Back to Journals » International Journal of Women's Health » Volume 11
Patients with cervical intraepithelial neoplasms show different states of health-related quality of life and different coping styles depending on the choice of therapy: findings from the CIN study
Authors Klügel S, Lücke C , Mehren A , Malik E, Philipsen A, Schild-Suhren M , Müller HHO
Received 11 March 2019
Accepted for publication 23 July 2019
Published 12 September 2019 Volume 2019:11 Pages 511—517
DOI https://doi.org/10.2147/IJWH.S208257
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Everett Magann
Stephanie Klügel,1 Caroline Lücke,2 Aylin Mehren,1,3 Eduard Malik,4 Alexandra Philipsen,2 Meike Schild-Suhren,4,* Helge HO Müller1,2,*
1Department of Psychiatry and Psychotherapy, Carl von Ossietzky University Oldenburg, Oldenburg, Germany; 2Department of Psychiatry and Psychotherapy, University of Bonn, Bonn, Germany; 3Biological Psychology Lab, Department of Psychology, Carl von Ossietzky University Oldenburg, Oldenburg, Germany; 4Department of Gynecology and Obstetrics, Carl Von Ossietzky University Oldenburg, Oldenburg, Germany
*These authors contributed equally to this work
Correspondence: Stephanie Klügel; Helge HO Müller
Department of Psychiatry and Psychotherapy, Carl von Ossietzky University Oldenburg, Oldenburg, Germany
Tel +49 171 799 0959
Email [email protected]; [email protected]
Purpose: To examine the effects of type of therapy (conservative therapy vs conization) on the psychosocial well-being of patients with cervical intraepithelial neoplasia grade II (CIN II) in a prospective cross-sectional study designed to simplify future choice of therapy.
Patients and methods: In a cross-sectional study comparing 24 CIN II patients who were treated via conservative therapy with 17 CIN II patients who were treated via conization (not randomized), we examined the association between therapy type and psychosocial well-being after the treatment. Scores on the Hospital Anxiety and Depression Scale (HADS) (prevalence of depression/anxiety), SF-12 (health-related quality of life (HRQoL)) and Brief COPE (coping mechanisms) questionnaires were compared between the two subgroups via nonparametric Mann-Whitney U-tests.
Results: The prevalence of depression/anxiety and mental HRQoL did not differ between patients undergoing conservative therapy and those undergoing conization but differed significantly from those of the healthy population. Regarding physical HRQoL and coping strategies, the conservative therapy subgroup achieved higher scores and better performance.
Conclusion: Patients with CIN II are at risk of developing depressive or anxiety symptoms. The choice of therapy seems to have an influence on physical HRQoL and coping strategies but not on depression/anxiety and mental HRQoL.
Keywords: cervical cancer, coping styles, health-related quality of life
Introduction
Cervical cancer and cervical intraepithelial neoplasia (CIN)
Cervical cancer is the fourth-most common cause of cancer and the fourth-most common cause of death from cancer in women.1 The premalignant transformation of cells of the cervix that can potentially lead to cervical cancer is classified as cervical intraepithelial neoplasia (CIN).2 The origin of CIN can be attributed to infections by human papilloma virus (HPV) in 80% of high risk-types (16 and 18).2 Risk factors include multiple sexual partners and cigarette smoking.3 A large number of women with an HPV infection will not develop CIN because the HPV infection tends to disappear on its own within three years.4 When this is not the case, infected women run a higher risk of developing CIN and cervical cancer. CIN is graded on an I-III scale, with III being the most abnormal; the Bethesda Classification classifies CIN I as “low-grade squamous intraepithelial lesion” (LSIL) and CIN II-III as “high-grade squamous intraepithelial lesions” (HSIL).2 When treating women with CIN, the goal is to prevent the occurrence of or progression to invasive cancer while avoiding overtreatment of lesions that are likely to regress. Because of that and in accordance with directives and studies, there is no medical or surgical treatment for CIN I, but the recommendation is to closely follow and reevaluate the results after 6–12 months (conservative therapy).5 The treatment of higher-grade CIN in general involves cervical surgery via laser conization or loop conization (LEEP/LEETZ), but it is also possible to manage CIN II with follow-up, particularly in younger or pregnant women.6,7 The choice of follow-up vs surgery depends on different factors, such as the age of the patient, pregnancy (conization is not indicated during pregnancy), duration, and lesion grading.5 It is not always easy to choose the right treatment method, especially because surgical treatment for CIN lesions is associated with an increased risk of subfertility and premature birth.8,9 In principle, the choice of therapy must be made not only by the doctors but also by the patient. However, this concept of shared decision-making has some disadvantages.10 For many patients, it is an additional burden because they must consider the potential risks and benefits of all treatment options without the benefit of a medical background.11,12 In a previous study, we showed that cervical cancer patients have a high prevalence of developing psychiatric comorbidities such as depression.13 With that in mind, we assumed that the psychosocial well-being of CIN II precancer patients is also reduced compared to the healthy population and hypothesized a difference between patients who were treated via follow-up and those who were treated via loop conization. This particularity of CIN II therapy offers a very interesting starting point for a cross-sectional study because one patient cohort automatically includes two subgroups that can be compared. Until now, to the best of our knowledge, there have not been any guideline recommendations for the choice of therapy from the psychological point of view. To simplify future choice of therapy, we examined the association between treatment method and psychosocial well-being of CIN II patients.
Methods
Participants
This cross-sectional study included 57 CIN II patients treated during dysplasia consultation at the Department of Gynecology (Klinikum Oldenburg). The study was conducted in accordance with the Declaration of Helsinki and approved by the ethics committee of the Carl von Ossietzky University of Oldenburg. After the patients were invited to participate, they signed a consent form that included information regarding the study design and aims. Data acquisition was then performed in a prospective manner by a single rater. The period of data acquisition was 12 months (September 2016 - August 2017).
Procedures
Because of missing data or prior history of depressive/anxiety symptoms, 16 patients were excluded from the analysis, so that data from 41 patients were analyzed. Patients were all women, age between 18 and 54 years, german, and had no prior history of depressive/anxiety symptoms. The conservative therapy group included 24 patients, and the loop conization group comprised 17 patients. The distribution of the patients into the two groups was not randomized because there was already a medical distribution done by the treating gynecologist. CIN was diagnosed by PAP smear and biopsy. The patients were asked to complete three questionnaires that assessed depression/anxiety (Hospital Anxiety and Depression Scale; HADS), health-related quality of life (HRQoL; SF-12), and coping (Brief COPE). In the initial step of the data analysis, the prevalence rates and the extent of depressive and/or anxiety symptoms were evaluated in a descriptive manner. We subsequently analyzed whether the psychological test scores differed between the conservative therapy group, the conization group and the healthy population.14–16
Questionnaires
To assess the prevalence rates of depressive and/or anxiety symptoms, we used the HADS.17 The HADS is a well-validated screening instrument for psychological burden in patients with somatic diseases and is widely used in hospital settings. It consists of two subscales (anxiety and depression) comprising 7 items each. Items are scored on a four-point Likert scale between 0 and 3. Subscale scores of 7 and below are considered as normal, whereas scores between 8 and 10 are considered borderline, and scores of 11 and above indicate clinical manifestations of depressive or anxiety symptoms.17,18
HRQoL can be understood as a complex concept encompassing social, psychological, and physical aspects of well-being and functioning.19,20 To measure HRQoL, we used the standardized and validated SF-12 questionnaire, which is a shortened version of the SF-36 questionnaire. Both are frequently used in clinical settings. The SF-12 records the subjective HRQoL (for example, in terms of physical, mental, and social functioning) and consists of 6 items on a physical and 6 items on a mental scale.21 To evaluate the HRQoL, we used the SF-12 evaluation tool, which includes the reversed questions 1, 6, 9 and 10 (so that higher points always correspond to a higher HRQoL) and is weighted using the standardized American regression coefficient and a standardized transformation of the values for better comparison. In the final step of the calculation, the 12 items are aggregated into two health summary scales that reflect physical (PCS) and mental (MCS) components ranging from 0 (worst) to 100 (best).
Coping mechanisms/styles are strategies we use to overcome difficult events or stages in life.22–24 Coping strategies may be effective, ineffective, or ambivalent. The Brief COPE is a common questionnaire used to identify coping strategies of patients. It consists of 28 items scored on a four-point Likert scale, where 1 means “not at all”, 2 means “some”, 3 means “quite”, and 4 means “a lot”. Strategies such as active coping (items 2 and 7), use of emotional (items 5 and 15) and instrumental (items 10 and 23) support, venting (items 9 and 21), positive reframing (items 12 and 17), planning (items 14 and 25), and humor (items 18 and 28) are considered effective, while denial (items 3 and 8), substance use (items 4 and 11), behavioral disengagement (items 6 and 16), and self-blame (items 13 and 26) are considered ineffective, and self-distraction (items 1 and 19), acceptance (items 20 and 24), and religion (items 22 and 27) are considered ambivalent.22 To evaluate the Brief COPE, we reverse-scored the ineffective strategies (so that higher points always corresponded to better coping strategies), and at the end, we counted effective and ineffective strategies (11 in total) to obtain a final score for each item ranging from 2 (worst) to 8 (best). We did not count the ambivalent strategies.
Statistical data analysis
The data were analyzed using SPSS version 25 (IBM Corp., Armonk, NY). In the initial step of the analysis, we investigated the prevalence and extent of depression and/or anxiety (HADS) and measured HRQoL (SF-12) and coping strategies (COPE). In a subsequent step, we compared the scores obtained from the subgroups and then compared them with a normal population via a nonparametric Mann-Whitney U-test with exact p-values (see Tables 1 and 2). We were not able to compare our measurements with the original values of the normal population because only arithmetic means (μ) and standard deviations (σ) were available. Using Python version 3.6 (Python Software Foundation), we generated 10,000 (μ,σ)-normally distributed observations to simulate the original values. We had intended to simulate the values for the analysis of the Brief COPE too, but we could not find any data for the normal population.
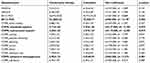 |
Table 1 Comparisons of HADS, SF-12 and COPE scores between CIN II patients who underwent conservative therapy and conization |
 |
Table 2 Comparisons of HADS and SF-12 between CIN II patients and the normal population |
Results
Anxiety and depression
In the conservative therapy subgroup, 12.5% of the patients had an increased HADS-D score, and 33.3% of the patients had an increased HADS-A score (subscale scores of ≥8), whereas in the loop conization subgroup, elevated scores were found in 29.4% (HADS-D) and 52.9% (HADS-A) of the patients.
The average HADS-D scores were 3.21±3.31 (conservative therapy) and 6.35±6.42 (conization). Higher scores were observed for anxiety (HADS-A): 6.58±3.89 for the conservative therapy subgroup compared to 9.35±5.80 for the loop conization subgroup.
The prevalence rates for depressive and anxiety symptoms were not significantly different between the subgroups of patients (HADS-D: U=147.500, z= −1.509, p=0.131; HADS-A: U=151.000, z= −1.409, p=0.159), but scores of both subgroups differed significantly from those of the healthy population normative sample (HADS-D: U=155093.000, z= −2.694, p=0.007; HADS-A: U =143573.000, z= −3.316, p=0.001), which showed average scores of 4.7±3.9 (HADS-D) and 5.0±3.4 (HADS-A).14
Health-related quality of life
In the conservative therapy subgroup, the SF-12 physical summary score (PCS, 53.26±5.52) indicated that physical HRQoL is not affected by the disease/therapy (in comparison, the mean values for a normal German population sample of 11,012 women was 49.49±10.22).15 Regarding mental health, the scores (MCS, 46.47±10.02) were slightly lower (normal sample: 48.94±10.21).
In the loop conization subgroup, the SF-12 physical (PCS, 45.0±9.77) and mental (MCS, 42.77±14.20) summary scores indicated considerable HRQoL impairment compared with the mean values for the normal German population sample.
Comparing the two subgroups with the normal sample, there was no significant difference in physical or mental HRQoL (PCS: U=184703.000, z= −1.096, p=0.273; MCS: U=178929.000, z= −1.407, p=0.159).15
Evaluating the differences between the two subgroups, the conservative therapy subgroup differed significantly from the loop conization subgroup on the PCS-12 (U=85.000, z= −3,149, p=0,002), which suggests that the patients treated via conservative therapy felt more comfortable in terms of physical HRQoL. There were no significant differences between the two subgroups with respect to mental HRQoL (U=181.000, z= −0.609, p=0.543).
Coping
Regarding the mean scores for coping strategies (see Figure 1), the conservative subgroup had higher mean scores for effective coping strategies than the loop conization subgroup did. This means that the conservative subgroup used effective coping strategies either more often or in a more intense way. The strategies with the highest scores were emotional support (conservative therapy subgroup) and planning (loop conization subgroup).
 |
Figure 1 Mean scores for effective coping strategies. |
In terms of ineffective coping strategies, the most commonly used strategies were self-blame (conservative therapy group) and behavioral disengagement (loop conization group). Once more, the conservative therapy subgroup exhibited higher mean scores. The scores for the strategies emotional support (U=127.000, z= −2.104, p=0.035), instrumental support (U=119.500, z= −2.355, p=0.019) and behavioral disengagement (U=84.500, z= −3.272, p=0.001) were significantly different between the two subgroups.
Discussion
The major aim of this study was to examine the effects of therapy type on the psychosocial well-being and coping structures of CIN II patients who underwent different types of treatments (conservative therapy vs loop conization) using a prospective cross-sectional study design and to further assess both groups regarding depression, anxiety, HRQoL and coping strategies to simplify future decisions regarding which therapy to choose.
The prevalence rates for depressive and anxiety symptoms were significantly higher than those of the healthy population14 and similar to the rates for other cancer groups.16 This shows that CIN II patients have a higher risk of developing depressive and anxiety symptoms, although they suffer from a premalignant lesions and have not yet developed cancer. When treating CIN II patients, these factors should be taken into consideration. It is possible to offer psycho-oncology and supportive care as is generally provided for cancer patients and to assist in establishing self-help groups for premalignant lesions. The patient’s disease should be taken seriously to prevent further depressive or anxiety disorders.
Within the two subgroups, the rates of depressive and anxiety symptoms were not significantly different. The present results suggest that the type of therapy does not influence the occurrence of depressive and anxiety symptoms in CIN II patients but that the patients’ psychiatric comorbidities should be taken care of. Regarding physical and mental HRQoL, the summary scores of the CIN II patients were lower than those of the normal German population, but taken together, the difference was not significant. One possible reason could be that the conservative therapy subgroup achieved higher summary scores. Between the two subgroups, the conservative therapy subgroup differed from the conization subgroup in terms of physical HRQoL (they felt more comfortable) but not in view of mental HRQoL. An explanation for this finding could be that patients who undergo surgery feel less comfortable in general, at least in terms of physical HRQoL.25
In terms of coping strategies, the results showed higher mean scores for both effective and ineffective coping strategies in the conservative therapy subgroup. This finding indicates that the conservative subgroup used effective coping strategies more often or in a more intense way and resisted ineffective coping strategies to the same degree as the surgical subgroup. There were significant differences on three of the items (emotional support, instrumental support, behavioral disengagement). The question for further research is: Is the fact that these patients underwent conservative therapy a main psychological influence factor in coping with the disease?
To summarize, the prevalence of depression/anxiety and reduced mental HRQoL remains surprisingly constant in patients who have undergone both conservative therapy and conization. In terms of physical HRQoL and coping strategies, the conservative therapy subgroup exhibited higher scores and better performance. Therefore, the type of therapy has a partial influence on the psychosocial well-being of CIN II patients. From the psychological/psychiatric point of view, this finding raises several questions. Should we advise patients to undergo conservative therapy? Other studies show similar results.26,27 Should we extend the treatment of CIN II in consideration of psychiatric comorbidities?
A possible limitation of our examination is that sociodemographic characteristics such as profession and family background may also have an impact on psychosocial well-being. In addition, it could be necessary to have a longer follow-up and reevaluate the questionnaires at a later time and/or include a larger number of participants.
Conclusion
Taken together, the findings of the present study indicate that patients with CIN II are at risk of developing depression or anxiety symptoms. The type of therapy seems to have an influence on physical HRQoL and coping strategies, namely in terms of physical HRQoL and coping strategies, the conservative therapy subgroup exhibited higher scores and better performance. Regarding depression/anxiety and mental HRQoL, the choice of therapy itself surprisingly does not seem to have an important impact. To better identify the reasons for the different performances of the two subgroups and other potentially causative factors, further longitudinal studies are necessary.
Abbreviations
CIN, cervical intraepithelial neoplasia; HRQoL, health related quality of life.
Ethical approval and informed consent
This study was conducted in accordance with the Declaration of Helsinki and was approved by the local ethics committee of the Carl von Ossietzky University Oldenburg, number 087/2016. All patients gave their written informed consent before participating in this study.
Consent for publication
All authors gave their consent for publication of this manuscript.
Data availability
The data of this study is available upon request to the first author (SK).
Acknowledgment
Publication of this study is supported by the DFG open access fund for publishing of the Carl von Ossietzky University Oldenburg.
Author contributions
All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors have no conflicts of interest to declare.
References
1. Stewart BW, Wild CP. World Cancer Report 2014. Lyon, France: International Agency for Research on Cancer; 2014.
2. Gätje R, Eberle C, Scholz C, Lübke M. Kurzlehrbuch Gynäkologie und Geburtshilfe. Stuttgart: Georg Thieme Verlag; 2011.
3. Winer RL, Lee SK, Hughes JP, Adam DE, Kiviat NB, Koutsky LA. Genital human papillomavirus infection: incidence and risk factors in a cohort of female university students. Am J Epidemiol. 2003;157(3):218–226. doi:10.1093/aje/kwf180
4. Schiffman M, Castle PE, Jeronimo J, Rodriguez AC, Wacholder S. Human papillomavirus and cervical cancer. Lancet. 2007;370(9590):890–907. doi:10.1016/S0140-6736(07)61416-0
5. Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften. S3-leitlinie diagnostik, therapie und nachsorge der patientin mit zervixkarzinom. 2014; https://www.awmf.org/uploads/tx_szleitlinien/032-033OLk_S3_Zervixkarzinom_2014-10.pdf.
6. Lindeque BG. Management of cervical premalignant lesions. Best Pract Res Clin Obstet Gynaecol. 2005;19(4):545–561. doi:10.1016/j.bpobgyn.2005.02.008
7. Massad LS, Einstein MH, Huh WK, et al. 2012 updated consensus guidelines for the management of abnormal cervical cancer screening tests and cancer precursors. J Low Genit Tract Dis. 2013;17(5 Suppl 1):S1–S27. doi:10.1097/LGT.0b013e318287d329
8. Spracklen CN, Harland KK, Stegmann BJ, Saftlas AF. Cervical surgery for cervical intraepithelial neoplasia and prolonged time to conception of a live birth: a case-control study. BJOG. 2013;120(8):960–965. doi:10.1111/1471-0528.12209
9. Kyrgiou M, Athanasiou A, Paraskevaidi M, et al. Adverse obstetric outcomes after local treatment for cervical preinvasive and early invasive disease according to cone depth: systematic review and meta-analysis. BMJ (clinical Research Ed). 2016;354:i3633.
10. Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango). Soc Sci Med. 1997;44(5):681–692. doi:10.1016/S0277-9536(96)00221-3
11. Faller H. Shared decision making: an approach to strengthening patient participation in rehabilitation. Rehabilitation (Stuttg). 2003;42(3):129–135. doi:10.1055/s-2003-40097
12. Coulter A. Partnerships with patients: the pros and cons of shared clinical decision-making. J Health Serv Res Policy. 1997;2(2):112–121. doi:10.1177/135581969700200209
13. Klugel S, Lucke C, Meta A, et al. Concomitant psychiatric symptoms and impaired quality of life in women with cervical cancer: a critical review. Int J Womens Health Wellness. 2017;9:795–805. doi:10.2147/IJWH.S143368
14. Hinz A, Schwarz R. Angst und Depression in der Allgemeinbevölkerung. Psychother Psych Med. 2001;51(05):193–200. doi:10.1055/s-2001-13279
15. Schupp J, Wagner G, Nübling M, Andersen HH, Mühlbacher A. Computation of standard values for physical and mental health scale scores using the SOEP version of SF12v2. Schmollers Jahrbuch. 2007;127(1):171–182.
16. Krebber AM, Buffart LM, Kleijn G, et al. Prevalence of depression in cancer patients: a meta-analysis of diagnostic interviews and self-report instruments. Psycho-oncology. 2014;23(2):121–130. doi:10.1002/pon.3409
17. Snaith RP, Zigmond AS. The hospital anxiety and depression scale. Br Med J (Clin Res Ed). 1986;292(6516):344. doi:10.1136/bmj.292.6516.344
18. Petermann F. Hospital anxiety and depression scale, deutsche version (HADS-D). Zeitschrift für Psychiatrie, Psychologie und Psychotherapie. 2011;59(3):251–253. doi:10.1024/1661-4747/a000077
19. Bullinger M. Erfassung der gesundheitsbezogenen Lebensqualität mit dem SF-36-health survey. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2000;43(3):190–197. doi:10.1007/s001030050034
20. Ware JE
21. Gandek B, Ware JE, Aaronson NK, et al. Cross-validation of item selection and scoring for the SF-12 health survey in nine countries: results from the IQOLA project. International quality of life assessment. J Clin Epidemiol. 1998;51(11):1171–1178. doi:10.1016/s0895-4356(98)00109-7
22. Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol. 1989;56(2):267–283. doi:10.1037/0022-3514.56.2.267
23. Zeidner M, Endler NS. Handbook of Coping: Theory, Research, Applications. Vol. 195. John Wiley & Sons; 1996.
24. Folkman S, Lazarus RS, Gruen RJ, DeLongis A. Appraisal, coping, health status, and psychological symptoms. J Pers Soc Psychol. 1986;50(3):571–579. doi:10.1037/0022-3514.50.3.571
25. Fanfani F, Landoni F, Gagliardi ML, et al. Sexual and reproductive outcomes in early stage cervical cancer patients after excisional cone as a fertility-sparing surgery: an Italian experience. J Reprod Infertil. 2014;15(1):29–34.
26. Loopik DL, Bekkers RLM, Massuger L, Melchers WJG, Siebers AG, Bentley J. Justifying conservative management of CIN2 in women younger than 25years - a population-based study. Gynecol Oncol. 2019;152(1):82–86. doi:10.1016/j.ygyno.2018.10.038
27. Moscicki AB. Conservative management of adolescents with abnormal cytology and histology. J Natl Compr Canc Netw. 2008;6(1):101–106.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
