Back to Journals » OncoTargets and Therapy » Volume 9
Pemetrexed had significantly better clinical efficacy in patients with stage IV lung adenocarcinoma with susceptible EGFR mutations receiving platinum-based chemotherapy after developing resistance to the first-line gefitinib treatment
Authors Yang C, Tsai M, Hung J, Liu T, Chou S, Lee J, Hsu J, Tsai Y, Huang M, Chong I
Received 9 November 2015
Accepted for publication 19 January 2016
Published 16 March 2016 Volume 2016:9 Pages 1579—1587
DOI https://doi.org/10.2147/OTT.S100164
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Min Li
Chih-Jen Yang,1–4 Ming-Ju Tsai,2,4 Jen-Yu Hung,2,3 Ta-Chih Liu,3,5 Shah-Hwa Chou,3,6 Jui-Ying Lee,6 Jui-Sheng Hsu,3,7 Ying-Ming Tsai,1,2,4 Ming-Shyan Huang,2–4 Inn-Wen Chong2,3
1Department of Internal Medicine, Kaohsiung Municipal Ta-Tung Hospital, 2Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Kaohsiung Medical University Hospital, 3Faculty of Medicine, College of Medicine, 4Graduate Institute of Medicine, College of Medicine, 5Division of Hematology and Oncology, Department of Internal Medicine, Kaohsiung Medical University Hospital, 6Division of Chest Surgery, Department of Surgery, Kaohsiung Medical University Hospital, 7Department of Medical Imaging, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Kaohsiung, Taiwan
Background: Increased evidences show that epidermal growth factor receptor (EGFR)-tyrosine kinase inhibitors such as gefitinib could prolong progression-free survival (PFS) compared with cytotoxic chemotherapy for metastatic lung nonsquamous cell carcinoma harboring susceptible EGFR mutation, and gefitinib was served as the first-line therapy. However, acquired resistance is inevitable, but the salvage therapies are still unclear.
Patients and methods: We designed a retrospective study of the salvage therapy and enrolled patients with stage IV lung adenocarcinoma who had mutated EGFR and developed an acquired resistance to the first-line gefitinib in two university-affiliated hospitals in Taiwan during June 2011 to December 2014. Age, sex, smoking history, EGFR gene mutation, performance statuses, response rate, PFS2 (the PFS in salvage therapy), and overall survival (OS2, the OS in salvage therapy) were recorded.
Results: Two hundred and nine patients with mutated EGFR and who took gefitinib as first-line therapy were identified in the period, and a total of 98 patients who had been treated with salvage therapy with cytotoxic chemotherapy or erlotinib were eligible for this study. The overall response rate of second salvage therapy is 13%, and none of them received erlotinib. Patients who received chemotherapy had a trend for better PFS2 than those who received erlotinib (4.3 months vs 3.0 months, P=0.1417) but not in OS. Furthermore, patients who received platinum-based doublet had a trend for better PFS2 and a significantly better OS2 than those who received chemotherapy without platinum (PFS2: 4.9 months vs 2.6 months, P=0.0584; OS2: 16.1 months vs 6.7 months, P=0.0007). Analyses of the patients receiving platinum-based doublet showed that patients receiving pemetrexed had a significantly better PFS2 (6.4 months vs 4.1 months, P=0.0083) and a trend for better OS2 than those without pemetrexed treatment.
Conclusion: Pemetrexed-based platinum chemotherapy may be the most optimal therapy in acquired resistance to gefitinib. Further prospective randomized controlled study is needed urgently.
Keywords: epidermal growth factor receptor, gefitinib, acquired resistance, pemetrexed, chemotherapy
Introduction
Lung cancer continues to be the leading cause of death among patients with malignant tumors worldwide. In 2004, mutations in epidermal growth factor receptor (EGFR) that cause oncogene addiction to EGFR were discovered in non-small-cell lung cancer (NSCLC), and these mutations have been found to be strongly associated with the susceptibility to EGFR-tyrosine kinase inhibitors (TKIs).1–4 Several Phase III studies showed that EGFR-TKIs were associated with a good response rate of approximately 70% and a progression-free survival (PFS) of 8–13 months in patients with NSCLC harboring EGFR-activating mutations.5–8 These outcomes were much better than those receiving cytotoxic chemotherapy as the first-line therapy.
However, the development of acquired resistance to the first-line EGFR-TKI treatment is inevitable, and most of these patients needed subsequent salvage therapy. Some new drugs were designed to conquer the mechanism of acquired resistance such as T790M mutation or MET amplification, and the associated clinical trials were still ongoing.9–13 In clinical practice, most of these therapies are still not available. Therefore, several retrospective studies were designed to explore the optimal second-line salvage therapy, whereas the results were discrepant.13–15 Because of the enrollment of heterogeneous study populations (including patients having NSCLC with or without EGFR mutations and even those with unknown EGFR mutation status), these studies showed variable outcomes and are, therefore, difficult to be applied to the daily clinical practice. After being covered as the first-line therapy to treat advanced lung adenocarcinoma harboring EGFR mutation by the National Health Insurance since June 2011, gefitinib has been the most popular first-line EGFR-TKI in Taiwan. Therefore, we conducted a retrospective study in two university-affiliated hospitals to elucidate the best second-line salvage treatment for these patients with stage IV lung adenocarcinoma with susceptible EGFR mutation who had disease progression during gefitinib treatment. This study demonstrated the real-world data of the second-line salvage therapy in patients with EGFR-mutated lung adenocarcinoma after gefitinib failure in Taiwan.
Patients and methods
Patient identification
In this retrospective study, patients with stage IV lung adenocarcinoma diagnosed between October 2009 and January 2015 in two university-affiliated hospitals (Kaohsiung Medical University Hospital [KMUH] and Kaohsiung Municipal Ta-Tung Hospital) in Taiwan were identified and followed-up until August 12, 2015. Patients who had susceptible EGFR mutation and received gefitinib as the first-line therapy were enrolled. The diagnosis of lung cancer was confirmed pathologically according to World Health Organization pathology classification, and the tumor staging was made according to the seventh American Joint Committee on Cancer staging system by a special committee including clinical pulmonologists, medical oncologists, chest surgeons, radiologists, pathologists, and radiation oncologists. Patients were included if they 1) had adequate tumor specimens for EGFR mutation examination and had susceptible EGFR mutation, including exon 18 point mutation, exon 19 deletion, and exon 21 point mutation; 2) were treated with gefitinib as the first-line therapy; and 3) subsequently received a second-line treatment. Those who had previous history of other malignancies were excluded.
Baseline clinical characteristics were determined by retrospective chart review, including age at diagnosis, sex, Eastern Cooperative Oncology Group performance status at the beginning of the gefitinib treatment and at the start of the second-line treatment, smoking history, and tumor histology. Smoking history was categorized as current smokers or ever smokers, which included ex-smokers (who had quit ≥5 years before diagnosis) and never smokers (<100 lifetime cigarettes). Mutations in the EGFR gene were analyzed using an EGFR RGQ kit (Qiagen NV, Venlo, the Netherlands), which utilized amplification refractory mutation-specific polymerase chain reactions and Scorpion technologies for detection and/or direct sequencing. The detection method was developed and validated by the Division of Molecular Diagnostics, Department of Laboratory Medicine, KMUH.
An initial treatment response was classified as complete response (CR), partial response (PR), stable disease, or progressive disease based on serial imaging studies using the revised Response Evaluation Criteria in Solid Tumors (RECIST 1.1) criteria.16 The response rate and disease control rate were defined as the percentages of patients with CR and PR and with CR, PR, and stable disease, respectively.
The second-line salvage therapy included erlotinib and cytotoxic chemotherapy, including pemetrexed, gemcitabine, vinorelbine, and taxanes (docetaxel), with or without platinum derivatives (cisplatin or carboplatin). The duration between the start of the second-line treatment to the date of disease progression thereafter and to the date of death were defined as PFS2 and overall survival (OS2).
The Institutional Review Board (IRB) of KMUH approved this study (KMUHIRB-E[II]-20150162) and waived the need for written informed consent from the participants due to the retrospective nature of this study.
Statistical analysis
Age, sex, smoking history, EGFR gene mutation site (exon 18, exon 19, and exon 21), thyroid transcription factor 1 immunostaining, metastatic sites on initial diagnosis, performance statuses when starting the treatments, and initial treatment responses were summarized and compared between patients receiving different second-line treatments. Categorical variables and continuous variables were compared using the χ2-test and the Student’s t-test, respectively. Survival times were estimated using the Kaplan–Meier method, with differences between the groups compared using the log-rank test. Cox proportional hazards regression analysis was used to identify the effect of different clinical features on PFS2 and OS2, and the results were presented as hazard ratio (HR) with 95% confidence interval (CI). After univariate analyses, all variables were included to obtain a maximal model of multivariable analysis to assess the independent effect of different variables. All statistical analyses were performed using SAS software (Version 9.3 for Windows; SAS Institute Inc., Cary, NC, USA). Statistical significance was set at a two-sided P-value of <0.05.
Results
Patient characteristics
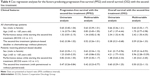
A total of 209 patients with stage IV adenocarcinoma harboring susceptible EGFR gene mutations who had been treated with gefitinib as the first-line treatment were identified. After excluding those who remained on gefitinib treatment and those who did not received erlotinib or cytotoxic chemotherapy as the second-line treatment after gefitinib failure, the remaining 98 patients were included for analyses. As shown in Table 1, 12 (12%), 26 (27%), and 60 (61%) patients received erlotinib, chemotherapy without platinum, and platinum-based doublet as their second-line treatment after gefitinib failure, respectively. In the 60 patients who received platinum-based doublet, 34 (57%) of them received pemetrexed (Table 1).
  | Table 1 Regimens used as the second-line treatment after gefitinib failure |
The clinical characteristics and treatment responses of all patients were summarized in Tables 2 and 3. No significant difference was noted in the baseline characteristics between patients receiving erlotinib and those receiving chemotherapy as the second-line treatment (Table 1). However, the disease control rate was significantly higher in those receiving chemotherapy than in those receiving erlotinib (79% vs 50%, P=0.0283). Although no significant differences in PFS2 and OS2 were noted between those receiving chemotherapy and those taking erlotinib, patients receiving chemotherapy had a trend for better PFS2 (median of PFS2: 4.3 months vs 3.0 months, log-rank P=0.1417) (Figure 1A and B).
To identify the chemotherapy regimen with better outcome, we performed further analyses with the 86 patients receiving chemotherapy as the second-line treatment, including 60 (70%) and 26 (30%) patients receiving platinum-based doublets and chemotherapy without platinum, respectively. As expected, those receiving platinum-based doublets were significantly younger in age than those receiving chemotherapy without platinum (P<0.0001), whereas no significant difference in the performance status was noted between groups (Table 3). The disease control rate was significantly higher in those receiving platinum-based doublet than in those receiving chemotherapy without platinum (90% vs 54%, P=0.0002) (Table 3). Patients receiving platinum-based doublet had a trend for better PFS2 and a significantly better OS2 than those receiving chemotherapy without platinum (median PFS2: 4.9 months vs 2.6 months, log-rank P=0.0584; median OS2: 16.1 months vs 6.7 months, log-rank P=0.0007) (Figure 1C and D). Cox regression analyses showed that platinum-based doublet was associated with a borderline effect for better PFS2 (HR: 0.52 [95% CI: 0.26–1.01], P=0.0545), after controlling for sex, age, and performance status while starting the second-line treatment (Table 4). Platinum-based doublet was associated with a significantly better OS2 on the univariate analysis (HR: 0.38 [95% CI: 0.21–0.68], P=0.0011), whereas the significance was not seen in the multivariable analysis controlling for sex, age, and performance status while starting the second-line treatment (HR: 0.59 [95% CI: 0.26–1.33], P=0.2021).
We further investigated whether pemetrexed provides better effect than other chemotherapy agents in the 60 patients receiving platinum-based doublet. The baseline characteristics were similar between patients receiving a platinum derivative with pemetrexed and those receiving a platinum derivative with cytotoxic chemotherapeutic agents other than pemetrexed (Table 3), while patients receiving a platinum derivative with pemetrexed had longer progression-free survival on gefitinib treatment. The disease control rate and response rate were similar in both groups (Table 3). In patients receiving platinum-based doublet, those receiving pemetrexed had a significantly better PFS2 and a trend for better OS2 than those without pemetrexed treatment (median PFS2: 6.4 months vs 4.1 months, log-rank P=0.0083; median OS2: 19.2 months vs 14.1 months, log-rank P=0.1639) (Figure 1E and F). Cox regression analyses showed that pemetrexed, as compared with other cytotoxic chemotherapeutic agents, was associated with a significantly better PFS2 (HR: 0.47 [95% CI: 0.26–0.84], P=0.0101) and a trend for better OS2 (HR: 0.50 [95% CI: 0.22–1.13], P=0.0972), after controlling for sex, age, and performance status while starting the second-line platinum-based doublet treatment (Table 4).
Discussion
Our study is one of the largest retrospective studies to investigate the treatment strategies for patients who initially harbored susceptible EGFR mutation and developed an acquired resistance to the initial EGFR-TKI treatment. For patients with stage IV adenocarcinoma harboring susceptible EGFR mutation who developed acquired resistance to the first-line gefitinib treatment, cytotoxic chemotherapy seemed more effective than a subsequent EGFR-TKI as the second-line salvage therapy. Platinum-based doublet chemotherapy was superior to non-platinum-based chemotherapy in terms of disease control rate, PFS2, and OS2. Among patients receiving platinum-based doublet, pemetrexed seemed better than other cytotoxic chemotherapeutic agents in terms of PFS2. Therefore, a platinum derivative with pemetrexed might be the best regimen for second-line salvage therapy.
Because of its great efficacy shown by several Phase III prospective studies, gefitinib has been covered by the National Health Insurance in Taiwan since June 2011 as the first-line treatment for patients with advanced lung adenocarcinoma harboring susceptible EGFR mutation. As a result, most of these patients received gefitinib as the first-line therapy in Taiwan. Despite gefitinib showed good efficacy and longer PFS than cytotoxic chemotherapy in this population, acquired resistance to EGFR-TKI almost always eventually occurred, resulting in the need of subsequent salvage therapy. Some strategies to overcome acquired resistance were proposed, including new-generation EGFR-TKIs for T790M mutation, MET inhibitors for MET amplification, and so on. However, these treatment strategies are still under investigation and are not currently available in daily clinical practice. In the real world, the lack of an established therapeutic strategy for patients with NSCLC who have disease progression after receiving the first-line EGFR-TKI treatment remains a great challenge for physicians. Shifting to erlotinib after gefitinib failure had been proposed but had modest efficacy,8,17,18 as shown in our study. Cytotoxic chemotherapy, based on the current concept, is the optimal salvage therapy to these patients with acquired resistance, and the researchers were trying to identify the best regimens to improve the outcome.
Several retrospective studies were designed to explore the most optimal salvage therapy for patients with advanced NSCLC, while most of them enrolled unselected patients (including those with mutated, nonmutated, and unknown EGFR mutation status).10,14,15,19 Kuo et al showed that patients who received cytotoxic chemotherapy had better PFS and OS than those who just received best supportive care. Furthermore, they also indicated that patients who received taxane-based subsequent chemotherapy exhibited a higher response rate (48.7%), higher disease control rate (79.5%), longer PFS (median: 5.1 months), and longer OS (median: 12.7 months) than those who received non-taxane-based regimens, including pemetrexed-based therapy.14 In contrast to their study, we found no significant difference in PFS and OS in patients receiving chemotherapy with or without taxanes as the second-line treatment (data not shown).
Wu et al10 showed that the salvage platinum-based chemotherapy was associated with a better OS than non-platinum-based chemotherapy (median: 21.7 months vs 8.9 months, P=0.006). In line with their finding, our study showed a trend for better PFS and a significantly longer OS in patients receiving platinum-based chemotherapy than those receiving non-platinum-based chemotherapy. Wu et al10 also indicated that platinum-based chemotherapy with gemcitabine provided longer OS than platinum-based therapy with taxane did. Kim et al15 suggested that pemetrexed-based therapy provided significantly longer OS (18.5 months vs 8.5 months, P=0.008) in unselected patients, while EGFR mutation status was unknown in most of them. In contrast to these studies enrolling unselected patients, we found that the pemetrexed use, along with platinum-based doublet, was associated with a significantly longer PFS and a trend for better OS in patients with stage IV lung adenocarcinoma with susceptible tumor EGFR mutation who received platinum-based doublet after gefitinib failure.
Recently, some studies enrolled patients who had tumors with EGFR mutation and received EGFR-TKI as the first-line therapy. Tseng et al11 indicated that using cytotoxic chemotherapy as the second-line therapy resulted in a median PFS of 4.5 months and OS of 14.6 months. Similarly, this study showed that patients treated with cytotoxic chemotherapy as the second-line treatment after gefitinib failure had a median PFS of 4.3 months and OS of 14.6 months.
Pemetrexed is a multiple antifolate drug for nonsquamous cell NSCLC and is currently regarded as one of the most effective and safest cytotoxic chemotherapeutic agents. Clinical trials showed that pemetrexed-based chemotherapy provided longer PFS and OS than gemcitabine-based chemotherapy did, while the regimen was used as the first-line therapy for patients with advanced NSCLC.20 Basically, high-level expression of thymidylate synthase in NSCLC conferred a reduced susceptibility to pemetrexed.21–23 However, NSCLC harboring EGFR mutation had decreased the expression of thymidylate synthase,24 which might lead to a better response to pemetrexed.25 Indeed, Park et al19 recently showed that pemetrexed used alone as a salvage drug after gefitinib failure provided significantly longer PPS than platinum-based doublet chemotherapy did (PFS: 4.2 months vs 2.7 months, P=0.008). Tseng et al11 also demonstrated that chemotherapy with pemetrexed as the second-line chemotherapy for patients having acquired resistance to the first-line EGFR-TKI seemed to provide better PFS (4.7 months vs 3.3 months, P=0.62) and better OS (15.1 months vs 8.1 months, P=0.17) than chemotherapy without pemetrexed did, but the differences were nonsignificant and inconclusive. In our study population, chemotherapy with pemetrexed was associated with a significantly longer PFS and OS in patients with stage IV lung adenocarcinoma receiving salvage chemotherapy as the second-line treatment after gefitinib failure (data not shown). Furthermore, in patients receiving platinum-based doublet as the second-line treatment, pemetrexed, along with a platinum derivative, provided a significantly longer PFS and a trend for better OS. Therefore, platinum-based doublet with pemetrexed might be the most optimal regimen for patients with stage IV lung adenocarcinoma with acquired resistance to gefitinib. Further prospective randomized studies might be needed to confirm our findings.
There were several limitations in this study. First, our study was a retrospective study, and selection bias was inevitable. Also, due to the retrospective nature of this study, almost no rebiopsy specimens were collected from the patients after developing acquired resistance to gefitinib, so the molecular mechanism underlying our findings could not be assessed. However, this retrospective study demonstrated the clinical conditions in the real world. Second, only patients with stage IV lung adenocarcinoma harboring susceptible EGFR mutation who received gefitinib as their first-line treatment were included in our analyses. Several EGFR-TKIs available nowadays, such as gefitinib, erlotinib, and afatinib, had different potency, resulting in different PFS and OS. Therefore, it remained questionable whether our findings could be applied in patients with stage IIIB adenocarcinoma, in patients with NSCLC other than adenocarcinoma, or in patients receiving EGFR-TKI other than gefitinib. However, the inclusion of a specific population receiving gefitinib as the first-line treatment reduced the heterogeneity of our study population, resulting in easier application of the results in daily clinical practice.
Conclusion
Our study demonstrated the real-world data in Taiwan, showing that platinum-based doublet chemotherapy with pemetrexed might be the most optimal second-line treatment for patients with stage IV adenocarcinoma harboring susceptible EGFR mutation after gefitinib failure. Further prospective studies are required to confirm our findings and uncover the underlying mechanisms.
Acknowledgments
The authors express their gratitude to the staff of the Statistical Analysis Laboratory, Department of Medical Research, Kaohsiung Medical University Hospital, Kaohsiung Medical University for their assistance. In addition, the authors also thank Dr Wu Kuan-Li for his kind assistance in data collection and study design.
Disclosure
The authors report no conflicts of interest in this work.
References
Costa DB, Kobayashi S, Tenen DG, Huberman MS. Pooled analysis of the prospective trials of gefitinib monotherapy for EGFR-mutant non-small cell lung cancers. Lung Cancer. 2007;58(1):95–103. | ||
Sequist LV, Martins RG, Spigel D, et al. First-line gefitinib in patients with advanced non-small-cell lung cancer harboring somatic EGFR mutations. J Clin Oncol. 2008;26(15):2442–2449. | ||
Gridelli C, De MF, Di MM, Cortinovis D, Cappuzzo F, Mok T. Gefitinib as first-line treatment for patients with advanced non-small-cell lung cancer with activating epidermal growth factor receptor mutation: review of the evidence. Lung Cancer. 2011;71(3):249–257. | ||
Paez JG, Janne PA, Lee JC, et al. EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science. 2004;304(5676):1497–1500. | ||
Mok TS, Wu YL, Thongprasert S, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med. 2009;361(10):947–957. | ||
Maemondo M, Inoue A, Kobayashi K, et al; North-East Japan Study Group. Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med. 2010;362(25):2380–2388. | ||
Mitsudomi T, Morita S, Yatabe Y, et al; West Japan Oncology Group. Gefitinib versus cisplatin plus docetaxel in patients with non-small-cell lung cancer harbouring mutations of the epidermal growth factor receptor (WJTOG3405): an open label, randomised phase 3 trial. Lancet Oncol. 2010;11(2):121–128. | ||
Rosell R, Carcereny E, Gervais R, et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol. 2012;13(3):239–246. | ||
Oxnard GR, Arcila ME, Chmielecki J, Ladanyi M, Miller VA, Pao W. New strategies in overcoming acquired resistance to epidermal growth factor receptor tyrosine kinase inhibitors in lung cancer. Clin Cancer Res. 2011;17(17):5530–5537. | ||
Wu JY, Shih JY, Yang CH, et al. Second-line treatments after first-line gefitinib therapy in advanced nonsmall cell lung cancer. Int J Cancer. 2010;126(1):247–255. | ||
Tseng YH, Hung HY, Sung YC, et al. Efficacy of chemotherapy in epidermal growth factor receptor (EGFR) mutated metastatic pulmonary adenocarcinoma patients who had acquired resistance to first-line EGFR tyrosine kinase inhibitor (TKI). J Chemother. Epub 2015 May 15. | ||
Engelman JA, Zejnullahu K, Mitsudomi T, et al. MET amplification leads to gefitinib resistance in lung cancer by activating ERBB3 signaling. Science. 2007;316(5827):1039–1043. | ||
Tartarone A, Lerose R. Clinical approaches to treat patients with non-small cell lung cancer and epidermal growth factor receptor tyrosine kinase inhibitor acquired resistance. Ther Adv Respir Dis. 2015;9(5):242–250. | ||
Kuo CH, Lin SM, Lee KY, et al. Subsequent chemotherapy improves survival outcome in advanced non-small-cell lung cancer with acquired tyrosine kinase inhibitor resistance. Clin Lung Cancer. 2010;11(1):51–56. | ||
Kim H, Yun T, Lee YJ, Han JY, Kim HT, Lee GK. Post-progression survival in patients with non-small cell lung cancer with clinically acquired resistance to gefitinib. J Korean Med Sci. 2013;28(11):1595–1602. | ||
Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–247. | ||
Cho BC, Im CK, Park MS, et al. Phase II study of erlotinib in advanced non-small-cell lung cancer after failure of gefitinib. J Clin Oncol. 2007;25(18):2528–2533. | ||
Horiike A, Yamamoto N, Tanaka H, et al. Phase II study of erlotinib for acquired resistance to gefitinib in patients with advanced non-small cell lung cancer. Anticancer Res. 2014;34(4):1975–1981. | ||
Park S, Keam B, Kim SH, et al. Pemetrexed singlet versus nonpemetrexed-based platinum doublet as second-line chemotherapy after first-line epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor failure in non-small cell lung cancer patients with EGFR mutations. Cancer Res Treat. 2015;47(4):630–637. | ||
Scagliotti GV, Parikh P, von PJ, et al. Phase III study comparing cisplatin plus gemcitabine with cisplatin plus pemetrexed in chemotherapy-naive patients with advanced-stage non-small-cell lung cancer. J Clin Oncol. 2008;26(21):3543–3551. | ||
Chen CY, Chang YL, Shih JY, et al. Thymidylate synthase and dihydrofolate reductase expression in non-small cell lung carcinoma: the association with treatment efficacy of pemetrexed. Lung Cancer. 2011;74(1):132–138. | ||
Wang L, Wang R, Pan Y, Sun Y, Zhang J, Chen H. The pemetrexed-containing treatments in the non-small cell lung cancer is -/low thymidylate synthase expression better than +/high thymidylate synthase expression: a meta-analysis. BMC Cancer. 2014;14:205. | ||
Takezawa K, Okamoto I, Okamoto W, et al. Thymidylate synthase as a determinant of pemetrexed sensitivity in non-small cell lung cancer. Br J Cancer. 2011;104(10):1594–1601. | ||
Giovannetti E, Lemos C, Tekle C, et al. Molecular mechanisms underlying the synergistic interaction of erlotinib, an epidermal growth factor receptor tyrosine kinase inhibitor, with the multitargeted antifolate pemetrexed in non-small-cell lung cancer cells. Mol Pharmacol. 2008;73(4):1290–1300. | ||
Wu SG, Yang CH, Yu CJ, et al. Good response to pemetrexed in patients of lung adenocarcinoma with epidermal growth factor receptor (EGFR) mutations. Lung Cancer. 2011;72(3):333–339. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.