Back to Journals » International Journal of Nephrology and Renovascular Disease » Volume 12
Patient engagement activities with health care professionals in continuous ambulatory peritoneal dialysis therapy: an exploratory pilot study
Authors Darmayanti D, Simatupang TM , Rudito P
Received 29 August 2018
Accepted for publication 1 February 2019
Published 6 May 2019 Volume 2019:12 Pages 103—112
DOI https://doi.org/10.2147/IJNRD.S185691
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Pravin Singhal
Dahlia Darmayanti,1,2 Togar M Simatupang,2 Priyantono Rudito2
1Management Department, Bina Nusantara University, Jakarta, Indonesia; 2School of Business and Management, Institut Teknologi Bandung, Bandung, Indonesia
Background: This pilot study aimed to explore the engagement activities between patients on continuous ambulatory peritoneal dialysis (CAPD) therapy and their health care professionals.
Methods: An exploratory qualitative study was conducted. In-depth semi-structured interviews were undertaken involving four CAPD patients who were selected through purposive sampling. The participants were asked questions about their engagement experiences with their health care professionals.
Results: Six main engagement activities were derived from the interview analysis: obtaining initial knowledge, developing knowledge and skills, feeling confident, following clinical advice, updating health condition, and supporting CAPD therapy.
Conclusion: Patients engagement activities played an important role in CAPD therapy. The engagement activities covered the cognitive, emotional, and behavioral dimensions. Obtaining initial knowledge as well as developing knowledge and skills are essential engagement activities before patients perform CAPD therapy.
Keywords: patient engagement, health care professionals, CAPD, exploratory pilot study
Introduction
Chronic kidney disease (CKD) is a global public health problem which is also one of the leading causes of mortality, morbidity, and economic problems worldwide.1,2 A Global Burden of Disease study indicated that in 2010 CKD was ranked 18th among the most common causes of death, but in 2015 CKD was ranked 12th.2,3 Diabetes and hypertension are the two common causes of CKD worldwide.1,4 Kidney Outcomes Quality Initiative has categorized CKD into five stages based on glomerular filtration rate.5 At stage V or end-stage renal disease (ESRD), patients have options for choosing one of the renal replacement therapies (RRTs) in the form of kidney transplantation, hemodialysis (HD), and peritoneal dialysis (PD) either with automated peritoneal dialysis or continuous ambulatory peritoneal dialysis (CAPD).6,7
In Indonesia, data from nationwide household survey on basic health research showed that the prevalence of CKD increased from 0.2% in 2013 to 0.38% in 2018.8,9 The major cause of CKD was hypertension, followed by diabetes.10. The available modalities for RRTs were kidney transplants, HD, and CAPD.11,12 HD was introduced as the first modality RRT treatment in 1967, followed by renal transplantation in 1970 and CAPD in 1985.13
The major cost of a renal transplant and dialysis was covered by Jaminan Kesehatan National (JKN), the National Health Insurance Scheme of Indonesia that is managed by the Health Social Security Institution or Badan Penyelenggara Jaminan Sosial (BPJS).11,14 Patients on HD therapy received dialysis treatments twice in a week with 5 hours for each treatment. Meanwhile for CAPD patients, the government supported the cost of catheter insertion and dialysate for up to four times daily fluid exchange.11,12 BPJS had spent around IDR 3.9 trillion in 2016 for supporting dialysis and the number increased to IDR 4.6 trillion in 2017. This cost burden caused CKD to be ranked second in Indonesian government spending for catastrophic illness.14,15 Although renal transplantation was the best therapy for ESRD patients, limited number of kidney donors had made the patients to opt for either HD or CAPD.12,14 It was estimated that only 53% of ESRD patients in Indonesia were on dialysis, and HD was still the most preferred option of RRT compared to CAPD.14 The 10th Report of Indonesian Renal Registry reported that from 433 HD centers in Indonesia, there were 77,892 HD-active patients covering 98% of active ESRD patients, meanwhile only 2% of the active patients were on CAPD modality at the end of 2017.10
Since the introduction of CAPD therapy in Indonesia, the therapy was not one of the options offered to patients because of limited experiences and support of health care professionals. Moreover, the Indonesian economic crisis in 1997–1998 made CAPD an expensive modality and caused many patients to transfer to HD. There were only 461 patients on CAPD therapy treatment from 1990 to 2000.12,13 However, since 2005, owing to an increase in experienced CAPD health care professionals, the number of CAPD patients has grown and reached 1,594 and 1,737 in 2016 and 2017 respectively.10 The number of patients undergoing CAPD increased by only 8%, while those undergoing HD increased by 40%–50% per year.16 The implementation of CAPD has several challenges in Indonesia. Low utilization of CAPD may be attributed to limited information and education dissemination about the therapy to health care professionals and patients, only one major or limited provider of CAPD dialysate solution, limited availability of CAPD apparatus, and lack of transportation and distribution system to cover the Indonesian archipelago.10,11,16,17 Even though there is a small growth in the number of CAPD patients, CAPD modality should be considered, especially for patients who are still active. CAPD therapy provides better quality of life than HD, allows for flexibility on schedules in conducting self-dialysis, there is less restriction on diet as well as fluid intake, guarantees better preservation of residual renal function, and is less expensive than HD.2,6,14A study by Novelia et al indicated that in terms of cost, the average total cost of HD in Indonesia was around IDR 133.4 million or about US$10,000 per patient per year, meanwhile CAPD modality was around IDR 81.7 million or about US$6,000 per patient per year.11
In order to know which therapy is appropriate for ESRD patients and to obtain positive outcomes, they have to consult a doctor, preferably a nephrologist because the decision depends on patient’s choice, medical, social, and geographical considerations.18 Holman and Lorig also argued that “for the effective treatment of a chronic disease, the patient must engage continuously in different healthcare practices ... to achieve effectiveness and efficiency in treatment, the patient and health care professional must share complementary knowledge and authority in the healthcare process”.19 Patient engagement recognized that patients have an active role in managing their health. They have motivation to manage their health and obtain health literacy skills on the basis of which they can understand and act on health information provided to them and choose the appropriate treatment in concert with health care professional in a shared decision-making process.20,21 Patient engagement also can be viewed as “a process-like and multi-dimensional experience, resulting from the conjoint cognitive (think), emotional (feel), and conative (act) enactment of individuals toward their health management”.22
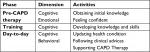
Previous research had indicated three primary periods, pre-CAPD therapy, training, and day-to-day dialysis, and three patient phases for CAPD therapy: 1) the adaptation phase was characterized by patients who were new and <1 year on CAPD therapy, 2) the stabilization phase was characterized by patients who were between 1 and 3 years on CAPD therapy, and 3) the last was the acceptance phase which consisted of patients who were >3 years on CAPD therapy (Figure 1).23
  | Figure 1 Phases of CAPD patient. Notes: Figure adapted from Darmayanti D, Simatupang TM, Rudito P. A pilot study on value cocreation activities in health care: A study on continuous ambulatory peritoneal dialysis. In: Proceedings of the 5th Naples Forum on Service; 2017; Sorrento, Naples, Italy;23 with permission from the 5th Naples Forum on Service (http://www.naplesforumonservice.it/public/index.php); Copyright © 2009–2019 SIMAS di Salerno for Naples Forum on Service - All rights reserved. Abbreviation: CAPD, continuous ambulatory peritoneal dialysis. |
If patient engagement is considered to be important for the effective and positive outcome, then it is critical to explore and investigate the patient engagement activities with health care professionals of CAPD therapy. Since there are a limited number of studies discussing engagement activities of the CAPD patients with their health care professionals, the aims of this pilot study were to explore and understand CAPD patients’ engagement activities with their health care professionals in each period of CAPD therapy.
Methods
This exploratory pilot study was conducted using a qualitative method. Qualitative method in health care helps to explore, describe, and develop an understanding of participants’ or patients’ experiences when they interact with health care professionals.24
Setting
The research context was CAPD patients in Indonesia who lived in the city of Jakarta and its suburbs.
Sampling
A purposive sampling technique was applied for selecting the participants undergoing CAPD therapy. Holloway and Galvin argued that “purposeful or purposive sampling is based on the judgment of the researcher”.24 One of the researchers who previously was a CAPD caregiver and joined the CAPD WhatsApp group had a list of a few CAPD patients. Regardless of whether the participants had ever used RRT before, the researcher looked for and contacted several CAPD patients who met the following inclusion criteria: male or female 18 years or above; were in adaptation, stabilization, or acceptance phase; and had a willingness to participate in this pilot study (Table 1).
  | Table 1 Inclusion criteria Abbreviations: ESRD, end-stage renal disease; CAPD, continuous ambulatory peritoneal dialysis; RRT, renal replacement therapy. |
Ethical issues
Ethical approval for this pilot study was obtained from the Ethics Committee of the School of Business Management of Institut Teknologi Bandung, Indonesia. Also, this study was conducted in accordance with the Declaration of Helsinki.
Before starting the interview, the participants were explained about the purpose of the study. They were informed that the discussion would be tape-recorded, the data would be kept confidentially, and the names of the participants would remain anonymous as well. After explaining the objectives, each participant was requested to sign a prepared written informed consent.
Data collection
A qualitative exploratory study was used to describe the patient engagement activities with their health care professionals. Interviewing, observing, collecting and examining, and feeling are several data collection types that can be used in a qualitative study.25 In this exploratory pilot study, the data were collected using an in-depth interview that included semi-structured and open-ended questions. The interviews were conducted one-on-one and face-to-face by the first author in person. With one-on-one interviews or individual interviews, the participants have the freedom to express and share ideas.26,27 The interviewer prepared a guide with the list of questions to be asked but was permitted to rephrase the questions.28,29 The interview question guideline was prepared and it was divided into three parts. The first part comprised introductory questions that asked about the general information of participant such as gender, age, marital status, and occupation. The second part asked about the medical history as well as the decision-making process and opinion on CAPD therapy, and the last part included questions related to participant’s experience with CAPD therapy that referred to engagement activities (Table 2). The interviews were conducted in Indonesian language at the locations preferred by each participant. With the permission of the participants, the interviews were tape-recorded and noted. The average time for each interview was about 45–60 minutes.
  | Table 2 Summary of interview questions Abbreviation: CAPD, continuous ambulatory peritoneal dialysis. |
Data analysis
The data were analyzed following the phenomenological method. The objective of the phenomenological research is to explore and describe the phenomena of people’s lived experiences.24 Each interview was tape-recorded, relistened, and transcribed. While reading and rereading the transcript, the recording was played several times to check if there was any missing or unclear information. While checking, the researcher conducted pre-coding by highlighting the significant quotes or statement from the participants. Then the complete transcribed data were coded using first- and second-cycle coding process developed by Saldana.30 Elemental methods including descriptive and in vivo coding techniques were applied in the first-cycle coding. To obtain the theme, pattern coding was used in the second-cycle coding. To keep the participant information confidential, the participants’ names were replaced with P1, P2, P3, and P4.
Trustworthiness
Credibility, dependability, confirmability, and transferability were used for trustworthiness in this pilot study.31 One of the researchers who joined CAPD WhatsApp group had interacted with the participants for some period of time. Thus, familiarity and trust had been established with the participants who represented each CAPD patient’s phase. The description on the context, the participant’s characteristics, data collection, and analysis of the findings are discussed in this study. During the interview, the notes were taken to enrich the data. Furthermore, the data from each interview were coded, reviewed, and re-read many times in detail in order to get the themes. To add to the authenticity, the themes from the data were obtained closely from participant’s own word. The lived experiences of the participants were disclosed.
Results
The researcher conducted four in-depth interviews with four participants who met the inclusion criteria. There were two males and two females. The age range of the participants was from 30 to 54 years. One participant was in the acceptance phase with >3 years on CAPD therapy, one was in the stabilization phase with 1 year on CAPD therapy, and the other two participants were in the adaptation phase with <1 year on CAPD therapy. The details of the participants are presented in Table 3.
  | Table 3 Characteristics of four participants included in exploratory pilot study Abbreviations: CAPD, continuous ambulatory peritoneal dialysis; HD, hemodialysis; P, patient. |
Theme
From analyzing the data, there were themes and subthemes that were generated from interviewing four participants (Table 4). Six themes of engagement activities between the patients and their health care professionals are as follows: obtaining initial knowledge, developing knowledge and skills, feeling confident, following clinical procedures, updating health condition, and advocating CAPD therapy. These were themes that emerged from the data with some exemplar quotations provided.
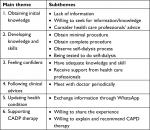  | Table 4 Main theme and subthemes Abbreviation: CAPD, continuous ambulatory peritoneal dialysis. |
Theme 1: obtaining initial knowledge
Being in ESRD stage that required an effective RRT or uncomfortable health condition after completing HD therapy led the participants to seek or consider alternatives other than HD therapy. All of the participants who were on HD therapy felt their health condition was weak and their appetite decreased after completing HD therapy. One of the participants who wanted to know another alternative for RRT besides HD therapy looked for information from the Internet because the hospital in the city where he lived only provided an HD therapy center. He also went to another city and met a nephrologist to consult about the possibility of switching from HD to CAPD therapy. Two other participants knew about CAPD from the nephrologist and PD nurse whom they always met and who helped them during HD therapy in a hospital center. They were advised to consider switching from HD to CAPD therapy. However, their initial information about CAPD therapy was limited to just revealing that it involves a clean and hygienic environment, less restrictions on diet, and low incidence of infections. One participant did not have a chance to examine various RRTs. He was advised directly by his nephrologist to use CAPD therapy because it was a suitable RRT for him, as he was still working and was active.
Being on HD therapy, I had lots of [health] problems such as I had low hemoglobin, I got skinnier, and I got darker skin. Therefore, I looked for another method and I found CAPD therapy. In fact, I did not know about it from the doctor or other CAPD patients. Rather, I often read from the Internet […] I tried to find out what developed countries do for kidney failure patients. I read that the nearest one was in country S. In fact, in country S, kidney failure patients are directly recommended to use CAPD […] I was curious and looked for references […] I went to see Doctor M. Once I consulted with him and I told him I intended to use CAPD therapy. He directly said OK […] CAPD was more suitable. [P1]
Every time [after finishing HD therapy], I got a fever. My blood pressure directly jumped to 190 or 200. I felt weak and could not do anything, could not eat, and I was tormented. [One day] after HD therapy, nurse T came and wanted to introduce CAPD. I went to her office and she gave me a video about CAPD. I watched the video. After watching the video, the nurse explained that CAPD could enhance the quality of my life. I could eat anything and I should consume fruit every day. [P4]
When I was on HD, I have been told about CAPD […] It should be sterilized. The room cannot be dirty and dusty […] you should consume lots of eggs, fish, and any kinds of food but not starfruit. Be careful of your drink [water intake], as it is in HD […] do not get infection. [P2]
[…] I don’t know about CAPD […] there is no choice, [I am] hospitalized and directly [had an operation]. [P3]
Theme 2: developing knowledge and skills
After a Tenckhoff catheter operation, the CAPD patients received a few days of training in the hospital conducted by a doctor or a designated CAPD nurse. All of the participants were trained in the steps of self-dialysis and self-care, from washing their hands, changing the dialysate, recording the outcome in the log book, and caring for the exit site. Two of the participants had <5 days training, one participant had to come for 5 consecutive days in a week, and the other participant stayed in the hospital for about 10 days and was tested to conduct a self-dialysis in front of a CAPD nurse.
[…] For hospital X, CAPD therapy was still new, so I had only been trained for one or two hours. Meanwhile, other hospitals conducted CAPD training for four days. [Hospital X] only trained in how to change the solution. So, there were no do’s and don’ts. Fortunately, I had a pharmaceutical background. In the clinical sphere, there are do’s and don’ts, about sterilization, I know. However, there were some steps that I did not know either; at the end I [got] an infection […] until now, I have not been taught the real [operating procedures] […] I never got the [procedures] of changing the solution. [P1]
[…] I only stayed for one day in the hospital. The nurse told me that [I] should be hospitalized for a week for learning, but I did not like to stay there; I wanted to go home […] [I] was told the next day about how to change [the solution], I had just known it […] it was easy […] only how to open and close it. [P3]
I was trained in the procedures from the very beginning, hand washing until the way to drain the fluid out and back in. And I learned how to maintain cleanliness in order to avoid an infection. I could not forget to put the face mask on, and I did not forget to wash my hands. [P4]
At first, I could not do anything after the operation; [it was] painful. The next day, right away for CAPD [I had] to see how the nurse [did it] […] in two or three days [I] myself […] was tested […] if [the nurse] was not so sure, the next day [I tried again]. I still forgot and it was dangerous. I forgot because I did everything by myself. [I] got a book. Every day […] in the blue log book […] I recorded it […] I was tested about CAPD. From the very beginning, taking the solution, washing my hands, everything was tested. The right or wrong way of washing my hands, putting the mask on, taking the solution for CAPD till the end, everything was observed. I could not do anything wrong. If I made a small mistake, it had to be repeated. [P2]
Theme 3: feeling confident
Gaining knowledge and skills about CAPD therapy and receiving attention from the CAPD nurse made the participants sure that CAPD therapy was the right choice. After seeing a CAPD video and being explained about CAPD therapy by the PD nurse, one of the participants was confident that CAPD was the right therapy for her. Another participant who experienced a home visit by a CAPD nurse in his early day-to-day period appreciated such a visit and felt that the visit was very meaningful and gave him more confidence toward CAPD therapy.
After watching a CAPD video, nurse E explained that CAPD could enhance the quality of my life […] with CAPD I had more freedom to eat, especially that fruits should be consumed every day. I thought it was complicated to do the change every four hours. Fortunately, my daughter who is a nurse and my husband supported me. Finally, I made a decision and had confidence. I registered [for CAPD therapy]. [P4]
Every three months, [the PD nurse] visited the patients, looked at the patients’ conditions […] the PD nurse often asked if there were any problems […] we got attention. Because what was needed by CAPD patients was guidance from the ones who knew more […] who could inform them about CAPD […] it was important for the patients’ mentality […] it built patients’ confidence. [P1]
Theme 4: following clinical advices
Besides following the procedure of day-to-day self-dialysis and self-care, it was also suggested that once a month the patients see the doctor or CAPD nurse to check their health condition, ask for a dialysate solution prescription, and any other necessary medication. Furthermore, every 6 months they had to go to the hospital to change the transfer set. One participant visited his doctor twice in 3 months to check his health condition on his early day-to-day stage. However, after consulting with another nephrologist in another hospital, he was advised to see the doctor with his laboratory records every month.
For CAPD only, I come, ask for prescription medication, a solution claim, that’s all […] the patient should remember. Only in the beginning, [I] was told every six months to [change] the transfer set. [P1]
I went [to the hospital] once a month to get the [dialysate] solution, to get X ([inject medication] […] I had to be injected with X once a week. [P3]
Theme 5: updating health condition
Since exchanging information about health condition and CAPD therapy was still needed and the home visit program activities became less frequent, one of the participants’ hospitals had created a WhatsApp group as one form of communication media between the patients and the health care professionals. This WhatsApp group was managed by the CAPD nurse. Furthermore, one of the participants took the initiative to form a community and WhatsApp group covering his geographical area as a medium of communication amongst patients.
Nurse E created the group [WhatsApp] […] if we had questions we asked and [our questions] were answered […] if I had a problem, I asked through WhatsApp […] what the medication was, how to solve it. [P2]
I created the group in [my city] city B; it was a month or two months after the CAPD operation. […] In the first year, there were only two people in CAPD [in my area]. Every time there was [a new patient], he [the PD nurse] informed me, [I added] […] in city B almost 30–40 patients [now] […] for instance, if there was a problem, he [the patient] could share in the group, could ask [his or her] seniors rather than go to the hospital […] not waste time. [P1]
Theme 6: supporting CAPD therapy
As the participants had more knowledge and positive experience about CAPD therapy, they shared and recommended CAPD therapy to other people. One of the participants besides sharing his experience organized a CAPD gathering where he invited health care professionals to introduce CAPD therapy. Another participant voluntarily explained and recommended CAPD therapy to an HD patient.
Because in city B, I also have a community. Sometimes when we met, I invited, I gathered all CAPD patients, and I invited [a healthcare provider] […] to give an opportunity to present about CAPD from A to Z. My role was as a committee person […] [I] organized it in order to [make people] know about CAPD. [P1]
I perhaps was a person who brought HD [patient] to CAPD. Every day on my mobile phone there were people who asked about CAPD. I did not know their names, and suddenly they asked about CAPD. It was often and almost every day. I replied, if I had time in the middle of the night. Then they became CAPD patients […] moreover, through my fan page. P1
Yesterday, I met Mrs EN who was an HD patient and I often met her when I went to the clinic. She had never been informed about CAPD and I explained it to her. I recommended her to talk to nurse E [PD nurse]. When I met her again in the clinic she was going to have an operation (Tenckoff). [P4]
Discussion
This pilot study was conducted to explore and understand CAPD patients’ engagement activities with their health care professionals. The results showed six engagement activities: obtaining initial knowledge, developing knowledge and skills, feeling confident, following clinical advices, updating the health condition, and supporting CAPD therapy.
Two important engagement activities which were “obtaining initial knowledge” and “developing knowledge and skill” occurred during pre-CAPD dialysis and training phases. These two activities mainly involve the cognitive dimension of the patients. In pre-CAPD dialysis, ESRD patients started to develop their personal health literacy skills by obtaining initial knowledge about CAPD therapy. They actively tried to get the information either from public information sites such as Internet, other CAPD patients, or health care professionals. Health literacy is defined as “patients’ ability to access, understand, interpret, and use health-related concepts that involve the cognitive and social skills which determine the motivation and ability of individuals to gain access and use information in ways which will promote and maintain good health.”32 A basic level of health literacy would minimize decisional conflict or uncertainty of a decision and support informed decision in shared decision-making process. Therefore, it was necessary to have pre-dialysis information as an element of informed decision.33 This was supported by Taylor et al that patients with advanced kidney disease should have health literacy that included motivation and ability to obtain knowledge and problem-solving strategies. Lelie also argued that the decision with regard to the form of dialysis should be a shared decision between patients and nephrologist.34 Thus, partnership between patients and health care professionals was required from the very beginning of treatment, and the health care professionals should provide health information and patients should act on the information provided.35
The second important cognitive engagement activity was developing knowledge and skills which happened during nurse-to-patients training phase. Proper training was considered as a critical factor that contributes to outcomes and minimizes the risk of infection.36 The patient was taught one-on-one regarding how to perform a self-dialysis, understanding the exchange cycle that includes draining and refilling of dialysate, caring for the exit site, understanding about a proper diet, and nutritional impact as well as the complications of CAPD therapy. As a part of training program, at the end of training, the patients had to demonstrate their ability to perform proper self-dialysis. This training material and procedure was in line with International Society for Peritoneal Dialysis (ISPD) guidelines that recommend teaching procedures and problem-solving strategies. The training program required specific cognitive and motor skills to understand the concept of self-management on PD and to perform self-dialysis.37,38 As for the schedule, it depends on hospital policy, and each patient has different ability to perform the self-dialysis and self-management activities. Barone et al argued that the learning capacity and skills of the patients vary, depending on their degree of education, comprehension, and dexterity.39 The study by Figuerido et al showed that there was no evidence on how the training schedule should be managed and organized.38
Over the years, receiving information and attention from health care professionals during all the three periods of CAPD therapy improved and enhanced patients’ confidence that CAPD was the right therapy when correctly implemented. The role of CAPD or pre-dialysis nurses in educational program was important because in the beginning, patients had limited knowledge about health literacy, and experienced uncertainty and decisional conflict. Therefore, decisional support intervention had helped to improve decision-making process.40 Using educational aids such as video could enhance the educational experience and this was supported by ISPD guidelines.36 Gaining confidence would lead to positive emotion and behavioral responses.41 Home visits were seen with great appreciation by patients as they felt being taken care of. This reflects the importance of the home visit and the construction of the viability of this procedure in addition to the initial stage of treatment.38
In day-to-day phase, the patients also followed the clinical procedures in order to get the best outcome of their health care, including starting day-to-day care process and continuing the monthly and 6-monthly commitment to check their health conditions with their health care professional. A previous study conducted by Yi et al indicated that patient–doctor contact interval of 2 months or less provided positive outcomes in CAPD patients.42
In order to continue and facilitate monitoring and communication, health care professionals initiated the WhatsApp’s group chat as a mobile digital communication channel. The use of social media such as WhatsApp as a medium for discussing health condition and health knowledge had been well established and used among CAPD patients in Indonesia to communicate with health care professionals and with other CAPD patients. Ganasegeran et al indicated that health professionals could communicate quickly and effectively with the patients through WhatsApp.43 A study conducted by Boulus et al showed that through the WhatsApp’ group, the patients can send text messages and share videos or images to health care professionals to update their health condition, especially if there is a health care problem. WhatsApp is a fast and low-cost technology supporting clinical learning and communication, thus improving patient’s adherence to treatment.44 Patient–health care professionals’ engagement activities were improved as a result of better response and understanding of health information.45 Participants who had a positive feeling and experience about CAPD therapy most likely would be persuasive and promote the therapy to others, either face-to-face or through digital media.46 Table 5 provides a summary of patient engagement activities.
  | Table 5 Summary of patient engagement activities Abbreviation: CAPD, continuous ambulatory peritoneal dialysis. |
Limitations and future study
There were some limitations in this study. Small number of participants or patients made it difficult to verify the results. More number of patients in each CAPD phase would generate clear understanding of patient engagement activities. Emotional and behavioral problems that occurred during the engagement process were not analyzed in detail. There was no information about the relationship between CAPD training and the outcome. Future study is recommended to cover in-depth patient engagement activities across the three dimensions (cognitive, emotional, and behavioral dimensions), especially during pre-CAPD therapy as well as training phases, and possibility to relate these activities and dimension with CAPD therapy outcomes, such as health-related quality of life, peritonitis complication, and technical survival. In addition, a study on effectiveness of using social media, with regard to CAPD therapy, as a communication medium between patients and health care professionals would be an interesting area to be explored.
Conclusion
Patient engagement with health care professionals plays an important role in CAPD therapy as it improves health outcomes. Patients should actively engage with health care professionals as early as possible to obtain knowledge about the available RRTs and their consequences. Generally, the engagement activities commenced from cognitive dimensions and were followed by emotional and behavioral dimensions. Obtaining initial knowledge and developing knowledge and skills as part of cognitive dimensions were essential engagement activities in pre-CAPD therapy and training phases. In the day-to-day phase, patients must have already gained sufficient engagement knowledge and experience by which they can share their experiences confidently and recommend other patients to adopt CAPD therapy as their RRT modality.
Disclosure
The authors report no conflicts of interest in this work.
References
Jha V, Garcia-Garcia G, Iseki K, et al. Chronic kidney disease: global dimension and perspectives. Lancet. 2013;382(9888):260–272. | ||
Wearne N, Kilonzo K, Effa E, et al. Continuous ambulatory peritoneal dialysis: perspectives on patient selection in low- to middle-income countries. Int J Nephrol Renovasc Dis. 2017;10:1–9. | ||
Neuen BL, Chadban SJ, Demaio AR, Johnson DW, Perkovic V. Chronic kidney disease and the global NCDS agenda. BMJ Glob Health. 2017;2(2):e000380–e000384. | ||
Hill NR, Fatoba ST, Oke JL, et al. Global Prevalence of Chronic Kidney Disease – A Systematic Review and Meta-Analysis. PLoS One. 2016;11(7):e0158765. | ||
International Society of Nephrology. KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney International Supplements. 2013;3(1):i–xiii;1-150. Available from: https://kdigo.org/wp-content/uploads/2017/02/KDIGO_2012_CKD_GL.pdf. | ||
Saxena R, West C. Peritoneal dialysis: a primary care perspective. J Am Board Fam Med. 2006;19(4):380–389. | ||
Fleming GM. Renal replacement therapy review: past, present and future. Organogenesis. 2011;7(1):2–12. | ||
Riset Kesehatan Dasar, Riskedas 2013, Badan Penelitian dan Pengembangan Kesehatan, Kementrian Keseharan Republik Indonesia [National Institute of Health Research and Development, Basic Health Survey]. Available from: http://www.depkes.go.id/resources/download/general/Hasil%20Riskesdas%202013.pdf. Accessed December 19, 2018. Indonesian. | ||
Hasil Utama Riskedas 2018, Badan Penelitian dan Pengembangan Kesehatan, Kementerian Kesehatan Republik Indonesia [National Institute of Health Research and Development, Basic Health Survey]. Available from http://www.kesmas.kemkes.go.id/assets/upload/dir_519d41d8cd98f00/files/Hasil-riskesdas-2018_1274.pdf. Accessed February 6, 2019. Indonesian. | ||
Indonesian Renal Registry. 10th Report of Indonesian Renal Registry 2017. Available from: https://www.indonesianrenalregistry.org/data/IRR%202017%20.pdf. Accessed December 19, 2018. Indonesian. | ||
Novelia E, Nugraha RR, Thabrany H. Cost effectiveness analysis between hemodialysis and peritoneal dialysis. Jurnal Ekonomi Kesehatan Indonesia. 2017;1(3):120–125. | ||
Prodjosudjadi W. Incidence, prevalence, treatment and cost of end-stage renal disease in Indonesia. Ethn Dis. 2006;16(2 Suppl 2):S2-14-6. | ||
Suhardjono. The development of a continuous ambulatory peritoneal dialysis program in Indonesia. Peritoneal Dialysis Int. 2008;28(3):S59–S62. | ||
Afiatin , Khoe LC, Kristin E, et al. Economic evaluation of policy options for dialysis in end-stage renal disease patients under the universal health coverage in Indonesia. PLoS One. 2017;12(5):e0177436. | ||
Susandijani. Solusi Terapi Penderita Gagal Ginjal? Cek Plus Minusnya. Available from: https://gaya.tempo.co/read/1147254/capd-solusi-terapi-penderita-gagal-ginjal-cek-plus-minusnya?page_num=2. Accessed December 1, 2018. | ||
Anastasia R. Defisit BPJS Kesehatan Membengkak, Pasien GAGAL Ginjal Diharapkan Bisa Cuci Darah Lewat Perut. Available from: http://www.tribunnews.com/nasional/2018/10/31/defisit-bpjs-kesehatan-membengkak-pasien-gagal-ginjal-diharapkan-bisa-cuci-darah-lewat-perut. Accessed December 10, 2018. | ||
Handayani I. Terapi CAPDCapD Lebih Efisien untuk Penyakit GagalGAGAL Ginjal. Available from: https://www.beritasatu.com/kesehatan/519747-terapi-capd-lebih-efisien-untuk-penyakit-gagal-ginjal.html,31 October 2018. Accessed December 1, 2018. | ||
Sinnakirouchenan R, Holley JL. Peritoneal dialysis versus hemodialysis: risks, benefits, and access issues. Adv Chronic Kidney Dis. 2011;18(6):428–432. | ||
Holman H, Lorig K. Patient self-management: a key to effectiveness and efficiency in care of chronic disease. Public Health Rep. 2004;119(3):239–243. | ||
Coulter A. Patient engagement--what works? J Ambul Care Manage. 2012;35(2):80–89. | ||
Hibbard JH. Patient activation and the use of information to support informed health decisions. Patient Educ Couns. 2017;100(1):5–7. | ||
Graffigna G, Barello S, Bonanomi A, Lozza E. Measuring patient engagement: development and psychometric properties of the patient health engagement (Phe) scale. Frontiers in Psychology. 2015;6(274):1–10. | ||
Darmayanti D, Simatupang TM, Rudito P. A pilot study on value co-creation activities in health care: A study on continuous ambulatory peritoneal dialysis. In: Proceedings of the 5th Naples Forum on Service; 6–9 June, 2017; Sorrento, Naples, Italy. | ||
Holloway I, Galvin K. Qualitative Research in Nursing and Healthcare. 4th ed. West Sussex, UK: Wiley Blackwell; 2017. | ||
Yin RK. Case Study Research Design and Methods. London: Sage; 2011. | ||
Patton MQ. Qualitative Research & Evaluation Methods. 3rd ed. Thousand Oaks, CA: Sage; 2002. | ||
Cresswell JW. Educational Research Planning, Conducting, and Evaluating Quantitative and Qualitative Research. Boston, MA: Pearson; 2012. | ||
Whiting LS. Semi-structured interviews: guidance for novice researchers. Nursing Standard. 2008;22(23):35–40. | ||
Dicicco-Bloom B, Crabtree BF. The qualitative research interview. Medical Education. 2006;40(4):314–321. | ||
Saldana J. The Coding Manual for Qualitative Researcher. London: Sage; 2009. | ||
Shenton AK. Strategies for ensuring trustworthiness in qualitative research projects. Education for Information. 2004;22(2):63–75. | ||
Taylor DM, Bradley JA, Bradley C, et al. Limited health literacy in advanced kidney disease. Kidney Int. 2016;90(3):685–695. | ||
Chen N-H, Lin Y-P, Liang S-Y, et al. Conflict when Making decisions about dialysis modality. J Clin Nurs. 2018;27(1–2):e138–e146. | ||
Lelie A. Decision-making in nephrology: shared decision making? Patient Educ Couns. 2000;39(1):81–89. | ||
Paterick TE, Patel N, Tajik AJ, Chandrasekaran K. Improving health outcomes through patient education and partnerships with patients. Proc. 2017;30(1):112–113. | ||
Zhang L, Hawley CM, Johnson DW. Focus on peritoneal dialysis training: working to decrease peritonitis rates. Nephrol Dial Transplant. 2016;31(2):214–222. | ||
Bernardini J, Price V, and Figueiredo A. Peritoneal dialysis patient training, 2006. Peritoneal Dial Int. 2006; 26:625–632. | ||
Figueiredo AE, Bernardini J, Bowes E, et al. A Syllabus for teaching peritoneal dialysis to patients and caregivers. Perit Dial Int. 2016;36(6):592–605. | ||
Barone RJ, Campora MI, Gimenez NS, et al. The importance of the patient’s training in chronic peritoneal dialysis and peritonitis. Adv Perit Dial. 2011;27:97–100. | ||
Loiselle M-C, O’Connor AM, Michaud C. Developing a decision support intervention regarding choice of dialysis modality. Cannt J. 2011;21(3):13–18. | ||
Hibbard JH, Mahoney E. Toward a theory of patient and consumer activation. Patient Educ Couns. 2010;78(3):377–381. | ||
Yi C, Guo Q, Lin J, et al. Patient-doctor contact interval and clinical outcomes in continuous ambulatory peritoneal dialysis patients. Am J Nephrol. 2017;45(4):346–352. | ||
Ganasegeran K, Renganathan P, Rashid A, Al-Dubai SAR. The m-Health revolution: exploring perceived benefits of WhatsApp use in clinical practice. Int J Med Inform. 2017;97:145–151. | ||
Kamel Boulos MN, Giustini DM, Wheeler, S. Instagram and WhatsApp in health and healthcare: an overview. Future Internet. 2016;8(3):37–50. | ||
Antheunis ML, Tates K, Nieboer TE. Patients’ and health professionals’ use of social media in health care: motives, barriers and expectations. Patient Educ Couns. 2013;92(3):426–431. | ||
Willis E. Patients’ self-efficacy within online health communities: facilitating chronic disease self-management behaviors through peer education. Health Commun. 2016;31(3):299–307. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
