Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 12
Painful tumors of the skin: “CALM HOG FLED PEN AND GETS BACK”
Authors Cohen PR, Erickson CP, Calame A
Received 18 November 2018
Accepted for publication 20 January 2019
Published 13 February 2019 Volume 2019:12 Pages 123—132
DOI https://doi.org/10.2147/CCID.S193359
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Jeffrey Weinberg
Philip R Cohen,1 Christopher P Erickson,2 Antoanella Calame2
1San Diego Family Dermatology, National City, CA, USA; 2Compass Dermatopathology, San Diego, CA, USA
Abstract: Painful tumors of the skin present as dermal or subcutaneous nodules. They can originate from several sources: adipose tissue, cartilage degeneration, deposition of bone or calcium, eccrine glands, fibrous tissue, infiltration of benign (endometrium) or malignant (metastatic neoplasm) tissue, muscle, nerve, or vascular structures. Although pathologic evaluation of the lesion is necessary to determine the diagnosis, it is possible to make a reasonable differential diagnosis based on knowledge of prior tumors that have appeared as tender lesions. Two women with painful skin tumors – either osteoma cutis or an organizing thrombus – are described. Based on our clinical experience and review of the literature, 25 painful skin tumors were identified: chondrodermatitis nodularis helicis, angioendotheliomatosis, leiomyoma, metastases, hidradenoma, osteoma cutis, glomus tumor, fibromyxoma, leiomyosarcoma, eccrine angiomatous hamartoma, Dercum’s disease, peizogenic pedal papule, neurilemmoma, angiolipoma, neuroma, dermatofibroma, granular cell tumor, endometriosis, thrombus, scar, blue rubber bleb nevus, angioma, calcinosis cutis, and keloid. An acronym – inspired by Charlotte’s Web, a book that many children have read – that can be used as a memory aid for recalling the list of painful skin tumors is introduced: “CALM HOG FLED PEN AND GETS BACK”.
Keywords: cutis, osteoma, painful, skin, thrombus, tumor
Corrigendum has been published for this paper.
Introduction
Painful tumors of the skin present as dermal or subcutaneous nodules. Pathologic evaluation is necessary to determine the diagnosis of the tender lesion. However, when presented with a painful skin nodule, it is possible to make a reasonable differential diagnosis. Many of the potential diagnoses are always painful, whereas some of the tumors can also present as asymptomatic dermal masses.
“GLENDA” and “ENGLAND” were the acronyms initially used to recall the first letter of each of these painful skin tumors: eccrine spiradenoma, neurilemma, glomus tumor, leiomyoma, angiolipoma, neuroma, and dermatofibroma.1,2 In 1993, a 19-year-old woman presented with a tender subcutaneous nodule on her right chest; a biopsy of the lesion demonstrated a granular cell tumor.1 This observation prompted Naversen et al to create a new acronym for painful tumors of the skin, which not only included the granular cell tumor, but also endometrioma: “LEND AN EGG”.1
Naversen et al’s acronym for painful tumors of the skin has persisted for nearly a quarter of a century. However, another group of dermatologists described a 31-year-old man with painful acquired tufted angiomas on his chest.3 In 2018, one of the researchers from this group, with new collaborators, modified Naversen et al’s acronym to include both blue rubber bleb nevus and tufted angioma: “BLEND TAN EGG”.2
We have recently treated two patients who had painful nodules that were not a “BLEND TAN EGG” lesion; their lesions were osteoma cutis and an organizing thrombus. This prompted us to use the PubMed search engine to access the MEDLINE database of references for the terms “painful tumors and skin”; combined with our clinical experience, 25 painful skin tumors were discovered.1–19 The acronym we suggest using to recall these painful tumors of the skin is “CALM HOG FLED PEN AND GETS BACK”.
Discussion
Acronym
An acronym is a word, or series of words, formed from the initial letters of other words. In medicine, acronyms can be used as a memory aid for recalling a list of terms related to a specific condition. An acronym that the person can associate with a prior experience is easier to remember.
Charlotte’s Web
Charlotte’s Web is a book that many children have read.20 The protagonist, Wilbur, is a pig whose life is spared when a barn spider, Charlotte, weaves praises of him into her web. In chapter 3, titled “Escape”, the calm Wilbur fled his pen only to get back when he is induced by a pail of slop. Therefore, since many physicians may have fond memories of reading Charlotte’s Web, we propose that the acronym “CALM HOG FLED PEN AND GETS BACK” be used to recall the list of painful skin tumors (Table 1).1–19
  | Table 1 Acronym for painful tumors of the skin: CALM HOG FLED PEN AND GETS BACK |
Painful tumors of the skin
Painful tumors of the skin can be classified by origin (Table 2).1–19 They can develop from adnexal structures in the dermis (such as eccrine glands, fibrous tissue, muscle, nerves, and blood vessels). They can also result from the subcutaneous fat or the tissue of other organs infiltrating into the skin. In addition, they can arise from the deposition of bone or calcium into the skin. Finally, some tumors occur secondary to the degeneration of cartilage. Some of the features of the painful skin tumors are summarized below.
  | Table 2 Painful tumors of the skin |
Adipose
Angiolipoma, Dercum’s disease (also known as adiposis dolorosa), and piezogenic pedal papule are adipose tissue–associated tumors that can be painful.1,2,4,5
Angiolipoma
Angiolipoma is a variant of lipoma, which is composed of mature fat lobules. In addition, there are varying numbers of blood vessels. Fibrin thrombi of the capillaries near the tumor’s capsule may cause the tumor-related pain.1,2
Dercum’s disease
The diagnostic criteria for Dercum’s disease include the patient being obese or generally overweight and chronic painful adipose tissue of >3 months duration. A recent classification – based on clinical presentation – includes four subtypes: generalized diffuse form (with diffusely widespread painful adipose tissue without lipomas), generalized nodular form (with general pain in the adipose tissue and intense pain in and around multiple lipomas), localized nodular form (with pain in and around multiple lipomas), and juxta-articular form (with solitary deposits of excess painful fat around joints). The pathogenesis for the associated pain remains to be determined; however, proposed etiologies include adipose tissue dysfunction, mechanical pressure on nerves, nervous system dysfunction, and trauma.4
Piezogenic pedal papule
Piezogenic pedal papule is most commonly observed in women older than 40 years. Its etiology may be related to collagen defects (in patients with Ehler–Danlos syndrome), hereditary factors, repeated pressure (in susceptible individuals), and vigorous physical activity. The papule forms by fusion of smaller fat lobules as the separating trabeculae degenerate. Subsequently, the subcutaneous fat herniates into the dermis. The lesion is often asymptomatic; however, the papule may become painful secondary to the ischemia caused by the extrusion of the fat with its associated vessels and nerves.5
Cartilage
Chondrodermatitis nodularis helicis
Chondrodermatitis nodularis helicis, also referred to as chondrodermatitis nodularis chronica helicis, is a painful nodule on the helix or antihelix of the external ear; it is fixed to the cartilage and develops a crust-filled central crater. The most common etiologic factor is pressure necrosis to the site with subsequent ischemia to the dermis, which results in degenerative changes of the cartilage and its overlying skin; several other etiologic factors in the pathogenesis of this condition have also been proposed: age, ear anatomy, genetics, glomus-like vascular changes, perforating dermatoses and transepidermal elimination, systemic associations (with autoimmune or connective tissue disorders), and trauma. Often, the lesions are biopsied to exclude squamous cell carcinoma; therapeutic interventions can include intralesional corticosteroid injections or surgical excision.6
Deposition
Deposits of calcium or bone in the dermis can result in painful skin lesions.7,8
Calcinosis cutis
Calcinosis cutis, the deposition of calcium in the skin, can be either dystrophic (secondary to tissue damage and often associated with either autoimmune diseases, skin neoplasms, collagen or elastic fiber diseases, infections, or trauma), iatrogenic (secondary to venipuncture sites or extravasation of intravenous calcium-containing solutions), idiopathic (such as tumoral calcinosis, calcified subepidermal nodules, and scrotal calcinosis, each of which occurs in the setting of no previous damage to the skin or metabolic disturbances), and metastatic (resulting from calcium precipitation in the skin secondary to chronic kidney failure, hyperparathyroidism, hypervitaminosis D, milk-alkali syndrome, malignant neoplasms, and sarcoidosis). In addition, calcinosis cutis may include calciphylaxis which may occur in patients with chronic kidney failure who develop calcification of the small vessel walls in the dermis and subcutaneous fat. Although most lesions of calcinosis cutis are asymptomatic, some lesions are tender to palpation; in addition, ulceration of the overlying skin can result in pain and infection.7
Osteoma cutis
Osteoma cutis, also referred to as cutaneous ossification, is characterized by the formation of bone in the skin; it is either primary (when it appears without any prior inflammatory skin lesion, injury, or tumor) or secondary (when there was a previous lesion at the site). The subtypes of primary osteoma cutis include congenital plate-like osteoma, isolated osteoma, multiple military osteoma of the face, widespread osteoma, and osteoma cutis occurring as an associated feature of syndromes with metabolic dysfunction: Albright’s hereditary osteodystrophy, fibrodysplasia of progressive ossification, and osseous progressive heteroplasia.
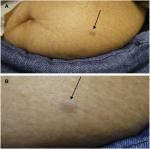
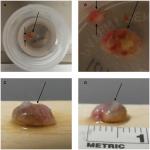
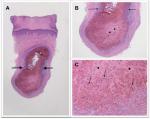
An isolated osteoma cutis typically presents as a painful dermal or subcutaneous nodule. Similar to the presentation of a solitary tender skin lesion of 4 years duration on the left lower abdomen of our patient as shown in Figures 1–3, an isolated osteoma cutis also presented as a painful lesion in a 30-year-old man; however, his lesion was only of 1-year duration and it was located on his palm.8
Eccrine
Painful dermal tumors have been observed, being neoplasms of eccrine gland origin such as angiomatous hamartoma, spiradenoma, and hidradenoma; to the best of our knowledge, a patient with a tender apocrine gland tumor has not been described.1,2,9,10
Eccrine angiomatous hamartoma
Eccrine angiomatous hamartoma is characterized by a proliferation of eccrine secretory coils and ducts; in addition, this proliferation is associated with capillary angiomatosis and occasionally, fat lobules and hair. It usually occurs as a solitary asymptomatic lesion on the extremities either at birth or in children prior to puberty. However, it can present either with multiple lesions, or in adults, and/or with associated hyperhidrosis (from angioma-related local increases in the temperature that produces the sweating) and pain (from the infiltration of small nerves).9
Eccrine spiradenoma
Eccrine spiradenoma usually presents as a painful dermal tumor. Its microscopic appearance is distinctive: “blue balls” in the dermis, since the tumor cells are deeply basophilic staining. Spiradenoma differentiates toward the intradermal eccrine ductal and secretory cells; there are two types of epithelial tumor cells arranged in intertwining cords: cells with small dark nuclei at the periphery of the cords and cells with large pale nuclei in the center of the cords. The intense pain is postulated to be caused by disorganized nerve fibers encasing the tumor nodules.1,2
Hidradenoma
Hidradenoma – also referred to as clear cell acrospiroma, clear cell hidradenoma, eccrine acrospiroma, nodular hidradenoma, and solid-cystic hidradenoma – is a benign tumor of eccrine origin. It typically presents as an asymptomatic nodule. However, an 81-year-old man was reported who presented with a 10-year history of a non-pruritic, bleeding, and painful 1 cm hyperpigmented, violaceous, shiny nodule on his right chest – with two superimposed serous nodules that would occasionally leak serous fluid. A deep-shave biopsy was performed and the diagnosis of nodular hidradenoma was established.10
Fibrous
Tumors of fibrous origin can also be painful. Dermatofibroma, keloid, and scar are common dermal tumors that may be tender. Digital fibromyxoma (superficial acral fibromyxoma) is an uncommonly described, yet distinctive tumor of the hands and feet – usually the distal digits – which often presents as a painful mass.1,2,11–13
Dermatofibroma
Dermatofibroma is the most common painful tumor of the skin. It typically presents as a hyperpigmented dermal papule or nodule; a “dimple sign” – demonstrated by a depression of the lesion and surrounding skin – can be noted by pinching the adjacent skin between the observer’s thumb and index finger. A proposed etiology for the pain may be secondary to entrapment of the collagen bundles in between the interlacing strands of fibroblasts or histiocytes.1,2
Digital fibromyxoma
Digital fibromyxoma, also referred to as superficial acral fibromyxoma, is a unique benign soft tissue tumor that has a predilection for the periungual and subungual areas of the hands and feet. In a study of 124 cases, the presenting symptoms were provided for 46 of the patients: the tumor presented as a painful mass in 39% of these individuals. Other presenting symptoms included nail deformity (9%), bleeding (9%), and infection (2%); however, the lesion was asymptomatic in 39% of the patients.11
Microscopic examination of a digital fibroxanthoma showed predominantly CD34-positive spindle-shaped, ovoid, or stellate-shaped cells that contained pale eosinophilic cytoplasm and were arranged in a random or loosely fascicular growth pattern within alternating areas of fibrous and myxoid stroma. Complete surgical excision may be necessary for individuals with persistent pain and/or local deformity. In the study of 124 digital fibroxanthomas, ten (24%) of the tumors recurred following incomplete excision.11
Keloid
A keloid can be painful or pruritic or both. It often occurs at the site of trauma and typically extends beyond the location of the original injury and does not regress with time. It results from an overgrowth of collagen and is frequently found on the earlobes, chest, posterior neck, proximal extensor arms, shoulders, and upper back. Microscopically, it is characterized by thick bundles of collagen (“bundles of rope”) that are randomly organized to the overlying epidermis.12,13
Hypertrophic scar
A hypertrophic scar – similar to a keloid – is also caused by an overgrowth of fibrous tissue and may itch or be tender. It usually appears on anatomic areas of high tension, such as ankles, chest, knees, and shoulders; in addition, it may regress with time. However, in contrast to a keloid, it typically remains confined to the original borders of the injury and is characterized by well-organized, relatively thin collagen bundles that are arranged parallel to the overlying epidermis.12,13
Infiltration
Infiltration of the dermis by benign or malignant organ tissue can result in painful skin tumors.1,2,14
Cutaneous endometriosis
Cutaneous endometriosis – frequently located near the umbilicus or lower abdomen – is a benign condition that can occur spontaneously or following implantation of endometrial cells in a surgical scar. Hormonal stimulation of the endometrial tissue usually results in pain. In addition to pain, cutaneous endometriosis is also typically associated with bleeding; both symptoms worsen during menstruation.1,2
Cutaneous metastases
Cutaneous metastases from primary visceral tumors or other malignancies can present as painful tumors of the skin. In addition, either B-cell or T-cell cutaneous lymphoma can occasionally present with tender skin lesions. A 72-year-old man, with a medical history of metastatic lower esophageal adenocarcinoma to his ribs that had been treated with surgery, radiotherapy, and chemotherapy, presented with several exquisitely tender scalp nodules; biopsy established the diagnosis of metastatic esophageal cancer. Successful relief of his symptom was provided by the palliative excisions of the painful cutaneous metastases; although he also received additional chemotherapy, he died from his cancer approximately a year later. The authors also identified additional patients with painful cutaneous metastases that had previously been described; the primary malignancies included carcinoid tumor, chondrosarcoma, colon adenocarcinoma, and renal pelvis transitional cell carcinoma.14
Muscle
Benign and malignant muscle tumors can also present as painful skin lesions.1,2,15
Glomus tumor
A glomus tumor is related to the Sucquet–Hoyer canal, which is the arterial segment of the cutaneous glomus; electron microscopy has demonstrated that the tumor’s glomus cells are vascular smooth muscle cells. A glomus tumor is typically solitary, frequently occurs in the nail bed, and presents with a characteristic triad of symptoms: cold sensitivity, point tenderness on palpation, and severe pain. A subungual glomus tumor may appear as a nail plate deformity or as a nodule beneath an intact, blue-discolored, nail.1,2
Leiomyoma
Leiomyoma is a benign smooth muscle tumor that can be solitary (angioleiomyoma and genital leiomyoma) or multiple (piloleiomyoma). It can be derived from arrector pili muscle (piloleiomyoma) or the muscles of veins (angioleiomyoma), or dartos, vulvar, or mammillary muscle (genital leiomyoma). Although a genital leiomyoma is usually asymptomatic, both angioleiomyoma and piloleiomyoma can spontaneously be a painful skin tumor; in addition, contraction of the lesion and pain can be elicited if a cold stimulus is applied to the tumor.1,2
Cutaneous leiomyosarcoma
Cutaneous leiomyosarcoma – a rare malignant smooth muscle tumor – originates from the dermis (superficial tumors from arrector pili muscle) or the subcutaneous tissue. Cutaneous pilar leiomyosarcoma typically presents as a painful, firm, slowly growing, solitary lesion on the extremity. In contrast to subcutaneous leiomyosarcoma that tends to be high-grade neoplasm, cutaneous pilar leiomyosarcoma is usually low grade, grows slowly, and remains confined to the dermis.15
Neural
Granular cell tumor, neurilemmoma, and neuroma are three tumors of neural origin that can present as painful tumors of the skin.1,2
Granular cell tumor
A granular cell tumor presented as a painful and tender subcutaneous nodule of 1-year duration on the right chest of a 19-year-old woman. Although granular cell tumor occurs more commonly on the tongue, it can also present on the skin. Immunohistochemistry studies and electron microscopic findings support that the tumor originates from Schwann cells; hence, the neural differentiation may account for the tumor being painful.1,2
Neurilemmoma
Neurilemmoma, also known as schwannoma, is a nerve sheath tumor. It occurs along the course of peripheral nerves and presents as a firm, tender, flesh-colored to pale-pink lesion. Microscopic evaluation of a neurilemmoma shows characteristic Verocay bodies consisting of cellular areas (referred to as Antoni A areas) intermixed with myxoid areas (Antoni B areas).1,2
Neuroma
A neuroma is a painful dermal tumor. It includes not only a traumatic neuroma, but also Morton’s neuroma. Traumatic neuroma presents as a painful nodule at the site of a severed nerve; microscopic examination shows bundles of nerve fibers that may be surrounded by a capsule. Morton’s neuroma, also referred to as an intermetatarsal neuroma, is a reactive process that presents as a tender nodule on the sole of the foot, most commonly between the third and fourth metatarsal bones, secondary to irritation and/or compression of the plantar digital nerve; microscopic examination shows perineural fibrosis surrounding the affected nerve.1,2
Vascular
Several lesions of vascular origin can present as a painful skin tumor.2,3,16–19
Reactive angioendotheliomatosis
A 57-year-old woman presented with a 2-year history of an increasing number of painful erythematous to violaceous nodules and papules on her left arm, upper back, and abdomen. An excisional biopsy of one lesion revealed microvascular thrombosis with capillary wall proliferation. These findings were diagnosed as reactive angioendotheliomatosis.16
The woman’s medical history was significant for two deep venous thromboses and one pulmonary embolus prior to discovery of protein C deficiency and life-long warfarin anticoagulation. Additional workup revealed a left subclavian steal syndrome and an elevated anticardiolipin antibody IgG level. Her pain responded to 10 mg of amitryptiline each evening. All of her lesions spontaneously resolved within 3 months after she stopped her job as a computer supervisor which had required keyboard use all day.16
The authors who described this woman also noted similar clinical and histopathologic features of reactive angioendotheliomatosis have been reported in other patients with antiphospholipid syndrome.16
Tufted angioma
Tufted angioma is a rare, benign, vascular tumor that usually presents in childhood. Lesion onset typically occurs prior to 5 years of age, with 50% of tumors appearing during the first year of life. However, albeit uncommon, acquired tufted angiomas in adulthood have been described.2,3
Tufted angioma usually appears on the neck, shoulders, upper back, or trunk. It can be a solitary tumor or can present as multiple lesions. It is a slowly growing, red to purple, mottled patch and/or firm plaque; tumor papules and nodules may be superimposed. Characteristic features are observed microscopically: multiple discrete ovoid angiomatous lobules or “tufts” of tightly packed capillaries are present in a “cannonball pattern” in the dermis.2,3
Paroxysmal pain and/or tenderness to palpation are often associated with the lesion. In addition, tufted angioma may be accompanied by localized hyperhidrosis and hypertrichosis. Growth factors, such as IL-8, and inflammation have been hypothesized to be responsible for the pain.2,3
Blue rubber bleb nevus
Blue rubber bleb nevus syndrome is a rare sporadic condition characterized by multiple venous malformations that occur predominantly on the skin, subcutaneous tissue, and gastrointestinal tract. However, other organs can also be involved, such as the central nervous system, liver, and muscles. The most common systemic symptoms include gastrointestinal bleeding and secondary iron-deficiency anemia.2,17
The vascular lesion (nevus) presents as a deep blue, soft, compressible rubbery bleb. The bleb can be painful. In addition, hyperhidrosis of the lesion – possibly secondary to the proximity of the blebs to sweat glands – has been observed.2,17
Microscopic examination of the nevus shows cavernous venous dilatations. The vascular lesion is lined by a simple layer of endothelial cells. Contraction of the smooth muscle fibers that surround the venous malformation is suggested as the etiology of the lesion’s pain.2,17
Organizing thrombus
An organizing thrombus can present as an acutely painful skin tumor (Figures 4–6). Cutaneous organizing thrombus was originally described as “capillary aneurysm of the skin” by Epstein et al in 1956 and 1965. Clinically, the lesions mimicked the appearance of melanoma.18
Subsequently, in 1966, Weiner described three additional patients. One of the individuals, a 21-year-old man, presented with a lesion on his right lower back that “had become tender and more raised than usual” 1 week prior to examination. Microscopic examination demonstrated thrombus formation in the enormously dilated capillaries of the upper dermis.18
Similar lesions of the oral cavity (including the buccal commissure, buccal mucosa, lip, and tongue) have been described as thrombosed oral varices; the appearance of the mucosal lesions could be confused with that of an oral melanoma. For example, the microscopic examination of a firm, dark blue, asymptomatic nodule on the upper lip of a 61-year-old man showed partial organization of a thrombus; it occurred 2 months following trauma to his face.19
Similar to individuals with angiolipomas and reactive angioendotheliomatosis, we suspect that the rapid expansion of the vessel by the blood clot may result in the acute onset of pain observed in our patient by her organizing thrombus.
Conclusion
Painful tumors of the skin can originate from several sources: adipose tissue, cartilage degeneration, deposition of bone or calcium, eccrine glands, fibrous tissue, infiltration of benign (endometrium) or malignant (metastatic neoplasm) tissue, muscle, nerve, or vascular structures. The tumors present as dermal nodules; hence, diagnostic considerations of a reasonable differential can be based on knowledge of prior tumors that have appeared as tender lesions. Based on our clinical experience and review of the literature, 25 painful skin tumors were identified: chondrodermatitis nodularis helicis, angioendotheliomatosis, leiomyoma, metastases, hidradenoma, osteoma cutis, glomus tumor, fibromyxoma, leiomyosarcoma, eccrine angiomatous hamartoma, Dercum’s disease, peizogenic pedal papule, neurilemmoma, angiolipoma, neuroma, dermatofibroma, granular cell tumor, endometriosis, thrombus, scar, blue rubber bleb nevus, angioma, calcinosis cutis, and keloid. An acronym inspired by Charlotte’s Web – a story that many children have read – is introduced to serve as a memory aid for enabling the astute clinician to recall the painful tumors of the skin: CALM HOG FLED PEN AND GETS BACK.
Disclosure
The authors report no conflicts of interest in this work.
References
Naversen DN, Trask DM, Watson FH, Burket JM. Painful tumors of the skin: “LEND AN EGG”. J Am Acad Dermatol. 1993;28(2 Pt 2):298–300. | ||
Bhat MR, George AA, Jayaraman J. Painful tumors of the skin – from ENGLAND to LEND AN EGG to BLEND TAN EGG. Indian J Dermatol Venereol Leprol. Epub 2018 Oct 3. | ||
Kamath GH, Bhat RM, Kumar S. Tufted angioma. Int J Dermatol. 2005;44(12):1045–1047. | ||
Hansson E, Svensson H, Brorson H. Review of Dercum’s disease and proposal of diagnostic criteria, diagnostic methods, classification and management. Orphanet J Rare Dis. 2012;7(1):23. | ||
Böni R, Dummer R. Compression therapy in painful piezogenic pedal papules. Arch Dermatol. 1996;132(2):127–128. | ||
Salah H, Urso B, Khachemoune A. Review of the etiopathogenesis and management options of chondrodermatitis nodularis chronica helicis. Cureus. 2018;10(3):e2367. | ||
Jiménez-Gallo D, Ossorio-García L, Linares-Barrios M. Calcinosis cutis and calcifilaxis. Actas Dermosifiliogr. 2015;106(10):785–794. | ||
Sánchez MEG, Martínez MLM, Mena JLA, Martín LIO. Osteoma cutis: rare painful tumor in atypical location. An Bras Dermatol. 2017;92(5 Suppl 1):113–114. | ||
Naik V, Arsenovic N, Reed M. Eccrine angiomatous hamartoma: a rare multifocal variant with features suggesting trauma. Dermatol Online J. 2009;15(9):6. | ||
Tarantino I, Fraga G, Fischer R. A chronic, bleeding, and painful nodule on the chest. Dermatol Online J. 2016;22(9):13030/qt0g72b28m. | ||
Hollmann TJ, Bovée JV, Fletcher CD. Digital fibromyxoma (superficial acral fibromyxoma): a detailed characterization of 124 cases. Am J Surg Pathol. 2012;36(6):789–798. | ||
McCabe J, Blades Z, McGrath EE. A spontaneous skin lesion. CMAJ. 2008;179(12):1297–1299. | ||
Krakowski AC, Totri CR, Donelan MB, Shumaker PR. Scar management in the pediatric and adolescent populations. Pediatrics. 2016;137(2):e20142065. | ||
Stein RH, Spencer JM. Painful cutaneous metastases from esophageal carcinoma. Cutis. 2002;70(4):230–232. | ||
Cammisuli F, Catania V, Nasca MR, Failla A, Micali G. A painful nodule on the leg: a quiz. Diagnosis: low-grade cutaneous pilar leiomyosarcoma. Acta Derm Venereol. 2015;95(5):633–634. | ||
Kirke S, Angus B, Kesteven PJ, Calonje E, Simpson N. Localized reactive angioendotheliomatosis. Clin Exp Dermatol. 2007;32(1):45–47. | ||
Jin XL, Wang ZH, Xiao XB, Huang LS, Zhao XY. Blue rubber bleb nevus syndrome: a case report and literature review. World J Gastroenterol. 2014;20(45):17254–17259. | ||
Weiner MA. Capillary aneurysms of the skin. Arch Dermatol. 1966;93(6):670–673. | ||
Weathers DR, Fine RM. Thrombosed varix of oral cavity. Arch Dermatol. 1971;104(4):427–430. | ||
White EB. Charlotte’s Web. New York: Harper & Brothers; 1952. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.