Back to Journals » Journal of Asthma and Allergy » Volume 15
Patient Characteristics and Caregiver Asthma Knowledge of Children with Well-Controlled and Poorly Controlled Asthma
Authors Com G, Amin R, Gunnett M, Antonetti C
Received 23 February 2022
Accepted for publication 5 May 2022
Published 11 June 2022 Volume 2022:15 Pages 793—802
DOI https://doi.org/10.2147/JAA.S361135
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Luis Garcia-Marcos
Gulnur Com,1 Raid Amin,2 Mohini Gunnett,3 Callah Antonetti4
1Department of Pediatric Pulmonology, University of Florida, Ascension Sacred Heart, Pensacola, FL, USA; 2Department of Mathematics & Statistics, University of West Florida, Pensacola, FL, USA; 3Department of Pediatric Pulmonology, University of Alabama, Birmingham, AL, USA; 4Department of Pediatrics, University of Florida, Ascension Sacred Heart, Pensacola, FL, USA
Correspondence: Callah Antonetti, Department of Pediatrics, University of Florida and Ascension Sacred Heart, Pensacola, FL, USA, Tel +1 850 416-4071, Fax +1 850 416-4246, Email [email protected]
Purpose: To describe the socio-demographics and clinical characteristics of children in a pulmonology clinic or admitted to a children’s hospital with well-controlled and poorly controlled asthma, and to assess caregiver knowledge of asthma pathogenesis, treatment, and self-management.
Patients and Methods: A cohort of 132 children aged 2– 18 years and their caregivers seen in a pediatric pulmonology clinic with a diagnosis of asthma (n=112) or admitted to the hospital with a diagnosis of asthma exacerbation (n=20) were invited to participate in a cross-sectional study. Caregivers completed a survey, which healthcare providers then used to tailor asthma education to the patient and caregiver. Two-tail t-tests and Chi-square tests were used to compare demographics and clinical characteristics of children with well-controlled vs poorly controlled asthma.
Results: Of 132 children, 111 children in this cohort had poorly controlled asthma (84%). Medicaid insurance was associated with poorly controlled asthma versus well-controlled asthma (63% vs 35% p=0.01). Asthma action plans (AAP) had previously been given to 113 caregivers (86%), but caregivers of children with both well-controlled and poorly controlled asthma still reported misconceptions about asthma pathology and management, such as stopping daily medications when asthma is controlled.
Conclusion: This study contributes to the existing evidence that socio-demographics have a significant impact on asthma prevalence and proper management. Our study suggests that caregivers of children with asthma need comprehensive asthma education beyond the AAP focusing on asthma-related misconceptions.
Keywords: asthma, asthma education
Introduction
Asthma is the third leading cause of hospitalization in children under 15 years of age.1 The Florida Department of Health reports that one in five children have a diagnosis of asthma in their lifetime.2 Asthma is prevalent among underprivileged, minority, and urban children, who also endure a disproportionate burden of preventable asthma-related morbidity including emergency department (ED) visits, hospitalization, and missed days of school.3 A multistate survey to identify racial disparities in children with asthma showed that 39% of Black children had asthma-related ED visits and hospitalizations compared with 18% of White children.4
In the United States, Medicaid insurance eligibility is determined by household income. In the state of Florida, a family of four would qualify for Medicaid insurance with a household income below $36,908 USD.5 Results from the 2008–2013 Medical Expenditure Panel Survey indicated that a significantly higher proportion of Medicaid coverage was required for persons with asthma (33%) in comparison to those without asthma (17%).6 Florida’s fiscal year 2010–2012 report noted that children with Medicaid coverage had a higher prevalence of asthma, and that there was a significant increase in the number of asthma-related ED visits among patients with Medicaid, whereas patients with commercial insurance demonstrated an overall decrease in asthma-related ED visits.7
In Escambia County, FL, the Black community represents 23% of the population, above the national average of 13%.8 Roughly 17% of all Escambia County residents live in poverty and households with children are disproportionately affected, with 26% of children living in poverty.8 While the average asthma prevalence is 11.2% across the state, Escambia County has a prevalence between 12.5% and 15%.2
The Studer Family Children’s Hospital at Ascension Sacred Heart, affiliated with University of Florida Health, is located in Escambia County and is the only pediatric hospital in the Florida panhandle. Approximately 1400 children per year were treated for asthma in the hospital’s ED between 2015 and 2017 and a majority of these children lived in Pensacola, Escambia County. Mirroring state data, 78% of these children treated in the ED had government-issued Medicaid insurance (unpublished data).
Studies have shown that asthma exacerbations are preventable when patients and caregivers receive formal education for asthma self-management.3,9 Empowering children and caregivers with the required knowledge and self-management skills is necessary to achieve proper asthma control.10 Despite this evidence, parents of children with asthma continue to have various misconceptions regarding asthma management.11,12 Therefore, caregiver knowledge of asthma management is an important component of pediatric asthma control. In this study, we aimed to investigate the socio-demographics and clinical characteristics of a cohort of children who reside in Northwest Florida with asthma, as well as caregiver knowledge and self-management skills. Objectives of this study were to:
- Describe the socio-demographics and clinical characteristics of children with asthma referred to the outpatient pediatric pulmonology clinic and those who were admitted to the hospital with an asthma exacerbation.
- Investigate the relationship between socio-demographics, clinical characteristics, and poor asthma control.
- Assess caregiver knowledge of basic asthma pathogenesis, treatment, and self-management.
Methods
Study Design
This cross-sectional study was conducted from September 2018 through October 2019. The study was approved by the Sacred Heart Clinical Institutional Review Board number 1204007-3. Participation was voluntary and informed consent was waived as approved by the IRB. The study was performed in two different settings:
Outpatient Pediatric Pulmonology Clinic
In this setting, children referred to the pediatric pulmonology clinic with a diagnosis of asthma were studied. Initial asthma diagnosis was made by the primary care physician, although some patients were diagnosed by other pediatric pulmonologists. After the asthma diagnosis was confirmed by the study pediatric pulmonologist (GC), the purpose of the study survey was explained to the patient’s caregiver. Caregivers completed the survey prior to receiving asthma education to gauge baseline asthma knowledge and self-management skills. Asthma education was then provided by the pediatric pulmonologist, respiratory therapists and specialty nurses. Education focused on pathogenesis, signs and symptoms of asthma, triggering factors, and asthma self-management. Additional education was provided through discussion of survey answers with caregivers, with focus placed on any incorrect and unknown answers.
Children’s Hospital Inpatient Units
In this setting, caregivers of children admitted to the hospital with an asthma exacerbation and treated as per the hospital’s asthma treatment protocol were approached by a provider on their care team and the purpose of the survey was explained. Inpatient care team providers included pediatric and family medicine residents, pediatric nurse practitioners, pediatric hospitalists, and the study pediatric pulmonologist. Asthma education in the hospital was completed by these providers based on the same curriculum above from the pulmonology clinic. Providers then completed additional education through discussion of survey answers with the caregivers, with focus placed on any incorrect and unknown answers.
Inclusion and Exclusion Criteria
Children between 2 and 18 years of age with a diagnosis of asthma as per the 2018 Global Initiative for Asthma (GINA) guidelines given by a pediatric pulmonologist or an admission to the hospital with a diagnosis of asthma exacerbation and treated as per the hospital’s asthma treatment protocol were included in the study.13 Children with morbidities other than asthma or with diagnoses of other pulmonary pathologies were excluded. No children included in the study used single maintenance and reliever therapy (SMART), as this had not been implemented in the community at the time of the study. Participation in the survey was optional and caregivers who declined to participate in the survey were excluded.
Data Collection for Socio-Demographics and Clinical Characteristics
The survey questionnaire consisted of four sections. The first section collected data on socio-demographic variables including child’s age, sex, self-reported race, type of the health insurance (Medicaid versus non-Medicaid), residential zip code, and BMI. Children were defined as obese if their BMI was at or above the 95th percentile for age and sex. Asthma-related hospitalizations within the past 12 months were self-reported or based on medical records when available. Additional data was collected for patients at their initial pulmonology clinic visit including Asthma Control Test (ACT) scores and forced expiratory flow in one second (FEV1) measurements. Total IgE levels and existence of allergies (indoor, outdoor) measured by an in-vitro quantitative assay were based on the medical record when available. Duration of asthma diagnosis, co-existence of atopic dermatitis, and allergic rhinitis were recorded from medical records when available.
Data Collection for Asthma Knowledge and Self-Management
The second section of the survey included 12 questions and aimed to investigate caregivers’ comfort level with asthma self-management at home. The third section included 12 Likert 5-point scale questions developed by the authors after review of literature, incorporation of professional experience, and with slight modification of a survey initially developed by Rodriguez-Martinez and adapted by Franken et al.3,14 These questions related to the fundamental aspects of asthma to assess parental understanding of the etiology and pathology of the disease, triggering factors, and signs and symptoms. The fourth section included 14 Likert 5-point scale questions assessing caregiver asthma self-management and monitoring skills. Some questions specifically focused on misconceptions about asthma management (see Appendix for survey questions). The survey was analyzed using Microsoft Word for Mac version 15.4 readability statistics. The survey had a Flesch-Kincaid readability test score of 5.8. This corresponds to a US 5th grade reading level or average reading ability of an 11-year-old student.
Definition of Children with Poor Asthma Control
Survey participants were divided into two groups: children with “well-controlled asthma” and “poorly controlled asthma,” to investigate if there were any differences in socio-demographics and clinical characteristics between the two groups. Patients were described as having poorly controlled asthma if they met any of the below criteria.15–18
Statistical Analysis
The Statistical Analysis System (SAS) was used throughout the statistical analysis. A significance level of 0.05 was chosen. A test was deemed significant if its p-value was less than 0.05. A two-tail t-test was used for comparing the two mean values for variables with continuous values, such as comparing the mean age of children with well-controlled asthma versus the mean age of children with poorly controlled asthma. A Chi-square test for independence was used when testing for an association between two categorical variables, such as insurance type and asthma control. These two types of tests do not require equal sample sizes.
Results
Socio-Demographics
Of 132 total survey participants, 112 were seen at the pediatric pulmonology clinic and 20 were admitted to the hospital with an asthma exacerbation. The mean age was 8.9 years (±4.658), with minimum age 2.5 years and maximum age 18 years. There were 73 males (55%) and 59 females (45%). White children comprised the majority (57%) of the patients, followed by Black or African American children (43%). Black and White race was reported by 1% of patients, and Pacific Islander and White race was also reported by 1% of patients. Seventy-seven (53%) children were under Medicaid insurance versus 54 (47%) children with non-Medicaid insurance. Out of 114 children with a documented BMI, 88 (77%) were obese. In 120 children whose asthma duration data was available, 39 (33%) had an asthma diagnosis of less than 1 year, 33 (28%) had an asthma diagnosis between 1 and 5 years, 19 (16%) between 5 and 10 years and 29 (24%) more than 10 years. Sixty-three children (48%) resided in Escambia County, FL. Remaining children were noted to be from neighboring counties including 37 (28%) from Santa Rosa County and 15 (11%) from Okaloosa County, within 1.5 hours from the hospital. Ten children (8%) were from surrounding counties in Alabama within a three-hour radius, and one child was from Gulf County, Florida, roughly three hours away from the hospital.
Clinical Characteristics
Out of 132 children, 20 were in the hospital with a current asthma exacerbation. Of the 112 children who were seen in the pediatric pulmonology clinic, 42 (35%) also had a history of hospitalization within the previous 12 months. FEV1 measurements were available for 86 out of 112 children seen in clinic, with 68 (79%) of these children having FEV1 <80% predictive values. ACT questionnaire was available for 109 out of 112 children seen in the clinic, with 66 (61%) of these children having an ACT score <20. Overall, 111 of 132 children (84%) had at least one of the three previously defined criteria of poorly controlled asthma. IgE measurements were available in 77 children, and in 30 (39%) of these children, the levels were above age-based normal levels. Indoor allergies were positive in 44 of 77 (62%) children, and outdoor allergies were positive in 34 of 77 (45%) children.
To determine if there were differences between children with well-controlled asthma and poorly controlled asthma, we compared the demographics and clinical characteristics of these two groups (Table 1). There were no statistically significant differences between the two groups in age, gender, and rate of obesity. Children with Medicaid insurance had significantly higher rates of poorly controlled asthma compared to well-controlled asthma (63% vs 35%, p = 0.01). Black or African American children were more common in the poorly controlled asthma group (44%) compared to the well-controlled asthma group (20%), however this did not reach a statistically significant level (p=0.09). The majority of children had atopic asthma (61%), but there was no statistically significant difference between the two groups regarding IgE levels, indoor/outdoor allergies, existence of atopic dermatitis, or allergic rhinitis.
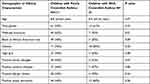 |
Table 1 Demographics and Clinical Characteristics of Children with Poorly Controlled versus Well-Controlled Asthma |
Evaluation of Caregiver Comfort Level of Asthma Management and Their Resources
Of the total 132 caregivers surveyed, 93 (71%) stated that they felt comfortable with their child’s asthma care at home, including 12 of 20 (63%) caregivers whose child was in the hospital with an asthma exacerbation. Asthma action plans (AAP) had been given to 113 (86%) caregivers before the survey encounter day. Survey results indicated that 42 (32%) caregivers expressed feelings of helplessness in dealing with their child’s asthma. Twenty (15%) caregivers agreed that they had problems with making or keeping appointments with their healthcare providers, and 22 (17%) caregivers stated they had run out of medicines for their child’s asthma and did not have any on hand when their child had an asthma exacerbation.
Caregiver Understanding of the Fundamental Pathology of Asthma, Triggers and Symptoms, Medications, and Self-Management
About 80% of caregivers knew that asthma is lung inflammation causing airway linings to swell and make muscles around the airways narrow during the asthma exacerbation. However, 75 (57%) caregivers did not know asthma can be a reaction to allergies, and 59 (45%) did not think that a common cold was one of the main triggers of asthma. More than 90% of caregivers were aware of asthma-related symptoms. Most caregivers (87 of 132, 65%) did not know the difference between daily asthma controller medications and rescue medications.
Caregiver Understanding of Asthma Myths and Misconceptions
Most caregivers (86%) disagreed with the statement that “asthma is an infection that one can catch from others.” Majority of the responders (89%) agreed that that children with asthma should be allowed to participate in sports, and 78% agreed that with proper treatment, children with asthma can lead a good quality of life. However, 85% of caregivers agreed and 13% were unsure that daily controllers can be stopped when the child’s symptoms were controlled. In addition, 67 (36%) caregivers either agreed or were unsure that asthma medications are addictive (Table 2). There were no significant differences between caregivers of children with well-controlled and poorly controlled asthma in their responses to the asthma myths and misconception questions.
 |
Table 2 Caregiver Response to Survey Statements About Asthma Myths and Misconceptions |
Discussion
In this study, we found that the majority of children in the study cohort had poorly controlled asthma. This finding could be expected, as patients were encountered either during a hospitalization for an asthma exacerbation or through referral to the pediatric pulmonologist. Black children comprised 43% of the total cohort, a greater rate than the general population in the area, and consistent with prior studies showing high asthma prevalence or asthma-related morbidity in Black children. Consistent with prior Florida asthma reports, more than half of the children received Medicaid coverage, which was a significant risk factor for poorly controlled asthma in this cohort. Most of the children were obese and had atopic asthma, but these factors were not significantly associated with poorly controlled asthma.
While our study was consistent with prior studies as noted above suggesting high prevalence of poorly controlled asthma in children with Medicaid coverage and who identify as Black, our study is unique in several ways. The socio-demographics are specific to our geographic location and describe a population of patients at a community-based hospital in a rural setting. By using the same pediatric pulmonologist and provider educational curriculum in the inpatient and outpatient setting, there was consistency in diagnosis, management, and education. We used multiple measures of asthma control and asthma phenotype including ACT, FEV1, blood eosinophils, and IgE levels. Despite 86% of our caregivers having previously received an asthma action plan and 71% reporting feeling comfortable with asthma management, most of our patients still had poorly controlled asthma and nearly one-third of caregivers reported feeling hopeless in managing their child’s asthma. This highlights the need for an increase in healthcare resources for asthma education, and consideration of social determinants of health when providing asthma education and management.
Despite the availability of effective treatment, children from minority communities continue to experience disproportionate morbidity from asthma.6 A survey-based study showed that twice as many Black children had asthma-related ED visits and hospitalizations compared to White children, 39% vs 18%, respectively.4 ED visits have been positively correlated with short-acting beta agonist use and were negatively correlated with inhaled corticosteroid use when stratified by race and ethnicity.4 Nearly half of the children in our cohort lived in Escambia County and mirroring the Florida asthma reports, Black children with asthma were represented at a higher rate at our institution. In addition, our study showed that Black children had a higher rate of poorly controlled asthma although this did not reach a statistically significant level.
Social determinants of health such as household income and access to medical care are used to describe the effect of these problems on health. Social determinants of health also impact some groups more negatively than others, leading to some groups being less healthy than others.19 Fiscal year 2010 report showed that in Florida, children under Medicaid coverage had a higher prevalence of asthma and a significant increase in the number of asthma-related ED visits, while visits decreased in individuals covered by commercial insurance.20 In our cohort, Medicaid insurance coverage was the only statistically significant socio-demographic factor associated with poorly controlled asthma. Households with the lowest income levels (<$15,000) have the highest prevalence of lifetime and current asthma.20 About 17% of Escambia County residents live in poverty, and households with children are disproportionately affected, with 26.4% of children living in poverty.21 Our survey showed that although most caregivers stated that they felt comfortable with their child’s asthma care, and they did not have problems with access or getting their prescriptions refilled, 32% felt helpless while dealing with their child’s asthma indicating that there may be factors that they cannot control to prevent their child’s asthma attacks. High out-of-pocket costs may preclude purchasing asthma medications, which is a common problem seen in our clinic. Transportation can be problematic for some families, and although Medicaid provides a van for those lacking transportation, this service is not always readily available. Many families in our cohort had to travel more than one hour and in some cases, up to three hours to be seen by a pulmonologist or to be treated in our hospital. These social determinants of health may be contributing to feelings of helplessness among caregivers of children with asthma.
Asthma is defined as “controlled” if a patient reports no day and nighttime symptoms, use of rescue medication less than twice a week, and no activity limitation.15–18 The ACT is a well validated test and is used in the clinical practice.22,23 The Childhood Asthma Control Test (C-ACT) is also among the validated instruments included in the current asthma guidelines to assess asthma control in children ages 4–11 years.22 Objective asthma control tools include spirometry testing (FEV1). Asthma exacerbations, asthma-related ED visits, and hospitalization within the past year are other objective measures of poor asthma control.15–17 Asthma-related hospitalization also is a predictor of future hospitalization.14 We used ACT (<20), FEV1 (<80pp) and asthma exacerbation-related hospitalization during the past year as asthma control measures. Most of the children had one of these measures indicating a high rate of poor asthma control in our cohort. As our patients were recruited either from the hospital or from a pulmonology clinic, this may have created a selection bias toward including children with persistent symptoms and may explain the high rate of uncontrolled asthma. However, other studies performed in varied settings have also shown a high rate of poorly controlled asthma in children. One study found that the majority of children (75%) with asthma aged 5 to 13 years were poorly controlled, as defined by the 1999 Canadian Asthma Consensus Report.24 In another study, 49% of 572 Swiss-German children with wheezing had unsatisfactory control associated with sleep disturbances, restricted activities and school absenteeism.25 A telephone-based survey found that of those with moderate persistent asthma, 63.8% had a physical activity limitation.26 Asthma control in children is multi-factorial and can be challenging for caregivers, and the high rate of poorly controlled asthma in our cohort is consistent with prior studies.
Obesity is not only a risk factor for the development of asthma but is also associated with worse asthma-related outcomes.27 Similar to asthma, racial and ethnic disparities exist within obesity prevalence in the United States.28 Non-Hispanic Black adults have a 51% higher rate of obesity, and Hispanic adults have a 21% higher rate of obesity when compared with non-Hispanic White adults.28,29 Obese children have a decreased response to inhaled budesonide on measures of lung function, ED visits, and hospitalizations for asthma.30 Obese children require more rescue medication and frequent oral steroid use.29 Children from low-income families are more likely to be obese.31 The 2010 Florida Asthma Report showed that students with current asthma had a higher prevalence of being overweight compared to students who never had asthma and students with former asthma.2 Our study found high rates of obesity in children with both poorly controlled and well-controlled asthma. Obesity remains a modifiable risk factor for asthma in children and should be addressed as part of a comprehensive asthma educational plan.
Prior studies have shown that better knowledge of asthma self-management is associated with improved lung function, reduction of school absenteeism and ED visits.9–12 Education of caregivers of children with asthma and clinician-generated AAPs are important components of asthma education and acceptable asthma control as recommended in the practice guidelines.22 Evidence indicates that written AAPs are effective in the self-management of childhood asthma.22 In this study, we found that 86% of caregivers had been provided with an AAP by previous healthcare providers. We found that majority of caregivers were knowledgeable about asthma pathology and its symptoms. However, a majority of the children still had poorly controlled asthma, suggesting that an AAP alone does not guarantee asthma control. Our survey showed that about half of caregivers did not know about asthma triggers such as allergen exposure or a common cold. Only 34% of the parents knew their child’s asthma medications correctly. These findings are similar to a Canadian report that investigated the characteristics of children with poor asthma control. In their cohort, 75% of 153 children had poorly controlled asthma, and in 59 children who reported receiving asthma education at any time in the past, 70% had poorly controlled asthma.24 Our findings may indicate that although our patients were given an AAP, they did not receive comprehensive asthma education, or their knowledge waned over time. In our daily practice, we frequently observe that AAPs are misplaced or discarded quickly. Asthma education is complex and needs repetition to understand and retain.3 Unfortunately, the traditional healthcare system does not always support the extensive educational role recommended by asthma guidelines. As a result, many providers do not have time to spend with their patients and discuss the fundamental pathology of asthma, triggering factors, and asthma self-management at home, which may contribute to poor control.
Popular misconceptions about asthma may amplify fears about the side effects of asthma medications, limit engagement of children in physical activities, and lead to behaviors that hamper the control of the disease.12,32,33 While many families reported a good understanding of the illness, most caregivers believed that inhaled steroids could be stopped when their child’s symptoms were controlled, and over one-third believed that asthma medications could cause addiction. There were no significant differences between responses of myths and misconceptions between caregivers of children with well-controlled vs poorly controlled asthma. This suggests that even if asthma is well-controlled misconceptions may persist, and that caregivers with correct asthma knowledge may still have difficulty controlling their child’s asthma due to factors beyond their control. These kinds of misconceptions about asthma management are not routinely addressed on AAPs, but are an essential part of asthma education for patients and caregivers to lead to improved control. To overcome these paradigms, much effort is required from all parties involved in asthma management. Asthma education programs involving local communities such as school asthma programs and asthma education delivered in the homes of young children may be helpful as well.
Study Limitations
When we designed the study, we did not expect that the majority of our children would have poorly controlled asthma that resulted in a very small number of children with well-controlled asthma. To prevent error when we compared this unequal number of two groups, we used statistical methods to compare the unequal sample sizes. A power analysis revealed that the t-test has power=68% while the Chi-square tests has statistical power ranging from 80% to 90% depending on the number of categories in the frequency table.
Since study children were enrolled either when they were admitted to the hospital with asthma exacerbations or when they were referred to the subspecialty clinic, there was a selection bias towards including sicker children to the study. Although we have made every effort to adjust the survey questionnaire language to the 5th grade education level, it is possible that parents may have misunderstood the questions or may have marked some questions erroneously. In addition, this study assessed caregiver asthma knowledge at one point in time and did not determine the effectiveness of the asthma education provided over a period of time. A future study following a cohort of children with poorly controlled asthma over time to determine how caregiver asthma knowledge and their child’s asthma control changes over time with repetitive education using the study survey could address this limitation.
Conclusions
This study provides a valuable understanding of the socio-demographic characteristics of children with asthma residing in Northwest Florida. It also helps to better understand caregiver perception of asthma pathology and management, to identify barriers to better asthma control. Our study provides evidence regarding caregivers’ perceptions and asthma management practices, which in turn may help healthcare providers focus their education on areas that are poorly understood by caregivers and to address common misconceptions.
In this study, the majority of patients had poorly controlled asthma and Medicaid insurance was associated with this. Most patients with both well-controlled and poorly controlled asthma were obese. Many caregivers demonstrated knowledge of basic asthma pathophysiology and self-management, though nearly 1 in 3 caregivers reported feelings of helplessness in managing their child’s asthma, suggesting social factors may play a role in asthma control. Multiple medication misconceptions were prevalent among caregivers of children with both well-controlled and poorly controlled asthma.
We hope that the current study and similar studies will encourage third-party payers and hospital administrations that providing an AAP alone is insufficient for asthma control without additional education. Initial comprehensive education should be followed by reinforcements during each patient encounter, along with addressing other modifiable risk factors such as obesity, as well as assessment of family and community resources to address social determinants of health. While providers generate revenue for their asthma education time, insurance companies, especially Medicaid, will save money in the long term with less frequent asthma-related ED visits and hospitalizations if they incentivize asthma education resources. We hope for a future where asthma education encompasses addressing asthma-related racial disparities, social determinants of health, comprehensive asthma education at schools and at home, and community awareness events to improve asthma control for children across the country.
Funding
This study has no funding support.
Disclosure
Authors have no conflict of interest.
References
1. AAFA. Asthma and Allergy Foundation of America; 2021. Available from: http://aafa.org.
2. Florida Department of Health, Division of Community Health Promotion, Bureau of Chronic Disease Prevention, Florida Asthma Program. Burden of Asthma in Florida; 2013. Available from: http://www.floridahealth.gov/diseases-and-conditions/asthma/_documents/asthma-burden2013.pdf.
3. Franken MMA, Veenstra-van Schie MTM, Ahmad YI, Koopman HM, Versteegh FGA. The presentation of a short, adapted questionnaire to measure asthma knowledge of parents. BMC Pediatr. 2018;18(1):14. PMID: 29373963; PMCID: PMC5785890. doi:10.1186/s12887-018-0991-4
4. Oraka E, Iqbal S, Flanders WD, Brinker K, Garbe P. Racial and ethnic disparities in current asthma and emergency department visits: findings from the National Health Interview Survey, 2001–2010. J Asthma. 2013;50(5):488–496. PMID: 23544662; PMCID: PMC4566965. doi:10.3109/02770903.2013.790417
5. Florida Medicaid. Department of Health And Human Services; 2022. Available from: https://www.benefits.gov/benefit/1625.
6. Nurmagambetov T, Kuwahara R, Garbe P. The economic burden of asthma in the United States, 2008–2013. Ann Am Thorac Soc. 2018;15(3):348–356. PMID: 29323930. doi:10.1513/AnnalsATS.201703-259OC
7. Florida Department of Health, Division of Environmental Health, Bureau of Environmental Public Health Medicine, Florida Asthma Program. Asthma Surveillance Plan; 2014. Available from: http://www.floridahealth.gov/diseases-and-conditions/asthma/_documents/surveillance-plan-09-14.pdf.
8. Quick Facts Escambia County, Florida. United States Census Bureau; 2021. Available from: https://www.census.gov/quickfacts/fact/table/escambiacountyflorida.
9. Noureddin AA, Shaaban KM, Mohamed SOO, Abdalla AA, Mahmoud AAA, Salman MST. The knowledge attitude and practice (KAP) of mothers of asthmatic children toward asthma in Khartoum asthma clinics. Sci Rep. 2019;9(1):12120. PMID: 31431663; PMCID: PMC6702345. doi:10.1038/s41598-019-48622-2
10. Al-Zalabani AH, Almotairy MM. Asthma control and its association with knowledge of caregivers among children with asthma. A cross-sectional study. Saudi Med J. 2020;41(7):733–739. PMID: 32601642. doi:10.15537/smj.2020.7.25167
11. Abu-Shaheen AK, Nofal A, Heena H. Parental perceptions and practices toward childhood asthma. Biomed Res Int. 2016;2016:6364194. PMID: 27843948; PMCID: PMC5097792. doi:10.1155/2016/6364194
12. Spykerboer JE, Donnelly WJ, Thong YH. Parental knowledge and misconceptions about asthma: a controlled study. Soc Sci Med. 1986;22(5):553–558. PMID: 3704691. doi:10.1016/0277-9536(86)90022-5
13. Global Initiative for Asthma. Global strategy for asthma management and prevention; 2018. Available from: www.ginasthma.org.
14. Rodríguez-Martínez CE, Sossa-Briceño MP, Castro-Rodriguez JA. Predictors of hospitalization for asthma in children: results of a 1-year prospective study. Pediatr Pulmonol. 2014;49(11):1058–1064. PMID: 24376022. doi:10.1002/ppul.22936
15. Papaioannou AI, Kostikas K, Zervas E, Kolilekas L, Papiris S, Gaga M. Control of asthma in real life: still a valuable goal? Eur Respir Rev. 2015;24(136):361–369. PMID: 26028647. doi:10.1183/16000617.00001615
16. Bime C, Nguyen J, Wise RA. Measures of asthma control. Curr Opin Pulm Med. 2012;18(1):48–56. PMID: 22081089; PMCID: PMC7274081. doi:10.1097/MCP.0b013e32834db0f2
17. Miller MK, Lee JH, Miller DP, Wenzel SE; TENOR Study Group. Recent asthma exacerbations: a key predictor of future exacerbations. Respir Med. 2007;101(3):481–489. PMID: 16914299. doi:10.1016/j.rmed.2006.07.005
18. Lo DK, Beardsmore CS, Roland D, et al. Lung function and asthma control in school-age children managed in UK primary care: a cohort study. Thorax. 2020;75(2):101–107. PMID: 3166638. doi:10.1136/thoraxjnl-2019-213068
19. Ungar WJ, Paterson JM, Gomes T, et al. Relationship of asthma management, socioeconomic status, and medication insurance characteristics to exacerbation frequency in children with asthma. Ann Allergy Asthma Immunol. 2011;106(1):17–23. PMID: 21195940; PMCID: PMC4940175. doi:10.1016/j.anai.2010.10.006
20. State financial reports. My Florida CFO; 2019. Available from: https://www.myfloridacfo.com/division/aa/reports/.
21. Community Needs Assessment. Escambia county official website; 2014. Available from: https://myescambia.com/docs/default-source/sharepoint-natural-resources-management/RESTORE/Meetings/10-6-2014/community-needs-assessment---report.pdf?sfvrsn=69a0c391_3.
22. Dinakar C, Chipps BE, Matsui EC. Clinical tools to assess asthma control in children. Pediatrics. 2017;139(1):e20163438. PMID: 28025241. doi:10.1542/peds.2016-3438
23. Guevara JP, Wolf FM, Grum CM, Clark NM. Effects of educational interventions for self -management of asthma in children and adolescents: systematic review and meta-analysis. BMJ. 2003;326(7402):1308–1309. doi:10.1136/bmj.326.7402.1308
24. McGhan SL, MacDonald C, James DE, et al. Factors associated with poor asthma control in children aged five to 13 years. Can Respir J. 2006;13(1):23–29. PMID: 16470250; PMCID: PMC2539007. doi:10.1155/2006/149863
25. Kuehni CE, Frey U. Age-related differences in perceived asthma control in childhood: guidelines and reality. Eur Respir J. 2002;20(4):880–889. PMID: 12412679. doi:10.1183/09031936.02.00258502
26. Fuhlbrigge AL, Adams RJ, Guilbert TW, et al. The burden of asthma in the United States: level and distribution are dependent on interpretation of the national asthma education and prevention program guidelines. Am J Respir Crit Care Med. 2002;166(8):1044–1049. PMID: 12379546. doi:10.1164/rccm.2107057
27. Mohanan S, Tapp H, McWilliams A, Dulin M. Obesity and asthma: pathophysiology and implications for diagnosis and management in primary care. Exp Biol Med. 2014;239(11):1531–1540. PMID: 24719380; PMCID: PMC4230977. doi:10.1177/1535370214525302
28. CDC. Differences in prevalence of obesity among black, white, and Hispanic adults–United States. MMWR. 2009;58:740–744.
29. Black MH, Smith N, Porter AH, Jacobsen SJ, Koebnick C. Higher prevalence of obesity among children with asthma. Obesity. 2012;20(5):1041–1047. PMID: 22252049; PMCID: PMC3348709. doi:10.1038/oby.2012.5
30. Forno E, Lescher R, Strunk R, Weiss S, Fuhlbrigge A, Celedón JC; Childhood Asthma Management Program Research Group. Decreased response to inhaled steroids in overweight and obese asthmatic children. J Allergy Clin Immunol. 2011;127(3):741–749. PMID: 21377042; PMCID: PMC3056233. doi:10.1016/j.jaci.2010.12.010
31. Centers for Disease Control and Prevention. Childhood obesity facts; 2018. Available from: https://www.cdc.gov/obesity/data/childhood.html.
32. Rubin BK. Asthma myths, controversies, and dogma. Paediatr Respir Rev. 2015;16(2):83–87. PMID: 25245191. doi:10.1016/j.prrv.2014.09.001
33. Rastogi D, Gupta S, Kapoor R. Comparison of asthma knowledge, management, and psychological burden among parents of asthmatic children from rural and urban neighborhoods in India. J Asthma. 2009;46(9):911–915. PMID: 19905917. doi:10.3109/02770900903191323
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
