Back to Journals » Clinical Ophthalmology » Volume 15
Peripheral Cystoid Degeneration Finding Using Intraoperative Optical Coherence Tomography in Rhegmatogenous Retinal Detachment
Authors Nishitsuka K , Nishi K , Namba H, Kaneko Y, Yamashita H
Received 14 February 2021
Accepted for publication 2 March 2021
Published 18 March 2021 Volume 2021:15 Pages 1183—1187
DOI https://doi.org/10.2147/OPTH.S306623
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Koichi Nishitsuka, Katsuhiro Nishi, Hiroyuki Namba, Yutaka Kaneko, Hidetoshi Yamashita
Department of Ophthalmology and Visual Sciences, Yamagata University Faculty of Medicine, Yamagata, Japan
Correspondence: Koichi Nishitsuka
Department of Ophthalmology and Visual Sciences, Yamagata University Faculty of Medicine, Yamagata City, Yamagata, Japan
Tel +81 23-628-5374
Fax +81 23-528-5377
Email [email protected]
Purpose: The interaction between the peripheral vitreous and retina is closely associated with the pathogenesis of rhegmatogenous retinal detachment (RRD). This study was conducted to examine the peripheral vitreous and retina in patients with RRD using intraoperative optical coherence tomography (iOCT).
Methods: This retrospective study included 50 eyes of 50 patients (mean age 59.42 ± 10.80 years) that underwent vitrectomy using iOCT for treating RRD at the Yamagata University Hospital between September 2015 and September 2016. Each patient underwent 25-gauge pars plana vitrectomy that was performed by a single surgeon. During vitreous shaving with ocular indentation, the iOCT findings of the peripheral vitreous and retina were recorded and analyzed postoperatively.
Results: In all patients, iOCT was able to detect the peripheral retina and vitreous around the vitreous base. Peripheral cystoid degeneration was detected on the peripheral retina of 27 eyes (54%). Furthermore, cystoid degeneration was detected around the retinal tear (5 patients), at the detached retinal area (8 patients), and at the attached retinal area (14 patients).
Conclusion: iOCT enabled the evaluation of peripheral cystoid degeneration in patients with RRD. Cystoid degeneration might be associated with the pathogenesis of RRD.
Keywords: peripheral retinal degeneration, rhegmatogenous retinal detachment, cystoid degeneration, intraoperative optical coherence tomography
Introduction
The interaction between the peripheral vitreous and retina is closely linked to the pathogenesis of rhegmatogenous retinal detachment (RRD). Peripheral retinal degenerations can result in the formation of atrophic retinal holes or tractional retinal tears and therefore predispose patients to the development of an RRD.1 However, it is difficult to observe a peripheral lesion in an objective manner. Moreover, existing research concerning the prevention of RRD does not provide sufficient data to strongly support the prophylactic treatment of lesions other than symptomatic flap tears.2
Ghazi et al3 were the first to report the optical coherence tomography (OCT) findings of peripheral cystoid degeneration in an enucleated human eye. Choudhry et al4 also demonstrated the ultra-widefield steering spectral-domain OCT (SD-OCT) technique that provided the image of the peripheral retina, including peripheral cystoid degeneration. However, it is difficult to observe the peripheral retina in patients with RRD using these procedures that are applicable to the attached retina. Therefore, we developed a technique that uses a microscope-integrated intraoperative OCT (iOCT) system5 to acquire an objective view of the peripheral vitreous and retina during vitrectomy. Such advances in the objective evaluation of the peripheral vitreous and retinal are important as the first step in future research related to the prevention and treatment of RRD. Hence, the purpose of this study was to observe the peripheral vitreous and retina in patients with RRD using iOCT.
Methods
This retrospective study was performed in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the Yamagata University Faculty of Medicine (approval number: H26-21). All data were fully anonymized before we accessed them and the institutional review board waived the requirement for informed consent. We performed retrospective analyses of the medical records of 50 eyes of 50 consecutive patients with RRD who underwent 25-gauge pars plana vitrectomy using the wide-angle noncontact viewing system (Resight®; Carl Zeiss Meditec AG, Jena, Germany) with the Constellation Vision System (Alcon Laboratories, Inc., Fort Worth, TX, USA). The mean ± standard deviation (SD) age of the patients was 59.4 ± 10.8 years. All the study procedures were approved by the institutional review board of Yamagata University Faculty of Medicine. The procedures also conformed to the tenets of the Declaration of Helsinki. Patients were enrolled from September 2015 to September 2016.
The primary outcome measures were iOCT findings of peripheral lesions in patients with RRD obtained during peripheral vitreous shaving. Vitreous shaving was performed under a coaxial microscope using a slit lamp (Visulux; Zeiss, Oberkochen, Germany) with ocular indentation. The peripheral vitreous and retina were detected using iOCT (RESCAN; Carl Zeiss Meditec AG, Jena, Germany), as described previously,5 and the findings were recorded for postoperative analysis. The procedures used for detecting the peripheral retinal lesions via iOCT were as follows. Step 1: Performance of a scleral indentation to observe the peripheral part of the retina using a coaxial microscope. Step 2: Activation of iOCT and adjustment of OCT by focusing on the images of the peripheral retina and vitreous. For all the analyses, P < 0.05 was statically significant.
Results
Table 1 shows the breakdown of the iOCT findings. In all patients, the peripheral retina and vitreous around the vitreous base were detected using iOCT. There were 27 eyes (54%) in the cystoid degeneration positive group (Group A) and 23 eyes (46%) in the cystoid degeneration negative group (Group B) according to the iOCT findings. The mean ± SD age was 54.8 ± 12.0 years in Group A and 61.5 ± 10.5 years in Group B (Mann–Whitney U-test, P = 0.271). There were 7 females in group A and 5 females in group B (Fisher’s exact test, P = 1). The mean ± SD number of retinal breaks was 1.81 ± 1.73 in group A and 2.26 ± 1.36 in group B (Mann–Whitney U-test, P = 0.064). The mean ± SD quadrant of RD was 1.74 ± 0.76 in group A and 1.78 ± 0.85 in group B (Mann–Whitney U-test, P = 0.976). In Group A, the cystoid degeneration findings detected by iOCT were observed in three types of locations (Figures 1–3), including around the retinal break (5 patients; 18.5%), at the detached retinal area (8 patients; 29.6%), and at the attached retinal area (14 patients; 51.9%).
 |
Table 1 Patient Characteristics and the Results of This Study |
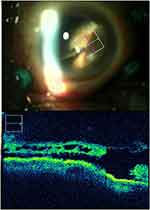 |
Figure 1 Peripheral cystoid degeneration around retinal break assessed by intraoperative optical coherence tomography (a 71-year-old-male). |
 |
Figure 2 Peripheral cystoid degeneration in detached retina assessed by intraoperative optical coherence tomography (a 49-year-old-female). |
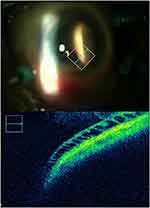 |
Figure 3 Peripheral cystoid degeneration in attached retina assessed by intraoperative optical coherence tomography (a 60-year-old-male). |
Discussion
Typical peripheral cystoid degeneration which appears as microscopic cystoid spaces in the inner to outer plexiform layers, has been detected in approximately 87% of autopsy eyes of patients of all age groups and in approximately 100% of eyes of older adults.6 It is believed that this finding is due to aging7(figure 1, figure 2, figure 3) and is defined as “peripheral retinal degeneration” in the International Classification of Diseases, 10th revision (ICD-10). In the case of retinal breaks merging with peripheral retinal degeneration, the ICD-10 classifies it as “retinal breaks without detachment,” Furthermore, when there is merging of retinal detachment with peripheral retinal degeneration, the ICD-10 classifies as “retinal detachment with retinal break.” Cheng et al8 reported that the prevalence of peripheral degeneration in myopic teenagers (aged 12–18 years) was 5% and was associated with an axial length of ≥26.5 mm. Hence, seemingly benign findings may also be associated with the onset of retinal detachment. Chu et al9 demonstrated that SD-OCT is a useful tool for evaluating peripheral retinal pathology and that it reliably provides structural details that may change clinical management.9
One of the advantages of OCT examination of the peripheral area is that the subject is a living eye rather than an autopsy eye. Moreover, iOCT allows the examination of detached retinas, which are difficult targets for normal preoperative OCT. Given that the prevalence of retinal detachment is approximately 10 in 100,000 persons per year,10 analysis of peripheral findings focusing on RRD may be better for iOCT analysis than the histological approach using autopsy eyes. In the present study, we found that 54% of patients with RRD had peripheral cystoid degeneration findings as evaluated by iOCT, suggesting that these findings are strongly associated with RRD. However, there were no statistically significant differences in age, gender, number of retinal breaks and quadrants of RD between group A and group B. Further analysis of the characteristics of patients with peripheral cystoid degeneration is needed.
The cystoid degeneration observed in the present study was found in the retinal break, detached retina, and attached retina and was primarily detected in the vitreous base. O’Malley et al6 demonstrated that 8 (11.3%) of 71 peripheral retinal holes occurred in areas of peripheral cystoid degeneration involvement in 1000 autopsy eyes. Based on their findings, they concluded that cystoid degeneration appears to be even more innocuous than generally believed.6 However, on the basis of our study findings, we believe that peripheral cystoid degeneration may not only develop itself into a retinal break, but it may also be a finding that reflects the pathogenesis of RRD like traction of the vitreous on the retina. Provided that peripheral cystoid degeneration may be a predictor of RRD or retinal break, the development of peripheral OCT may change the current clinical management such as follow-up, prophylactic retinal photocoaglation9 and appropriate vitreous shaving.11 In conclusion, we propose further prospective studies comprising a large number of patients with RRD to verify our study findings, and iOCT may be a useful technique for that purpose.
Acknowledgments
The Annual Meeting of the Association for Research in Vision and Ophthalmology, Honolulu (USA), April 29 to May 3, 2018.
Funding
This work was supported by JSPS KAKENHI Grant Number JP25462704.
Disclosure
Mr Koichi Nishitsuka reports personal fees from Santen, RE MEDICAL, INC., Carl Zeiss, Alcon, NOVARTIS, Kowa Company. Ltd., Johnson & Johnson, SENJU Pharmaceutical Co., Ltd., SANWA KAGAKU KENKYUSHO CO., LTD., and HOYA, outside the submitted work. Mr Hidetoshi Yamashita reports grants from Atsuzawa Prosthesis Co., Ltd., Alcon Japan Ltd., Santen Pharmaceutical Co., Ltd., Eisai Co., Ltd., SENJU PHARMACEUTICAL Co., Ltd., B.L.J Company, Ltd., Bayer Yakuhin, Ltd., AMO Japan, NOVARTIS Pharma Japan, Trust Medical Co., Ltd., and Taisho Pharma Japan, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Lewis H. Peripheral retinal degenerations and the risk of retinal detachment. Am J Ophthalmol. 2003;136(1):155–160. doi:10.1016/S0002-9394(03)00144-2
2. Wilkinson CP. Evidence-based analysis of prophylactic treatment of asymptomatic retinal breaks and lattice degeneration. Ophthalmology. 2000;107:
3. Ghazi NG, Dibernardo C, Ying H, et al. Optical coherence tomography of peripheral retinal lesions in enucleated human eye specimens with histologic correlation. Am J Ophthalmol. 2006;141:740–742. doi:10.1016/j.ajo.2005.10.058
4. Choudhry N, Golding J, Manry MW, et al. Ultra-widefield steering-based spectral-domain optical coherence tomography imaging of the retinal periphery. Ophthalmology. 2016;123(6):1368–1374. doi:10.1016/j.ophtha.2016.01.045
5. Nishitsuka K, Nishi K, Namba H, et al. Intraoperative optical coherence tomography imaging of the peripheral vitreous and retina. Retina. 2018;38(3):e20–e22. doi:10.1097/IAE.0000000000001979
6. O’Malley PF, Allen RA. Peripheral cystoid degeneration of the retina. Incidence and distribution in 1000 autopsy eyes. Arch Ophthalmol. 1967;77(6):769–776. doi:10.1001/archopht.1967.00980020771010
7. Grossniklaus HE, Nickerson JM, Edelhauser HF, et al. Anatomic alterations in aging and age-related diseases of the eye. Invest Ophthalmol Vis Sci. 2013;54(14):ORSF23–27. doi:10.1167/iovs.13-12711
8. Cheng SC, Lam CS, Yap MK. Prevalence of myopia-related retinal changes among 12–18 year old Hong Kong Chinese high myopes. Ophthalmic Physiol Opt. 2013;33:652–660. doi:10.1111/opo.12082
9. Chu RL, Pannullo NA, Adam CR, et al. Morphology of peripheral vitreoretinal interface abnormalities imaged with spectral domain optical coherence tomography. J Ophthalmol. 2019;2019:3839168. doi:10.1155/2019/3839168
10. Bechrakis NE, Dimmer A. [Rhegmatogenous retinal detachment: epidemiology and risk factors]. Ophthalmologe. 2018;115(2):163–178. doi:10.1007/s00347-017-0647-z.German.
11. Nishitsuka K, Nishi K, Namba H, et al. Quantification of the peripheral vitreous after vitreous shaving using intraoperative optical coherence tomography. BMJ Open Ophthalmol. 2021;6(1):e000605. doi:10.1136/bmjophth-2020-000605
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
