Back to Journals » Journal of Multidisciplinary Healthcare » Volume 12
Parental child feeding practices and their relationship with children’s dietary intake and weight status in Nepal
Authors Pandey S , Rai S, Paudel N , Shrestha A, Gautam S
Received 18 November 2018
Accepted for publication 6 March 2019
Published 30 April 2019 Volume 2019:12 Pages 325—333
DOI https://doi.org/10.2147/JMDH.S195106
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Shrijana Pandey,1 Suja Rai,1 Narayani Paudel,1 Anu Shrestha,1 Saroj Gautam2
1Department of Nursing, Kathmandu Medical College, Kathmandu University, Kathmandu, Nepal; 2Department of Orthopedics, Kathmandu Medical College, Kathmandu University, Kathmandu, Nepal
Background: Small children have less control over their dietary intake and parents have a major role to play in it. The aim of our study was to determine parental child feeding practices and their association with the weight status and dietary intake of the child.
Design and methods: A cross-sectional study was conducted among 138 parents and preschool children attending two private schools in Kathmandu Valley, Nepal using a structured questionnaire. Parents filled in a self-report questionnaire to assess child feeding practices, perceived activity level of the child, and dietary intake at home. Child’s height and weight was measured using a standard height scale and a digital weighing scale. A digital food scale was used for measuring dietary intake.
Results: Eight percent of the children were overweight and another 8% were obese. On bivariate analysis, the BMI of parents had weak, positive, and significant correlation (r=0.206, p=0.016 for fathers; r=0.307, p≤0.001 for mothers) with child’s weight status. Similarly, concern about child’s overweight had a significant, positive correlation (r=0.232, p=0.006) with the weight status of the child. Furthermore, these three independent variables were found to be significant predictors of a child’s weight status on multivariate analysis. None of the studied independent variables was associated with dietary intake.
Conclusion: The study concludes that parental BMI and parental concern about the child being overweight is significantly associated with the weight status of the child.
Keywords: childhood obesity, Kathmandu valley, private schools, role of parents, young children
Introduction
Parents have a major role in the development of healthy eating behaviors, food values, and preferences in a child. The health of a child largely depends on the nutritional habits that are formed in the earlier stages of their life.1 The first 5 years of life, which comprise rapid physical as well as psychological growth, are the time when eating behaviors develop that serve as the basis for future eating.2 Dietary intake and lifestyle are modifiable risk factors associated with childhood obesity and preventive interventions should be directed to change these behaviors.3 Furthermore, any intervention to cut down the risk of childhood obesity should start before school years as parents have significant control of what children eat and how to control their environment.4 Certain child feeding practices like exerting excessive control over what and how much children eat, pressurization, and restriction have been found to contribute to increased weight gain in childhood.5,6 Similarly, parents can control a child’s food choices by either restricting them from eating high sugar food, pressurizing them to eat more, or using food as a reward for good behavior.7 In addition to feeding practices, a research study has also shown that a child’s physical activity and amount of television viewing are important contributors to increased weight gain in childhood in which parents have an influential role to play.8
Childhood obesity has reached epidemic levels in developed countries. The prevalence of obesity in the USA among the youth aged 2–19 years is 17% while that in preschool children is 8.9%.9 Similarly, in England, 30% of children aged 2–15 years are reported to be overweight and 17% are obese.10 The overall burden of childhood overweight/obesity has been reported to have increased remarkably in the last three decades and the rate is more alarming in developing countries.11 According to the World Health Organization (WHO), the number of Asian children under 5 years of age who are overweight has risen from 13.9 million in 2000 to 17.5 million in 2017. Furthermore, in Africa, this has increased from 6.6 million in 2000 to 9.7 million in 2017.12 In Nepal, overall, 1% of children under 5 years of age were found to be overweight.13 Even so, studies have shown that a remarkably significant number of children studying at private schools in Nepal are overweight as compared to those going to government schools.14,15 Moreover, studies have also revealed that the percentage of overweight children attending private schools ranges from 13.7 to 14.6% while obesity lies between 5.8 and 11.3%.15,16 In Nepal, factors associated with childhood obesity have been reported to be an advantaged ethnic group, families with higher socioeconomic status, watching television for long durations, consuming less fruit/vegetables, and families with fewer siblings.16,17 To the researchers’ best knowledge, no study has been carried out to assess parental feeding practices and child’s weight status or dietary intake. Overweight children of today are more likely to turn into obese adults, which is a great public health concern.18 Since parents can have a significant contribution in shaping the eating habits of young children, we were interested in carrying out a study to assess the child feeding practices used by parents and identify their association with the dietary intake and weight status of their child.
Design and methods
A cross-sectional study was carried out and parent–child respondents were enrolled from two private schools in Kathmandu Valley, Nepal. One of either parent was eligible to be included in our study if they had a child aged 3–6 years of age and played a significant role in feeding their children. In terms of children, those who did not have any chronic medical problems, were living with biological parents, and were non-vegetarian were included in the study. Our study was approved by the Institutional Review Committee of Kathmandu Medical College (Ref: 30122016), Kathmandu University, Nepal. Written informed consent was taken from respondents prior to data collection.
Questionnaire
The questionnaire used in this study included questions about sociodemographic variables and anthropometric measurements of the parent and child, the parental perception of the child’s activity, child feeding practices, and dietary intake of the children. The sociodemographic variables included educational level of parents (dichotomized as <class 12/high school=less than higher secondary level and ≥class 12/high school=higher secondary and above), occupation (employed=services, business and agriculture, unemployed=homemaker), relationship of parent with child, type of family in which child lived, age of parent, age and sex of child, and the class in which the child studied. Ethnicities of parents were organized into a privileged group (including upper caste and relatively advantaged Janajatis) and an underprivileged group (including Dalits, disadvantaged Janajatis, disadvantaged non-Dalit Terai people, and religious minorities) on the basis of people’s access to education, health, and socioeconomic representation in Nepal. The anthropometric measurements included the height and weight of children and parents. To measure the parental perception of physical activity of the child, a separate section of the questionnaire with questions related to the general activity level of the child before breakfast, in the morning, in the early afternoon, in the late afternoon, and after dinner was used. For this, parents had to tick on a 5-point Likert scale which was numbered as (1) “not at all active”, (2) “slightly active”, (3) “moderately active”, (4) “very active”, and (5) “highly active”. The information related to child feeding practices was assessed by the Child Feeding Questionnaire (CFQ). This has seven domains: perceived feeding responsibility, perceived parent overweight, perceived child overweight, concern about child's overweight, restriction, the pressure to eat, and monitoring. Out of these seven domains, our study included five domains of the CFQ: perceived feeding responsibility, concern about child's overweight, restriction, the pressure to eat, and monitoring. The CFQ assesses parental feeding attitudes, beliefs, and practices concerned with child feeding and obesity proneness.19 The psychometric properties of the CFQ, its internal consistency, its test–retest reliability, and its construct validity have been rigorously assessed.20 A study carried out in Japan revealed that when translated into the native language, the CFQ is useful to assess child feeding practices and attitudes of parents of elementary schoolchildren.21 For the assessment of dietary intake at home, a table was created in the questionnaire with space to fill in information about the place, time, amount, type of food consumed as well as items used in preparation of that particular food to be fillled up by the parents. At school, the information about the food consumed was observed and recorded by the researchers in the same table. We performed forward and backward translation as well as pretesting of the questionnaire to ensure its validity. The outcome variables of our study were the child’s weight status and dietary energy intake. The child’s weight status was assessed using BMI Z-scores while dietary energy intake was obtained from 1 day of 24-h dietary recall. One-day 24-h dietary recall has been reported to be a valid measure of assessing dietary intake among young children.22
Data collection and statistical analysis
For the purpose of data collection, two private schools were chosen purposively during March–May 2017. Data was gathered from all children and parents, and necessary exclusions were made at the time of analysis. The schools were visited on prearranged dates by the researchers. Verbal informed consent to include children was taken from school heads and teachers while written informed consent was obtained from the parents to ensure their willingness to participate in the study. The children were weighed and their height was measured using a standard digital weighing scale (model: SECA 874) and a height machine (model: SECA 217) on the school premises, and the results were recorded on the questionnaire. Children’s height was measured in centimeters using a standard technique of measuring to the nearest 0.1 cm and weight was measured in kilograms. Parent’s height and weight were self-reported.
For measuring dietary intake at home, all parents were invited to the school premises and taught about approximating and recording the dietary intake of their children at home using the standardized plastic glass, bowl, and spoon provided to them by the researchers. Prior to distribution, researchers assessed the capacity of these utensils by measuring a few commonly cooked food items through the use of a food scale (XY-8006 digital gram scale). Parental reporting of their young child’s dietary intake has been validated by research studies.23 In addition to standardized utensils, photographs with pictorial illustrations of common Nepali food measuring techniques as referred to by Adhikari and Krantz24 were attached along with the questionnaire to ease meal portion estimation. Parents were also given instructions to fill out the rest of the questionnaire and a self-administered questionnaire was then provided to the parent for completion at home. For assessing dietary intake at school, the food given to children was weighed and approximated using the same standardized utensils prior to serving and the children were observed during meals to note any spillage or exchange that may occur between peers.
On the follow-up visits, the filled in questionnaires were collected from the children. Out of 215 distributed questionnaires, 29 children did not meet the inclusion criteria (as they did not live with their biological parents or were vegetarian), 20 respondents did not respond, and 28 of the returned questionnaire were incomplete. Hence, only 138 of the completed questionnaires were used in the final analysis. Data were edited, coded, and entered into MS Excel and analyzed using SPSS 16 software. Descriptive and inferential statistics were used for analyzing data. Mann–Whitney U-test, Kruskal–Wallis H-test, Spearman rank correlation, and multiple regression analysis were carried out. The parental perception of child’s activity level was categorized into three groups as inactive (an average score <3.0), moderately active (an average score ≥3.0 and <4.0), and highly active (an average score ≥4.0).8 For the analysis of scores obtained in each domain of the CFQ, the mean number of items included in the domain was calculated for each parent respondent. This was done following the instructions given by CFQ developers from The Pennsylvania State University.25
To describe the child’s weight status, BMI age percentiles of 2–5 years and 5–19 years were used where overweight meant BMI percentile 85–94.9 and obesity meant ≥95th percentile. Similarly, for classifying the parent’s weight status, BMI≥25 was defined as overweight and BMI≥30 as obese. The BMI of parents was calculated using weight/height in meters squared.26,27 To test the association between variables, BMI Z-scores were used as a measure of weight status while dietary consumption was expressed in kilocalories. The BMI Z-scores describe the weight status of a particular child at a certain age and sex, and can be obtained using WHO Anthro Plus software. Anthro Plus is a software program devised by the WHO and used for nutrition surveys among children 2–19 years of age. A cutoff value of <−2 and ≥+2 Z-scores is used to identify undernutrition and overweight respectively.28 The calorie calculation was done using the common Nepali approximations listed by Adhikari and Krantz,24 and dietary intake was assessed on a single day.
Results
Characteristics of respondents
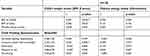
This study included 138 parent–children dyads; the sociodemographic characteristics of parents and children are presented in Table 1. More than half of the respondents were mothers and the majority of them were employed. About 54% lived in a joint family and almost all belonged to a privileged ethnic group. The majority of parents (83.3%) obtained higher educational degrees and earned about 280 USD (30,000 NPR) per month on average. Approximately an equal number of boys and girls were included and they were mostly perceived as being active by their parents. The majority of children watched television for ≤2 h.
 | Table 1 Sociodemographic characteristics of the respondents |
Parental BMI and child’s weight status
In the study, 2.9% of the children were underweight, 81.1% were of normal weight, 8% were overweight, while the remaining 8% were obese. The mean maternal BMI was found to be 23.91±3.24 while 31.2% of mothers were overweight and 4.3% were obese. Similarly, the mean BMI of the fathers was 24.62±2.68 while 37% of them were overweight and 2.9% were obese.
No significant association was found between child’s sex, parent’s age, relationship with child, employment status, ethnicity, level of education, and child’s weight status. Family type and parental perception of child’s activity, however, showed significant association with weight status (p=0.041 and p=0.004 respectively) (Table 2).
 | Table 2 Association of variables with child’s weight status and energy intake |
Table 3 shows that the BMI of parents had a positive, weak but significant correlation with the weight status of the child (r=0.307, p≤0.001 for mothers and r=0.206, p=0.016 for fathers). Monthly family income, however, had no correlation with child’s weight status. BMI of parents and family income had no statistically significant association with the dietary intake of the child. In regard to CFQ variables, only concern about a child being overweight had a weak, positive, and significant correlation with the child’s weight status (r=0.232, p=0.006).
 | Table 3 Correlation of variables with child’s weight status and energy intake |
The significantly correlated variables were assessed for their strength of association with the dependent variable using multiple regression analysis. The overall obtained equation was statistically significant:

Figure 1 shows that about 18% (R2=0.187) of the variance in the child’s weight status (displayed as BMI Z-scores) is accounted for by the three independent variables (BMI of father, BMI of mother, and concern about child’s overweight) depicted in the multiple linear equation model.
 | Figure 1 Multiple linear regression scatter plot. |
Discussion
Our study found that 8% of children were overweight while another 8% were obese. This finding is comparable to the findings of a study carried out in the USA where obesity among preschool children was found to be 8.9%.9 Another study carried out among urban school children in southern India showed that obesity is 7.5% and overweight is 21.9%.29 To the researcher’s best knowledge, no study has been carried out in Nepal to assess overweight/obesity among preschool children. However, two studies carried out in Lalitpur, Nepal among schoolgoing and adolescent students revealed that childhood overweight is 12–14%.16,17 These findings suggest that overweight and obesity among young children included in our study is comparable to the international trend.
In our study, the type of family of the child was significantly associated with the child’s weight status as children belonging to a joint family had higher BMI Z-scores. This finding is not in agreement with a study done elsewhere17 and the difference may be because of random fluctuations. Our study showed that the parental perception of activity of the child is associated with their weight status as highly active children had lower BMI Z-scores when compared to moderately active and inactive children. The finding is further supported by the findings of various other studies in which over-involvement in sedentary activities was found to be associated with childhood overweight and obesity.17,30 In our study, the BMI of both fathers and mothers was found to be positively correlated with the weight status of the child, which is supported by the results of studies done elsewhere.10,31 These findings infer that parents who have high BMI tend to have children with higher weight status which could be due to either genetic makeup or the dietary trend present in the family. Our study showed that the CFQ subscale, perceived feeding responsibility is not associated with weight status of the child, which is in contrast to the findings from a study where higher weight status of the child was associated with lower feeding responsibility.32 In our study, the CFQ variable concern about child’s overweight was found positively correlated with the weight status of the child, suggesting that parents who were concerned about their child’s overweight had children with higher weight status. The relationship may be vice versa; that is, the children who are already overweight may have parents who show more concern in their eating. The finding is further supported by other studies where parental concern was reported to be associated with the child’s weight status.32,33 In our study, the CFQ subscales restriction, pressure to eat, and monitoring were not found to be significantly associated with the weight status of the child and a similar finding has been reported in other studies worldwide.34–36 These findings suggest that the weight status of a child may not be determined by parental feeding practices like constantly monitoring or restricting a child from eating energy-dense food. Furthermore, pressurizing a child to eat everything that has been given is not associated with the child’s weight status. There could be other factors like genetic makeup, familial dietary habits, and so on which affect a child’s weight.
Dietary intake
Our study showed that parental BMI is not associated with the dietary consumption of a child, which is not in agreement with the results of studies carried out in Germany and the USA where the parent’s BMI was found to be an important correlate of a child’s intake.37,38 The difference in findings may be because in our study 24-h dietary consumption was assessed for only one weekday whereas the compared two studies used a food frequency questionnaire and obtained two or three 24-h recalls. It could also be because of the differences in eating culture and food values between these countries. In our study, the CFQ variables perceived feeding responsibility, concern about child’s overweight, and monitoring were not found significantly associated with dietary intake. Furthermore, the CFQ variables restriction and pressure to eat also showed no significant association with the dietary intake of the child. However, another study has shown that maternal feeding practices like control and pressure have a significant impact on the child’s food intake.39 This disagreement of the findings may be because in this study all of the children, irrespective of their obesity risk, were included while the compared study was done only among children with an obesity risk.
Programmatic implications, strengths, and limitations
Our study findings give a realization that overweight/obesity could be a public health threat in the near future even in Nepal. To the researchers’ best knowledge, this is the first study to assess the child feeding practices used by parents on childhood overweight in young children of Nepal. However, the study included only two purposively selected private schools which limits the generalizability of findings. The study findings are based on self-reporting by the parents and such findings are likely to suffer from over-reporting or under-reporting and recall bias. Since the study is of a cross-sectional nature, inferences about causation cannot be drawn. It was not feasible to obtain multiple-pass 24-h dietary recalls, which gives a narrow insight into the dietary consumption of the children. The CFQ, although valuable, does not measure every possible aspect of a feeding style that might influence the child’s dietary intake and weight status.
Conclusion and recommendation
The study concludes that parental BMI and parental concern are significant predictors of a child’s weight status. It is recommended that longitudinal studies to assess how the dietary consumption and weight status of the children change with time should be carried out and studies assessing the status of the double burden of diseases (childhood overweight and infectious diseases) among children should be carried out.
Acknowledgments
The authors would like to thank the University Grants Commission for providing funds for the study. The authors thank Dr Leann L. Birch for helping us acquire the standard tool for the study. The authors also thank Dr Bidur Gyawali, Ms Meena Gautam, and Ms Santoshi Gautam for their help in tool translation. The authors are grateful to Dr Naresh Manandhar for statistical help and the selected schools of Kathmandu Valley for their support in data collection.
Disclosure
SP, SR, AS, NP and SG receievd grants from the University Grants Commission of Nepal. The authors report no other conflicts of interest in this work.
References
1. Scaglioni S, Arrizza C, Vecchi F, Tedeschi S. Determinants of children’s eating behavior. Am J Clin Nutr. 2011;94:2006S–2011S.
2. Savage JS, Fisher JO. Parental influence on eating behavior: conception to adolescence. J Law Med Ethics. 2007;35:22–34. doi:10.1111/j.1748-720X.2007.00111.x
3. Benjamin SE, Cradock A, Walker EM, Slining M, Gillman MW. Obesity prevention in childcare: A review of US state regulations. BMC Public Health. 2008;8. doi:10.1186/1471-2458-8-188
4. Anzman SL, Birch LL. Parental influence on children’s early eating environments and obesity risk: implications for prevention. Int J Obes. 2010;34:1116–1124. doi:10.1038/ijo.2010.43
5. Clark HR, Goyder E, Bissell P, Blank L, Peters J. How do parents’ child-feeding behaviours influence child weight? Implications for childhood obesity policy. J Public Health (Bangkok). 2007;29:132–141. doi:10.1093/pubmed/fdm012
6. Johnson SL, Birch LL. Parents’ and children’s adiposity and eating style. Pediatrics. 1994;94:653–661.
7. Faith MS, Scanlon KS, Birch LL, Francis LA, Sherry B. Parent-child feeding strategies and their relationships to child eating and weight status. Obes Res. 2004;12:1711–1722. doi:10.1038/oby.2004.212
8. Zecevic CA, Michel L. Parental influence on young children’s physical activity. Int J Pediatr. 2010;2010.
9. Ogden CL, Fryar CD, Flegal KM;
10.
11. Pant S, Vaidya A. Over-nutrition in children and influence of parental attributes. J Kathmandu Med Coll. 2018;7:102–109. doi:10.3126/jkmc.v7i3.22679
12.
13.
14. Sah VK, Giri A, Acharya R. Prevalence of overweight, obesity and its associated risk factors among school children aged 6–16 years of Biratnagar. J Nobel Med Coll. 2016;5:22–25. doi:10.3126/jonmc.v5i2.16311
15. Shakya T, Shakya N, Sharma S. Overweight and obesity among early adolescents from government and Private Schools of Dharan, Nepal: a comparativestudy. Eur J Pharm Med Res. 2017;4:315–319.
16. Koirala M, Khatri RB, Khanal V, Amatya A. Prevalence and factors associated with childhood overweight/obesity of private school children in Nepal. Obes Res Clin Pr. 2015;9:220–227. doi:10.1016/j.orcp.2014.10.219
17. Piryani S, Baral KP, Poudyal AK, Piryani RM. Overweight and its associated risk factors among urban school adolescents in Nepal: a cross-sectional study. BMJ Open. 2016;6. doi:10.1136/bmjopen-2015-010335
18. Sahoo, K, Sahoo B, Choudhury AK, et al. Childhood obesity: causes and consequences. J Fam Med Prim Care. Kathmandu, Nepal: 2015;4:187–192.
19. Nowicka P, Sorjonen K, Pietrobelli A, Flodmark CE, Faith MS. Parental feeding practices and associations with child weight status. Swedish validation of the Child Feeding Questionnaire finds parents of 4-year-olds less restrictive. Appetite. 2014;81:232–241. doi:10.1016/j.appet.2014.06.027
20. De Lauzon-Guillain B, Oliveira A, Charles MA, et al. A review of methods to assess parental feeding practices and preschool children’s eating behavior: the need for further development of tools. J Acad Nutr Diet. 2012;112:1578–1602. doi:10.1016/j.jand.2012.06.356
21. Geng G, Zhu Z, Suzuki K, et al. Confirmatory factor analysis of the Child Feeding Questionnaire (CFQ) in Japanese elementary school children. Appetite. 2009;52:8–14. doi:10.1016/j.appet.2008.06.015
22. Wright J, Beaton E, Do L, Scott J, Devenish G. Relative validity of a 24-h recall in assessing intake of key nutrients in a cohort of Australian toddlers. Nutrients. 2018;10:80. doi:10.3390/nu10010080
23. Wallace A, Kirkpatrick SI, Darlington G, Haines J. Accuracy of parental reporting of preschoolers’ dietary intake using an online self-administered 24-h recall. Nutrients. 2018;10:987. doi:10.3390/nu10080987
24. Adhikari RK, Krantz ME. Child Nutrition and Health. Kathmandu, Nepal: Educational Publishing House; 2013.
25. Birch LL, Fisher JO, Grimm-Thomas K, Markey CN, Sawyer R, Johnson SL. Confirmatory factor analysis of the Child Feeding Questionnaire: a measure of parental attitudes,beliefs and practices about child feeding and obesity proneness. Appetite. 2001;36:201–210. doi:10.1006/appe.2001.0398
26.
27. Wang Y, Chen HJ. Use of percentiles and Z -scores in anthropometry. In: Handbook of Anthropometry: Physical Measures of Human Form in Health and Disease; 2012:29–48. doi:10.1007/978-1-4419-1788-1_2
28.
29. Cherian AT, Cherian SS, Subbiah S. Prevalence of obesity and overweight in urban school children in Kerala, India. Indian Pediatr. 2012;9:475–477.
30. Hills AP, Andersen LB, Byrne NM. Physical activity and obesity in children. Br J Sport Med. 2011;45:866–870. doi:10.1136/bjsports-2011-090199
31. Raut, BK, Jha MK, Baidya D, et al. Determination of risk factors associated with childhood obesity and the correlation with adult obesity- A random cross sectional study from Nepal. Am J Heal Res. 2014;2:134–139. doi:10.11648/j.ajhr.20140204.15
32. Karp SM, Barry KM, Gesell SB, Po’e EK, Dietrich MS, Barkin SL. Parental feeding patterns and child weight status for Latino preschoolers. Obes Res Clin Pract. 2014;8:e88–e97. doi:10.1016/j.orcp.2012.08.193
33. Montgomery C, Jackson DM, Kelly LA, Reilly JJ. Parental feeding style,energy intake and weight status in young Scottish children. Br J Nutr. 2006;96:1149–1153. doi:10.1017/BJN20061968
34. Watterworth JC, Hutchinson JM, Buchholz AC, et al. Food parenting practices and their association with child nutrition risk status: comparing mothers and fathers. Appl Physiol Nutr Metab. 2017;42:667–671. doi:10.1139/apnm-2016-0572
35. Webber L, Hill C, Cooke L, Carnell S, Wardle J. Associations between child weight and maternal feeding styles are mediated by maternal perceptions and concerns. Eur J Clin Nutr. 2010;64:259–265. doi:10.1038/ejcn.2009.146
36. Huang SH, Parks EP, Kumanyika SK, et al. Child-feeding practices among Chinese -American and non-hispanic white caregivers. Appetite. 2012;58:922–927. doi:10.1016/j.appet.2012.02.008
37. Pei Z, Flexeder C, Fuertes E, et al. Mother’s body mass index and food intake in school-aged children: results of the GINIplus and the LISAplus studies. Eur J Clin Nutr. 2014;68:898–906. doi:10.1038/ejcn.2014.92
38. Robson SM, Couch SC, Peugh JL, et al. Parent diet quality and energy intake are related to child diet quality and energy intake. J Acad Nutr Diet. 2016;116:984–990. doi:10.1016/j.jand.2016.02.011
39. Kröller K, Warschburger P. Associations between maternal feeding style and food intake of children with a higher risk for overweight. Appetite. 2008;51:166–172. doi:10.1016/j.appet.2008.01.012
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
