Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 11
Perceived stigma among people living with HIV AIDS in Pokhara, Nepal
Authors Subedi B , Timilsina BD, Tamrakar N
Received 24 July 2018
Accepted for publication 31 December 2018
Published 7 May 2019 Volume 2019:11 Pages 93—103
DOI https://doi.org/10.2147/HIV.S181231
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Bassel Sawaya
Babita Subedi,1 Bishow Deep Timilsina,2 Neeta Tamrakar3
1Matrisishu Miteri Hospital, Pokhara, Nepal; 2Surgical Department, Manipal Teaching Hospital, Pokhara, Nepal; 3Tribhuwan University, Institute of Medicine, Pokhara Campus, Pokhara, Nepal
Background: HIV-related stigma among people living with HIV/AIDS (PLWHA) is the foremost barrier to HIV prevention, treatment, care, and support. The aim of this study was to identify the perceived stigma level of PLWHA and its relation with selected demographic and situational factors in Pokhara, Nepal.
Methods: Cross-sectional descriptive study was conducted among 282 PLWHA after probability sampling from antiretroviral treatment center of Western Regional Hospital, Pokhara, Nepal. Face-to-face interview was taken by using Bunn standard HSS tool. Stigma was measured in terms of felt stigma (public attitude concern [PAC], disclosure concern [DC], negative self-image [NSI]), enacted stigma [ES], as well as overall stigma.
Result: The mean score of PAC, DC, NSI, ES, and overall stigma was 3.09, 3.02, 2.79, 1.66, and 2.52, respectively, where mean score of all domains of felt stigma (PAC, DC, and NSI) was >2.5, thus reflecting a higher level of felt stigma. ANOVA and t-test revealed higher level of overall stigma among younger age group (P<0.001), highly educated group (P=0.007), unmarried group (P<0.001), and recently HIV-diagnosed group (P=0.003).
Conclusion: The study suggests high level of felt stigma, which has devastating effects on PLWHA as well as leads to nondisclosure of sero-positive status. So considering the significant impact of felt stigma on control of HIV epidemic, it is important to have a broader comprehension of this phenomenon and its repercussions on PLWHA via timely intervention like better educational intervention and counseling to PLWHA, wide-scale societal awareness campaigns, and more focused local interventions.
Keywords: stigma, felt stigma, public attitude concern, disclosure concern, negative self-image, enacted stigma, people living with HIV/AIDS
Introduction
AIDS is a chronic, potentially life-threatening condition caused by the HIV. Infection with the virus results in progressive deterioration of the immune system, leading to immune deficiency.1
HIV-related stigma remains highly prevalent across the globe.2,3 There is growing recognition that gaps across the cascade of HIV prevention, testing, and treatment services are fuelled by stigma and discrimination faced by people living with HIV and people at high risk of HIV infection.4 Studies on stigma and discrimination and health-seeking behavior show that people living with HIV who perceive high levels of HIV-related stigma are 2.4 times more likely to delay enrolment in care until they are very ill.5 Furthermore, it is a disease that probably brings separation among families in triggering a compassionate, solidarity response.6 So addressing stigma affecting people living with HIV/AIDS (PLWHA) is a global priority.7
HIV-related stigma and discrimination may be internalized and experienced as shame or guilt or externalized as discrimination.8 Enacted stigma (ES) (discrimination) is experiences such as being denied, improperly treated due to HIV-positive status, while internalization is the adoption of society’s negative views into the self-concept. It may lead to self-blame, shame, lack of disclosure, reduced self-confidence, loss of motivation, withdrawal from social contact and health-based interactions, and abandonment of planning for the future.9
Moreover, stigma level is comparatively more prevalent in developing countries. A study carried out in Tamil Nadu, India, showed that prevalence of severe level of stigma is high. It was also concluded that ensuring high-quality comprehensive services at the antiretroviral treatment (ART) centers and social support for the PLWHA is vital to decrease stigma and depression, and increase the quality of life.10 In Nepal, stigma and discrimination against the PLWHAs are found in family, society, health care setting, and fellow PLWHA. Though Nepal is said to achieve a significant progress in policy and human rights for PLWHA,11 enforcement is yet needed to be strong.
HIV/AIDS-related stigma is recognized to be a major obstacle to successfully control the spread of this disease.6,12 A consistent, negative association has been found between fear of stigma and use of testing and treatment services. Therefore, it is worthwhile to identify the perceived stigma among PLWHA so that unique associated factors can be identified early. Hence, this study was carried out:
- To find out the level of perceived stigma in terms of enacted and felt stigma.
- To examine the differences in perceived stigma score according to selected sociodemographic variables.
- To determine the differences in perceived stigma score according to selected clinical characteristics.
Methods
Descriptive cross-sectional research design was used to identify the perceived stigma among people living with HIV/AIDS. The study was conducted in ART center of Kaski District, Western Regional Hospital (WRH), which is situated in Ramghat, Pokhara.
Patients diagnosed with HIV/AIDS who were under antiretroviral therapy in ART center of Kaski District were the study population of the study. Total number of adult patients (≥20 years) under antiretroviral therapy at that time was 724. So sample size was calculated by standard formula. Hence, sample size calculated was 282. Systematic random sampling was used to collect the sample. Sampling interval was 724/282=2.56, that is, 2. So researcher took every second client as sample. For the first sample, simple random sampling was done by lottery method from 1 and 2. By lottery method, number 2 got selected, and hence, the first sample taken was second patient of the day.
Data collection instrument/procedure
Research proposal was approved by Ethical Review Board of Tribhuwan University, Institute of Medicine, Kathmandu. The data collection unit was people living with HIV/AIDS who were under ART of Kaski ART center, WRH. All respondents were informed briefly regarding objectives of the study and verbal and written informed consent was taken from them. Respondents were not influenced by any means to participate in the study. Strict confidentiality of their identities was reassured. Voluntary participation of respondents was ensured with the choice to withdraw any time without fear and clarification. Data were collected from 282 respondents who came for ART services in ART center, using interview schedule in the separate room (ie, extra counseling room) of ART center after completion of their ART services, considering their convenient time. Data were collected for one-and-a-half month period. Study was carried out in accordance with the principle of Helinski.
Data were collected using the interview schedule, which consisted of two parts. Part I (A) dealt with background information, which consisted of sociodemographic data, and Part I (B) dealt with questions related to HIV diagnosis, risk practices, and its disclosure. Researcher herself developed the questionnaire of this section, through extensive literature search.
Part II consisted of standard tool HSS developed by Bunn,13 which was the adopted version of Berger14 HIV stigma scale. Permission to use that scale was taken from Bunn. This tool was a 4-point Likert scale (from strongly disagree to strongly agree) containing 32 questions with 4 domains, where questions 8 and 18 had negative scoring. The specific questions and the domains they cover are given below.
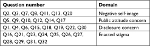  |
The scores ranged from 32 to 128 [1 × 32 items to 4 × 32 items]. For the ES domain, scores ranged from 11 to 44. For the disclosure domain, scores ranged from 8 to 32. For the negative self-image (NSI) domain, scores ranged from 7 to 28. For the public attitudes domain, scores can range from 6 to 24. All 32 questions measure overall stigma.
The validity of the tool was established by adopting the valid previous tool, extensive literature review, and consultation with subject matter experts (ART counselor, PLWHA volunteer of HIV/AIDS support group). To use the tool in Nepalese context, first forward translation (from English to Nepali) and then backward translation (From Nepali to English) were done by two independent bilingual translators.
Pretesting of the Nepali version tool was done for its feasibility and appropriateness among 10% of the sample who met sample criteria in a similar setting (ART center of Bharatpur Hospital). Reliability in terms of internal consistency of part II of the tool was tested with Cronbach’s alpha from the pretested data and overall internal consistency was found to be 0.907.
Statistical analyses
Data were analyzed using SPSS 21. Stigma score was obtained by summing up the responses of each item of subscale and later mean was computed from the composite value of each subdomain by the number of items corresponding to each subscale in order to obtain a comparable figure. The higher the mean value, higher the stigma level was considered while calculating the mean difference of stigma scores.
Mean score ≥2.5 was considered as high-level and <2.5 as low-level stigma as in the previous study12 in order to identify the stigma level. To find out the difference in stigma scores with different sociodemographic variables and clinical characteristics, independent t-test and ANOVA test were done. Independent t-test was used to compare means of two variables, whereas ANOVA test was used to compare the means of more than two variables. The level of significance was considered at 5% with P<0.05 and 95% CI.
Results
Sociodemographic characteristics of PLWHA
Table 1 shows the sociodemographic characteristics of PLWHA. Among PLWHA, 27.3% belonged to the age group of 40–49 years, where female occupied 50.7%. Overall mean and SD of age of the PLWHA was 39.04±11.03. More than two-third (67.7%) of them reported living with partner and 63.1% were from municipality. Considering ethnicity, 46.5% of them were Janajati. Majority (86.2%) of them were literate and 54.3% were unemployed.
  | Table 1 Sociodemographic variables of PLWHA, n =282 Note: Mean age 39.04 ± SD 11.03. |
Clinical characteristics of respondents
Sixty eight percent of PLWHA were diagnosed with HIV before 3 years and 48.2% had tested their HIV status mainly during treatment of other illnesses due to HIV-related symptoms. The preceding risk factor of acquiring HIV was sexual relationship with multiple partners, that is, 45%. Among 282 PLWHA, 85.3% (n=221) disclosed their HIV status to others.
Perceived stigma level of PLWHA
Table 2 summarizes perceived stigma level of PLWHA. Among felt stigma domains, majority (83.3%) of PLWHA had high level of public attitude concern (PAC), while 25.4% and 46.1% had high level of enacted and overall stigma, respectively.
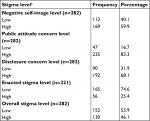  | Table 2 Perceived stigma level of PLWHA Notes: Stigma mean score <2.5= low-level stigma, stigma mean score ≥2.5= high-level stigma. aCriteria for stigma level according to Bunn.12 |
Mean score of overall stigma and their domains
Table 3 demonstrates mean score of overall stigma and their domains. Out of 282 PLWHA the mean score of overall stigma was 2.52, with score ranges from 1.21 to 3.81, with the SD of 0.48. Among the four domains, PAC had the highest mean score of 3.09 with SD of 0.52 and ES had the least mean score of 1.66 with the SD of 1.08.
  | Table 3 Mean score of overall stigma and their domains Abbreviation: SE, standard error. |
Differences on NSI score according to sociodemographic and clinical characteristics
Relation between NSI and sociodemographic and clinical characteristics is highlighted in Table 4. It depicts that there was significant difference in NSI mean score with regard to age (P<0.0001), educational status (P<0.0001), marital status (P<0.0001), place of residence (P=0.014), and time of HIV diagnosis (P<0.0001). NSI mean score was significantly high among young adult, PLWHA who resided in urban area, had higher-level education status, were unmarried, and who were diagnosed as having HIV/AIDS for <3 years. Conversely, no significant difference in mean score between the groups in terms of sex and high-risk behavior practices was noted.
Difference in PAC scores according to sociodemographic and clinical characteristics
Table 5 summarizes the relation between sociodemographic characteristics and PAC score. Mean score of PAC was found to be significantly high among young adult PLWHA (P<0.0001), female (P=0.003), unmarried (P=0.010), those with higher-level education status (P=0.007), those with high-risk behavior practices (P=0.034), and those PLWHA who were diagnosed as having HIV infection for <3 years (P<0.0001). However, there was no significant difference in PAC scores according to place of residence.
Difference in disclosure concern (DC) scores according to sociodemographic and clinical characteristics
Table 6 summarizes the relation between sociodemographic characteristics and DC score. There was a statistically significant variation in DC scores with regard to age group, marital status, education, and time of HIV diagnosis, that is, P<0.0001. DC score was significantly high among adult PLWHA who were younger, unmarried, highly educated, and diagnosed as having HIV for <3 years. On the other hand, no significant difference in DC score was found in terms of sex, residence, and high-risk behavior practices.
Difference in ES scores according to sociodemographic and clinical characteristics
Table 7 shows the difference in ES scores according to sociodemographic and clinical characteristics. There was statistically significant difference in ES score with regard to marital status (P=0.003) and sex (P=0.024). ES mean score was significantly high among divorced/separated and female adult PLWHA.
Difference in overall stigma scores according to sociodemographic and clinical characteristics
Difference in overall stigma scores according to sociodemographic and clinical characteristics is displayed in Table 8. Significant difference was observed in age groups, marital status, educational status, and time of HIV diagnosis, that is, P<0.05. Significant overall stigma mean score was higher among younger adult (20–29 years), divorced/separated, highly educated adult PLWHA, and those diagnosed with HIV >3 years ago. On the other hand, the mean score of sex as well as high-risk behavior practices was found to be almost similar.
Discussion
The study focused on the perceived stigma level of PLWHA residing in Pokhara, Nepal. As far as the sociodemographic characteristics of the adult PLWHA are concerned, the study indicates that the mean age calculated was 39.04 years, where 27.3% of PLWHA were of 40–49 years old, 50.7% were females, 46.5% were janajati, 63.1% were residing in urban area, and 67.7% were married. The group was predominantly literate (86.2%), and among them 54.3% were unemployed.
Regarding the time of HIV diagnosis, 68.1% adult PLWHA were diagnosed as HIV positive since >3 years ago. Among them, 48.2% tested their HIV during treatment of other illnesses due to HIV-related symptoms. Concerning the high-risk behavior practices, 45.0% was in sexual relationship with multiple partners.
The primary finding of the current study revealed that high level of overall stigma was prevalent among 46.1% of adult PLWHA. Remaining 53.9% of PLWHA had low level of overall stigma. Similarly, a majority (83.3%) of adult PLWHA had high level of PAC followed by DC (68.1%) and NSI (59.9%), whereas only 25.4% of adult PLWHA had a higher level of ES. It reveals that fear of being stigmatized is more than actual stigma experience.
Similar to the study of Oli and Onta, many participants experienced internalized stigma related to their HIV status.9 This finding is also consistent with the results from a study in Kenya using the PLHIV Stigma Index.15 An important observation of the study is that the level of experience of most types of internalized stigma is much higher than the levels of external stigma (ES) and discrimination experienced.
Relationship of felt stigma with sociodemographic and clinical characteristics
Stigma against PLWHA remains one of the central barriers to effective prevention, treatment, and care of HIV. Internalized/felt stigma is said to be harsher than ES and its effects are very devastating to PLWHA if it remains unresolved.
The mean score ± SD of domains of felt stigma, that is, NSI, PAC, and DC were 2.79±0.70, 3.09±0.52, and 3.02±0.88, respectively. This study shows that there was significant difference in mean scores of all domains of felt stigma with younger age group, single/divorced, highly educated, and recently HIV-diagnosed PLWHA. Moreover, PAC mean score was significantly different with female PLWHA and those who were involved in high-risk behavior practices.
A study in South Africa supports the findings of this study. It revealed that 43% of respondents reported that they had some experiences of internalized stigma. Internalized stigma had significant association with age (P<0.001), length of time living with HIV (P<0.001), relationship status (P<0.001), and high education (P<0.001).16 Inversely the South African married respondents had high personal stigma (NSI) mean score of 3.1 in comparison to unmarried (2.8) and unmarried with partner (2.6).17
This study depicts that regarding the age group, mean score of all domains of felt stigma was significantly high in younger (20–29 years) adult PLWHA. NSI being less in older adults might be due to the reason that older PLWHA had developed ways of managing life with HIV. Similar studies in Canada, Brazil, and New York found internalized stigma to be significantly lower in older adults compared to those younger than 40 years.6,18–20 In agreement with the results herein, other studies have reported that older people tend to divulge HIV status more frequently than do younger ones.21 Less disclosure by the young respondents was probably due to negative public attitude regarding cause of HIV, fear of exposure of their risky behavior, and fear of breakup in relationship. This finding is worrisome as due to less disclosure status by young adult PLHWA, there is a higher chance of transmission of HIV to unaffected sexual partner. Therefore, an interventional educational program targeting students and young people is necessary to promote disclosure.
Similarly, significant mean differences were observed in educational status in relation to NSI, PAC, and DC. It was revealed that higher the education, higher the mean score of NSI (3.20), PAC, (3.27), and DC (3.27). This study contradicts the findings of many studies that suggest that higher the education level, lower the felt stigma.22 Positive relation between DC and higher education level might be due to perceived susceptibility and perceived severity of stigma and fear of abandonment. So despite their higher knowledge, they still refuse to disclose their status.
The mean score of the domains of felt stigma of the adult PLWHA who were diagnosed with HIV before 3 years and after 3 years differed significantly. Same result has been obtained in the studies carried out in India, Chicago, and South Africa.6,17,23 More the time of HIV diagnosis, lower the internalized stigma.6,20 A study carried out in Chicago revealed that the most recently diagnosed HIV-positive young patients consistently reported higher levels of stigma on all scales and subscales when compared to those diagnosed more than a year ago.23 It might be partly due to increased acceptance of HIV because of the availability of more time and effectiveness of counseling. With more time people usually learn to live their life even in difficult circumstances in acceptance level, as the patients’ coping increases with time.
The difference in the mean score of marital status was found to be statistically significant in the domains of NSI (P<0.0001), PAC (P=0.010), and DC (P<0.0001). Mean score of NSI, DC, and PAC was high in unmarried followed by divorced, married, and widower/widowed. It means that felt stigma is high in unmarried adult PLWHA. Similar findings have been found in other studies in DC and PAC domain24 but regarding NSI finding was refuted.6
In this study female PLWHA had a high mean score of NSI (2.82) and DC (3.08) than male adult PLWHA though no statistical differences were found, while in the domain of PAC, statistically significant (P=0.003) differences were present in sex. A study in New York city and Nigeria revealed that NSI was high in female,20,25 whereas the study in India, South Africa, and Nepal showed a contradictory result that male had high NSI in comparison to female.6,17,26
Considering the place of residence, a higher level of NSI was seen more in PLHWA who reside in urban area, which was significantly different (P=0.014), but the mean score of other domains of felt stigma based on the place of residence was not significantly different. Similarly, adult PLWHA involved in any one of the risk practices had statistically significant (P=0.034) PAC mean score but not in other domains. This concludes that NSI is high in those who reside in urban area, whereas PAC level is high in those involved in risk practices. However, many studies have not taken this variable into consideration.
Based on these findings, it can be concluded that internal stigma is very common among all adult PLWHA. The silence surrounding HIV virus and disease, along with the misconceptions and widely perceived negative risk factors associated with HIV/AIDS (eg, promiscuity, drug use) among both PLWHA and general population, might be the potential cause of felt stigma.
Relationship of ES with sociodemographic and clinical characteristics
When stigma is acted upon, the result is discrimination (ES). PLWHA are stigmatized and were looked at negatively by people at large. Discrimination and prejudice extend its reach to people associated with HIV-positive people in various levels in various places. ES against PLWHA is primarily due to low level of community awareness about the epidemic, sources of epidemic, routes of transmission, and prevention.27 A study carried out on discrimination of PLWHA in Asia Pacific, Caribbean, Europe, North America, and South America revealed that between 5% and 30% of respondents (depending on the geographical region) had perceived or experienced exclusion from taking part in family and social interactions, love and sexual relationships, work, and education. Two percent of respondents in developed countries and 6.5% in the rest of the world are physically assaulted by perpetrators including family members, medical authorities, and police.28
This study was carried out among 282 adult PLWHA though the ES was measured among those PLWHA who disclosed their seropositive status more than their spouse/partner, that is, 221 adult PLWHA. The overall mean ± SD score of ES among 221 adult PLWHA was 1.66±1.08. This study portrays that there is significant association between sex (P=0.024) and marital status (P=0.003) but not with other selected variables under study.
In this study mean score of ES was high in female (2.24) than male (2.01). A study carried by UNAIDS in Asian countries (Bangladesh, Cambodia, China, Fiji, Myanmar, Pakistan, the Philippines, Sri Lanka, and Thailand) also found that women were significantly more likely than men to experience HIV-related discrimination within their family and community.30 This might be due to existing social inequality/male-dominant society that makes women inferior to men thus getting less support and women become victims of their spouses’ irresponsible sexual behaviors. These findings were also supported by the studies in Nigeria, Uganda, India, and Thailand.25,30–32
It was found that ES mean score was high in divorced/separated (2.80) followed by widowed/widower (2.27), married (2.05), and unmarried respondents (1.98). It revealed that the highest ES was seen among those respondents who were not residing with their partners. This finding is supported by a study carried out in Central China. A study in South Central China revealed that a high level of ES included lack of presence of a spouse or significant other (P=0.001), single/divorced, or widowed (P=0.001).33
In this study no significant differences (P>0.05) were observed with ES and other variables like age, educational status, place of residence, time of HIV diagnosis, and high-risk behavior practices. While considering sociodemographic conditions with ES, limited evidence has suggested that older adults experience greater stigma and disclose HIV status to fewer individuals than their younger counterparts.33 Moreover, a study carried out in Central China revealed that younger age in comparison with older age (P=0.03) and urban residence (P=0.003) had a higher level of ES.34 Similarly, a study in Nepal stated that more discrimination was experienced by those PLWHA who had been found to be HIV positive over 1 year ago than who were diagnosed <1 year.26 A study in South Africa found that the variables that make a significant contribution to ES are age group (t=−2.118; P=0.0357), disability (t=−3.517; P=0.0006), province (t=−3.197; P=0.0017), and whether the participant was living in an urban, town/village, or rural area (t=2.263; P=0.0250).35
This result might be due to the variation in disclosure status as limited adult PLWHA disclosed their status to others and many of them only disclosed their status to their partner and within close family members only with whom they had trust with disclosure of their serostatus.
Overall stigma
While going through all subscales by compiling the value, a difference in the magnitude of overall stigma was reported by age (P<0.0001), marital status (P<0.0001), educational status (P=0.041), and time of HIV diagnosis (P=0.003). Overall stigma mean score was significantly high among young adults (20–29 years), divorced/separated, PLWHA who had high-level education, and those who were diagnosed as having HIV >3 years ago. The lack of major differences in stigma score by respondent’s characteristics such as sex, place of residence, and risk practices was notable.
Conclusion
Given the prominence in findings, it is concluded that felt stigma level is high in comparison to ES, which has devastating effects on PLWHA. Practically, results of the study have their significance in adding valuable information to ART center as well as VCT center to intensify their effort on educating/counseling PLWHA, managing peer support group, and so on, which add self-image level of PLWHA to improve disclosure. Moreover, the findings of the study on ES guide the responsible authorities to educate PLWHA, advocating the right of PLWHA and fostering awareness and knowledge among the public. The findings can be ultimately used to inform programs and interventions to reduce stigma experienced by PLWHA.
Limitations
Comorbidity and disability status in relation with stigma were not included. Similarly, this study could not address the domain of ES properly as the respondents had limited disclosure status.
Recommendations
Qualitative and mixed method may be used to find out the in-depth feelings, perspectives, and experiences of PLWHA regarding stigma that quantitative aspect cannot reveal.
Acknowledgments
The authors would like to sincerely express their gratitude to TU IOM Pokhara Campus and Western Regional Hospital for providing opportunity for conducting research. Our sincere thanks to all PLWHA who participated in the study for their valuable information for the research.
Disclosure
The authors report no any conflicts of interest in this work.
References
Bank W. HIV/AIDS in Nepal. 2011. Available from: http://www.worldbank.org/en/news/feature/2012/07/10/hiv-aids-nepal. Accessed January 12, 2017. | ||
World Health Organization. HIV/AIDS; 2015. Available from: www.who.int:http://www.who.int/features/qa/71/en/. Accessed January 12, 2017. | ||
Rueda S, Mitra S, Chen S, et al. Examining the associations between HIV-related stigma and health outcomes in people living with HIV/AIDS: a series of meta-analyses. BMJ Open. 2016;6(7):e011453. | ||
UNAIDS [homepage on the Internet]. Confronting discrimination: overcoming HIV-related stigma and discrimination in health-care settings and beyond. Geneva: Joint United Nations Program on HIV/AIDS; 2017. Available from: http://www.unaids.org/sites/default/files/media_asset/confronting-discrimination_en.pdf. Accessed August 1, 2017. | ||
Gesesew HA, Tesfay Gebremedhin A, Demissie TD, Kerie MW, Sudhakar M, Mwanri L. Significant association between perceived HIV related stigma and late presentation for HIV/AIDS care in low and middle-income countries: a systematic review and meta-analysis. PLoS One. 2017;12(3):e0173928. | ||
Steward WT, Herek GM, Ramakrishna J, et al. HIV-related stigma: adapting a theoretical framework for use in India. Soc Sci Med. 2008;67(8):1225–1235. | ||
UNAIDS [homepage on the Internet]. An ambitious treatment target to help end the AIDS epidemic. Geneva: Joint United Nations program on HIV/AIDS; 2014. Available from: http://www.unaids.org/sites/default/files/media_asset/90-90-90_en.pdf. Accessed April 10, 2018. | ||
Joint United Nations Programme on HIV/AIDS. People Living with HIV Stigma Index: Asia Pacific Regional Analysis. Geneva, Switzerland: Joint United Nations Programme on HIV/AIDS; 2011. Available from: http://www.unaids.org/sites/default/files/media_asset/20110829_PLHIVStigmaIndex_en_0.pdf. Accessed December 28, 2017. | ||
Oli N, Onta SR. Self-perception of stigma and discrimination among men having sex with men. J Nepal Health Res Counc. 2012;10(22):197–200. | ||
Charles B, Jeyaseelan L, Pandian AK, Sam AE, Thenmozhi M, Jayaseelan V. Association between stigma, depression and quality of life of people living with HIV/AIDS (PLHA) in South India - a community based cross sectional study. BMC Public Health. 2012;12:463. | ||
Neupane D, Khanal V, Sharma S, Aro AR. Perceived discrimination among people living with HIV in Nepal. J Nepal Health Res Counc. 2012;10(21):136–140. | ||
Rongkavilit C, Wright K, Chen X, Naar-King S, Chuenyam T, Phanuphak P. HIV stigma, disclosure and psychosocial distress among Thai youth living with HIV. Int J STD AIDS. 2010;21(2):126–132. | ||
Bunn JY, Solomon SE, Miller C, Forehand R. Measurement of stigma in people with HIV: a reexamination of the HIV stigma scale. AIDS Educ Prev. 2007;19(3):198–208. | ||
Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Res Nurs Health. 2001;24(6):518–529. | ||
National Aids Control Council. The National HIV and AIDS Stigma and Discrimination Index – Summary Report. Nairobi, Kenya: National Aids Control Council; 2014. Available from: https://reliefweb.int/sites/reliefweb.int/files/resources/HIV%20stigma%20index.pdf. Accessed January 28, 2017. | ||
Human Science Research Council. The People Living with Stigma Index: South Africa. Cape Town, South Africa: Human Science Research Council; 2015. Available from: http://www.stigmaindex.org/sites/default/files/reports/Summary-Booklet-on-Stigma-Index-Survey%20South%20Africa.pdf. Accessed January 28, 2017. | ||
Visser MJ, Makin JD, Vandormael A, Sikkema KJ, Forsyth BW. HIV/AIDS stigma in a South African community. AIDS Care. 2009;21(2):197–206. | ||
Emlet CA, Brennan DJ, Brennenstuhl S, Rueda S, Hart TA, Rourke SB. The impact of HIV-related stigma on older and younger adults living with HIV disease: does age matter? AIDS Care. 2015;27(4):520–528. | ||
Kerrigan D, Stigma BFI, Vazzano AA, Bertoni N, Malta M. Stigma, discrimination and HIV outcomes among people living with HIV in Rio de Janeiro, Brazil: the intersection of multiple social inequalities. Int J Res Pol Pract. 2015;18(2):1–15. | ||
Radcliffe S, Neaigus A, Bernard MA, Shepard C. HIV-related stigma in a New York City sample of adults in outpatient care for HIV infection: a short report. AIDS Care. 2015;27(9):1156–1161. | ||
Jimenez J, Morales M, Castro E. Levels of felt stigma among a group of people with HIV in Puerto Rico. P R Health Sci J. 2012;31(2):64–70. | ||
Rivera AV, Decuir J, Crawford ND, Amesty S, Harripersaud K, Lewis CF. Factors associated with HIV stigma and the impact of a nonrandomized multi-component video aimed at reducing HIV stigma among a high-risk population in New York City. AIDS Care. 2015;27(6):772–776. | ||
Dowshen N, Binns HJ, Garofalo R. Experiences of HIV-related stigma among young men who have sex with men. AIDS Patient Care STDS. 2009;23(5):371–376. | ||
Ebuenyi ID, Ogoina D, Ikuabe PO, Harry TC, Inatimi O, Chukwueke OU. Prevalence pattern and determinants of disclosure of HIV status in an anti retroviral therapy clinic in the niger delta region of Nigeria. Af J Infect Dis. 2014;8(2):27–30. | ||
Blessed NO, Ogbalu AI. Experience of HIV-related stigma by people living with HIV/AIDS (PLWHA), based on gender: a case of PLWHA attending clinic in the federal medical center, Owerri, IMO states, Nigeria. J Public Health Epidemiol. 2013;1(1):32–36. | ||
Family Planning Association of Nepal. The People Living with HIV Stigma Index Nepal. Harihar Bhawan, Lalitpur: Family Planning Association of Nepal; 2011. Available from: http://www.stigmaindex.org/nepal. Accessed August 22, 2017. | ||
Song JY, Lee JS, Seo YB, et al. Depression among HIV-infected patients in Korea: assessment of clinical significance and risk factors. Infect Chemother. 2013;45(2):211–216. | ||
Global Network of People Living with HIV. HIV Related Stigma Measures & Measurement Tools. Amsterdam, The Netherlands: Global Network of People Living with HIV; 2010. Available from: http://www.gnpplus.net/resources/hiv-related-stigma-measures-and-measurement-tools/. Accessed January 22, 2017. | ||
Joint United Nations Programme on HIV/AIDS. People Living with HIV Stigma Index. Geneva, Switzerland: Asia Pacific Regional Analysis; 2011. Available from: http://www.unaids.org/sites/default/files/media_asset/20110829_PLHIVStigmaIndex_en_0.pdf. Accessed January 28, 2017. | ||
Kuteesa MO, Wright S, Seeley J, et al. Experiences of HIV-related stigma among HIV-positive older persons in Uganda – a mixed methods analysis. SAHARA J. 2014;11(1):126–137. | ||
Bharat S. India: HIV and AIDS-Related Discrimination, Stigmatization and Denial; 2010. Available from: http://data.unaids.org/Publications/IRC-pub02/JC587-India_en.pdf. Accessed December 22, 2016. | ||
Pannetier J, Lelievre E, Coeur SL. HIV-related stigma experiences: understanding gender disparities in Thailand. AIDS Care. 2015;28(2):170–178. | ||
Nattabi B, Li J, Thompson SC, Orach CG, Earnest J. Factors associated with perceived stigma among people living with HIV/AIDS in post-conflict Northern Uganda. AIDS Educ Prev. 2011;23(3):193–205. | ||
Li X, Wang H, Williams A, He G. Stigma reported by people living with HIV in South Central China. J Assoc Nurses AIDS Care. 2009;20(1):22–30. | ||
Dos Santos MML, Kruger P, Mellors SE, Wolvaardt G, van der Ryst E. An exploratory survey measuring stigma and discrimination experienced by people living with HIV/AIDS in South Africa: the people living with HIV stigma index. BMC Public Health. 2014;14:80. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.





