Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 12
Perceived Stigma and Associated Factors Among HIV Positive Adult Patients Attending Antiretroviral Therapy Clinics at Public Facilities of Butajira Town, Southern Ethiopia, 2020
Authors Melis T, Fikadu Y , Lemma L
Received 4 September 2020
Accepted for publication 14 October 2020
Published 9 November 2020 Volume 2020:12 Pages 717—724
DOI https://doi.org/10.2147/HIV.S280501
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Bassel Sawaya
Tamirat Melis,1 Yohannes Fikadu,2 Lire Lemma1
1Wachamo University, College of Medicine & Health Sciences, Department of Public Health, Hosanna, Ethiopia; 2Wolkite University, College of Medicine & Health Sciences, Department of Public Health, Wolkite, Ethiopia
Correspondence: Tamirat Melis Email [email protected]
Background: Stigma refers to attitudes and beliefs that lead people to reject, avoid, or fear those they perceive as being different. It identifies people as criminals, slaves, or traitors to be shunned. Globally 30– 80% of people living with HIV experience stigma during their lifetime. There is a paucity of research in identifying determinants of stigma on HIV positive patients in Ethiopia. The aim of this study is to assess magnitude and factors associated with stigma among HIV positive adults attending antiretroviral therapy (ART) clinics at public health facilities of Butajira town.
Methods: Institution-based cross-sectional study was conducted at public health facilities of Butajira town. A total of 403 study participants were selected by systematic random sampling technique. Data were collected by using pre-tested interviewer-administered semi-structured questionnaire. The collected data were entered into EpiData3.1 and exported to SPSS version 23. Bivariate and multivariable logistic regression analysis were used to identify factors associated with stigma. The strength of association was assessed by crude odds ratio and adjusted odds ratio for bivariate and multivariable logistic regression analysis, respectively. Statistical significance was declared at p-value < 0.05 and 95% CI.
Results: The magnitude of stigma among HIV positive patient was 28.9%. Discussing about safer sex (AOR: 2; 95% CI: (1.14,3.18), disclosing HIV positive status (AOR: 6;95% CI: (2.3,14.9), being a female (AOR: 2.5; 95% CI: (1.41,4.12) and age > 34 years (AOR: 4; 95% CI: (1.46,12.9) were the independent factors associated with stigma in HIV positive patients.
Conclusion: The magnitude of stigma in ART patient is still unresolved problem. Discussing about safer sex, disclosing HIV positive status, being a female and age were the independent factors associated with stigma in HIV positive patients.
Keywords: stigma, associated factors, ART patients
Background
Since the start of the HIV epidemic, over 70 million people have been infected with the HIV virus and it has killed 35 million people worldwide. There have been 36.9 million peoplehaving HIV in their blood. Africa (WHO region) is one of the HIV-prevalent regions, with 4.1% of the population living with HIV, and accounts for 66% of people living with HIV at the end of 2017.1 Ethiopia has a large and very vulnerable population and there were more than half million (729,089) HIV positive population, 21,606 new HIV infections and 10,960 deaths in 2018.2
Stigma refers to attitudes and beliefs that lead people to reject, avoid, or fear those they perceive as being different.3 It identifies people as criminals, slaves, or traitors to be shunned.3 HIV-related perceived stigma remains pervasive and disallows people with HIV the right to fully participate in their communities, affecting all aspects of people’s lives, including access to treatment and care, and access to work, creating a negative impact due to HIV-related stigma,4 with poor HIV outcomes.5
Perceived stigma greatly affects the quality of life for people living with HIV (PLWH), their family members and the healthcare providers who work with them,6 and causes serious care limitation.7 Stigma can also cause serious social and psychological damage and significantly increases loneliness, depression, anxiety, on-disclosure of HIV status and overall poor health outcomes.8,9
Sub-saharan Africa contributed 76% (29 million) of the total HIV infected people.10 In Ethiopia the adult prevalence rate is estimated at 2.4%.11–13 over the last decade, evidence based effective programming to reduce stigmatizing and discrimination attitude has expanded substantially.14 However almost no country has prioritized activities to reduce or eliminate them in their national plans or programs.15 People who experience stigma report a range of negative effects including loss of income or job, isolation from communities and inability to participate as a productive member of society.16,17 Globally 30–80% of people living with HIV experience stigma during their lifetime.18 The magnitude of stigma in North Bengal medical college attending antiretroviral therapy (ART) centers was 25.8%19 (21) while in Iran the magnitude among women living with HIV was 69.7%20 and 26% in Chennai.21
Another study revealed the prevalence of perceived stigma among people living with HIV attending ART clinic at the University of Port Harcourt Teaching Hospital, Nigeria as 59.9%.22 The people living with HIV/AIDS (PLWHA) in Ethiopia experienced stigmatization through gossip, verbal insult, isolation, and rejection according to a stigma index survey conducted by networks of HIV positive people.23 The aim of this study was to assess the magnitude and factors associated with perceived stigma among ART patients attending public health facilities of Butajira town, Southern Ethiopia, 2019.
Methods
Study Setting and Design
This study was conducted at public health facilities of Butajira town, Gurage Zone, Southern Ethiopia, 135 km south from Addis Ababa, located at the base of the Zebidar massive in the Gurage Zone of the Southern Nations, Nationalities and Peoples’ Region. The town has an estimated total population of 50,290 (24,642 males and 25,648 females). The town has one General hospital, one private hospital, one health center, ten private clinics and five health posts.
ART services provided both at Butajira General Hospital and Butajira Health Center with average monthly attendance of 1021 ART follow-up patients. An institution-based cross-sectional study was conducted from March 01, 2019 to March 30, 2019 on ART clients. The study populations were all HIV positive adult patients who were attending ART clinics at public health facilities of Butajira town that fulfill the eligibility criteria.
Sample Size and Sampling Procedure
The sample size was determined by using single population proportion formula by considering the following assumptions: 95% CI, 5% margin of error and the value of “p” (p= proportion of prevalence) was taken as prevalence of perceived stigma among PLWH which was found to be 61.1% (done in Jimma town, Ethiopia).24
Accordingly the calculated sample size with 10% non-response rate for this study was 403. The total number of adults attending ART clinic at public health facilities of Butajira town was 945 (813 from Butajira General Hospital and 132 from Butajira Health Center). The sample size was allocated proportionally for the hospital and health center and selected by using systematic random sampling. Since total sample size for this study was 403, k=945/403=2.34=2. Lottery method was used to determine every 1st or the 2nd case. Therefore every 1st client from the first two patients who came for ART service was selected systematically as the study participants.
Operational Definition
Perceived Stigma (Yes)
Study participants who scored mean and above from 10 stigma assessment questions were classified as had perceived stigma.25
Stigma (No)
Study participants who scored less than mean from ten stigma assessment questions were classified as had no perceived stigma.25
Data Collection Tools and Procedure
The standardized data collection tool was developed through reviewing of related literature. It contains information on socio-demographic, individual factors and disease-related factors. Perceived stigma was assessed by a 10-item perceived HIV stigma scale assessment tool which contains 10 stigma assessment questions with Likert scale. The level of perceived stigma was measured by agreement question (strongly disagree–strongly agree from a value of 1–5, respectively. The mean value was 30. Those study participants who scored 30 and above from 10 stigma assessment questions were classified as “perceived stigma” while a score of less than 30 were considered as “not perceived stigma”.
First the questionnaire was prepared in English, translated to Amharic and then back to English. A week before the beginning of actual data collection, a pre-test was done on 5% of the sample size in Agena town. The data were collected by six case managers/adherence supporters and supervised by two public health officers who were trained on HIV/AIDS comprehensive management and care. Training was given for data collectors and supervisors on how to manage the data collection process. The data were collected by face-to-face interview and reviewing patient card by using interviewer-administered semi-structured questionnaire.
Data Processing and Analysis
Data were entered into EpiData version 3.1 and then exported to SPSS version 23 for further analysis. The descriptive analysis such as percentage, frequency and mean were calculated. Bivariate and multivariable logistic regression analysis were used to identify presence of associations between dependent and independent variables. In bivariate analysis variables with p≤0.25 were entered to multivariable logistic regression analysis. The Hosmer–Lemeshow test was used to check the appropriateness of the model for analysis. The possible effects of confounders were controlled through multivariable logistic regression analysis. The association between the explanatory and dependent variables were assessed at the p-value of 0.05. The variables that show p-value <0.05 were declared as statistically significant variables in multivariable logistic regression analysis. The degree of association between independent and dependent variables were assessed using crude odds ratio (COR) and adjusted odds ratio (AOR) for bivariate and multivariable logistic regression respectively with 95% confidence interval.
There were 15 (discussing about safer sex, marital status, age, sex, belonging to HIV/AIDS support group, disclosing HIV positive status, knowing importance of HIV positive status disclosure, religion, educational status, marital status, knowing HIV status of sexual partner, viral load, CD4 count, stages of HIV, income) variables done for bivariate analysis. Variables which had p-value less than 0.25 were chosen for multivariate analysis. There were six variables (discussing about safer sex, marital status, age, sex, belonging to HIV/AIDS support group and disclosing HIV positive status) which were underwent multivariate analysis (p-value less than 0.25).
Results
Socio-Demographic Characteristics
A total of 403 ART patients participated in this study giving the response rate of 97.8%. The age of respondents ranged from 19 to 70 years with a mean age of 38 +±10 years. Of the total participants, 270 (67.7%) were females. Majority 317 (79.4%) of respondents were from urban areas. About 247 (62%) of the study participants were from Gurage ethnic group. More than half 214 (53.6%) of the respondents were orthodox Christian. One hundred sixty three (40.9%) did not attended formal education. Two hundred seven of the respondents (51.9%) were married (Table1)
 |
Table 1 Socio Demographic Characteristics of ART Patients Attending Public Health Facilities of Butajira Town, Southern Ethiopia, 2019 (n=399) |
From a total of 387 respondents who had tested for current viral load, 313 (79%) had current suppressed viral load (<1000 copies/mL) and 209 (59%) had low CD4 count at ART start while 325 (91%) of the participants had current CD4 count ≥ copies/mL. (Table 2)
 |
Table 2 Individual- and Disease-Related Factors of ART Patients Attending Public Health Facilities of Butajira Town, Southern Ethiopia, 2019 (n=399) |
Individual Characteristics of Study Participants
Among 307 (77%) of study participants who had history of sexual intercourse within previous six months, 250 (81%) of them utilized a condom during sexual intercourse. Two hundred forty seven (60%) of the study participants had discussed about safer sex freely (Table 3).
 |
Table 3 Individual and Psychosocial Factors of Adult ART Patients Attending Public Health Facilities of Butajira Town, Southern Ethiopia, 2019 (n=399) |
Magnitude of Stigma on HIV Positive Patient
Among the study participants 28.8% of them had perceived stigma. See Figure 1.
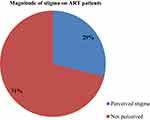 |
Figure 1 Magnitude of perceived stigma among adult ART patients attending ART clinics at public health facilities of Butajira town, Southern Ethiopia, 2019 (n=399). |
Assessment of Stigma on HIV Positive Patient
Among the total of study participants 240 (60%) strongly disagree “I think that people would be afraid of me if they knew their HIV status”. One hundred twenty (30%) of the study participants agree that ”they are afraid about people discriminating against them”. See Table 4.
 |
Table 4 Individual and Psychosocial Factors of Adult ART Patients Attending Public Health Facilities of Butajira Town, Southern Ethiopia, 2019 (n=399) |
Factors Associated with Perceived Stigma
Bivariate analysis was performed to assess factors which were significantly associated with perceived stigma. The bivariate analysis showed that discussing about safer sex; marital status, age, sex, belonging to HIV/AIDS support group and disclosing HIV positive status were variables which were candidates for multivariable binary logistic regression analysis.
In multivariable logistic regression analysis discuss about safer sex, disclosing HIV positive status, sex and age were factors significantly associated with stigma on HIV positive patients.
The odds of perceived stigma in ART patients who had free discussion about safer sex was 2 times more likely to develop stigma than their counterparts (AOR: 2; 95% CI: (1.14,3.18). ART patients who had disclosed their HIV positive status were 6 times more likely to have stigma than those who had not disclosed their HIV positive status (AOR: 6; 95% CI: (2.30,14.90). Being female is 2.5 times more likely to develop stigma than being male (AOR: 2.5; 95% CI: (1.41, 4.12) (Table 5).
Discussion
This study assessed the magnitude of perceived stigma and factors associated with it among PLWHA attending ART Clinic in public health facilities of Butajira town, Gurage zone, Southern Ethiopia. From the total respondents, 399 (29%) have perceived stigma. This finding is lower than studies conducted in Nigeria 59.9%,22 Iran (69.7%)20 and from world pooled magnitude (30–80%).18
The possible explanation for this difference might be because of the collaboration work of governmental and nongovernmental organizations working in public health facilities of Butajira town. There were four nongovernmental projects which work on activities like providing counseling services, partner notification, educating the community on stigma and discrimination and adhering the patient for ART service. Study time difference might be the other possible explanation. Initiation of test and treat program might be another justification. Those who newly entered into ART program had high stigma score as compared to those using ART for a long period.26
This study revealed that, disclosing HIV status caused less likely to experience stigma than those who did not disclose their HIV positive status. This might be because of those who had disclosed their HIV positive status to someone would get trust and a good friendship which in turn will help them to cope up with HIV with reduced stigma.
This study showed that those who had discussion about safer sex were less likely to develop stigma than those that did not discuss about safer sex. It is consistent with study conducted at Jimma town, Ethiopia, in which those who had discussion about safer sex were more likely to disclose their HIV positive status than their counterparts.27 This might be due to the fact that discussion about safer sex may encourage them to have open communication and freedom to disclose their HIV status.
These findings revealed that females were more likely to experience stigma than males. This finding is consistent with studies conducted in Dilla and Jimma of Ethiopia and Kenya.27–29 This might be due to the fact that if females are infected by HIV, the community views them as having been promiscuous at least once in their lifetime when they are infected with HIV.26
This study showed that study participants who are aged older than 34 years are exposed to stigma than being an age of 18–24 years. It is consistent with a study conducted in Dilla, Ethiopia.28 This might be due to the fact that those who are older than 34 years are in productive age groups. Therefore they are prone to participate in different social and economic activities.
Limitations of the Study
The findings may not be inferenced to the general population since it was a facility-based study. The cross sectional study design has weakness in the establishing temporal relationship. The wealth index was not assessed. It would be better supported by utilizing a qualitative method.
Conclusion
The magnitude of perceived stigma among ART patient in public health facilities of Butajira town is low. Disclosing HIV positive status, Discussing about safer sex, being a female and age were the independent factors associated with stigma in HIV positive patients. Therefore, increased efforts are needed from stakeholders on strengthening of HIV positive status disclosure. Also females need special attention to tackle the level of stigma. In addition, health workers have to give a due emphasis on awareness creation of stigma on HIV positive patients.
Declaration
Ethical clearance was obtained from Arbaminch University, College of Medicine and Health Science, Institutional Ethical Review Board. By using support letter which was approved by from Arbaminch University Institutional Ethical Review Board, Department of Public Health, permission to conduct the research was obtained from Gurage zone health office, Butajira General Hospital and Butajira Health Center. Verbal informed consent was obtained from study participants and approved by the ethical committee. The study was conducted according to the declaration of Helsinki.
Respondents were informed about the purpose and procedure of the study, the importance of their participation, the right to withdraw at any time if they want and about privacy and confidentiality of the information given by each respondent which was kept properly and that their name would not be recorded.
Abbreviations
AOR, adjusted odds ratio; HIV, human immunodeficiency virus; ART, antiretroviral therapy; AIDS, acquired immunodeficiency syndrome.
Data Sharing Statement
The data sets used/or analysed during the current study available at all authors on reasonable request.
Acknowledgment
We would like to express our heartfelt appreciation to data collectors and all ART patients who were involved as study participant in this study. We are also grateful to all health professionals who supported the study process.
Author Contributions
TM, LL and YF made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no competing interests.
References
1. WHO. Global Health Observatory Data on Prevalence of HIV Among Adult Age 15–49. WHO; 2017.
2. HAPCO/EPHI. HIV Epidemic Estimates 2017–2021. Ethiopia: EPHI; 2017.
3. Disability rights oc, California, definition of stigma and discrimination. Available from: https://www.disabilityrightsca.org/. Accessed November 02, 2020.
4. Friedland BASL, Nyblade L, Baral SD, et al. Measuring intersecting stigma among key populations living with HIV: implementing the people living with HIV stigma index 2.0. J Int AIDS Soc. 2018;21(SupplSuppl 5):e25131. doi:10.1002/jia2.25131
5. Dlamini PSWDML, Greeff M, Kohi TW, Greeff M, Naidoo J, Mullan J. HIV stigma and missed medications in HIV-positive people in five african countries. AIDS Patient Care STDS. 2009;23(5):377–387. doi:10.1089/apc.2008.0164
6. Pourmarzi DKA, Gaeeni M. Perceived stigma in people living with HIV in qom. J Fam Reprod Health. 2017;11(4):202.
7. Katz ITRA, Onuegbu AG, Psaros C, et al. Impact of HIV‐related stigma on treatment adherence: systematic review and meta‐synthesis. J Int AIDS Soc. 2013;2013(16):18640.
8. Mukolo ATI, Bechtel RM, Sidat M, Vergara AE, Vergara AE. Consensus on context-specific strategies for reducing the stigma of human immunodeficiency virus/acquired immunodeficiency syndrome in Zambézia Province, Mozambique. SAHARA. J Soc Aspects HIV AIDS. 2013;10(3–4):119–130. doi:10.1080/17290376.2014.885847
9. Rao DCW-T, Pearson CR, Simoni JM, et al. Social support mediates the relationship between HIV stigma and depression/quality of life among people living with HIV in Beijing, China. Int J STD AIDS. 2012;23(7):481–484. doi:10.1258/ijsa.2009.009428
10. Wang HWT, Carter A, Nguyen G, et al. Estimates of global, regional, and national incidence, prevalence, and mortality of HIV, 1980–2015: the global burden of disease study 2015. Lancet HIV. 2016;3(8):e361–e87. doi:10.1016/S2352-3018(16)30087-X
11. Mbonu NC, De Vries NK, De Vries NK. Stigma of people with HIV/AIDS in SubSaharan Africa: a literature review. J Trop Med. 2009;2009:1–14. doi:10.1155/2009/145891
12. Ortblad KFLR, Murray CJ, Murray CJL. The burden of HIV: insights from the global burden 12 of disease study 2010. AIDS. 2013;27(13):2003. doi:10.1097/QAD.0b013e328362ba67
13. Luiz, B. Can [Conditional] Cash Transfers Contribute to HIV Prevention for Girls. Vol. 2012. geneva: UnESCO, gender Equality, HIV and Education; 2012.
14. Brihnu Z. HIV stigma and associated factors among antiretroviral treatment clients in Jimma town, Southwest Ethiopia. HIV AIDS (Auckl). 2016;8:183.
15. CS. G. Stigmatization and AIDS: critical issues in public health. Soc Sci Med. 1994;1359–1366.
16. Il O. Recommendation Concerning HIV and AIDS and the World of Work,2010 (No. 200). Geneva: ILO; 2010.
17. Sorsdahl KRMS, Stein DJ, Joska JA, Joska JA. The prevalence and predictors of stigma amongst people living with HIV/AIDS in the Western Province. AIDS Care. 2011;23(6):680–685. doi:10.1080/09540121.2010.525621
18. Datta SBS, SherPa PL, Banik S. Perceived HIV related stigma among patients attending art center of a tertiary care center in rural West Bengal, India. J Clin Diagn Res. 2016;10(10):VC09.
19. Zarei NJH, Fararouei M. Perceived stigma and quality of life among women living with HIV/AIDS. Womens Health. 2016;2016(4):e34535.
20. Thomas BRF, Suryanarayanan D, Josephine K, et al. How stigmatizing is stigma in the life of people living with HIV: a study on HIV positive individuals from Chennai, South India. AIDS Care. 2005;17(7):795–801. doi:10.1080/09540120500099936
21. Kanu CTMO, Okeafor CU. Perceived stigma and highly active antiretroviral 13 treatment adherence among persons living with HIV/AIDS in the University of Port Harcourt Teaching Hospital. Orient J Med. 2017;29(1–2):40–47.
22. Feyissa GTAL, Girma E, Woldie M, Woldie M. Stigma and discrimination against people living with HIV by healthcare providers, Southwest Ethiopia. BMC Public Health. 2012;12(1):522. doi:10.1186/1471-2458-12-522
23. The people living with HIV stigma index. Addis Ababa: nEP;2012.
24. Z MJ L, Khoshnood K, Hsieh E, Sheng Y, Sheng Y. HIV-related stigma among people living with HIV/AIDS in rural Central China. 2018. BMC Health Serv Res. 2018;18(1):453. doi:10.1186/s12913-018-3245-0
25. Berger BEFC, Lashley FR, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. 2001. Res Nurs Health. 2001;24(6):518–529. doi:10.1002/nur.10011
26. AVERT. Women and HIV/AIDS. 2015:2015.
27. Neno Nikus MA, Zewdie B. HIV Stigma and Associated Factors Among Antiretroviral Treatment Clients in Jimma Town, Southwest Ethiopia, 2016. dove press; 2016.
28. Yirgalem A. HIV related perceived stigma and associated factors among patient with HIV, Dilla, Ethiopia, 2019. AIDS Care. 2019.
29. Colombini MMR, Kivunaga J, Stackpool Moore L, Mayhew SH, Mayhew SH. Integra initiative experiences of stigma among women living with HIV attending sexual and reproductive health services in Kenya: a qualitative study. BMC Health Serv Res. 2014;14(1):412. doi:10.1186/1472-6963-14-412
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

