Back to Journals » Journal of Multidisciplinary Healthcare » Volume 13
Perceptions and Management of Allergic Rhinitis Among Ecuadorian Otorhinolaryngologists: A Survey-Based Study
Authors Felix M , Vera Paz C , Mata VL, Vanegas E , Larenas-Linnemann D , Rosario NA , Letort J, Cherrez-Ojeda I
Received 26 June 2020
Accepted for publication 3 November 2020
Published 17 December 2020 Volume 2020:13 Pages 1975—1981
DOI https://doi.org/10.2147/JMDH.S269531
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Miguel Felix,1,2 Carlos Vera Paz,1,2 Valeria L Mata,1,2 Emanuel Vanegas,1,2 Désirée Larenas-Linnemann,3 Nelson A Rosario,4 Jose Letort,5 Ivan Cherrez-Ojeda1,2
1Universidad Espíritu Santo, Samborondón, Ecuador; 2RespiraLab Research Group, Guayaquil, Ecuador; 3Investigational Center, Medica Sur Clinical Foundation and Hospital, Mexico City, Mexico; 4Departamento de Pediatria, Universidade Federal do Parana, Curitiba, Brazil; 5Departamento de Otorrinolaringología, Hospital, Quito, Ecuador
Correspondence: Ivan Cherrez-Ojeda
Universidad Espíritu Santo, Km. 2.5 Vía La Puntilla, Samborondón 0901-952, Ecuador
Tel +593 4511455
Email [email protected]
Objective: Allergic rhinitis (AR) represents a large burden to the healthcare system due to its high prevalence and impact on patients’ lives. Despite the existence of evidence-based guidelines, some studies have found that physicians do not always follow the latest recommendations. The aim of our study was to determine how Ecuadorian otorhinolaryngologists (ENTs) perceive some epidemiological aspects related to AR, as well as their preferences for managing the disease.
Methods: We conducted an observational, survey-based cross-sectional study, among 116 Ecuadorian ENTs. The survey used was adapted from a previous publication and consisted of 30 multiple choice questions, concerning several topics of AR. Descriptive statistics (frequency, and standard deviation) were performed for clinical and demographic variables.
Results: A total of 116 Ecuadorian ENTs completed the survey. Of them, 62.9% were male, with an average age of 42 years (SD ± 11.58). Computed tomography (CT) scan and nasal cytology were selected as the main diagnostic tests for AR by 62/91 (68.1%) and 45/91 (49.5%) of participants, respectively. Moreover, only 12/116 (10.3%) of participants performed skin prick tests (SPT). Allergen immunotherapy (AIT) was performed by 37/107 (36.4%) of participants.
Conclusion: In general, most participants agreed that the prevalence of AR appears to be increasing, with increased exposure to allergens, irritants, and pollutants as the main probable cause. Children and adolescents were accounted as the group most affected by AR, with sinusitis and asthma identified as the most frequent comorbidities. Finally, we found unmet needs in the diagnostic and management of AR that should be addressed among Ecuadorian ENTs, in particular the high use of CT scans as part of routine evaluations, as well as the low use of allergen immunotherapy.
Keywords: allergic rhinitis, Ecuador, epidemiology, Latin America, management
Introduction
Allergic Rhinitis (AR) is a disease characterized by symptoms of sneezing, nasal pruritus, and airflow obstruction mediated by an IgE response against inhaled allergens, causing mucosal inflammation driven by T helper (Th2) lymphocytes.1 This persistent Th2 response and eosinophilic inflammation may release several cytokines to the bloodstream that stimulate the bone marrow, and may function as a systemic amplifier of the eosinophilic inflammation.2 The diagnosis of AR is often based on its clinical presentation: a history of symptoms related in time with the exposure to the sensitizing allergens. However, testing can confirm the diagnosis and determine the specific allergens, either by measuring the presence of allergen-specific IgE in the serum, or by positive epicutaneous skin prick tests (SPT) (ie, wheal and flare responses to allergen extracts).3
There is a strong association between AR and other atopic conditions, in particular asthma.4 In general, radiological studies indicate that around 40% of adult and pediatric patients with asthma have sinus abnormalities, which interestingly enough increases among patients with severe asthma and/or a longer history of respiratory disease.2 Asthma and AR are characterized by eosinophilic inflammation, and it appears that children with both conditions tend to present with a more severe inflammatory response when compared to those who only present with AR.2 Thus, when evaluating patients with AR it is relevant to assess for other atopic conditions, as the former may act as a trigger or contribute to worsening of the disease.
Throughout the world the prevalence of allergic rhinitis has slightly increased, with recent estimates suggesting that between 10% and 30% of adults and 40% of children are affected.5,6 Due to geographic differences in the type and potency of different allergens, and overall aeroallergen burden, the prevalence of AR varies within countries. For instance, the European Community Respiratory Health survey recorded a prevalence of AR between 10% and 41% among adults, while a Scandinavian study reported a lower cumulative prevalence at 14%.7,8 In a large-scale study covering the major regions of the world, the highest prevalence of severe AR symptoms among children was observed in Africa and Latin America.9
Current guidelines advocate for a stepwise approach to the management of AR, recommending the initiation of treatment based on clinical presentation, and performing additional testing in patients who have persistent symptoms.10,11 New management strategies have also been incorporated in the care of patients with AR, mainly related to advances in the understanding of the role of specific allergen determination, and immunotherapy, in reducing symptoms and improving quality of life.12 However, AR still represents a large burden to the healthcare system due to its high prevalence and impact on patient’s lives, highlighting the importance of adequate management by healthcare providers to improve patients’ outcomes.13
Despite the existence of evidence-based guidelines, some studies have found that physicians do not always follow the latest recommendations.14,15 For instance, in an international survey of healthcare providers, 54.4% of physicians claimed to know the ARIA (Allergic Rhinitis and its Impact on Asthma) guidelines, while only 49.7% said they used them in clinical practice.15 The same study also noted that physicians who followed the guideline were more likely to offer allergen testing and immunotherapy than those who did not.15 On the other hand, patient satisfaction may be a reason for the frequent non-adherence to therapy seen in AR.16 To the best of our knowledge, there are no studies assessing how Ecuadorian otorhinolaryngologists manage patients with AR. Consequently, our study aims to determine how this specific subset of clinicians perceive some epidemiological aspects related to AR, as well as their preferences for managing the disease.
Methods
Study Design and Population
We conducted an observational, survey-based cross-sectional study, among Ecuadorian physicians participating at a national scientific meeting in July 2019. Due to accessibility and availability, convenience sampling was applied to include participants that had a specialization in otorhinolaryngology, as well as an active medical practice either at private or public centers.
Procedure
A survey from a previous publication which included 25 multiple choice questions concerning several topics of allergic rhinitis (see Table S1) was used.14 Questions 1 to 9 inquired participants about general perceptions of allergic rhinitis regarding epidemiology and clinical presentation (eg, prevalence, most frequently affected groups, most commonly found comorbidities, most common suspected causal aero allergens, most frequently reported symptoms, etc.). Questions 10 to 21 were related to diagnostic strategies (eg, SPT, most frequently tested allergens, measurement of total and specific IgE, and other diagnostic modalities used). Finally, questions 22 to 25 were about the preferences for managing patients with allergic rhinitis (eg, immunotherapy, and most prescribed medications)
Participants were approached by qualified previously trained personnel during meeting breaks. After explaining the purpose of the study and obtaining the consent to participate, a printed copy of the survey was handed. Participants filled their questionnaire either by following the instructions by themselves or with the help of the trained personnel.
Ethical Considerations
This study was approved by the ethics committee Comité de ética e Investigación en Seres Humanos (HCK-CEISH-19-0058), Guayaquil, Ecuador. Prior to obtaining verbal informed consent, the investigators explained the purpose of the study to the participants and their role in it. With the information recollected in the survey, personal identification was not possible; as such anonymity/personal data protection was conserved. The survey for our study was used under the terms of the Creative Commons Attribution Non-Commercial License (CC NC 4.0), which permits unrestricted non-commercial use provided the original work is properly cited.
Statistical Analysis
Descriptive statistics were performed for participant’s demographics and questions of interest. Data gathered from the surveys was examined descriptively in terms of general perceptions regarding epidemiology and clinical presentation, diagnostic strategies, and preferences on patient management. Frequencies and percentages were the selected method to represent proportions of nominal variables, whereas mean and standard deviation were preferred to summarize continuous data given a normal sample distribution with no significant outliers. All data were analyzed using SPSS, version 24.0 software (SPSS Inc., Chicago, IL, USA).
Results
Demographic Statistics
Of the 200 participants approached for the study, 116 completed the survey and were included in the analysis (response rate 58%), with a gender distribution of 62.9% male, and an average age of 42 years (SD ± 11.58) (Table 1). 43.1% of the participants offered their services in private practices.
 |
Table 1 Demographics of the Surveyed Population (n=116) |
General Perceptions About Allergic Rhinitis Regarding Epidemiology and Clinical Presentation
75/115 (65.2%) of the participants estimated the prevalence of allergic rhinitis to be over a third of the general population. 102/112 (91.1%) described its status as “surely increasing”. Increased exposure to allergens, irritants and pollutants was chosen by 85/113 (75.2%) of the participants as the main cause for the increased prevalence. Children and adolescents were appointed as the group most commonly affected by allergic rhinitis by 60/113 (53.1%) of the surveyed participants. Sinusitis and asthma were the most commonly reported comorbidities, whereas nasal blockage and rhinorrhea were the symptoms most often indicated by the ENTs as bothersome to their patients (Table 2). Furthermore, 51/113 (45.1%) of the participants selected ENT as the specialty most likely to be consulted by their patients in case of allergic rhinitis. House dust mites were regarded as the most common aeroallergen in our country.
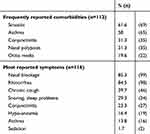 |
Table 2 Comorbidities and Symptoms Most Commonly Reported in Patients with Allergic Rhinitis by Ecuadorian Otorhinolaryngologists |
Diagnostic Strategies
Computed tomography (CT) scan and nasal cytology were selected as the main diagnostic tests for allergic rhinitis by 62/91 (68.1%) and 45/91 (49.5%) of participants, respectively. In addition, nasal cytology in outpatients was performed by only 27/111 (24.3%) of participants. 57/108 (52.8%) of the sample participants considered the rationale for performing nasal cytology as an aid in the differential diagnosis between allergic and non-allergic or infectious rhinitis. 40/84 (47.5%) of participants routinely requested serum total and specific IgE in cases of allergic rhinitis after SPT. From all the participants that performed nasal provocation tests, 8/15 (53.3%) considered this test useful for cases of occupational rhinitis.
Moreover, only 12/116 (10.3%) of participants performed SPT. The frequency of specific extracts tested for those who performed SPT was as follows: animal dander 12/12 (100%), mites 8/12 (66.6%), fungal 6/12 (50%), pollens 6/12 (50%), and insect allergens 6/12 (50%). 34/45 (75%) of ENTs considered a wheal’s diameter >3mm after 15 minutes as the criteria for a positive SPT.
Preferences for Managing Patients
Regarding symptomatic treatment for allergic rhinitis, oral H1-antihistamines and intranasal corticosteroids were the most prescribed medications (Figure 1). Allergen-specific immunotherapy was performed by 37/107 (36.4%) of surveyed participants. Intranasal administration was chosen as the preferred route for immunotherapy 27/80 (33.8%).
Discussion
Allergic rhinitis is a disease with varying prevalence according to the demographic characteristics of the population studied. For instance, in Latin America, the prevalence of AR in children has been estimated between 8.9% and 45.1%.17,18 Even though in Ecuador the prevalence of AR has been estimated at 23.9%, in our study, around two-thirds of participants considered the prevalence to be higher than 35%.18 This discrepancy could be attributed to the paucity of epidemiological data readily available for practitioners. Furthermore, they agreed that children and adolescents are the most affected group.
Regarding clinical presentation, current evidence points to nasal congestion, postnasal drip, repeated sneezing, and nasal discharge as the most common complaints among patients with AR.3 In accordance, most participants in our study reported nasal blockage and rhinorrhea as the main presenting symptoms of AR encountered in the clinical practice. Furthermore, roughly a third of participants selected snoring and sleeping problems as a frequent complaint among their patients, highlighting the need for increased awareness of sleep-related pathologies, since it has been documented that AR affects sleep patterns by producing microarousals through an increase in upper airway resistance, leading to chronic non-restorative sleep which alters daytime performance.19–21
Specific allergen testing is an important part of the workup of AR, especially of the more severe cases, where co-management with allergen immunotherapy can improve the general outcome.11 The two main tests available for this purpose are SPT and serum-specific IgE testing. SPT is a reliable method to diagnose IgE-mediated allergic diseases.22 A recent meta-analysis reported that SPT sensitivity ranged from 68% to 100% and SPT specificity from 70% to 91%.23 Interestingly, in our survey, amongst all participants, only 10.3% performed prick tests as part of the workup of AR. Although this is not a direct comparison, this rate stands in contrast with a British ENT survey, where SPT was the most frequently ordered test (81%) for the evaluation of this disease.22 On the other hand, 47.5% of participants routinely requested serum total and specific IgE after performing SPT. Studies comparing these two testing methods have found substantial differences between specific IgE and SPT results, suggesting that these methods complement each other and cannot be used interchangeably.24
Additional testing is often unwarranted in the initial evaluation of AR. For instance, recent guidelines recommend against routinely ordering computed tomography (CT) scans, unless other characteristics such as very severe disease, additional complications, or vulnerable patient populations are present.10,25 Despite this recommendation, we found in our study that most physicians reported ordering CT scans of the paranasal sinuses as part of the evaluation of AR (68.1%). Concerns regarding unnecessary exposure to ionizing radiation and the potential risk for future cancer development have been well described in the literature.26,27 Consequently, it is relevant to address this finding by raising awareness to the associated risks of unnecessary imaging studies, excluding any recommendation for its routine use.
Currently, AR management is based on symptomatic control with nasal corticosteroids, nasal antihistamines, leukotriene receptor antagonists, antihistamines, mast cell stabilizers, short-term nasal decongestants, and in the most severe cases, systemic corticosteroids.11 In our study, oral antihistamines and intranasal corticosteroids were the most commonly prescribed treatments for symptomatic management of AR. Different organizations have produced consensus statements highlighting research that supports the efficacy, safety, and pharmacology of newer generation oral H1 antihistamines and intranasal corticosteroids (INCSs), giving a strong recommendation for use of the latter in AR, while the former are still considered a good option in milder cases.28 The potent anti-inflammatory properties of INCSs are directed against the pathophysiologic mechanisms of nasal inflammation in AR.29 In comparative studies, INCS therapy has shown superior efficacy to H1 antihistamines and antileukotrienes in controlling nasal symptoms, including nasal congestion.30–32
In the case of allergen immunotherapy (AIT), this treatment modality is considered as the only disease-modifying treatment currently available for AR, and has been regarded as effective in reducing allergy symptoms.33–35 Research has shown that AIT can achieve long-term clinical results by improving symptoms, and reducing medication need.36 Interestingly, despite the current evidence and guideline recommendations, only a third of the surveyed ENTs recommended AIT. This finding stands contrasts with a survey among Chinese ENTs, which found that over 70% of specialists recommended AIT as early as possible for the treatment of AR.37 In this regard, a recent position paper on the international consensus on allergy immunotherapy argued that the main reasons for the slow rate of adoption are a lack of agreement on AIT efficacy, and insufficient data on its cost-effectiveness and long-term pharmacoeconomic impact.38
Finally, in light of our findings, there are several limitations that need to be disclosed. Firstly, even though we used a method of back to back translation, as well as a certified translator, and an expert panel of physicians review the final questionnaire, this instrument has not been validated yet. Secondly, there are different sample sizes for the proportions depicted in the results, which are the consequence of missing values in some questions. Thirdly, the epidemiological aspects studied in the questions stem directly from the surveyed ENTs' perspectives, and as such should not be interpreted as factual reality of the disease. Fourthly, even though convenience sampling is widely used in clinical research, it is certain that non-probability methods are often not representative of the population of interest, which is why the results may be subject to bias and are thus left under the reader’s discretion and interpretation. However, to the best of our knowledge, this is the first study to assess the perceptions and management of AR among Ecuadorian ENTs, and may provide insights into the management of AR that could extend to other countries in South America.
Conclusion
Adequate knowledge of recent evidence-based recommendations related to AR is important for adequate management of the disease by healthcare providers. In our study, we found that most Ecuadorian ENTs surveyed agreed that the prevalence of AR appears to be increasing, with increased exposure to allergens, irritants and pollutants as the main probable cause. Children and adolescents were appointed as the group most affected by AR, with sinusitis and asthma identified as the most frequent comorbidities. However, there are unmet needs in the diagnostic and management of AR that should be addressed among Ecuadorian ENTs, in particular the high use of CT scans as part of routine evaluations, as well as the low use of allergen immunotherapy. Further studies and potential interventions are needed to increase the awareness of guideline recommendations and their application in the clinical practice.
Abbreviations
AR, allergic rhinitis; ENTs, otorhinolaryngologists; SD, standard deviation; AIT, allergen immunotherapy; SPT, skin prick tests; ARIAallergic rhinitis and its impact on asthma; CT, computed tomography; INCSs, intranasal corticosteroids.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval
This study was approved by the ethics committee Comité de ética e Investigación en Seres Humanos (HCK-CEISH-19-0058) in accordance to the principles established by the declaration of Helsinki.
Consent for Publication
Not applicable.
Acknowledgments
The authors acknowledge the guidance and knowledge imparted by the MECOR Program for this study. Special thanks to all members of Respiralab Research Group, in particular Erick Calero, for his initial input in regard to this project. Finally, we want to express our gratitude to Universidad Espiritu Santo for their continuous support.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
This study was funded and supported by Universidad Espiritu Santo, Ecuador. The sponsor had no role in the design of the study or in the collection, analysis, and interpretation of data.
Disclosure
Désirée Larenas-Linnemann reports grants from GSK, Novartis, AZ, and Sanofi, outside the submitted work. The authors declare no other relevant conflicts of interest related to this work.
References
1. Wheatley LM, Togias A. Allergic rhinitis. N Engl J Med. 2015;372(5):456–463. doi:10.1056/NEJMcp1412282
2. Poddighe D, Brambilla I, Licari A, Marseglia GL. Pediatric rhinosinusitis and asthma. Respir Med. 2018;141:94–99. doi:10.1016/j.rmed.2018.06.016
3. Small P, Keith PK, Kim H. Allergic rhinitis. Allergy Asthma Clin Immunol. 2018;14(2):51. doi:10.1186/s13223-018-0280-7
4. Rosati MG, Peters AT. Relationships among allergic rhinitis, asthma, and chronic rhinosinusitis. Am J Rhinol Allergy. 2016;30(1):44–47. doi:10.2500/ajra.2016.30.4252
5. Björkstén B, Clayton T, Ellwood P, Stewart A, Strachan D. Phase III Study Group TI. Worldwide time trends for symptoms of rhinitis and conjunctivitis: phase III of the International Study of Asthma and Allergies in Childhood. Pediatr Allergy Immunol. 2008;19(2):110–124. doi:10.1111/j.1399-3038.2007.00601.x
6. Pawankar R, Canonica G, Holgate S, Lockey R, Blaiss M. WAO white book on allergy: update 2013. World Allergy Organ. 2013;248.
7. Heinrich J, Richter K, Frye C, et al. European Community Respiratory Health Survey in Adults (ECRHS). Pneumol Stuttg Ger. 2002;56(5):297. doi:10.1055/s-2002-30699
8. Nihlén U, Greiff L, Montnemery P, et al. Incidence and remission of self‐reported allergic rhinitis symptoms in adults. Allergy. 2006;61(11):1299–1304. doi:10.1111/j.1398-9995.2006.01166.x
9. Aït‐Khaled N, Pearce N, Anderson HR, et al. Global map of the prevalence of symptoms of rhinoconjunctivitis in children: the International Study of Asthma and Allergies in Childhood (ISAAC) phase three. Allergy. 2009;64(1):123–148. doi:10.1111/j.1398-9995.2008.01884.x
10. Seidman MD, Gurgel RK, Lin SY, et al. Clinical practice guideline: allergic rhinitis. Otolaryngol Neck Surg. 2015;152(1_suppl):S1–S43. doi:10.1177/0194599814561600
11. Brożek JL, Bousquet J, Agache I, et al. Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines – 2016 revision. J Allergy Clin Immunol. 2017;140(4):950–958. doi:10.1016/j.jaci.2017.03.050
12. Calderon MA, Alves B, Jacobson M, Hurwitz B, Sheikh A, Durham S. Allergen injection immunotherapy for seasonal allergic rhinitis. Cochrane Database Syst Rev. 2007;1.
13. Meltzer EO. Allergic rhinitis: burden of illness, quality of life, comorbidities, and control. Immunol Allergy Clin North Am. 2016;36(2):235–248. doi:10.1016/j.iac.2015.12.002
14. Passali D, Cingi C, Staffa P, Passali F, Muluk NB, Bellussi ML. The international study of the allergic rhinitis survey: outcomes from 4 geographical regions. Asia Pac Allergy. 2018;8:1. doi:10.5415/apallergy.2018.8.e7
15. Baena-Cagnani CE, Canonica GW, Zaky Helal M, et al. The international survey on the management of allergic rhinitis by physicians and patients (ISMAR). World Allergy Organ J. 2015;8(1):10. doi:10.1186/s40413-015-0057-0
16. Baiardini I, Braido F, Bonini M, Compalati E, Canonica GW. Why do doctors and patients not follow guidelines? Curr Opin Allergy Clin Immunol. 2009;9(3):228–233. doi:10.1097/ACI.0b013e32832b4651
17. Chong Neto HJ, Rosário NA, Solé D. Asthma and rhinitis in South America: how different they are from other parts of the world. Allergy Asthma Immunol Res. 2012;4(2):62–67. doi:10.4168/aair.2012.4.2.62
18. Solé D, Mallol J, Camelo‐Nunes IC, Wandalsen GF, Latin American ISAAC Study Group. Prevalence of rhinitis‐related symptoms in Latin American children – results of the International Study of Asthma and Allergies in Childhood (ISAAC) phase three. Pediatr Allergy Immunol. 2010;21(1‐Part‐II):e127–e136. doi:10.1111/j.1399-3038.2009.00947.x
19. Lavie P, Gertner R, Zomer J, Podoshin L. Breathing disorders in sleep associated with “microarousals” in patients with allergic rhinitis. Acta Otolaryngol. 1981;92(1–6):529–533.
20. Flemons WW, Tsai W. Quality of life consequences of sleep-disordered breathing. J Allergy Clin Immunol. 1997;99(2):S750–S756. doi:10.1016/S0091-6749(97)70123-4
21. Craig TJ, McCann JL, Gurevich F, Davies MJ. The correlation between allergic rhinitis and sleep disturbance. J Allergy Clin Immunol. 2004;114(5):S139–S145. doi:10.1016/j.jaci.2004.08.044
22. Heinzerling L, Mari A, Bergmann K-C, et al. The skin prick test – European standards. Clin Transl Allergy. 2013;3(1):3. doi:10.1186/2045-7022-3-3
23. Nevis IF, Binkley K, Kabali C. Diagnostic accuracy of skin-prick testing for allergic rhinitis: a systematic review and meta-analysis. Allergy Asthma Clin Immunol. 2016;12(1):20. doi:10.1186/s13223-016-0126-0
24. de Vos G. Skin testing versus serum-specific IgE testing: which is better for diagnosing aeroallergen sensitization and predicting clinical allergy? Curr Allergy Asthma Rep. 2014;14(5):430. doi:10.1007/s11882-014-0430-z
25. Fokkens WJ, Lund VJ, Mullol J, et al. EPOS 2012: European position paper on rhinosinusitis and nasal polyps 2012. A summary for otorhinolaryngologists. Rhinology. 2012;50(1):1–12. doi:10.4193/Rhino50E2
26. Brenner DJ, Hall EJ. Computed tomography – an increasing source of radiation exposure. N Engl J Med. 2007;357(22):2277–2284. doi:10.1056/NEJMra072149
27. Pearce MS, Salotti JA, Little MP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet. 2012;380(9840):499–505. doi:10.1016/S0140-6736(12)60815-0
28. Dykewicz MS, Wallace DV, Baroody F, et al. Treatment of seasonal allergic rhinitis: an evidence-based focused 2017 guideline update. Ann Allergy Asthma Immunol. 2017;119(6):489–511.e41. doi:10.1016/j.anai.2017.08.012
29. Watts AM, Cripps AW, West NP, Cox AJ. Modulation of allergic inflammation in the nasal mucosa of allergic rhinitis sufferers with topical pharmaceutical agents. Front Pharmacol. 2019;10:294. doi:10.3389/fphar.2019.00294
30. Weiner JM, Abramson MJ, Puy RM. Intranasal corticosteroids versus oral H1 receptor antagonists in allergic rhinitis: systematic review of randomised controlled trials. BMJ. 1998;317(7173):1624–1629. doi:10.1136/bmj.317.7173.1624
31. Yáñez A, Rodrigo GJ. Intranasal corticosteroids versus topical H1 receptor antagonists for the treatment of allergic rhinitis: a systematic review with meta-analysis. Ann Allergy Asthma Immunol. 2002;89(5):479–484. doi:10.1016/S1081-1206(10)62085-6
32. Berger WE, Nayak AS, Staudinger HW. Mometasone furoate improves congestion in patients with moderate-to-severe seasonal allergic rhinitis. Ann Pharmacother. 2005;39(12):1984–1989. doi:10.1345/aph.1G202
33. Kouzegaran S, Zamani MA, Faridhosseini R, et al. Immunotherapy in allergic rhinitis: it’s effect on the immune system and clinical symptoms. Open Access Maced J Med Sci. 2018;6(7):1248. doi:10.3889/oamjms.2018.264
34. Corren J, Baroody F, Pawankar R, Adkinson N, Bochner B, Burks A. Middleton’s allergy: principles and practice. Elsevier Health Sciences. 2013. Published online.
35. Cox L, Esch RE, Corbett M, Hankin C, Nelson M, Plunkett G. Allergen immunotherapy practice in the United States: guidelines, measures, and outcomes. Ann Allergy Asthma Immunol. 2011;107(4):289–299. doi:10.1016/j.anai.2011.06.018
36. Pipet A, Botturi K, Pinot D, Vervloet D, Magnan A. Allergen-specific immunotherapy in allergic rhinitis and asthma. Mechanisms and proof of efficacy. Respir Med. 2009;103(6):800–812. doi:10.1016/j.rmed.2009.01.008
37. Zhou H, Tao Q-L, Wei J-M, Xu G, Cheng L. Trends in specific immunotherapy for allergic rhinitis: a survey of Chinese ENT specialists. Allergy Asthma Immunol Res. 2014;6(4):296–303. doi:10.4168/aair.2014.6.4.296
38. Jutel M, Agache I, Bonini S, et al. International consensus on allergy immunotherapy. J Allergy Clin Immunol. 2015;136(3):556–568. doi:10.1016/j.jaci.2015.04.047
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

