Back to Journals » International Medical Case Reports Journal » Volume 14
Ovarian Torsion Due to Mature Cystic Teratoma During the Early Postpartum Period: A Rare Case Report
Authors Adam Osman A , Tahtabasi M, Gedi Ibrahim I , Issak Hussein A, Mohamud Abdullahi I
Received 8 March 2021
Accepted for publication 13 May 2021
Published 20 May 2021 Volume 2021:14 Pages 333—338
DOI https://doi.org/10.2147/IMCRJ.S310071
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ronald Prineas
Ahmed Adam Osman,1 Mehmet Tahtabasi,1 Ismail Gedi Ibrahim,1 Ahmed Issak Hussein,2 Ismail Mohamud Abdullahi3
1Department of Radiology, University of Health Sciences, Somalia Turkey Recep Tayyip Erdogan Education and Research Hospital, Mogadishu, Somalia; 2Department of Obstetrics and Gynecology, University of Health Sciences, Somalia Turkey Recep Tayyip Erdogan Education and Research Hospital, Mogadishu, Somalia; 3Department of Pathology, University of Health Sciences- Somalia Turkey Recep Tayyip Erdogan Education and Research Hospital, Mogadishu, Somalia
Correspondence: Mehmet Tahtabasi
Somalia Recep Tayyip Erdogan Education and Research Hospital, 30 Street, Black Sea, Hodan District, Mogadishu, Somalia
Tel +905076159932
Email [email protected]
Abstract: Mature cystic teratoma (MCT) is a benign and unilateral ovarian neoplasm usually seen in premenopausal women. Its most common complication, torsion, is a well-known cause of acute abdominal pain. However, it is rare in the early postpartum period. In this paper, we present a case of ovarian torsion due to MCT, which was diagnosed radiologically in the early postnatal period and surgically confirmed. A 25-year-old woman vaginally delivered a healthy baby on time and without any problems. She presented with acute abdominal pain in the right lower quadrant on the postpartum 5th day. Abdominal ultrasound (US) and computed tomography (CT) demonstrated an ovarian mass containing fat and calcification in the right adnexa and non-enhancing ovarian parenchyma. The patient was discharged on the 5th day after the salpingo-oophorectomy operation without any complications. US and CT provided crucial information to make an accurate and rapid management decision in ovarian torsion due to MCT.
Keywords: adnexal torsion, mature cystic teratoma, early postpartum, pregnancy, computed tomography
Introduction
Mature cystic ovarian teratomas (MCTs), also known as dermoid cysts, are one of the most common ovarian neoplasms found in women that are characterized by the presence of all three embryonic germ cell layers.1 Although MCTs are usually benign, 1% to 2% undergo malignant transformation. In addition, while habitually unilateral, 10% to 15% are bilateral. More importantly, 15% of these lesions may lead to the risk of ovarian torsion.1–3 Moreover, ovarian torsion considers about 3% of cases of acute abdominal discomfort that present at emergency departments.4 Although ovarian torsion during pregnancy or the postpartum period is often confused with other acute abdominal diseases, it should not be missed. A delay in the diagnosis of ovarian torsion can lead to irreversible ovarian necrosis. In this paper, we report a rare case of ovarian torsion with MCT during the early postpartum period that was diagnosed by radiological modalities and treated surgically.
Case Presentation
Patient’s Sociodemographic Characteristics
The patient was a 25-year-old female and had her first menstruation when she was 15 years old. She has four living children and the gravida was four.
Clinical Presentation and Imaging Findings
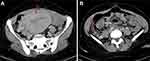
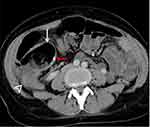
The patient presented to our emergency department with severe pain right lower quadrant of the abdomen and vomiting. She had a vaginal delivery at home five days ago. The patient did not receive antenatal care and ultrasound (US) was not performed. On physical examination, her temperature was 37.8° Celsius. She was in severe distress due to abdominal pain. Her abdomen was rebound tenderness, guarding, and moderately distended. Bowel sounds were present but hypoactive. At the time of admission, blood pressure was 116/72 mm Hg, heart rate was 110 beats/min, respiratory rate was 22 breaths/min. Laboratory investigations in emergency department showed that she had white cell count of 9.60 × 109/L and raised C-reactive protein of 34 g/dL. Bedside transabdominal US as the first imaging modality revealed well-defined hypoechoic lesion with internal echoes and posterior acoustic shadow in the right adnexa of the uterus, having no vascularity in color Doppler. Furthermore, there was also an echogenic mural nodule compatible with the Rokitansky nodule (dermoid plug) within the heterogeneous lesion (Figure 1). An abdominal contrast-enhanced computed tomography (CT) scan of the abdomen showed that the appendix is normal and the uterus increased in size (Figure 2). Furthermore, CT demonstrated a heterogeneous density lesion containing subtle peripheral calcification, fat and fluid density areas in the right adnexa consistent with a MCT (Figure 3).
Treatment, Outcome and Follow-Up
We performed a small transverse incision that allowed the externalization of the ovarian mass containing hair, sebum, and calcifications in the right adnexa (Figure 4). During the operation, dark, enlarged and nonviable ovarian tissue was detected. There was no cyst rupture. We then carried out a right total salpingo-oophorectomy. The uterus and contralateral adnexa were macroscopically normal. Surgical specimen and histopathological examination showed that unilocular cysts filled with sebaceous material, hair and focal solid area, extensive hemorrhage, congestion, dilated blood vessels, and ischemia of mucosa and parenchyma (Figure 5). The patient recovered well postoperatively and was discharged home five days after her operation pain-free. The abdominal US performed two weeks after discharge demonstrated no pathological finding in the right adnexa.
 |
Figure 4 Surgical specimens showing unilocular cysts filled with sebaceous material, hair, and focal solid area with calcification area. |
Discussion
Mature cystic teratoma is the most common benign ovarian neoplasm comprising 10–15% of all ovarian tumors. Although it occurs at all stages of life, the majority of cases being diagnosed between 20 and 30 years of age. Therefore, the most common tumor during pregnancy is MCT (22–40% of all ovarian tumors). The risk of complications including rupture, torsion, infection and malignant degeneration increases significantly during pregnancy.5 MCT is the most common ovarian mass associated with torsion, which is reported in 3–16% of patients with ovarian teratomas.2 Ovarian torsion occurs as a result of the twist of the suspensory ligament that connects the ovary and its vascular peduncle to the pelvic lateral wall. Torsion gradually results in ovarian parenchyma edema, ischemia, and eventually hemorrhagic infarction. Ovarian torsion is usually accompanied by an underlying ovarian mass such as physiological cysts, endometriomas, benign neoplasms (eg, cystadenoma, teratoma, or fibroma), and malignancies (primary or metastatic).6 The incidence of ovarian masses during pregnancy is approximately 1 in 100 to 2000 pregnancies. However, torsion occurs in only 3% of pregnant women with ovarian cysts. Treatment management in pregnant patients is still unclear and changes according to the characteristics of the lesion. In the literature, it is recommended to remove masses larger than 10 cm because of the risk of torsion and malignancy. Although the incidence of torsion decreases as the gestational age increases, it can also occur at any time of pregnancy or in the postpartum period.7 In this present case, torsion due to the mass occurred in the early postpartum period. This can be interpreted as vaginal delivery triggering ovarian torsion. However, the level of evidence should be increased with studies with large series.
Previous most studies show that clinical evaluation is insufficient in the diagnosis of ovarian torsion. In most cases, non-specific pelvic pain is accompanied by nausea, vomiting, low-grade fever, and moderate leukocytosis. The most common diagnoses that can be confused with this condition include acute appendicitis, renal colic, diverticulitis, pelvic inflammatory disease, and endometriosis. For this reason, imaging methods are often needed to make the appropriate treatment and to make a diagnosis.6–9
Various tumor markers have increased depending on the component tissues of ovarian germ cell tumors, including MCT. Elevated serum tumor marker levels may serve as an adjunct in initial diagnosis, therapy monitoring, and posttreatment surveillance.10 The important markers of germ cell tumors are serum alpha feto protein (AFP), human chorionic gonadotropin (hCG), and lactic dehydrogenase (LDH). AFP is present in 100% women with yolk sac tumor, 61.9% in immature teratoma, and 11.8% in dysgerminoma, but no positive case for AFP in mature cystic teratoma and mature cystic teratoma with malignant transformation is seen.11 Human chorionic gonadotropin is a glycoprotein produced by syncytiotrophoblasts and has been shown not to increase in MCTs. In addition, LDH usually rises in association with dysgerminoma.10,11 Furthermore, the importance of markers such as CA 19–9, CA-125, and CA15-3 in the diagnosis of MCT has been investigated. According to the study, high serum CA 19–9 levels were found to be associated with larger tumor size. However, the diagnostic value of high CA 19–9 has been reported to be poor if the test is used alone.12
In our present case, the patient had severe abdominal pain and vomiting accompanied by low-grade fever, mild tachypnea, and tachycardia. In addition, our patient had a history of vaginal delivery five days ago. In our case, serum markers AFP and LDH were found to be normal and others were not investigated. Gray-scale US revealed a heterogeneous mass with fat and calcifications in the right adnexa and showed compression of the ovarian parenchyma and absence of vascularity. Moreover, contrast-enhanced abdominal and pelvic CT confirmed the diagnosis of MCT by showing lesion content, enhancement pattern, and surrounding tissues.
For diagnosis of ovarian torsion, US, CT, and magnetic resonance imaging (MRI) are the imaging methods used.8 The US is the first preferred modality because of its advantages such as being available in many centers, being able to be performed at the bedside, and is not containing ionizing radiation. The sonographic appearance of ovarian torsion may vary depending on the duration of the torsion, the presence of the underlying mass, and the bleeding status. The most commonly reported finding in the literature is the enlarged ovary. In addition, peripherally aligned follicle cysts accompanied by pain are also stated as another finding of torsion. The presence of free pelvic fluid in the cul-de-sac is a finding seen in 87% of the cases. It has been suggested that this is a late finding and is generally associated with hemorrhagic ovarian tissue. Twisted vascular pedicle, visualization of circular or spiral vessels in color Doppler US is the classic whirlpool sign. Although this sign is specific to ovarian torsion, it has been reported variably, as seen in 13–88% of patients with ovarian torsion.8,9 In the presented case, the ovarian parenchyma was compressed due to MCT and the separation of the parenchyma from the mass could not be clearly made sonographically. Color Doppler US examination revealed the absence of vascularity in both the mass and the ovarian parenchyma. The classic whirlpool sign described in the literature was absent in this case. However, MRI is not considered as the first choice for cases with suspected torsion, but it can be useful as a problem solver in pregnant women that cannot be decided by the US or in suspected cases.8 CT findings of ovarian torsion include asymmetric ovarian enlargement similar to the US, multiple peripheral follicles in an asymmetrically enlarged ovary, decreased adnexal enhancement on the side of the torsion following administration of intravenous contrast, a twisted vascular pedicle, pelvic free fluid, inflammatory fat stranding adjacent to the ovary, and uterine deviation towards the side of torsion. In addition to the US, it can provide useful information to exclude other diseases in differential diagnosis and to evaluate the internal structure of the ovarian mass.8 In our present case, CT provided valuable information about the content and enhancement of the ovarian mass. Thus, the patient was urgently referred to the operating room and surgical treatment was performed.
The characteristic imaging feature of a MCT is a cystic adnexal mass with a distinct capsule containing sebaceous fluid that is most often unilocular (88%) but can be multilocular. MCTs characteristically contain components of fat (93%), calcifications (56%) such as bone or teeth, and often floating masses of hair or soft tissue.13 In this case, both US and CT demonstrated fat in the ovarian mass. Furthermore, the CT showed calcification at the periphery of the lesion. The excised surgical material revealed the necrotic ovarian tissue, hair, and fat tissue. In addition to all these, histopathological examination confirmed the diagnosis of MCT.
Conclusion
Ovarian torsion in the postpartum period is a rare but serious complication. It may be difficult to distinguish clinically from many pathologies such as acute appendicitis, pelvic inflammatory disease, and ovarian hemorrhage. Therefore, imaging methods play an important role in early diagnosis and treatment. In addition, this situation should be diagnosed immediately and appropriate imaging methods should be used in order to perform emergency surgery.
Abbreviations
MCT, mature cystic teratoma; US, ultrasound; CT, computed tomography; MRI, magnetic resonance imaging.
Ethical Approval
The patient was treated in accordance with the ethical standards of institutional and national committees on human experimentation and with the Declaration of Helsinki (1975, and subsequent revisions). According to the guidelines of the Ethics Committee of Somali Turkey Recep Tayyip Erdogan Hospital institutional approval was not required to publish the case details.
Informed Consent
The patient provided written informed consent for publication of the details of her case and the images shown in the figure.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The authors declare that this study has received no financial support.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Artunc Ulkumen B, Goker A, Pala HG, Ordu S. Abnormal elevated CA 19-9 in the dermoid cyst: a sign of the ovarian torsion? Case Rep Obstet Gynecol. 2013;2013:1–2. doi:10.1155/2013/860505
2. Fayez I, Khreisat B, Athamneh T, Omoosh R, Daibes MA. Multiple bilateral ovarian mature cystic teratomas with ovarian torsion: a case report. Oman Med J. 2018;33(2):163–166. doi:10.5001/omj.2018.30
3. Outwater EK, Siegelman ES, Hunt JL. Ovarian teratomas: tumor types and imaging characteristics. RadioGraphics. 2001;21(2):475–490. doi:10.1148/radiographics.21.2.g01mr09475
4. Lobo R, Gershenson D, Lentz G. Comprehensive Gynecology.
5. Maiti S, Fatima Z, Anjum Z, Hopkins R. Ruptured ovarian cystic teratoma in pregnancy with diffuse peritoneal reaction mimicking advanced ovarian malignancy: a case report. J Med Case Rep. 2008;2(1):203. doi:10.1186/1752-1947-2-203
6. Duigenan S, Oliva E, Lee SI. Ovarian torsion: diagnostic features on CT and MRI with pathologic correlation. Am J Roentgenol. 2012;198(2):W122–W131. doi:10.2214/AJR.10.7293
7. Tanaka Y, Koyama S, Shiki Y. Torsion of a normal ovary during the early postpartum period. CRSLS MIS Case Rep SLS. 2015;19(1). doi:10.4293/crsls.2013.00250
8. Lourenco AP, Swenson D, Tubbs RJ, Lazarus E. Ovarian and tubal torsion: imaging findings on US, CT, and MRI. Emerg Radiol. 2014;21(2):179–187. doi:10.1007/s10140-013-1163-3
9. Khalil RM, El-Dieb LR. Sonographic and MRI features of ovarian torsion. Egypt J Radiol Nucl Med. 2016;47(2):621–629. doi:10.1016/j.ejrnm.2016.02.004
10. Shaaban AM, Rezvani M, Elsayes KM, et al. Ovarian malignant germ cell tumors: cellular classification and clinical and imaging features. RadioGraphics. 2014;34(3):777–801. doi:10.1148/rg.343130067
11. Kawai M, Kano T, Kikkawa F, et al. Seven tumor markers in benign and malignant germ cell tumors of the ovary. Gynecol Oncol. 1992;45(3):248–253. doi:10.1016/0090-8258(92)90299-X
12. Emin U, Tayfun G, Cantekin I, Ozlem UB, Umit B, Leyla M. Tumor markers in mature cystic teratomas of the ovary. Arch Gynecol Obstet. 2009;279(2):145–147. doi:10.1007/s00404-008-0688-2
13. Bernot JM, Haeusler KA, Lisanti CJ, Brady RO, Ritchie BL. Mature cystic teratoma: AIRP best cases in radiologic-pathologic correlation. RadioGraphics. 2017;37(5):1401–1407. doi:10.1148/rg.2017170003
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.