentration, but not with serum iron or TSAT. Complex iron metabolism, involving storage and transport processes, may underlie the motor components of RLS. (3) As well as PLMS, other LMs were related to peripheral iron metabolism. PLMS/LMs during wakefulness and arousal were not associated with peripheral iron measures. Overall, our study demonstrates that peripheral iron metabolism is involved in several complex RLS mechanisms. Further studies are needed to determine how peripheral iron status participates in the pathophysiology of RLS.
Introduction
Restless legs syndrome (RLS) is a common sensorimotor disorder characterized by a prominent circadian pattern and a rest-induced, movement-responsive, mostly nocturnal urge to move the legs.1 Brain iron deficiency is the key initial pathobiological factor in RLS; it induces the hypoadenosinergic, hyperglutamatergic, and hyperdopaminergic states involved in the sensorimotor signs and arousal components of RLS.1 The clinical expression of RLS is variable and may depend on genetic, environmental, or medical factors.2 However, in a systematic review, only iron deficiency and kidney disease increased the prevalence of RLS.3 Based on clinical research,4,5 iron deficiency is currently recognized as an independent risk factor for RLS, and iron supplementation has effectively treated some forms of RLS.6–9 Additionally, based on imaging and postmortem findings1 as well as genome-wide association studies10−12, the pathophysiology of RLS is linked to iron homeostasis.11,13
As the current RLS treatment guidelines14–16 recommend iron treatment for patients with low peripheral iron levels, the systemic iron parameters of patients with RLS should be measured routinely. To examine the iron status of patients with RLS, initial and periodic measurement of the serum iron, transferrin, and ferritin concentrations; total iron-binding capacity (TIBC); and transferrin saturation (TSAT) is recommended.17 Ferritin is a circulating iron storage protein and acute-phase reactant; thus, the C-reactive protein (CRP) level or erythrocyte sedimentation rate should be considered when interpreting the ferritin concentration.17
Although iron deficiency has been considered an independent risk factor for RLS, the association is controversial. Leung et al18 published a review of the association of iron deficiency with RLS based on 74 studies and identified gaps in the research. Although most of the studies found a positive association, this was not seen in some cross-sectional (10/25) and cohort studies (4/5).18 Moreover, the CRP level was measured together with the ferritin concentration in only three studies19–21 and iron deficiency was not associated with RLS in any of them. In addition to potential cofounders such as CRP, these contradictory results regarding the association of iron deficiency with RLS may be due to the use of univariate analysis, small sample sizes,22 and non-linear relationships.23 To date, the effects of the serum iron and transferrin concentrations, TIBC, and TSAT on RLS have received much less attention. A few studies demonstrated that iron ions, transferrin, soluble transferrin receptor concentrations, and TSAT were not significantly different between patients with RLS and Healthy controls.24–26 Hence, the generalizability of the relationship between peripheral iron metabolism and RLS is limited.
Periodic leg movements during sleep (PLMS) are defined as movements in which at least four LMs take place, with intervals of 5–90 s between them.27 However, LMs during sleep also include other movements not meeting this requirement or separated by interval > 90s. PLMS may therefore differ from other types of LM in terms of its specific characteristics and duration, as well as other features such as high sensitivity to dopamine agonists, reduced frequency at night, and associations with diseases other than RLS.28 As LMs have yet been thoroughly assessed, the associations of PLMS and LMs with peripheral iron status remain to be determined.
The aim of this study was to investigate the associations of various peripheral iron parameters with LMs on polysomnography (PSG), RLS severity, and the impact on patients, after adjusting for confounding variables. As well as the serum ferritin concentration (the only indicator of iron-status measured in most studies), this study analyzed several other indicators, including serum iron and transferrin concentrations, TIBC, and TSAT. Other categories of LM in addition to PLMS were also examined. Moreover, patient demographics, symptom characteristics, RLS severity, on the impact on patients, and polysomnographic data were assessed.
Materials and Methods
Patients
We continuously recruited patients with RLS to this study conducted at the Center for Sleep Medicine, Sir Run Run Shaw Hospital, Zhejiang University School of Medicine, from March 2019 to December 2020. According to the International RLS Study Group,29 five essential diagnostic criteria for RLS are uncomfortable and unpleasant sensations in the limbs usually causing an urge to move (mainly in the legs), initiation or worsening of these symptoms when at rest or inactive, partial or complete remission of the symptoms while activity continues, the occurrence or increased severity of symptoms at night, and the absence of another condition explaining the symptoms.
Written informed consent was obtained from all individuals included in the study. This study was approved by the Institutional Review Board of Sir Run Shaw Hospital (permit number: 20190226–9), and all procedures involving human subjects adhered to the Helsinki Declaration as revised in 1989. The study was registered in Chinese Clinical Trial Registry (clinical trial registration number: ChiCTR2000040784).
Clinical Assessments
A neurologist with expertise in sleep medicine administered a semi-structured questionnaire to the study participants to collect information on their demographic characteristics, symptom characteristics (age at time of RLS onset, duration of RLS, family history of RLS), and medical histories/co-morbidities. Current RLS medication use was recorded, and levodopa equivalent doses were calculated for patients receiving dopaminergic therapy.30 Augmentation was assessed using the criteria of the Max Planck Institute.31
Although not life-threatening, patients with RLS often have compromised health and poor quality of life. Thus, comprehensive clinical assessment is essential to fully understand the impacts of RLS on patients. In this study patients were assessed in terms of sleep quality, daytime sleepiness, fatigue, quality of life, emotional state (depression/anxiety), and cognitive function using the following validated scales: the International Restless Legs Syndrome Study Group Severity Scale (IRLS),32 Pittsburgh Sleep Quality Index (PSQI),33 Epworth Sleepiness Scale (ESS),34 Chalder Fatigue Scale (CFS),35 Medical Outcomes Study 36-item short-form health survey (SF-36),36 Beck Depression Inventory-13 (BDI-13),37 Beck Anxiety Inventory (BAI),38 Montreal Cognitive Assessment (MoCA),39 and Mini-Mental Status Examination (MMSE).40
Comorbidities
Given the complex etiology of RLS, which likely involves environmental and genetic interactions, it can occur in isolation or with comorbidities.41 Only iron deficiency anemia and kidney disease have been identified as factors increasing the prevalence of RLS, although it may be associated with other comorbidities such as cardiovascular disease, arterial hypertension, diabetes, migraine and Parkinson disease.3 Therefore, patients were questioned about these diseases when their demographic information was collected (Table 1) (Pregnancy, kidney disease, migraine, and Parkinson’s disease were not reported by any of the patients).
 |
Table 1 Comparison of Demographic and Disease Characteristics Between RLS Patients with and without a Ferritin Concentration < 50 µg/L |
Because the sleep scales used in this study were not specific to RLS, participants with other non-RLS sleep disorders according to third edition of the International Classification of Sleep Disorder42 were included in the analysis (Table 1) (No patient had been diagnosed with central disorders of hypersomnolence, circadian rhythm sleep-wake disorders, sleep-related movement disorders (except RLS), parasomnias, or other sleep disorders).
Polysomnography Recordings
PSG was performed using a Trackit 32-channel PSG monitor (Nihon Kohden Corporation, Tokyo, Japan), which has six electroencephalogram leads, two electro-oculograms, one chin electromyogram, and an electrocardiogram. Nasal cannula/pressure transducer, mouth thermistor, chest and abdominal bands, and pulse oximeter data were obtained to monitor respiration. Similarly, PLMS/LMs were recorded by surface electromyogram electrodes placed on the anterior tibialis muscles.
Measurements of sleep stage, respiratory events, microarousals, and LM parameters (such as LM events and PLMS) were based on the criteria of the American Academy of Sleep Medicine (version 2.4).27 All of the above parameters were analyzed by at least one physician specializing in sleep medicine.
The PLMS arousal index is calculated as flows: PLMS with arousals × 60 / total sleep time (TST, in min). The PLMS sequence index is calculated as the number of PLM series × 60 / TST (in min). PLMS sequence duration is calculated as the total duration of PLMS (in min) × 60 / TST (in min). The LM index with microarousal is calculated as LM with microarousals × 60 / TST (in min). The LM index without arousal is calculated as the total LM with microarousal × 60 / TST (in min).
No patients took RLS medications on the night of the PSG examination.
Laboratory Measurements
Antecubital venous blood samples were obtained from patients between 6:00 and 8:00 a.m. after an overnight fast following standardized procedures. Hemoglobin and CRP levels were measured. Peripheral iron metabolism was evaluated by measuring the serum ferritin, iron, and transferrin concentrations, unsaturated iron-binding capacity (UIBC), TIBC, and TSAT.
Serum ferritin concentrations were measured by an electrochemiluminescence assay (Roche Diagnostics, Mannheim, Germany). Serum iron concentrations and TSAT were determined using an iron/UIBC kit (Roche Diagnostics). The concentration of transferrin was determined by immuno-turbidimetry using a transferrin assay kit (332028; Shanghai Jiemen Bio-Technology Co. Ltd., Shanghai, China).
Statistical Analysis
Data on participants’ demographics, disease characteristics, RLS severity and impact on patients, and polysomnographic parameters are presented as means ± standard deviations for normally distributed variables, medians (interquartile ranges) for non-normally distributed variables, and frequencies (percentages) for categorical variables. These variables were analyzed using independent t-tests, non-parametric tests, and chi-squared tests, respectively.
Associations of participants’ peripheral iron status with RLS severity and impact on patients, as well as LM parameters, were examined. A crude comparative analysis was employed to assess ferritin deficiency (concentration < 50 µg/L), and Spearman correlation analysis was applied to examine the other iron-status indicators. Variables associated with LM parameters (at P < 0.3) and disease severity/impact (at P < 0.15) were included in an ordinal logistic regression model adjusted for age, sex, body mass index (BMI), years of education, age at RLS onset, prior treatment (yes/no), CRP/hemoglobin level, TST and the apnea-hypopnea index (AHI) to obtain adjusted odds ratios (ORs) for indicators of peripheral iron status; non-normally distributed continuous independent variables were grouped into quartiles. When the parallel regression assumption was rejected, we used binary logistic regression to analyze the data. All tests were two-sided and the significance level was set to P < 0.05. Statistical analyses were performed using IBM SPSS Statistics 25.0 (IBM Corp., Armonk, NY, USA).
The original LM data for six patients were lost. They were replaced using multiple imputations, and the averages of four imputation values were included in the analysis.
Results
Characteristics of Patients with RLS
We analyzed data from 108 of the 119 participants enrolled in this study. Eleven participants were excluded because their symptoms mimicked RLS (n = 6) or they did not have RLS, nor any mimicking symptoms (n = 5). In 32 of the 108 patients the ferritin concentration was < 50 µg/L and in 76 patients it was ≥ 50 µg/L. Among the 107 participants examined for associations of peripheral iron status with LM parameters, one patient refused PSG. The average age of the 108 patients with RLS was 51.1 ± 14.8 years; 73 (67.6%) patients were female, the average age at the time of RLS symptom onset was 39.7 ± 17.2 years and RLS was untreated in 66 (61.1%) patients.
The demographic and disease characteristics of patients with and without ferritin deficiency are shown in Table 1. The levodopa-equivalent dose for commonly used agents was calculated according to a previously reported protocol.33 Patients with ferritin deficiency were more likely to be female (χ2 = 11.013, P = 0.001), were younger (t = –3.077, P = 0.003), and had more years of education (z = –2.474, P = 0.013) and a lower BMI (z = –2.870, P = 0.004) compared with those without ferritin deficiency.
Patients with ferritin deficiency had longer TSTs (z = −2.218, P = 0.027), were more likely to have an AHI < 5 (χ2 = 4.537, P = 0.033), and had lower 3% oxygen desaturation indices than patients without ferritin deficiency (z = −2.429, P = 0.015; Table 2).
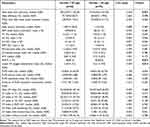 |
Table 2 Polysomnography in RLS Patients with and without a Ferritin Concentration < 50 µg/L |
Association of Peripheral Iron Measures with PSG Leg Movement Parameters
In the Multivariate logistic regression analyses, ferritin deficiency was associated with the PLMS index [odds ratio (OR) = 3.074; 95% confidence interval (CI), 1.266–7.456; P = 0.013], PLMS sequences index (OR = 3.655; 95% CI, 1.484–9.007; P = 0.005), duration of PLMS sequences (OR = 3.238; 95% CI, 1.334–7.870; P = 0.009), LM index during N2 sleep (OR = 3.579; 95% CI, 1.458–8.785; P = 0.005), and LM index during N3 sleep (OR = 3.099; 95% CI, 1.256–7.645; P = 0.014) (Table 3).
 |
Table 3 Associations of Leg Movement Parameters on Polysomnography with a Ferritin Concentration < 50 µg/L in RLS Patients According to Ordinal Logistic Regression Models |
LMs during N2 sleep were related to UIBC (r = 0.221, P = 0.022) and TIBC (r = 0.229, P = 0.018); no other correlations were significant in Spearman’s correlation analyses(data not shown).
After adjustment for potential confounders, the UIBC was related significantly to the PLMS sequences index (OR = 1.046; 95% CI, 1.003–1.091; P = 0.035), total LM index (OR = 1.052; 95% CI, 1.008–1.099; P = 0.021), and LM index without arousal (OR = 1.050; 95% CI, 1.005–1.096; P = 0.028; Table 4). The TIBC was related significantly to the PLMS index (OR = 1.062; 95% CI, 1.009–1.117; P = 0.022), PLMS sequences index (OR = 1.055; 95% CI, 1.002–1.111; P = 0.041), duration of PLMS sequences (OR = 1.070; 95% CI, 1.017–1.127; P = 0.010), LM index during N2 sleep (OR = 1.070; 95% CI, 1.015–1.127; P = 0.011) and LM index during REM sleep (OR = 1.084; 95% CI, 1.027–1.143; P = 0.003) (Table 5). Serum transferrin concentration was associated with the duration of PLMS sequences (OR = 2.980; 95% CI, 1.025–8.654; P = 0.045), the LM index during N2 sleep (OR = 3.607; 95% CI, 1.206–10.794; P = 0.022), and the LM index during REM sleep (OR = 4.450; 95% CI, 1.465–13.504; P = 0.008) (Table 6). Neither the serum iron concentration (Table 7) nor the TSAT (Table 8) was associated with any of the PSG LM parameters.
 |
Table 4 Associations of Unsaturated Iron Binding Capacity with Leg Movement Parameters on Polysomnography in RLS Patients According to Ordinal Logistic Regression Models |
 |
Table 5 Associations of Total Iron-Binding Capacity with Leg Movement Parameters on Polysomnography in RLS Patients According to Ordinal Logistic Regression Models |
 |
Table 6 Associations of Serum Transferrin with Leg Movement Parameters on Polysomnography in RLS Patients According to Ordinal Logistic Regression Models |
 |
Table 7 Associations of Serum Iron Level with Leg Movement Parameters on Polysomnography in RLS Patients According to Ordinal Logistic Regression Models |
 |
Table 8 Associations of Transferrin Saturation with Leg Movement Parameters on Polysomnography Models in RLS Patients According to Ordinal Logistic Regression Models |
Peripheral Iron Measures are Not Associated with RLS Severity or Impact
Comparison of the severity/impact of RLS between patients with and without ferritin deficiency revealed no significant difference in the IRLS, PSQI, ESS, CFS, SF-36, BDI-13, BAI, MoCA, or MMSE score (all P > 0.05), but there was a significant difference in the MoCA recall score (z = –2.009, P = 0.045; Supplementary Table 1). In the Spearman correlation analysis, other indicators of peripheral iron status were not related to the severity/impact of RLS, except the serum iron concentration, which was associated with SF-36 physical function (r = 0.198, P = 0.040; data not shown).
The severity and impact of RLS were not significantly associated with ferritin deficiency (Table 9). The relationships of other iron-status indicators and RLS severity and impact were also non-significant after adjustment for confounders (Table 10).
 |
Table 9 Associations of Severity and Impact of RLS with a Ferritin Concentration < 50 µg/L According to Ordinal Logistic Regression Models |
 |
Table 10 Associations of Severity and Impacts of RLS with Other Peripheral Iron Status Indicators According to Ordinal Logistic Regression Models |
Discussion
Our study showed that a ferritin concentration < 50 µg/L, UIBC, TIBC and the serum transferrin concentration, but not the serum iron concentration or TSAT, were associated with most LMs; peripheral iron indicators were not related to RLS severity or impacts.
The association of peripheral iron indicators with LMs in patients with RLS in this study was surprising. Most LMs were not related significantly to iron metabolism in unadjusted analyses, but the associations changed in our multivariate logistic regression model. On PSG, patients with ferritin deficiency were about three times more likely to have higher PLMS and LM index values during N2 and N3 sleep than patients with a ferritin concentration ≥ 50 µg/L. A similar association was found between low ferritin concentrations and more PLMS by Li et al, independent of genetic polymorphisms, in a general population of older adults, implying that low iron stores play a role in the expression of these phenotypes.43 However, in a study of Korean patients with RLS,44 there was no correlation between the ferritin concentration and PLMS in logistic regression models. However, the credibility of the results is undermined by the lack of adjustment for the CRP level. Stefansson et al11 identified a common variant in an intron of BTBD9 on chromosome 6p21.2, as a genetic determinant of PLMS, which correlated inversely with serum ferritin levels, indicating that iron metabolism was involved in the pathogenesis of PLMS.
In this study, ferritin deficiency, the serum transferrin concentration, TIBC, and UIBC, but not the serum iron concentration or TSAT, were associated with certain LM parameters. The transferrin concentration serves as a proxy for the TIBC; it decreases as blood iron levels increase and increases with iron deficiency.17 Peripheral iron is transmitted to the brain across the blood-brain barrier. During this process, transferrin, as a receptor-mediated transporter, plays a key role in iron metabolism and maintaining iron homeostasis.45,46 Magnetic susceptibility in the substantia nigra was significantly associated with PLMS measures, suggesting a link between brain iron deficiency and PLMS.47 Earley et al48 reported that the serum ferritin value was associated with the ferritin concentration in the cerebrospinal fluid. Compared with the control group, there was a significant reduction in the slope of the linear regression line for RLS patients. We therefore speculate that iron deficiency in the substantia nigra is more severe in RLS patients with more PLMS, in whom iron transport across the blood-brain barrier is altered. Serum iron represents the level of circulating iron, ie, of iron bound to transferrin. TSAT is the ratio of total iron and TIBC.17 Serum iron levels are highly variable and may be affected by several factors, such as diet, stress, and sleep,48 which could explain the lack of a significant correlation between serum iron, TSAT and LM parameters. Therefore, complex iron metabolism involving iron storage and transport may contribute to the abnormal LMs seen in RLS.
RLS severity and impact on patients were not related to peripheral iron indicators, implying that abnormal peripheral iron metabolism may not be a risk factor for RLS. Brain iron insufficiency and the iron–dopamine interaction play important roles in the etiology of RLS.49 Recent studies of the mechanism of peripheral iron metabolism in RLS have focused on lymphocytes,50 extracellular vesicles,51 and mitochondrial dysfunction25 and suggested that abnormal peripheral iron transport, rather than iron storage levels, is the mechanism underlying RLS. During the uptake of iron by the brain, the blood-brain barrier not only serves as a channel for iron transport, but also regulates the iron transport process.52–54 However, in a blood-brain barrier model there was no correlation between the serum ferritin concentration and iron transport.54 Other indicators, such as hepcidin55,56 have been investigated and merit further exploration in patients with RLS. We conclude that the peripheral iron indicators measured in common clinical practice should be interpreted carefully, and that ferritin may not be the best RLS biomarker.
Why were peripheral iron parameters in our patients with RLS related to motor components (ie, LMs on PSG) but not sensory components (RLS severity and impact on patients)? Although PLMS occur in > 80% of patients with RLS2,29,44,57 and support the diagnosis of this syndrome,2,29 the relationship between PLMS and RLS is controversial.44,58 The motor and sensory symptoms of RLS may be separate but loosely linked, since the PLMS index alone does not reliably predict the diagnosis of RLS in children or adolescents59 and the phenotypical presentation of RLS may differ by sex22 (with women experiencing more sensory symptoms than men, who have more motor symptoms). PLMS may also be an endophenotype of RLS10 and PLMS may be a biomarker60 or genetic risk marker of RLS.61 Furthermore, the pathophysiology of LMs may not generalize to idiopathic RLS.11,62–64 The characteristic “urge to move” may be due to lesions in ascending sensory pathways or thalamocortical circuits, and may not be accompanied by PLMS.65 Our study and previous ones together indicate that the motor and sensory features of RLS are two different presentations of a common basic neurologic disorder.66 As a complex disease with multiple manifestations and undefined mechanisms, the etiology of RLS may involve genetic defects in brain iron homeostasis and developmental abnormalities in cortico-striatal-thalamic-cortical circuits related to hypoadenosinergic, hyperglutamatergic, and hyperdopaminergic states.1 It is therefore likely that the different clinical features of RLS are modulated by multiple neurotransmitter systems and downstream signaling pathways.
The classical PLMS index does not appear to be specific enough for the diagnosis of RLS or assessment of its clinical significance.67 When used alone, the PLMS index is insufficient for characterizing the nature and structure of LM activity during sleep,67 although the duration and number of PLM sequences are associated with sleep disturbances in patients with RLS.68,69 In this study, the duration of PLMS sequences was measured. The ferritin concentration, UIBC, TIBC, and serum transferrin concentration were all related to at least one PLMS measurement. In Dauvilliers et al,56 only the hepcidin level and hepcidin/ferritin ratio were measured, and both correlated positively with PLM during both sleep and wakefulness. Consequently, our study therefore adds to the limited knowledge regarding relationship between peripheral iron status and PLMS. In addition to PLMS, total LMs and their distribution in different sleep stages were analyzed. No peripheral iron measures were related to LM indexes during N1 sleep, while TIBC and serum transferrin and ferritin concentrations were all associated with the LM index during N2 sleep. We also found that serum ferritin and transferrin correlated with LMs during N3 and REM sleep, respectively. However, as the relationship between peripheral iron status and LMs was not assessed in previous studies, this result should be interpreted with caution and confirmed in future studies. It should be noted that none of the peripheral iron measures were related to PLM/LMs during wakefulness or arousal. Given the association of peripheral iron measures with PLM/LMs in sleep, we speculate that distinct biological mechanisms underlie the coupling of arousal and motor systems. First, dopamine agonists may have little impact on arousals, despite strongly reducing PLMS, and a targeted pharmaceutical strategy may be able to separate PLMS from arousal events.69 Second, different neurotransmitters may be involved in PLMS and short-interval LM wakefulness (and arousal).70 Third, a hierarchy has been described in the arousal response, from autonomic activation to cortical arousals and PLMS.71 The above findings support the notion that the complex mechanisms subtending the fluctuating arousal and motor systems may partly explain the lack of an association between peripheral iron measures and PLMs/LMs during wakefulness and arousal.
Our study had several limitations. First, its cross-sectional design and observational nature prevented determination of the causal relationship between peripheral iron metabolism and RLS. Second, the participants underwent only one night of PSG, such that night-to-night variability in LM parameters could not be captured, although this issue might have been mitigated by the inclusion of a large number of patients. Third, there may have been bias in patient selection and unmeasured confounding factors. For patients with low educational attainment, some self-report scales were completed orally, such that an influence of dialects cannot be excluded. Fourth, the population under study was relatively small, although it was well characterized clinically and through a PSG assessment.
Conclusion
In conclusion, this study examined the association of peripheral iron metabolism with RLS and demonstrated that peripheral iron status was associated mainly with the motor rather than sensory components of RLS, indicating that, in RLS, the metabolic factors potentially underlying sensory symptoms differ from those underlying movement symptoms. The findings of this study strengthen the idea that the commonly used peripheral iron metabolism indicators may not be ideal biomarkers of RLS severity and impact on patients. Considering the key role of brain iron deficiency in the mechanism of RLS, further research on other iron metabolism indicators is an essential next step in confirming the role of iron metabolism in RLS.
Data Sharing Statement
The datasets analyzed in the current study are available from the corresponding author on reasonable request.
Acknowledgments
Abstracts of this study were displayed for colleagues at the 3rd Congress of the Asia Society of Sleep Medicine (2021). The authors gratefully thank Professor Fang Guo for helpful suggestions.
Disclosure
The authors declare that there are no conflicts of interest related to this work. This research was supported by the Medical Health Science and Technology Project of Zhejiang Provincial Health Commission under award number 2020383055/2020KY164.
References
1. Ferré S, García-Borreguero D, Allen RP, Earley CJ. New insights into the neurobiology of restless legs syndrome. Neuroscientist. 2018;25(2):113–125. doi:10.1177/1073858418791763
2. Garcia-Borreguero D, Cano-Pumarega I. New concepts in the management of restless legs syndrome. BMJ. 2017;356:j104. doi:10.1136/bmj.j104
3. Trenkwalder C, Allen R, Högl B, Paulus W, Winkelmann J. Restless legs syndrome associated with major diseases: a systematic review and new concept. Neurology. 2016;86(14):1336–1343. doi:10.1212/WNL.0000000000002542
4. Allen RP, Auerbach S, Bahrain H, Auerbach M, Earley CJ. The prevalence and impact of restless legs syndrome on patients with iron deficiency anemia. Am J Hematol. 2013;88(4):261–264. doi:10.1002/ajh.23397
5. Frauscher B, Gschliesser V, Brandauer E, et al. The severity range of restless legs syndrome (RLS) and augmentation in a prospective patient cohort: association with ferritin levels. Sleep Med. 2009;10(6):611–615. doi:10.1016/j.sleep.2008.09.007
6. Cho YW, Allen RP, Earley CJ. Clinical efficacy of ferric carboxymaltose treatment in patients with restless legs syndrome. Sleep Med. 2016;25:16–23. doi:10.1016/j.sleep.2016.06.021
7. Allen RP, Adler CH, Du W, Butcher A, Bregman DB, Earley CJ. Clinical efficacy and safety of IV ferric carboxymaltose (FCM) treatment of RLS: a multi-centred, placebo-controlled preliminary clinical trial. Sleep Med. 2011;12(9):906–913. doi:10.1016/j.sleep.2011.06.009
8. Macher S, Herster C, Holter M, et al. The effect of parenteral or oral iron supplementation on fatigue, sleep, quality of life and restless legs syndrome in iron-deficient blood donors: a secondary analysis of the ironwoMan RCT. Nutrients. 2020;12(5):1313. doi:10.3390/nu12051313
9. Wang J, O’Reilly B, Venkataraman R, Mysliwiec V, Mysliwiec A. Efficacy of oral iron in patients with restless legs syndrome and a low-normal ferritin: a randomized, double-blind, placebo-controlled study. Sleep Med. 2009;10(9):973–975. doi:10.1016/j.sleep.2008.11.003
10. Winkelman JW. Periodic limb movements in sleep - endophenotype for restless legs syndrome? N Engl J Med. 2007;357(7):703–705. doi:10.1056/NEJMe078129
11. Stefansson H, Rye DB, Hicks A, et al. A genetic risk factor for periodic limb movements in sleep. N Engl J Med. 2007;357(7):639–647. doi:10.1056/NEJMoa072743
12. Schormair B, Zhao C, Bell S, et al. Identification of novel risk loci for restless legs syndrome in genome-wide association studies in individuals of European ancestry: a meta-analysis. Lancet Neurol. 2017;16(11):898–907. doi:10.1016/S1474-4422(17)30327-7
13. Catoire H, Dion PA, Xiong L, et al. Restless legs syndrome-associated MEIS1 risk variant influences iron homeostasis. Ann Neurol. 2011;70(1):170–175. doi:10.1002/ana.22435
14. Winkelman JW, Armstrong MJ, Allen RP, et al. Practice guideline summary: treatment of restless legs syndrome in adults: report of the guideline development, dissemination, and implementation subcommittee of the American Academy of neurology. Neurology. 2016;87(24):2585–2593. doi:10.1212/WNL.0000000000003388
15. Winkelmann J, Allen RP, Hogl B, et al. Treatment of restless legs syndrome: evidence-based review and implications for clinical practice (revised 2017) (section sign). Mov Disord. 2018;33(7):1077–1091. doi:10.1002/mds.27260
16. Allen RP, Picchietti DL, Auerbach M, et al. Evidence-based and consensus clinical practice guidelines for the iron treatment of restless legs syndrome/Willis-Ekbom disease in adults and children: an IRLSSG task force report. Sleep Med. 2018;41:27–44. doi:10.1016/j.sleep.2017.11.1126
17. Garcia-Malo C, Miranda C, Peralta S, Cano-Pumarega I, Ponte S, Garcia-Borreguero D. Iron replacement therapy in restless legs syndrome. Curr Treat Option Neurol. 2020;22(114):1–6. doi:10.1007/s11940-020-0617-7
18. Leung W, Singh I, McWilliams S, Stockler S, Ipsiroglu OS. Iron deficiency and sleep – a scoping review. Sleep Med Rev. 2020;51:101274. doi:10.1016/j.smrv.2020.101274
19. Kim KW, Yoon IY, Chung S, et al. Prevalence, comorbidities and risk factors of restless legs syndrome in the Korean elderly population - results from the Korean longitudinal study on health and aging. J Sleep Res. 2010;19(1 Pt 1):87–92. doi:10.1111/j.1365-2869.2009.00739.x
20. Benediktsdottir B, Janson C, Lindberg E, et al. Prevalence of restless legs syndrome among adults in Iceland and Sweden: lung function, comorbidity, ferritin, biomarkers and quality of life. Sleep Med. 2010;11(10):1043–1048. doi:10.1016/j.sleep.2010.08.006
21. Berger K, von Eckardstein A, Trenkwalder C, Rothdach A, Junker R, Weiland SK. Iron metabolism and the risk of restless legs syndrome in an elderly general population--the MEMO-study. J Neurol. 2002;249(9):1195–1199. doi:10.1007/s00415-002-0805-2
22. Holzknecht E, Hochleitner M, Wenning GK, Hogl B, Stefani A. Gender differences in clinical, laboratory and polysomnographic features of restless legs syndrome. J Sleep Res. 2019;29:e12875. doi:10.1111/jsr.12875
23. Connor JR, Patton SM, Oexle K, Allen RP. Iron and restless legs syndrome: treatment, genetics and pathophysiology. Sleep Med. 2017;31:61–70. doi:10.1016/j.sleep.2016.07.028
24. Lammers N, Curry-Hyde A, Smith AJ, et al. Are serum ferritin and transferrin saturation risk markers for restless legs syndrome in young adults? Longitudinal and cross-sectional data from the Western Australian pregnancy cohort (raine) study. J Sleep Res. 2019;28(5):e12741. doi:10.1111/jsr.12741
25. Haschka D, Volani C, Stefani A, et al. Association of mitochondrial iron deficiency and dysfunction with idiopathic restless legs syndrome. Mov Disord. 2019;34(1):114–123. doi:10.1002/mds.27482
26. Mizuno S, Mihara T, Miyaoka T, Inagaki T, Horiguchi J. CSF iron, ferritin and transferrin levels in restless legs syndrome. J Sleep Res. 2005;14(1):43–47. doi:10.1111/j.1365-2869.2004.00403.x
27. Richard B, Berry MC, Rita Brooks MRR, et al. The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications (version 2.4); 2017.
28. Ferri R, DelRosso LM, Silvani A, et al. Peculiar lifespan changes of periodic leg movements during sleep in restless legs syndrome. J Sleep Res. 2020;29(3):e12896. doi:10.1111/jsr.12896
29. Allen RP, Picchietti DL, Garcia-Borreguero D, et al. Restless legs syndrome/Willis-Ekbom disease diagnostic criteria: updated International Restless Legs Syndrome Study Group (IRLSSG) consensus criteria--history, rationale, description, and significance. Sleep Med. 2014;15(8):860–873. doi:10.1016/j.sleep.2014.03.025
30. Tomlinson CL, Stowe R, Patel S, Rick C, Gray R, Clarke CE. Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov Disord. 2010;25(15):2649–2653. doi:10.1002/mds.23429
31. Garcia-Borreguero D, Allen RP, Kohnen R, et al. Diagnostic standards for dopaminergic augmentation of restless legs syndrome: report from a world association of sleep medicine-international restless legs syndrome study group consensus conference at the Max Planck Institute. Sleep Med. 2007;8(5):520–530. doi:10.1016/j.sleep.2007.03.022
32. Walters AS, LeBrocq C, Dhar A, et al. Validation of the international restless legs syndrome study group rating scale for restless legs syndrome. Sleep Med. 2003;4(2):121–132. doi:10.1016/s1389-9457(02)00258-7
33. Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi:10.1016/0165-1781(89)90047-4
34. Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–545. doi:10.1093/sleep/14.6.540
35. Chalder T, Berelowitz G, Pawlikowska T, et al. Development of a fatigue scale. J Psychosom Res. 1993;37(2):147–153. doi:10.1016/0022-3999(93)90081-P
36. McHorney CA, Ware JE Jr, Lu JF, Sherbourne CD, The MOS. 36-item short-form health survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care. 1994;32(1):40–66. doi:10.1097/00005650-199401000-00004
37. Vandeputte M, de Weerd A. Sleep disorders and depressive feelings: a global survey with the Beck depression scale. Sleep Med. 2003;4(4):343–345. doi:10.1016/S1389-9457(03)00059-5
38. Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56(6):893–897. doi:10.1037/0022-006X.56.6.893
39. Nasreddine ZS, Phillips NA, Bédirian V, et al. The Montreal cognitive assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–699. doi:10.1111/j.1532-5415.2005.53221.x
40. Folstein MF, Folstein SE, McHugh PR. ”Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. doi:10.1016/0022-3956(75)90026-6
41. Trenkwalder C, Allen R, Högl B, et al. Comorbidities, treatment, and pathophysiology in restless legs syndrome. Lancet Neurol. 2018;17:994–1005. doi:10.1016/S1474-4422(18)30311-9
42. Darien I. American Academy of Sleep Medicine International Classification of Sleep Disorders.
43. Li J, Moore HT, Lin L, et al. Association of low ferritin with PLM in the Wisconsin sleep cohort. Sleep Med. 2015;16(11):1413–1418. doi:10.1016/j.sleep.2015.05.015
44. Shin J, Koo YS, Lee BU, et al. Prevalence and characteristics of periodic limb movements during sleep in Korean adult patients with restless legs syndrome. J Clin Sleep Med. 2016;12(08):1089–1097. doi:10.5664/jcsm.6042
45. Belaidi AA, Bush AI. Iron neurochemistry in Alzheimer’s disease and Parkinson’s disease: targets for therapeutics. J Neurochem. 2016;139(Suppl 1):179–197. doi:10.1111/jnc.13425
46. Piao YS, Lian TH, Hu Y, et al. Restless legs syndrome in Parkinson disease: clinical characteristics, abnormal iron metabolism and altered neurotransmitters. Sci Rep. 2017;7(1):10547. doi:10.1038/s41598-017-10593-7
47. Li X, Allen RP, Earley CJ, et al. Brain iron deficiency in idiopathic restless legs syndrome measured by quantitative magnetic susceptibility at 7 tesla. Sleep Med. 2016;22:75–82. doi:10.1016/j.sleep.2016.05.001
48. Earley CJ, Connor JR, Beard JL, Malecki EA, Epstein DK, Allen RP. Abnormalities in CSF concentrations of ferritin and transferrin in restless legs syndrome. Neurology. 2000;54(8):1698–1700. doi:10.1212/WNL.54.8.1698
49. Earley CJ, Connor J, Garcia-Borreguero D, et al. Altered brain iron homeostasis and dopaminergic function in restless legs syndrome (Willis-Ekbom disease). Sleep Med. 2014;15(11):1288–1301. doi:10.1016/j.sleep.2014.05.009
50. Earley CJ, Ponnuru P, Wang X, et al. Altered iron metabolism in lymphocytes from subjects with restless legs syndrome. Sleep. 2008;31(6):847–852. doi:10.1093/sleep/31.6.847
51. Chawla S, Gulyani S, Allen RP, et al. Extracellular vesicles reveal abnormalities in neuronal iron metabolism in restless legs syndrome. Sleep. 2019;42(7). doi:10.1093/sleep/zsz079
52. Simpson IA, Ponnuru P, Klinger ME, et al. A novel model for brain iron uptake: introducing the concept of regulation. J Cereb Blood Flow Metab. 2015;35(1):48–57. doi:10.1038/jcbfm.2014.168
53. Connor JR, Ponnuru P, Wang XS, Patton SM, Allen RP, Earley CJ. Profile of altered brain iron acquisition in restless legs syndrome. Brain. 2011;134(4):959–968. doi:10.1093/brain/awr012
54. Connor JR, Duck K, Patton S, et al. Evidence for communication of peripheral iron status to cerebrospinal fluid: clinical implications for therapeutic strategy. Fluids Barriers CNS. 2020;17(1). doi:10.1186/s12987-020-00190-8
55. Chenini S, Delaby C, Rassu AL, et al. Hepcidin and ferritin levels in restless legs syndrome: a case-control study. Sci Rep. 2020;10(1):11914. doi:10.1038/s41598-020-68851-0
56. Dauvilliers Y, Chenini S, Vialaret J, et al. Association between serum hepcidin level and restless legs syndrome. Mov Disord. 2018;33(4):618–627. doi:10.1002/mds.27287
57. Ohayon MM, O’Hara R, Vitiello MV. Epidemiology of restless legs syndrome: a synthesis of the literature. Sleep Med Rev. 2012;16(4):283–295. doi:10.1016/j.smrv.2011.05.002
58. Montplaisir J, Boucher S, Poirier G, Lavigne G, Lapierre O, Lespérance P. Clinical, polysomnographic, and genetic characteristics of restless legs syndrome: a study of 133 patients diagnosed with new standard criteria. Mov Disord. 1997;12(1):61–65. doi:10.1002/mds.870120111
59. Ferri R, DelRosso LM, Aricò D, et al. Leg movement activity during sleep in school-age children and adolescents: a detailed study in normal controls and participants with restless legs syndrome and narcolepsy type 1. Sleep. 2018;41(4). doi:10.1093/sleep/zsy010
60. Ferri R, Koo BB, Picchietti DL, Fulda S. Periodic leg movements during sleep: phenotype, neurophysiology, and clinical significance. Sleep Med. 2017;31:29–38. doi:10.1016/j.sleep.2016.05.014
61. Högl B, Stefani A. Restless legs syndrome and periodic leg movements in patients with movement disorders: specific considerations. Movement Disord. 2017;32(5):669–681. doi:10.1002/mds.26929
62. Moore HT, Winkelmann J, Lin L, Finn L, Peppard P, Mignot E. Periodic leg movements during sleep are associated with polymorphisms in BTBD9, TOX3/BC034767, MEIS1, MAP2K5/SKOR1, and PTPRD. Sleep. 2014;37(9):1535–1542. doi:10.5665/sleep.4006
63. Czesnik D, Howells J, Bartl M, et al. I(h) contributes to increased motoneuron excitability in restless legs syndrome. J Physiol. 2019;597(2):599–609. doi:10.1113/JP275341
64. Kim T, Cha KS, Lee S, et al. Brain regions associated with periodic leg movements during sleep in restless legs syndrome. Sci Rep UK. 2020;10(1):1610–1615.
65. Ferri R, Sparasci D, Castelnovo A, et al. Leg movement activity during sleep in multiple sclerosis with and without restless legs syndrome. J Clin Sleep Med. 2022;18(1):11–20. doi:10.5664/jcsm.9466
66. Pelletier G, Lorrain D, Montplaisir J. Sensory and motor components of the restless legs syndrome. Neurology. 1992;42(9):1663–1666. doi:10.1212/WNL.42.9.1663
67. Ferri R. The time structure of leg movement activity during sleep: the theory behind the practice. Sleep Med. 2012;13(4):433–441. doi:10.1016/j.sleep.2011.10.027
68. Boehm G, Wetter TC, Trenkwalder C. Periodic leg movements in RLS patients as compared to controls: are there differences beyond the PLM index? Sleep Med. 2009;10(5):566–571. doi:10.1016/j.sleep.2008.04.009
69. Manconi M, Ferri R, Zucconi M, et al. Dissociation of periodic leg movements from arousals in restless legs syndrome. Ann Neurol. 2012;71(6):834–844. doi:10.1002/ana.23565
70. Manconi M, Ferri R, Feroah TR, Zucconi M, Ferini-Strambi L. Defining the boundaries of the response of sleep leg movements to a single dose of dopamine agonist. Sleep. 2008;31(9):1229–1237.
71. Sforza E, Nicolas A, Lavigne G, Gosselin A, Petit D, Montplaisir J. EEG and cardiac activation during periodic leg movements in sleep: support for a hierarchy of arousal responses. Neurology. 1999;52(4):786–791. doi:10.1212/WNL.52.4.786
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
