Back to Journals » Patient Preference and Adherence » Volume 10
Patients’ attitudes to the use of modern technologies in the treatment of diabetes
Authors Cerna L, Maresova P
Received 25 July 2016
Accepted for publication 10 August 2016
Published 22 September 2016 Volume 2016:10 Pages 1869—1879
DOI https://doi.org/10.2147/PPA.S118040
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Lucie Cerna, Petra Maresova
Department of Economics, Faculty of Informatics and Management, University of Hradec Kralove, Hradec Kralove, Czech Republic
Background: The incidence of diabetes is rising across the world. This global problem significantly affects the economic and social development in the 21st century. If the disease is diagnosed in time, the number of complications as well as the costs of therapy will be lower. Modern technologies permeate all spheres of medicine, and diabetes treatment is no exception. Therefore, the aim of this article is to analyze patients’ attitudes to the use of modern technologies in the treatment of diabetes (type 1 diabetes mellitus [T1DM] and type 2 diabetes mellitus [T2DM]).
Methods: A total of 313 respondents from the Czech Republic in the period from June 24, 2015, to July 24, 2015, participated in a questionnaire survey. The target group was diabetics regardless of the type of illness. Collected data were analyzed using descriptive statistical methods, Z-test, and test of independence (Pearson’s chi-squared test).
Results: Although in other areas mobile applications are used to monitor patients’ health condition in ~30% of cases, in the case of diabetes they are used by only 4% of respondents. Approximately 8% of participants use an application, but they do not like it. The rest of the respondents have never used any mobile application. These low figures are due to a lack of knowledge about the availability and possibilities of mobile applications. A positive correlation was proven between technical skills and methods of entering data. Gender and age show only a weak dependency of the method of writing data on their own health condition. Furthermore, the monitored parameters show that patients with T1DM control and know more about their health condition than patients with T2DM, which is reflected, for example, by more frequent blood glucose measurements or larger track of their physical activity. Conversely, the relationship between the associated complications and self-care activities has not been demonstrated.
Conclusion: Despite the current fast development of modern technologies, these technologies are not frequently used in treating patients. The principal problem lies in patients’ low technological knowledge and their higher age, which makes learning new skills, including the use of modern technologies, more difficult.
Keywords: modern technologies, patients’ attitudes, diabetes mellitus, survey
Introduction
Diabetes mellitus (DM) is a chronic disease manifesting itself by a metabolic disorder, when sugar, fat, and proteins in organisms are not processed. The cause of diabetes is not known, but the trigger factors may be genetic predispositions, environmental effects (stress, virus infection, or obesity), or constitutional point factors (race, gender, or age). According to the causes, there are different types of diabetes: type 1 DM (T1DM), type 2 DM (T2DM), gestational diabetes, DM in chronic pancreas, and maturity-onset diabetes of the young (MODY) diabetes. Approximately 85%–90% of all patients with diabetes are patients with T2DM.1 The incidence of diabetes is rising across the world. Like other diseases,2,3 the treatment of diabetes significantly affects the economic and social expenditure of developed countries. According to the latest estimates of the International Diabetes Federation, 8.3% of adults suffer from this disease. At the same time, 175 million people with diabetes were not diagnosed. The high increase in prevalence and economic burden leads to efforts to seek more effective ways to treat and care for these people. In this way, a significant contribution can be the area called “mobile health” (mHealth). mHealth is one of the subcategories of the electronic health (eHealth). According to the World Health Organization, mHealth is defined as the practice of medicine through mobile devices.4 The mobile device may be a sensor, a wireless medical device, personal digital assistant, and similar devices. The use of mobile applications can help improve control of the disease, improve overall health, and delay associated complications.5,6 People suffering from diabetes have to monitor several factors, including blood glucose levels, weight, intake of carbohydrates, and insulin dosage. Self-monitoring of blood glucose is recognized by leading medical organizations as an important tool in the management of diabetes, particularly in insulin-treated patients.7 Large, randomized, controlled trials have clearly demonstrated a causal relationship between poor glycemic control and the development of microvascular disease.8 The link between effective management of diabetes and real macrovascular disease has also been established.9 Studies by Gaede et al9 showed that intensive management of all risk factors, including elevated lipids, blood pressure, and glycemia, results in significant beneficial effects on cardiovascular-related deaths.10
Keeping the record of all results is priceless as gathered data offer a complex view of the patient’s health state. The effectiveness and benefits of applying new web, mobile, and communication technologies in managing diabetes have been investigated in a number of studies.11–13 The review by El-Gayar et al14 showed that 74% of studies confirmed some form of added benefit. The Prospective Diabetes Study15,16 has shown that improved glycemic control is associated with sustained decreased rates of retinopathy, nephropathy, and neuropathy. In these trials, treatment regimens that reduced average A1C to ~7% (~1% above the upper limits of normal) were associated with fewer long-term microvascular complications; however, intensive control was found to increase the risk of severe hypoglycemia and weight gain.17,18 Epidemiological studies support the potential of intensive glycemic control in the reduction of cardiovascular diseases.7 Furthermore, the qualitative benefits in the life of people suffering from diabetes have been described. Van Damme et al19 acknowledged that better knowledge of the ways in which social support operated was vital for enhancing diabetes patient self-care, ensuring adherence to advice from professionals, encouraging lifestyle changes, and helping to improve outcomes of care and increase personal freedom. Donald et al20 noted that young adults with diabetes had expressed an interest in email and mobile text messaging in earlier studies to enhance disease management and that text messaging had been proven to be beneficial as a possible motivational tool.
There are also a number of studies examining not only the impacts themselves but also the expectations and knowledge of patients on medical mobile technologies.21 The dependencies of the selected characteristics of patients on the access to the use of modern technologies in the treatment have also been investigated.
In the study by Anglada-Martínez et al,22 they solved the question of the expectation of technology, in addition to identifying values, beliefs, hopes, concerns, and needs related to the use of telemonitoring services. Participants expressed their opinion that technology can improve not only the physical management of the disease but also the social and psychological conditions.22 It has been revealed that age is an important barrier to smartphone use in health care. The main monitored indicators and key parameters in many studies related to diabetes include, of course, the type of diabetes, factors related to treatment such as the glycated hemoglobin (HbA1c) level, fasting blood glucose level, physical activity, insulin doses, and the health technologies used for monitoring.23 Chomutare et al21 drew attention to the fact that a wide selection of mobile applications seems to be available for people with diabetes, but the obvious gaps between evidence-based recommendations and the functionality used exist.21
The abovementioned information indicates both the usefulness of technology in the treatment of diabetes and the different effectiveness, given by the age and skills of users and the type of diabetes, which are related to different health monitoring needs of certain health parameters.
Therefore, the aim of this article is to analyze the attitudes of patients with diabetes to the use of mobile medical technologies.
In greater detail, the attention is focused on the following research questions (RQs):
- RQ1: Do patients know modern technologies for the control of diabetes?
- RQ2: Do patients with T1DM control and know about their health condition more than patients with T2DM?
- RQ3: Do patients with associated complications control and know about their health condition more than other patients with diabetes?
- RQ4: Is there any dependence between the level of HbA1c and record of blood glucose level, the frequency of measuring blood glucose level, the type of treatment (pump/pen), or controlling other aspects of health?
- RQ5: Is there any dependence between the assessment of technical skills and the type of record of blood glucose level?
- RQ6: Is there any dependence between the age of the patient and the type of record of blood glucose level?
Methods
Informed consent was obtained from the participants. The University of Hradec Kralove, Faculty of Informatics and Management review board waived the requirement for approval for this study. Respondents were members of online communities and they voluntarily participated in survey. The methods include a quantitative research and questionnaire survey. The questionnaire was divided into four parts. It consisted of 26 questions and two sub-questions. The first part was focused on general information, ie, age group and education. Another part consisted of eleven questions relating solely to diabetes treatment and self-monitoring. The next four questions investigated the sources of information and awareness of diabetes itself. The last set of questions concerned mobile applications. The target group was diabetics regardless of the type of illness from diabetes clinic in Hradec Kralove and from three online diabetic communities (the group of “T1DM” with ~1,500 members, “diabetes” with 600 members, and “the fullest with diabetes” with >3,000 members).
Finally, the questionnaire had the sample of 313 respondents, and the rate of return was 5%. The questionnaire was available via a unique IP address on the Web site Vyplnto.cz in the period from June 24, 2015, to July 24, 2015. The questionnaire used two main types of questions – closed and semi-opened – with multiple-choice answers. The options menu contained six to ten options. Furthermore, there were questions with yes/no answers, which were followed by other questions.
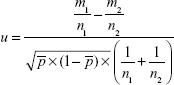
When analyzing dependencies, the conformity tests of the relative frequencies of two basic files were used (Z-test; RQ2–RQ3), where on the basis of sufficiently long-range choice (n1>100 and n2>100) and the number of the desired occurrence of m1 and m2 obtained from the two files, the differences of relative frequencies (probability of occurrence) of the given characteristic π1 and π2 of the two basic files were tested. Two types of alternative hypotheses were tested, namely right handed (RQ2) and both sided (RQ3). The calculation of the test criterion is based on the following statistics:
|
|
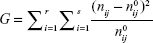
To verify RQ4–RQ6, tests of independence in the pivot table (Pearson’s chi-squared test) were carried out. This test assumes division of the basic files into k groups, according to certain statistical character. The test includes the input condition of use, and for its verification the following condition is sufficient: np(1−p) >5. The hypotheses are tested in the following form:
H0: pi = π0, i for all i ∈ {1,2,…, k} | (2) |
H1: pi ≠ π0, i for some i | (3) |
To calculate the test criterion, the following formula is used:
|
|
and with degrees of freedom df=k−1.
The result of the test criterion is compared with the critical value, which has the following form:  .
.
The null hypothesis is not rejected if  .
.
Conversely, the null hypothesis is rejected if  .24
.24
Results
Characteristics of respondents
A total of 313 patients with diabetes participated in this research (42% males and 58% females). Most of them were in the 50+ age group (48.6%) suffering from T2DM (127 respondents). Type 1 diabetics usually belonged to younger age groups. Although the sample of respondents in terms of the type of diabetes did not totally correspond with the distribution in the population (where there are significantly less patients with T1DM), it enables better testing of the diversity of approaches in some areas using selected statistical tests. Most respondents had a primary or secondary education (Table 1). Other types of diabetes were gestational diabetes (two respondents) and DM in chronic pancreas (one respondent).
  | Table 1 Basic characteristics of the respondents |
Subjective assessment of one’s technical skills was one of the first questions the patients were asked. It was an important factor having a significant impact on the patients using mobile applications during their treatment of diabetes. Most participants assessed themselves as users (61.7% of respondents) characterized as follows:
“I easily use basic functions of the device, have no problems with some complementary functions like various settings of the device, or installing applications.”
It is interesting to compare male and female respondents. Approximately 25% of females and only 15% of males assessed themselves as having basic knowledge (Table 1). On the other hand, 23% of males and only 13% of females assessed their skills as expert, and 74.6% of patients with T1DM and 50% of patients with T2DM have their own smartphone. This situation was different in relation to the glucose meter, where most respondents with T1DM and T2DM own this device.
Diabetes treatment
Most respondents suffer from diabetes for >10 years (41.5%), and 81% of patients do not have any other associated complications. The most commonly used medical devices include insulin pens and insulin pumps. HbA1c belongs among the main indicators of diabetes. Therefore, one of the most significant goals is to keep it low. It is important for the patient to know their HbA1c level. Table 2 suggests that most patients (88%) are aware of HbA1c. There are no significant differences between the T1DM and T2DM groups in this parameter (Table 2).
  | Table 2 Health information |
Patients’ attitudes to data recording
Every patient should keep a record of and analyze the data related to the course of their disease. There are a lot of ways of keeping this record, from paper documentation to downloading data to the computer or cell phone. Type 1 diabetics kept more records than type 2 diabetics, which can also be attributed to the requirements of the physician to the patient for treatment settings. Table 3 shows that 36% of patients with T2DM do not keep any record of their blood sugar concentration. They did not own any glucose meter (13% T2DM) or do not measure their concentrations. On the other hand, only 20% of patients with T1DM did not keep any record. Paper documentation was most common (56%).
  | Table 3 Patients’ attitude to data recording and personal monitoring |
The treatment of diabetes is more than just following blood glucose levels. It also involves monitoring one’s weight, intake of carbohydrates, insulin dosage, and physical activity. All these items of information make a complex picture of one’s health state. Results showed that only 40% of type 2 diabetics and 70% of type 1 diabetics monitor their intake of carbohydrates. This parameter is even the base for determining the number of insulin units to cover the body’s need for this hormone, which is very typical for patients treated with insulin. Being overweight is a frequent cause of T2DM, which makes it necessary to lose some weight in the initial phases of its treatment. Therefore, patients with T2DM should monitor not only carbohydrates but also the overall caloric values in foods and fats contained in them. Consequently, patients with T2DM monitor their weight more closely (78.6%).
Use of mobile applications in diabetes treatment
Mobile applications in treating diabetes make sense only if the patient owns a smartphone. The statistics are shown in Table 4, where 61% of respondents answered that they own one. There are mainly patients with T1DM as their average age is lower. Nevertheless, with the aging population and the development of technologies, it is expected that the number of smartphone owners will be rising, which means that the target audience will be growing, too.
  | Table 4 Absolute and relative frequency of smartphone owners according to the type of diabetes |
Unfortunately, only 25% of respondents knew any application for diabetics. The others did not know any. Doctors do not actively suggest patients to use apps for management. As few as 9% respondents were informed about this option by their diabetologist. In this research, it was possible to choose from eleven – both domestic and foreign – apps. Domestic ones were: iFora Diabetes Management, SiDiary, Diabetes M, Mobiab, and Denik pacienta. The following ones were foreign: OnTrack Diabetes, Glucose Buddy, MySugr, Fooducate, Diabetes App, and Dbees. The most familiar ones were SiDiary and Denik pacienta, both 27 times. Denik pacienta serves as a way of keeping a record of used drugs, allergies, inoculations, and blood glucose levels without any further processing of this information.
Approximately 36% of respondents stated that app usage in treatment did not come to their minds at all, and 30% of respondents complained that their “doctor did not offer it to them”. Other answers were chosen by <20% of respondents, they included: paper documentation preference, they considered their use as a waste of time, or too difficult. Diabetics’ requirements for apps are mostly connected with the functionality of applications. More than 45% of them would start using a mobile app if it helped improve their blood glucose levels. For 33.5% of respondents, the apps would have to be user-friendly, ie, easy to use. Another finding is lower frequency of the answer “direct communication with the doctor via the app” (only 28.1%). Diabetics would appreciate the apps most if they informed them about their treatment of diabetes. Patients are aware of the significance of new scientific findings for their treatment and are interested in them. To increase the usage of apps, it is necessary to improve the import and export of data from glucose meters and other devices. Only a few glucose meters enable sending data by means of a wireless technology (eg, Bluetooth), but 38% of participants would welcome it. Such an improvement could lead to spreading mobile apps. All processes would be simpler, and the number of user’s operations would be lower. An interesting finding is using mobile apps in other areas of health control (pace calculators, diet nutrition controllers, sleep control apps), which shows that the apps are useful.Other health control apps are used by as many as 30% of respondents, whereas diabetes apps are used by only 4%.
Assessment of other findings
RQ1: Do patients know modern technologies for the control of diabetes?
The awareness of technical possibilities is defined by having information about continuous glucose monitoring devices, electronic insulin pens, insulin pumps, glucose meters, and mobile diabetes apps. These findings are presented in Figure 1. It was proved that patients have basic information about treatment possibilities, although their awareness decreases when it comes to the latest treatment possibilities. It is evidenced by their low awareness of mobile apps or continuous glucose monitoring devices. To sum up, patients have low awareness of modern technical possibilities of the treatment of diabetes.
  | Figure 1 Relative frequency of using modern devices. |
RQ2: Do patients with T2DM control and know more about their health condition than patients with T1DM?
One of the key factors for the success of treatment is the adherence to diabetes treatment, which is often quite low. According to various studies, it is between 39% and 96%.25 More recent findings have revealed that, from a large part of it, it is a deliberate action when a patient intentionally decides to use the medicine differently than it is prescribed.23 T2DM is often associated with a poor lifestyle; therefore, a lower exposure of patients can be assumed. The emergence of T1DM has an autoimmune cause, which tells you nothing about their possible access to treatment. It is therefore possible that patient adherence varies across the groups. To verify possible differences, H0 hypothesis was set:
H0: Knowledge of last measured HbA1c value is statistically more significant for T2DM compared with T1DM.
Regardless of the type of DM, the HbA1c value is one of the indicators of whether the patient is well compensated. The patient should be aware of what the value of the given indicator is.
H0: Data recording of the measured glucose values are statistically significant for T2DM compared with T1DM.
For proper adjustment of treatment, it is based on blood glucose readings during a day. It is therefore important that a physician has the data available and can respond according to a particular pattern (trend of glycemia). The test of hypotheses only included patients who have their own glucose meter.
H0: They seek information from sources other than from a physician is statistically significant for T2DM compared with T1DM.
Trying to learn more about their disease and not totally rely on information from the physician is another indicator of how patients approach their illness.
H0: The frequency of blood sugar testing is statistically more significant for T2DM compared with T1DM.
To set the treatment correctly, it is necessary to obtain blood glucose readings throughout the day to avoid high hyperglycemia or vice versa – hypoglycemia. If a patient knows their actual value of blood glucose, they can react effectively. Patients treated with insulin are entitled to a higher amount of strips covered by insurance, and therefore the test included only patients who meet this condition. The categories (blood glucose measurements four times or more a day, two to three times a day, one time a day) were compared.
H0: Self-care activities are statistically more significant for T2DM compared with T1DM.
For DM, it is also important to control the food that a patient consumes, especially carbohydrates, which significantly affects the value of blood glucose. Similarly, physical activity significantly affects the value of blood glucose (Table 5).
  | Table 5 Overview of testing hypothesis (comparing T2DM and T1DM) |
Nearly in all hypotheses tested, the hypothesis was not confirmed at a significance level of α=5%. Access of patients in each set indicators within groups of diabetes differ, and the T1DM group seems to be more responsible. This claim cannot be confirmed only when monitoring (T2DM > T1DM).
RQ3: Do patients with associated complications control and know about their health condition more than the other patients with diabetes?
The same procedure is to evaluate the RQ3. The groups that are compared in individual factors are patients who have already some complications associated with diabetes and patients who have so far had no complications. In all investigated factors, it is believed that patients with complications will exhibit a much higher exposure to the disease than patients without complications, as they are already aware of the risks (Table 6).
  | Table 6 Overview of testing hypothesis (comparing patients with/without complication) |
Although the patients have already experienced health complications associated with diabetes, it does not mean that they are more responsible and more committed to self-care activities compared with patients without complications. In any of the monitored indicators, no statistically significant difference was demonstrated at a significance level of 5% between patients with and without complications. Patients with complications do not show any more responsibility than other diabetics. The hypothesis was disproved.
RQ4: Is there any dependence between the level of HbA1c and record of blood glucose level, the frequency of measuring blood glucose level, the type of treatment (pump/pen), or controlling other aspects of health?
HbA1c is one of the indicators for assessing DM compensations. It is believed that certain factors greatly affect its value. Evaluation of HbA1c dependency was conducted based on the chi-square test of independence in the pivot table and the following H0 were developed (not counting the patients who did not know their HbA1c value).
H0: There is no effect of blood glucose data logging on HbA1c.
The testing only included patients who are treated with insulin or in combination with insulin, since the coverage of the strips from an insurance company in these groups is comparable and therefore does not affect the test result.
H0: There is effect on the frequency of blood glucose measurements on HbA1c.
H0: There is no influence of the type of treatment (pen/pump) on HbA1c.
The account was taken of patients treated with insulin or in combination with insulin.
H0: There is no influence of the monitored factors on HbA1c.
Within the test, the number of monitored aspects of health (physical activity, carbohydrates, blood sugar, etc.) was compared to know whether they affect the value of HbA1c (Table 7).
  | Table 7 Overview of testing hypothesis |
Effect of the tested factors on HbA1c at a significance level of 5% was not proved in most cases. When you merge the groups in the hypothesis of a frequency measurement and its impact on HbA1c, the claim is confirmed; however, it is a weak dependence (as indicated by the correlation coefficient).
RQ5: Is there any dependence between the assessment of technical skills and the type of record of blood glucose level?
As in the earlier case of RQ4, chi-square test of independence in the pivot table was used for testing. H0 was set:
H0: There is no correlation between the type of data entry and technical skills assessed.
After testing, patients were selected depending on who owns a personal glucose meter. Categories for recording data are no record, paper diary, and use cell phone/PC. At a significance level of 5%, a weak dependence of the glucose value and assessed technical skills was proved. H0 is therefore refused.
RQ6: Is there any dependence between the age of patient and the type of record of blood glucose level?
H0 was determined as follows:
H0: there is no correlation between the type of data entry and the age of the respondent.
At a significance level of 5%, a weak correlation between the age of the respondent and how the measured blood glucose values are recorded was proved.
Discussion
The aim of this article was to analyze patients’ attitudes to the use of modern technologies in the treatment of diabetes (T1DM and T2DM). The respondents were 313 patients with diabetes who proved to have basic knowledge of treatment possibilities of diabetes but little knowledge of using modern technologies for the treatment of diabetes. Although in other areas, it is ~30% of respondents who use mobile apps to monitor their health; in the treatment of diabetes only 4% of respondents use apps and 8% of respondents have used an app but were not satisfied with it. The rest of them have never used any app. The low percentage is caused by little knowledge of the existence and possibilities of diabetes apps. In using apps, respondents emphasize that the most sought-after functions are providing information, blood glucose level assessment, insulin dose reminders, and blood glucose level measurement. Compatibility is also important.
The low use of modern technologies is confirmed by other studies in the field of diabetes as well as in that of other chronic diseases. For instance, a study25 looked into data download from diabetes devices and double check of values by patients with T1DM. The study showed that ~70% of respondents had never downloaded data from their monitoring devices. Among the reasons for this include insufficient patients’ education in this area and difficult manipulation with measured data. The Diabetes Mine 2013 survey had better results with 40% of patients using data download from monitoring devices, which is a better result than in this study. Participants also assessed apps. They pointed at the main problems, including bad interface and hardware–software compatibility.26 Concerning the use of technologies in treating other chronic diseases, the study27 showed that 8% of the asthma and COPD patients knew of the term eHealth. Knowledge of specific eHealth applications (eg, electronic medical record, electronic consultations, and monitoring from a distance) was higher and ranged from 21% to 88%. Most available applications were used by <20% of the patients, although figures differ by age and educational level.
The actual results of the examination of other dependencies showed that there is a dependence between technical skills and methods of entering data; gender and age show a weak dependence on the way of data entry about their own health. Furthermore, patients with T1DM control and know more about their health condition than patients with T2DM, which is reflected, for example, in frequent blood glucose measurements or larger track of their physical activity. Conversely, the relationship between the associated complications and self-care activities has not been demonstrated.
Conclusion
Despite the current fast development of modern technologies, these technologies are not frequently used in treating patients.28–30 The principal problem does not lie in the lack of apps and technologies but rather in patients’ low technological knowledge and their higher age, which makes learning new skills, including the use of modern technologies, more difficult.
This study did not capture several significant aspects related to the topic in question, including doctors’ knowledge of modern technologies and their possibilities. As doctors play a vital role in treating diseases, they are extremely important for spreading technologies among patients. The authors expect that solutions to problems in question will be found and other aspects, including implementation costs of modern technologies or technical linking of individual devices for monitoring individual parameters of diabetes treatment, will also be treated.
Acknowledgment
This research was supported by the project of excellence (University of Hradec Kralove, Faculty of Informatics and Management) and Economical and Managerial aspects in Biomedicine.
Disclosure
The authors report no conflicts of interest in this work.
References
International Diabetes Federation. IDF Diabetes Atlas Sixth edition [online]. Belgie; 2013. Available from: http://www.diabetesatlas.org/. Accessed March 2016. | ||
Maresova P, Mohleska H, Kuca K. Social and family load of Alzheimer’s disease. Appl Econ. 2015;48:1936–1948. | ||
Mohelska H, Maresova P, Valis M, Kuca K. Alzheimer’s disease and its treatment costs: case study in the Czech Republic. Neuropsychiatr Dis Treat. 2015;11:2349–2354. | ||
European Commission [webpage on the Internet]. The Green Paper on Mobile Health (“Health”). European Commission. Brussels; 2014. Available from: https://ec.europa.eu/digital-single-market/en/news/green-paper-mobile-health-mhealth. Accessed March 2016. | ||
Ventola CL. Mobile devices and apps for health care professionals: uses and benefits. P T. 2014;39(5):356–364. | ||
International Diabetes Federation. Global Diabetes Scorecard Tracking Progress for Action. Belgium; 2014. Available from: www.idf.org/global-diabetes-scorecard/assets/downloads/Scorecard-29-07-14.pdf. Accessed March 2016. | ||
Stratton IM, Adler AI, Neil HA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321(7258):405–412. | ||
Rodbard HW, Blonde L, Braithwaite SS, et al. Medical guidelines for clinical practice for the management of diabetes mellitus. Endocr Pract. 2007;13(suppl 1):1–68. | ||
Gaede P, Lund-Andersen H, Parving HH, Pedersen O. Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med. 2008;358(6):580–591. | ||
Parkin CG, Davison JA. Value of self-monitoring blood glucose pattern analysis in improving diabetes outcomes. J Diabetes Sci Technol. 2009;3(3):500–508. | ||
Berndt RD, Takenga C, Preik P, et al. Impact of information technology on the therapy of type-1 diabetes: a case study of children and adolescents in Germany. J Pers Med. 2014;4(2):200–217. | ||
Raiff BR, Dallery J. Internet-based contingency management to improve adherence with blood glucose testing recommendations for teens with type-1 diabetes. J Appl Behav Anal. 2010;43:487–491. | ||
Årsand E, Tatara N, Østengen G, Hartvigsen G. Wireless and Mobile Technologies Improving Diabetes Self-Management: Handbook of Research on Mobility and Computing: Evolving Technologies and Ubiquitous Impacts. Hershey, PA: IGI Global; 2011. | ||
El-Gayar O, Timsina P, Nawar N, Eid W. A systematic review of IT for diabetes self-management: are we there yet? Int J Med Inform. 2013;82(8):637–652. | ||
UK Prospective Diabetes Study Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352:837–853. | ||
UK Prospective Diabetes Study Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet. 1998;352:854–865. | ||
DCCT/EDIC Research Group. Retinopathy and nephropathy in patients with type 1 diabetes four years after a trial of intensive therapy. N Engl J Med. 2000;342:381–389. | ||
Lawson ML, Gerstein HC, Tsui E, Zinman B. Effect of intensive therapy on early macrovascular disease in young individuals with type 1 diabetes. Diabetes Care. 1999;22(suppl 1):B35–B39. | ||
Van Damme P, Martens L, Van Damme J, et al. Caspase-specific and nonspecific in vivo protein processing during Fas-induced apoptosis. Nat Methods. 2005;2(10):771–777. | ||
Donald H, Franklin V, Greene AH. The use of mobile phones in dietary assessment in young people with Type 1 diabetes. J Human Nutr Diet. 2009;22(3):256–257. | ||
Chomutare T, Fernandez-Luque L, Arsand E, Hartvigsen G. Features of mobile diabetes applications: review of the literature and analysis of current applications compared against evidence-based guidelines. J Med Internet Res. 2013;13(3):e65. | ||
Anglada-Martínez H, Rovira-Illamola M, Martin-Conde M, Sotoca-Momblona JM, Codina-Jané C. mHealth intervention to improve medication management in chronically ill patients: analysis of the recruitment process. Postgrad Med. 2016;128(4):427–431. | ||
Haluzík M, Vrablík M, Herber O. Risk Patient from the Perspective Internist, Diabetologist and General Practitioner. Practicus. 2015:29–34. Available from: http://web.practicus.eu/sites/cz/Documents/Practicus-2015-06/29-Rizikovy-pacient.pdf. Accessed August 19, 2015. | ||
Draessler J. Applied Statistic. Hradec Kralove: Gaudeamus; 2013. | ||
Tenderich A [webpage on the Internet]. Our Survey: Diabetes Patients Rank Tech Tools, Quality of Life [online]. Available from: http://www.healthline.com/diabetesmine/diabetes-patients-rank-biggest-drawbacks-of-technology-tools. Accessed August 19, 2015. | ||
Hofstede J, de Bie J, van Wijngaarden B, Heijmans M. Knowledge, use and attitude towards eHealth among patients with chronic lung diseases. Int J Med Inform. 2014;83(12):967–974. | ||
Free C, Phillips G, Galli L, et al. The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: a systematic review. PLoS Med. 2013;10(1):e1001362. | ||
Diabetes Control and Complications Trial (DCCT) Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977–986. | ||
Spanakis EG, Chiarugi F, Kouroubali A, et al. Diabetes management using modern information and communication technologies and new care models. Interact J Med Res. 2012;1(2):e8. | ||
Or C, Tao D. A 3-month randomized controlled pilot trial of a patient-centered, computer-based self-monitoring system for the care of type 2 diabetes mellitus and hypertension. J Med Syst. 2016;40(4):81. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.