Back to Journals » Clinical Interventions in Aging » Volume 9
Outcomes of trochanteric femoral fractures treated with proximal femoral nail: an analysis of 100 consecutive cases
Authors Korkmaz MF , Erdem MN, Disli Z, Selcuk EB, Karakaplan M, Gogus A
Received 28 December 2013
Accepted for publication 6 February 2014
Published 3 April 2014 Volume 2014:9 Pages 569—574
DOI https://doi.org/10.2147/CIA.S59835
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Mehmet Fatih Korkmaz,1 Mehmet Nuri Erdem,2 Zeliha Disli,3 Engin Burak Selcuk,4 Mustafa Karakaplan,1 Abdullah Gogus5
1Department of Orthopedics and Traumatology, Inonu University School of Medicine, Malatya, Turkey; 2Department of Orthopedics and Traumatology, Nisantasi University School of Medicine, Istanbul, Turkey; 3Department of Anesthesiology, Malatya Government Hospital, Malatya, Turkey; 4Department of Family Medicine, Inonu University School of Medicine, Malatya, Turkey; 5Department of Orthopedics and Traumatology, Florence Nightingale Hospital, Istanbul, Turkey
Purpose: In this study, we aimed to report the results of a retrospective study carried out at our institute regarding cases of patients who had suffered proximal femoral fractures between January 2002 and February 2007, and who were treated with a proximal femoral nail.
Materials and methods: One hundred consecutive cases were included in the study. A case documentation form was used to obtain intraoperative data including age, sex, mechanism of injury, type of fracture according to Association for Osteosynthesis/Association for the Study of Internal Fixation (AO/ASIF) classification and the American Society of Anesthesiologists' (ASA) physical status classification (ASA grade). Clinical and radiographic examinations were performed at the time of admission and at the 6th week; subsequent visits were organized on the 3rd month, 6th month, and 12th month, and in patients with longer follow-up and annually postoperatively. The Harris score of hip function was used, and any change in the position of the implants and the progress of the fracture union, which was determined radiologically, was noted.
Results: The mean age of the patients was 77.66 years (range: 37–98 years), and the sex distribution was 32 males and 68 females. Seventy-three fractures were reduced by closed means, whereas 27 needed limited open reduction. The mean follow-up time for the study group was 31.3 months (range: 12–75 months). Postoperative radiographs showed a near-anatomical fracture reduction in 78% of patients. The Harris hip score was negatively correlated with the ASA score and patient age. No cases of implant failure were observed. Three patients died before discharge (one due to pulmonary embolism, two due to cardiac arrest), and five patients died due to unrelated medical conditions within the first 3 months of the follow-up.
Conclusion: Our study showed that proximal femoral nail is a reliable fixation with good fracture union, and it is not associated with major complications in any type of trochanteric femoral fracture.
Keywords: ASA, femoral fracture, Harris score, proximal femoral nail
Introduction
The trochanteric femoral fracture is common in elderly patients; with societies growing continuously older, the incidence has increased markedly in recent years.1 Due to their poor bone quality, it is very difficult to achieve and maintain a stable fixation in elderly patients.2 The aim of surgery is to achieve early mobilization and the prompt return to prefracture activity levels. The treatment of this fracture remains a challenge to the surgeon.
Numerous variations of intramedullary nails have been devised to achieve a stable fixation and early mobilization of pertrochanteric fractures; among these, the proximal femoral nail (PFN), devised by the AO/ASIF group in 1996, has proven to be a promising implant in per-, inter-, or subtrochanteric femoral fractures.3 These intramedullary devices are more stable under loading with a shorter lever arm, so the distance between the hip joint and the nail is reduced compared with that for a plate, thus diminishing the deforming forces across the implant.4 Furthermore, these devices minimize soft-tissue dissection and thereby reduce surgical trauma, blood loss, infection, and wound complications.4
In this study, we aimed to report the results of a retrospective study carried out at our institute on 100 consecutive cases who had suffered proximal femoral fractures between January 2002 and February 2007, and who were treated with a PFN.
Materials and methods
Study design
This retrospective study was approved by the local Institutional Ethics Board in accordance with the standards of the Declaration of Helsinki, and informed written consent forms were obtained from all the participants. From January 2002–February 2007, we treated 100 consecutive cases of proximal femoral fractures with a PFN (Synthes GmbH, Oberdorf, Switzerland). A case documentation form was used to obtain intraoperative data, including age, sex, mechanism of injury, type of fracture according to AO/ASIF classification, and the American Society of Anesthesiologists (ASA) physical status classification (ASA grade).
All operations were performed by the same group of experienced surgeons. All patients were operated in the supine position under image intensifier control by either consultants or registrars using standard techniques and a protocol.3
Operative technique
Implantation of the PFN can be done with or without a fracture table. Using the fracture table, the hip should be placed in a slight adduction position to facilitate the insertion of the nail. About 5 cm cranial to the tip of the greater trochanter, the skin is incised for about 5 cm. After passing the fascia and muscles, a 2.8 mm threaded K-wire is inserted at the tip of the greater trochanter under C-arm control. The K-wire is advanced into the femoral shaft in such a way that it is located in the middle of the shaft in both directions. The proximal part of the femoral shaft is reamed manually with a 17 mm reamer. After mounting the nail on the radiolucent insertion device, the nail can be introduced manually into the femoral shaft. Via the aiming arm, which is attached to the insertion device, the guide wire for the neck screw is first introduced into the femoral neck in such a way that the screw will be placed into the lower half of the neck on the anteroposterior view and centrally on a lateral view. Thereafter, the guide wire for the antirotational hip pin is introduced. The hip pin is introduced first with the tip just about 25 mm medial to the fracture line; then, the neck screw is inserted. Afterwards, depending on the type of fracture, distal interlocking is either statically or dynamically achieved via the same aiming arm. In all cases antithrombotic prophylaxis was given using low molecular weight heparin (Fraxiparine®; GlaxoSmithKline, Brentford, UK), and antibiotic prophylaxis was provided (cefazolin). Anteroposterior and lateral radiographs were obtained 24–72 hours postoperatively, and analyzed for reduction and position of the implant.
The rehabilitation protocol was demonstrated, and the patients were mobilized on the first postoperative day. Partial weight bearing as tolerated or restricted weight bearing was allowed according to the surgeon’s recommendation on the day following surgery.
Outcome analysis
Clinical and radiographic examinations were performed at the time of admission and at the 6th week; subsequent visits were organized on the 3rd month, 6th month, and 12th month, and patients with longer follow-up and annually postoperatively (Figures 1A, B, 2A and B). Clinical evaluation was made using the Harris hip scoring system, which considers pain, walking capacity, and physical examination findings.5 Radiographic evaluations included union, calcification in the greater trochanter, cortical thickening at the distal locking site, cut-out of the helical screw in the femoral head, lateral migration of the helical screw (telescoping), and shortening of the femoral neck length.
  | Figure 1 Preoperative posteroanterior and lateral X-ray of an 82-year-old patient. |
  | Figure 2 Postoperative (12th month) posteroanterior and lateral X-ray of an 82-year-old patient. |
Statistical analysis
All of the data were processed by SPSS 14.0 software (SPSS Inc., IL, USA). Data were first tested for normality of distribution by the Shapiro–Wilk test. Differences in the continuous variables between the two groups were compared using Student’s t-test for normally distributed data, or the Wilcoxon rank-sum test for data not normally distributed. Fisher’s exact test was used for categorical variables, and the Kruskal–Wallis test was performed for ordinal variables. The differences were considered to be statistically significant when P≤0.05.
Results
The mean age of the patients was 77.66 years (range: 37–98 years) and the sex distribution was 32 males and 68 females. The preoperative variables are listed in Table 1. The mean time from injury to surgery was 1.83 days (range: 0–17 days).
  | Table 1 Preoperative data of the patients |
Eighty-five patients were operated on under combined general and epidural anesthesia – five under spinal and epidural anesthesia, eight under spinal anesthesia, and two under epidural anesthesia. Seventy-three fractures were reduced by closed means, whereas 27 needed limited open reduction. Intraoperative femoral fracture occurred in one patient and was managed with Dall–Miles wires. The mean duration of the operation was 87.9 minutes (range: 30–300 minutes). Active and passive exercises were initiated within 48 hours of the operation.
The mean duration of hospitalization was 13.34 days (range: 4–65 days). The mean follow-up for the study group was 31.3 months (range: 12–75 months). Postoperative radiographs showed a near-anatomical fracture reduction in 78% of patients.
Changes in the hip score in relation to the type of fractures, ASA score, and patient age were shown in Table 2. The data were analyzed to see whether there was an association between the Harris hip score (HHS) and fracture classification, ASA score, and age. The results revealed that HHS was negatively correlated with ASA score and patient’s age.
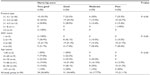  | Table 2 The relationship between fracture type, ASA score, patient age, and Harris hip score |
Of the patients, one had superficial infections, which were controlled with antibiotics. Hematomata of the surgical wound resolved satisfactorily in six patients; migration of the screws was not observed. In three patients, there was ectopic new bone formation at the insertion point of the stabilizing and compression screw, but this did not affect the patient’s condition. No cases of implant failure were observed. Revision surgery was needed in one patient due to pseudarthrosis. Three patients died before discharge (one due to pulmonary embolism, two due to cardiac arrest), and five patients died due to unrelated medical conditions within the first 3 months of follow-up.
Discussion
Advances in the treatment of chronic diseases and improvements in living standards have resulted in a considerable increase in the life expectancy of individuals.6 However, as the quality of bone decreases with age, the prevalence of hip fractures increases.7 The stability of fixation for intertrochanteric fractures depends on many factors: the age of the patient; the patient’s general health; the time from fracture to treatment; the adequacy of treatment; concurrent medical treatment; and the stability of fixation.
Which appropriate method and ideal implant to use are topics that are still open to debate, with proponents of the various approaches each claiming advantages over the other methods. Dynamic hip screws are accepted as the gold standard in the surgical treatment of stable intertrochanteric fractures.7 The advantages of making dynamic hip screws the first choice in the treatment of stable fractures do not show similar success rates in unstable fractures. Wolfgang et al8 reported mechanical complication rates of 9% for stable fractures and 19% for unstable fractures in intertrochanteric fractures treated with sliding screw plates. Simpson et al9 listed the causes of fixation failure in intertrochanteric fractures in the following order: cut-out of the screw from the femoral head; pull-out of the plate from the lateral cortex together with the screws; and plate break. Failure of dynamic hip screws in unstable fractures may be as high as 56% in special conditions such as reverse obliquity fractures.10 Intramedullary devices, such as the Gamma nail (Stryker, Kalamazoo, MI, USA), have some theoretical advantages over the dynamic hip screws, as they do not depend on screw fixation of a plate to the lateral cortex, which can be a problem in very osteoporotic bone. In addition, they have a shorter moment arm, because the load is transmitted to the femur along a more medial axis. On the other hand, the Gamma nail has a significantly increased risk of fracture at the tip of the nail, which had reached up to 18% in various studies, and other technical failures (8%–15% of the cases), resulting in a high risk of reoperation.11 In terms of complications, cut-out of the screw, pull-out of the nail, or nail break were not observed in our study.
Gotfried12 reported that the fractures, which were preoperatively classified as type 3.1.A.2, might turn to type 3.2.A.3 fractures postoperatively due to lateral cortex fracture. He attributed fracture of the lateral cortex to weakening of the bone during the use of a lateral cortex drill with a 16 mm diameter for the placement of the sliding screw. The stabilizing and compression screws of the PFN adequately compress the fracture, leaving between them a bone block for further revision, should the need arise. In our study, fracture of the greater trochanter with lateral extension did not occur in any patients during surgery. We concluded that this complication could be avoided by careful determination of the insertion site and sufficient drilling.
Femoral shaft fracture is a complication associated with the use of intramedullary hip nails, and is more frequent with the use of the Gamma nail.13 Fogagnolo et al14 reported one case (1/47) and Banan et al15 reported two cases (2/46) of femoral diaphyseal fractures that occurred distal to the nail. So far, the exact reason for the shaft fractures at the tip of the Gamma nail has not yet been found. Friedl et al16 suggested that the necessary over-reaming of the shaft (3 mm more than the nail diameter) weakens the entire shaft. Frequent drilling for a proper distal interlocking because of malalignment of the aiming device torque of the nail when jammed in an unsatisfactorily reamed shaft is also seen as a cause.17 The PFN has been shown to prevent fractures in the femoral shaft, as it has a smaller distal shaft diameter, which reduces the stress concentration at the tip (a 4.9 mm PFN compared with a 6.28 mm regular Gamma nail).18 Due to its position close to the weight-bearing axis, the stress generated on the intramedullary implants is negligible.18 In our study, only one case had intraoperative femoral fracture and was managed with Dall–Miles wires.
The PFN system, developed by AO/ASIF, offers some major biomechanical innovations that can overcome the known limitations of the Gamma nail. First, the addition of the 6.5 mm antirotation hip pin reduces the incidence of implant cut-out and the rotation of the cervicocephalic fragment.18 Second, the smaller diameter and fluting of the tip of the nail is specially designed to reduce stress forces below the implant and, therefore, reduces the incidence of low-energy fracture at the tip.18 Third, the PFN has a greater implant length, a smaller valgus angle, and this angle is set at a higher level. Fourth, the more proximal positioning of the distal locking helps to avoid abrupt changes in the stiffness of the construct.18 Although the rates of failure of fixation and femoral shaft fracture are low with the PFN, other problems, such as persisting thigh pain and the need for hardware removal because of iliotibial tract irritation, are of concern. Extension of the nail to the distal femoral cortex was not associated with fracture occurrence, but it presented as pain at the medial aspect of the femur.18 This condition was not encountered in our study.
In the series of 295 patients with trochanteric fractures treated with the PFN by Domingo et al,4 the authors emphasized that the surgical technique is not complex, the number of complications recorded was acceptable, and the overall results obtained were comparable with those of other fracture systems. In our study, the intraoperative variables and the systemic complications were similar to those encountered by other authors.3,19 Most patients (78%) showed a near-anatomical fracture reduction, and fracture healing occurred in all patients at the final follow-up. There were few postoperative complications associated with mechanical failure. No cases of implant breakage and fatigue were seen during the follow-up period. The high incidence of open reduction in our study was mainly due to the complexity of the fractures, and not due to delayed operations. In PFN fixations, proper alignment between the two main fragments and proper placement of the lag screws in the femoral head should be ensured. In accordance with similar reports, systemic and local complications, as well as the death rate observed in our study were not different.20,21 The number of reoperations due to technical or mechanical failures was quite high, as was the incidence of intraoperative difficulties in PFN implantation. We also believe that variables such as the duration of hospitalization, commencement of the sitting posture, and early weight-bearing in unstable fractures are related to the pathology, which is associated with advanced age, general health status, and type of fracture, rather than with the surgical technique itself. At present, we consider that the PFN is an acceptable and minimally invasive implant for unstable proximal femoral fractures.
Various studies concerning the functional outcomes of operative treatments of hip fractures have been performed.20,21 For an elderly patient with a femoral neck fracture, the ability to mobilize in their own home and in their community would determine their ability to live independently.22 Before surgical treatment of a femoral neck fracture, the patients and their relatives have to be informed of what should be expected concerning the effect of pre-and perioperative risk factors on the outcome of surgery, postoperative rehabilitation, daily care, and other social issues. Quality of life and function are usually measures that are important for patients and health care providers. The HHS was developed to evaluate outcomes following orthopedic surgery of the hip joint. In our study, the HHS was negatively correlated with the ASA score and patient age.
Conclusion
Our study showed that PFN is a reliable fixation method with good fracture union and no major complications noted across all types of trochanteric femoral fractures.
Disclosure
The authors report no conflicts of interest in this work.
References
Evans PJ, McGrory BJ. Fractures of the proximal femur. Hospital Physician. 2002;38:30–38. | |
Bonnaire F, Zenker H, Lill C, Weber AT, Linke B. Treatment strategies for proximal femur fractures in osteoporotic patients. Osteoporos Int. 2005;16 Suppl 2:S93–S102. | |
Simmermacher RK, Bosch AM, Van der Werken C. The AO/ASIF-proximal femoral nail (PFN): a new device for the treatment of unstable proximal femoral fractures. Injury. 1999;30(5):327–332. | |
Domingo LJ, Cecilia D, Herrera A, Resines C. Trochanteric fractures treated with a proximal femoral nail. Int Orthop. 2001;25(5):298–301. | |
Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51(4):737–755. | |
Siegmeth AW, Gurusamy K, Parker MJ. Delay to surgery prolongs hospital stay in patients with fractures of the proximal femur. J Bone Joint Surg Br. 2005;87(8):1123–1126. | |
Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am.1995;77(7):1058–1064. | |
Wolfgang GL, Bryant MH, O’Neill JP. Treatment of intertrochanteric fracture of the femur using sliding screw plate fixation. Clin Orthop Relat Res. 1982;(163):148–158. | |
Simpson AH, Varty K, Dodd CA. Sliding hip screws: modes of failure. Injury. 1989;20(4):227–231. | |
Haidukewych GJ, Israel TA, Berry DJ. Reverse obliquity fractures of the intertrochanteric region of the femur. J Bone Joint Surg Am. 2001; 83-A(5):643–650. | |
Haynes RC, Pöll RG, Miles AW, Weston RB. Failure of femoral head fixation: a cadaveric analysis of lag screw cut-out with the gamma locking nail and AO dynamic hip screw. Injury. 1997;28(5–6):337–341. | |
Gotfried Y. Percutaneous compression plating of intertrochanteric hip fractures. J Orthop Trauma. 2000;14(7):490–495. | |
Seral B, García JM, Cegoñino J, Doblaré M, Seral F. Finite element study of intramedullary osteosynthesis in the treatment of trochanteric fractures of the hip: Gamma and PFN. Injury. 2004;35(2):130–135. | |
Fogagnolo F, Kfuri M, Paccola CA. Intramedullary fixation of pertrochanteric hip fractures with the short AO-ASIF proximal femoral nail. Arch Orthop Trauma Surg. 2004;124(1):31–37. | |
Banan H, Al-Sabti A, Jimulia T, Hart AJ. The treatment of unstable, extracapsular hip fractures with the AO/ASIF proximal femoral nail (PFN) – our first 60 cases. Injury. 2002;33(5):401–405. | |
Friedl W, Colombo-Benkmann M, Dockter S, Machens HG, Mieck U. [Gamma nail osteosynthesis of per- and subtrochanteric femoral fractures. 4 years experiences and their consequences for further implant development]. Chirurg. 1994;65(11):953–963. German. | |
Aune AK, Ekeland A, Odegaard B, Grøgaard B, Alho A. Gamma nail vs compression screw for trochanteric femoral fractures. 15 reoperations in a prospective, randomized study of 378 patients. Acta Orthop Scand. 1994;65(2):127–130. | |
Radford PJ, Needoff M, Webb JK. A prospective randomised comparison of the dynamic hip screw and the gamma locking nail. J Bone Joint Surg Br. 1993;75(5):789–793. | |
Simmermacher RK, Ljungqvist J, Bail H, et al; AO – PFNA studygroup. The new proximal femoral nail antirotation (PFNA) in daily practice: results of a multicentre clinical study. Injury. 2008;39(8):932–939. | |
Ishida Y, Kawai S, Taguchi T. Factors affecting ambulatory status and survival of patients 90 years and older with hip fractures. Clin Orthop Relat Res. 2005;(436):208–215. | |
Parker MJ, Gurusamy KS, Azegami S. Arthroplasties (with and without bone cement) for proximal femoral fractures in adults. Cochrane Database Syst Rev. 2010;(6):CD001706. | |
Tinetti ME. Clinical practice. Preventing falls in elderly persons. N Engl J Med. 2003;348(1):42–49. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
