Back to Journals » Advances in Medical Education and Practice » Volume 11
Perception of Pathology of Otolaryngology-Related Subjects: Students’ Perspective in an Innovative Multidisciplinary Classroom
Authors Atta IS , Alzahrani RA
Received 3 April 2020
Accepted for publication 13 May 2020
Published 29 May 2020 Volume 2020:11 Pages 359—367
DOI https://doi.org/10.2147/AMEP.S256693
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Balakrishnan Nair
Ihab Shafek Atta,1,2 Rajab A Alzahrani3
1Pathology Department, Faculty of Medicine, Al-Azhar University, Assuit, Egypt; 2Pathology Department, Faculty of Medicine, Albaha University, Albaha, Saudi Arabia; 3Surgery Department, Otolaryngology Division, Faculty of Medicine, Albaha University, Albaha, Saudi Arabia
Correspondence: Ihab Shafek Atta
Pathology Department, Faculty of Medicine, Al-Azhar University, Assuit 71524, Egypt
Tel +20882148103/4
Fax + 20882148119
Email [email protected]
Rajab A Alzahrani
Surgery Department, Otolaryngology Division, Faculty of Medicine, Albaha University, Saud Arabia
Tel +966509766298
Email [email protected]
Aim: Multidisciplinary, as a term, is used to define people from different scientific backgrounds working together, each drawing on their field of expertise. Some related terms are frequently used interchangeably, such as interdisciplinary and transdisciplinary, but they are confusing and ambiguous. Introduction of a multidisciplinary teaching method in the early phases of medical curricula is insufficient for effective learning. Here, we aim to implement a multidisciplinary approach in the early phase of medical education and identify outcomes.
Methods: Two groups were evaluated in this study, each representing phases II and III of the Albaha medical curriculum, and including 90 and 86 students, respectively. “Hearing tests and their clinical applications” was selected as a subject to evaluate the understanding of special senses as studied by the phase II group, while “pathology of otolaryngology-related tumors and clinical correlations” was selected as a subject to evaluate the understanding of otolaryngology as studied by the phase III group. These subjects were selected by faculty members from otolaryngology, pathology and physiology departments and taught in successive stations. Teaching sessions were followed by a formative test that included 10 multiple-choice questions and a mini-clinical evaluation exercise (mini-CEX). A questionnaire to evaluate student satisfaction was completed after the exam.
Results: Students’ satisfaction for the “hearing tests and their clinical applications” and “pathology of otolaryngology-related tumors and clinical correlations” subjects were 80% and 90.5%, respectively. The formative assessment revealed good student performance at 63.28%, and 60.46% of all students in both phases attained scores above 80%.
Conclusion: Introduction of a multidisciplinary approach early in the medical curriculum improves knowledge and skill acquisition. This is reflected in student performance, especially if evaluated using the mini-CEX format, thus providing rapid feedback to students concerning their performance.
Keywords: integration, multidisciplinary, mini-CEX, otolaryngology, pathology, student performance
Introduction
Integrated curricula have been extensively implemented due to widespread dissatisfaction with the teaching of basic sciences as unrelated disciplines with no connection to clinical practice.1 Conventional instructional tools no longer meet existing needs in multidisciplinary and interdisciplinary medical training settings.2,3 At the same time, advocates of cognitive learning suggest that integrated advances in schooling offer imperative benefits for active learning and knowledge retention as content application and contextualization are encouraged. Networks that motivate effective clinical interpretation are thus additionally supported.4–7 Terms such as multidisciplinary, interdisciplinary, and transdisciplinary are ambiguously defined and commonly used, accurately or not, interchangeably.8 Multidisciplinary, as a term, defines people from different scientific backgrounds working together while individually drawing on their field of expertise.9,10 In such a multidisciplinary approach, both students and instructors are motivated to connect seemingly different subject areas and work together to plan and present lessons that focus on a central theme.11,12
A multidisciplinary level of integration, as described by Harden,14 is opposite that of the word “webbed” introduced by Fogarty15 as it considers different subject areas to be the center of student learning to approach a particular set of problems, topics or subjects. Central subjects in an integrated module may serve different purposes. These subjects can define an area in which pragmatic decisions have to be made and hence serve as a crucial point for interdisciplinary judgment.
In the integrated Albaha medical school curriculum, we adopted the first eight levels of integration established by Harden et al14 (ie isolation, awareness, harmonization, nesting, temporal coordination, sharing, correlation, and complementation) and introduced multidisciplinary, interdisciplinary, and transdisciplinary levels into clinical practice. Aiming to improve student performance with minor curricular reforms,16–20 we selected the multidisciplinary level to be the one first evaluated. The aim of this study was to introduce and assess the multidisciplinary approach to teaching at the Albaha medical school curriculum by selecting subjects taught during different phases of medical education. Student and peer feedback was evaluated to establish an improved action plan for implementation in the near future.
Materials and Methods
This study was performed after receiving permission from the Quality Unit of the Albaha Faculty of Medicine, Saudi Arabia. A written agreement was also obtained from all of the participating students included in this study.
This study was performed during the teaching of special senses and otolaryngology modules, mapped in phases II and III of the medical program, respectively. As a component of continuous curriculum reform, the medical education and quality units started to implement the multidisciplinary approach in all program modules; special senses and otolaryngology modules were mapped to phases II and III of the medical curriculum, respectively, and evaluated as upcoming modules. A committee was formed encompassing staff from medical education, quality, and special senses and otolaryngology departments that decided on a process of teaching delivery after consultation with instructors. Subjects were to be selected in a multidisciplinary context. After evaluating teaching materials of both special senses and otolaryngology modules, both modules were selected after consultation with instructors. Learning outcomes were optimally matched with teaching strategies. Subject contents are detailed in Tables 1 and 2. These two subjects were selected considering the availability of teaching and learning resources in pathology and physiology labs, as well as diverse clinical and imaging modalities available within the otolaryngology department. The “hearing tests and their clinical applications” subject was taught to 90 students (60 male and 30 female), thus representing evaluation of the entire class studying the module in phase II of the medical curriculum. The “pathology of otolaryngology-related tumors and clinical correlations” subject was taught to a class of 86 students (58 male and 28 female) as part of the otolaryngology module taught in phase III of the medical curriculum.
 |
Table 1 Data for the “Hearing Tests and Their Clinical Applications” Module Taught to Phase II Medical Students |
 |
Table 2 Data for the “Pathology of Otolaryngology-Related Tumors and Clinical Correlations” Module Taught to Phase III Medical Students |
Learning outcomes for both subjects were assessed by faculty members from the three aforementioned departments; findings were also reviewed by the medical education unit.
Teaching of the “hearing tests and their clinical applications” module started with identification of the physiological basis and interpretation of hearing tests whilst individually monitoring students. The second station, taught by pathology faculty, clarified disease pathogenesis and etiologies of hearing loss. The third station, taught by otolaryngology faculty, instructed students how to perform a practical hearing examination including the utilization of imaging modalities. These stations were taught in two practical skill rooms (skill-labs) while the entire class was divided into two main groups. Each group was further subdivided into three subgroups circulating in one direction, starting from the physiology station and finishing at the otolaryngology station. The students spent 40 minutes in each station followed by a 15-minute break.
In the “pathology of otolaryngology-related tumors and clinical correlations” subject, basic pathology was taught in parallel with clinical and radiological applications. Both topics were taught by pathology and otolaryngology experts. Teaching was delivered in the skill-lab over three sessions, two hours each in duration. Each session consisted of two successive stations; in the first station students studied the pathogenesis and morphology (gross and microscopic images) of otolaryngology-related tumors using materials distributed by a pathology instructor. In the second station, clinical and radiological assessments were made by an otolaryngology instructor. These two stations were taught in the skill-lab and the entire class was divided into two main groups, further subdivided into two subgroups circulating in one direction, starting from the pathology station and ending at the otolaryngology station. The students spent 40 minutes in each station followed by a 15-minute break.
At the end of the multidisciplinary station, an exam consisting of 10 multiplechoice questions (MCQs) for each subject was administered. Exam questions were formed from scenario-based material covering all subject learning outcomes. Exam MCQs of the “hearing tests and their clinical applications” module consisted of three physiology questions, three pathology questions and four otolaryngology questions. Exam MCQs of the “pathology of otolaryngology-related tumors and clinical correlations” module consisted of five pathology questions and five otolaryngology questions, including radiological content.
Following the MCQ exam, a mini-clinical evaluation exercise (mini-CEX) was administered and consisted of four stations for each module. In the “hearing tests and their clinical applications” module, the first station evaluated student performance of different hearing tests in real patients; the second station evaluated diagnosis of a hearing problem in a standard patient; the third station evaluated student interpretation of gross and microscopic otolaryngological specimens; the fourth station evaluated student ability to formulate a management plan for the disorder in the third station. In the “pathology of otolaryngology-related tumors and clinical correlations” module, the first station evaluated student history taking skills via interaction with a patient simulating otolaryngological tumor symptoms; the second station evaluated student performance of physical and local head and neck examinations on a manikin with neck swelling; the third station evaluated student skills in the diagnosis of otolaryngological tumors both grossly and microscopically; the fourth station evaluated student skills in interpreting radiological data collected via different imaging modalities. In all stations, students were evaluated according to well-prepared checklists tailored for each station; each carried 5 marks. Station data are summarized in Table 3. Students were quickly provided with individualized, written feedback at the end of examination. We administered the mini-CEX as previously reported.21–24
 |
Table 3 Mini-Clinical Evaluation Exercise Data (Mini-CEX) for Both Modules |
Upon module completion, degree of student satisfaction was evaluated. Questionnaires structured separately for each module were designed by a committee composed of faculty members from pathology, physiology and otolaryngology departments. Questions were formulated and revised thoroughly by an educational specialist and a small pilot study evaluating groups composed of junior faculty members and students were performed to support reliability. During each module, a questionnaire was distributed to all the students included in this study. The questionnaire used was quantitative and consisted of a 5-point Likert scale25–27 collecting information concerning student satisfaction regarding the teaching of subjects as a multidisciplinary learning approach. Questionnaires measured the degree of satisfaction among participants with values of 5 (strongly satisfied), 4 (satisfied), 3(neutral), 2 (dissatisfied), and 1 (strongly dissatisfied).16–19,25–27
Results
Students’ satisfaction and formative assessments were very impressive. Satisfaction on the “hearing tests and their clinical applications” revealed that 63 out of 90 (70%) students were strongly satisfied, 14 (15.5%) were satisfied, 5 (5.6%) were neutral, 4 (4.4%) were dissatisfied, and 4 (4.4%) were strongly dissatisfied.
In the “pathology of otolaryngology-related tumors and clinical correlations” module, findings revealed that 60 out of 86 (69.7%) students were strongly satisfied, 6 (6.97%) were satisfied, 5 (5.8%) were neutral, 8 (9.3%) were dissatisfied, and 7 (8.13 %) were strongly dissatisfied. These data are detailed in Figure 1 and Table 4. Formative assessment (consisting of the mini-CEX and 10-MCQ exam) data for both modules are summarized in Table 5.
 |
Table 4 Student Satisfaction Data for a Multidisciplinary Approach to Teaching in Both Phases (Phase II and III) of the Medical Curriculum |
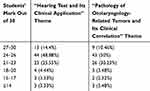 |
Table 5 Mini-Clinical Evaluation Exercise and 10-Question Multiple-Choice Exam Performance Data for Both Modules |
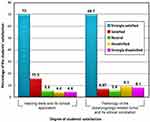 |
Figure 1 Graph represents the students’ satisfaction against the multidisciplinary subjects of phase II and phase III. |
For the “hearing tests and their clinical applications” module, evaluation of student MCQ exam performance in physiology revealed that 60 (69.7%) of the students scored 3/3, 17 (19.7%) scored 2/3 and 9 (10.6%) scored 1/3. Evaluation of student performance in pathology revealed that 64 (74.4%) of the students scored 3/3 and 22 (25.6%) scored 2/3. Evaluation of student performance in otolaryngology revealed that 62 (72%) of the students scored 4/4, 13 (15.1%) scored 3/4, and 9 (10.4%) scored 2/4 and 2 (2.3%) scored 1/4.
For the “pathology of otolaryngology-related tumors and clinical correlations” module, evaluation of student performance in pathology revealed that 65 (72.2%) of the students scored 5/5, 16 (17.8%) scored 4/5 and the remaining 9 (10%) scored ≤ 3. Evaluation of student performance in otolaryngology revealed that 66 (73.3%) of the students scored 5/5, 16 (17.8%) scored 4/5 and 8 (8.8%) scored ≤3.
Student performance on the mini-CEX was evaluated using a checklist. For the ”hearing tests and their clinical applications” module, student performance evaluation revealed that 63 (70%) of the students scored ≥4/5 in the first station; 76 (84.4) % of the students scored ≥ 4/5 in the second station, 73 (81.1%) of the students scored ≥4/5 in the third station, and 63 (70%) of the students scored ≥4/5 in the fourth station. For the “pathology of otolaryngology-related tumors and clinical correlations” module, student performance evaluation revealed that 62 (72%) of the students scored ≥4/5 in the first station, 69 (80.2%) of the students scored ≥4/5 in the second station, 66 (76.7%) of the students scored ≥4/5 in the third station, and 60 (69.7%) of the students scored ≥4/5 in the fourth station.
Discussion
In our multidisciplinary approach, students and instructors were encouraged to join diverse subject areas and work together to map and present lessons that focused on a central theme.10–13
Our study integrated otolaryngology, pathology, and physiology instruction so that teaching was delivered in successive stations by participating faculty from each discipline. This was achieved following the general outline concerning implementation of a multidisciplinary teaching approach as described by Harden.14
In order to monitor this newly adopted teaching methodology, students were administered a 10-question MCQ exam followed by a mini-CEX to assess their degree of acquired knowledge as well as cognitive and psychomotor skills. Students received feedback immediately after completing the exam as in other studies that used the mini-CEX assessment.21–24 The validity of data obtained from both assessment models was done through the followings; good feedback from the students and peers regarding the whole process and mode of assessment and from the psychometric studies such as item analysis and discrimination index and the data obtained was within normal values. The introduction of both multiple-choice questions and mini-CEX at the end of the multidisciplinary sessions achieved all levels of the Miller’ triangle;28,29 the multiple-choice questions used in this current methodology were based mainly on the first two levels know and knows how, while the show s how and does achieved through the mini-CEX. However it is recognized that mini-CEX only capture one element of evaluating clinical competency. In order to evaluate the full range of clinical competency multi-method assessments are required. By using MCQs beside the mini-CEX, the defects of individual assessment formats can be overcome. The addition of practical sessions in the mini-CEX, such as diagnosing a histopathological specimen, integrated elements of basic science into the context of clinical examination. The spiral curriculum of the medical school mandates basic science teaching in all phases of the curriculum. Questionnaire data revealed that student satisfaction in this multidisciplinary approach was 85.5%, and 77% for both modules (as detailed in Figure 1 and Table 4). Our results were supported by both MCQ and mini-CEX formative assessment performance data (Table 5) that detailed students performance in each discipline separately as determined by thorough analysis of exam results. Our findings were consistent with those reported by Muller et al,30 where effects of a multidisciplinary approach to introductory teaching of anatomical pathology and radiology were investigated. Course content was delivered by faculty from both disciplines and this approach garnered a highly positive response from the students. Similar results were also reported by Flaherty et al, Tawfek and Redick, Mihalik et al, and Galvin et al, who studied the diagnosis of pneumonia, breast cancer, benign breast lesions, and lung fibrosis using a multidisciplinary approach.31–34
In order to differentiate between the terms multidisciplinary, interdisciplinary and transdisciplinary, Choi and Pak explained that a multidisciplinary approach represents utilization of knowledge gathered from diverse disciplines which, at the same time, is clearly classified as originating within the boundaries of their respective fields. The interdisciplinary approach integrates relationships between disciplines into coherent and coordinated processes. The transdisciplinary approach integrates health, social, and natural sciences in a humanities framework, exceeding the conventional boundaries of these fields by themselves.35 These three terms refer to the contribution of several disciplines in different quantities and contexts but on a similar scale.
Sorace et al36 found that multidisciplinary integration is essential for attaining precise diagnoses and managing patients appropriately. Atta and AlQahtani37 found that all integration across disciplines, especially in multidisciplinary and interdisciplinary manners, has major positive effects on learning outcomes. They thus recommended the adoption of such an approach for teaching of all content starting early in the curriculum. In addition, modification of teaching modalities and selection of appropriate integrative approaches, along with suitable alignment with relevant teaching/learning tools, has been reported to positively impact student achievement.38,39 Choi and Pak40 also stated that disciplines that are more different from one another in nature and knowledge type are more likely to lead to novel approaches for composite objectives. The proposed theoretical framework of knowledge identifies many knowledge subsystems, each containing several disciplines. This inter-disciplinary divide direct selection of suitable disciplines for multidisciplinary instruction.
In some circumstances, task-based learning an be considered to be an example of a hidden multidisciplinary approach as it possesses multidisciplinary features in which learning is focused not only on ingenuity in task performance but also in skill building, thus increasing understanding of relevant basic and clinical sciences. There is continuous debate on this subject as task-based learning is mainly student-centered, whilst the multidisciplinary method is taught in a teacher-centered fashion with faculty members playing a major role in bringing their field of expertise to the course module.
Conclusion
Introducing a multidisciplinary integrated approach to teaching early in the medical curriculum positively impacts the acquisition of student knowledge and skills. This is reflected in student performance and achievement, especially if followed by mini-CEX assessment with rapid feedback sharing with students regarding their performance. Modification of the mini-CEX assessment in alignment with the academic curriculum warrants consideration, such as by introduction of practical sessions in a clinical context. Our findings revealed that student satisfaction was high in regards to our curricular modification and they strongly supported implementation of such a teaching approach in upcoming modules.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Atwa HS, Gouda EM. Curriculum integration in medical education: a theoretical review. Intel Prop Rights. 2014;2(2):113. doi:10.4172/2375-4516.1000113
2. Cooke M, Irby DM, Sullivan W, Ludmerer KM. American medical education: 100 years after the Flexner report. N Engl J Med. 2006;355(13):1339–1344. doi:10.1056/NEJMra055445
3. Custers E, Cate OT. Medical students’ attitude towards and perception of the basic sciences: a comparison between students in the old and new curriculum at the University Medical Centre Utrecht, the Netherlands. Med Educ. 2002;36:1142–1150. doi:10.1046/j.1365-2923.2002.01371.x
4. Mann KV. Thinking about learning: implications for principle based professional education. J Contin Educ Health Prof. 2002;22(2):19–26. doi:10.1002/chp.1340220202
5. Vidic B, Weitlauf HM. Horizontal and vertical integration of academic disciplines in the medical school curriculum. Clin Anat. 2002;15(3):233–235. doi:10.1002/ca.10019
6. Regehr G, Norman GR. Issues in cognitive psychology: implications for professional education. Acad Med. 1996;96(9):988–1002. doi:10.1097/00001888-199609000-00015
7. Bordage G. Elaborated knowledge: a key to successful diagnostic thinking. Acad Med. 1994;69(11):883–885. doi:10.1097/00001888-199411000-00004
8. Flores‐Sandoval C, Sibbald S, Ryan BL, Orange JB. Healthcare teams and patient‐related terminology: a review of concepts and uses. Scand J Caring Sci. doi:10.1111/scs.12843
9. Doyle M, Bozzone D. ‘Multidisciplinary teaching providing undergraduates with the skills to integrate knowledge and tackle “Big” questions. J Center Interdisciplinary Teach Learn. 2018;7:12–17.
10. Klaassen RG. Interdisciplinary education: a case study. Eur J Eng Educ. 2018;43(6):842–859.
11. Bradley P, Mattick K. Integration of Basic and Clinical Sciences. AMEE; 2008.
12. Leathard A. Going Inter-Professional: Working Together for Health and Welfare. London: Psychology Press; 1994.
13. Frenk J, Chen L, Bhutta ZA, et al. Health professionals for a new century. Transforming education to strengthen health systems in an interdependent world. Lancet. 2010;376:1923–1958.
14. Harden RM. The integration ladder: a tool for curriculum planning and evaluation. Med Educ. 2000;34:551–557.
15. Fogarty R. Ten ways to integrate curriculum. Educ Leadership. 1991;49:61–65.
16. Atta IS, Alqahtani FN. How to adjust the strategy of radiopathologic teaching to achieve the learning outcomes? Int J Med Sci Public Health. 2018;7(2018):1130015122017.
17. Atta IS, Alqahtani FN, Alghamdi TA, Mankrawi SA, Alamri AM. Can Pathology. Teaching’ strategy be affected by the students’ learning style and to what extent the students’ performance be affected? Glob Adv Res J Med Med Sci. 2017;6(11):296–301.
18. Atta IS, Alqahtani FN. Hybrid PBL radiology module in an integrated medical curriculum al-baha faculty of medicine experience. J Contemp Med Edu. 2015;3(1):46–55. doi:10.5455/jcme.20150525033016
19. Atta IS, Alghamdi AH. The efficacy of self-directed learning versus problem-based learning for teaching and learning ophthalmology: a comparative study. Adv Med Educ Pract. 2018;9:623–630. doi:10.2147/AMEP.S171328
20. Atta IS, El-Hag MA, Ihab Shafek S, Al-Ghamdi HS, Alghamdi TH. Drawbacks in the implementation of an integrated medical curriculum at medical schools and their potential solutions. Educ Med Jl. 2020;12(1):29–42. doi:10.21315/eimj2020.12.1.4
21. Lörwald AC, Lahner FM, Nouns ZM, et al. The educational impact of Mini-Clinical Evaluation Exercise (Mini-CEX) and Direct Observation of Procedural Skills (DOPS) and its association with implementation: a systematic review and meta-analysis. PLoS One. 2018;13(6):1–15. doi:10.1371/journal.pone.0198009
22. Lau Yanting S, Sinnathamby A, Wang DB, et al. Conceptualizing workplace based assessment in Singapore: undergraduate mini-clinical evaluation exercise experiences of students and teachers. Tzu Chi Med J. 2016;28(3):113–120. doi:10.1016/j.tcmj.2016.06.001
23. Hoseini BL, Jafarnejad F, Mazloum SR, Foroughipour M. Practical experience of the Mini-CEX in undergraduate trainees. Procedia - Soc Behav Sci. 2013;83:803–807. doi:10.1016/j.sbspro.2013.06.151
24. Norcini JJ, Blank LL, Duffy FD, Fortna GS. Academia and clinic the Mini-CEX: a method for assessing clinical skills. Ann Intern Med. 2003;138(6):476–481. doi:10.7326/0003-4819-138-6-200303180-00012.
25. Boynton PM, Greenhalgh T. Selecting, designing, and developing your questionnaire. BMJ. 2004;328:1312–1315. doi:10.1136/bmj.328.7451.1312
26. Boynton PM. Administering, analysing, and reporting your questionnaire. BMJ. 2004;328(7452):1372–1375. doi:10.1136/bmj.328.7452.1372
27. Rattray J, Jones M. Essential elements of questionnaire design and development. J Clin Nurs. 2005;16(2):234–243. doi:10.1111/j.1365-2702.2006.01573.x
28. Miller GE. The assessment of clinical skills/competence/performance. Acad Med. 1990;65(9):S63–70. doi:10.1097/00001888-199009000-00045
29. Williams BW, Byrne PD, Welindt D, Williams MV. Miller’s pyramid and core competency assessment: a study in relationship construct validity. J Contin Educ Health Prof. 2016;36(4):295–299. doi:10.1097/CEH.0000000000000117
30. Muller J, Jain S, Loeser H, Irby D. Lessons learned about integrating a medical school curriculum: perceptions of students, faculty and curriculum leaders. Med Educ. 2008;42(8):778–785. doi:10.1111/j.1365-2923.2008.03110.x
31. Flaherty K, King TJ, Raghu G, et al. Idiopathic interstitial pneumonia: what is the effect of a multidisciplinary approach to diagnosis? Am J Respir Crit Care Med. 2004;170:904–910. doi:10.1164/rccm.200402-147OC
32. Tawfik O, Redick M. Integrated radiology/pathology service for breast cancer. Crit Values. 2009;2(3):23–26. doi:10.1093/criticalvalues/2.3.23
33. Mihalik JE, Krupka L, Davenport R, Tucker L, Toevs C, Smith RS. The rate of imaging-histologic discordance of benign breast disease: a multidisciplinary approach to the management of discordance at a large university-based hospital. Am J Surg. 2010;199(3):319–323. doi:10.1016/j.amjsurg.2009.11.004
34. Galvin J, Frazier A, Franks T. Collaborative radiologic and histopathologic assessment of fibrotic lung disease. Radiology. 2010;255(3):692–706. doi:10.1148/radiol.10090717
35. Choi BCK, Pak AWP. Multidisciplinarity, interdisciplinarity and transdisciplinarity in health research, services, education and policy: 1. Definitions, objectives, and evidence of effectiveness. Clin Invest Med. 2006;29(6):351–364.
36. Sorace J, Aberle DR, Elimam D, Lawvere S, Tawfik S, Wallace WD. Integrating pathology and radiology disciplines: an emerging opportunity? BMC Med. 2012;10(1):100. doi:10.1186/1741-7015-10-100
37. Atta IS, AlQahtani FN. Integrated pathology and radiology learning for a musculoskeletal system module: an example of an interdisciplinary integrated form. Adv Med Educ Pract. 2018;9:527–533. doi:10.2147/AMEP.S167692
38. Atta IS. AlQahtani FN Matching medical student achievement to learning objectives and outcomes: a paradigm shift for an implemented teaching module. Adv Med Educ Pract. 2018;9:227–233. doi:10.2147/AMEP.S158784
39. Atta IS, AlQahtani FN. Mapping of pathology curriculum as quadriphasic model in an integrated medical school: how to put into practice? Adv Med Educ Pract. 2018;7(9):549–557. doi:10.2147/AMEP.S163971
40. Choi BC, Pak AW. Multidisciplinarity, interdisciplinarity, and transdisciplinarity in health research, services, education and policy: 3. Discipline, inter-discipline distance, and selection of discipline. Clin Invest Med. 2008;31(1):E41–8.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
