Back to Journals » Clinical Ophthalmology » Volume 13
Outcomes of resident-performed small incision cataract surgery in a university-based practice in the USA
Authors Zafar S, Chen X, Sikder S , Srikumaran D , Woreta FA
Received 19 December 2018
Accepted for publication 4 February 2019
Published 20 March 2019 Volume 2019:13 Pages 529—534
DOI https://doi.org/10.2147/OPTH.S198870
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Sidra Zafar, Xinyi Chen, Shameema Sikder, Divya Srikumaran, Fasika A Woreta
Wilmer Eye Institute, Johns Hopkins Hospital, Baltimore, MD, USA
Purpose: To assess outcomes of resident-performed small incision cataract surgery (SICS) at a single academic institute and to determine the availability of SICS-oriented educational resources in residency programs across the USA.
Patients and methods: A retrospective chart review was conducted on all patients who underwent SICS performed by postgraduate year 4 residents between January 2014 and January 2018 at the Wilmer Eye Institute, Baltimore, MD, USA. Postoperative visual acuity, intraoperative complications, and postoperative complications were the main outcomes measured. In addition, a survey was administered to all ophthalmology residency program directors in the USA to assess the presence of SICS-related content in their surgical training curriculum.
Results: Twenty-two eyes of 17 patients underwent planned resident-performed SICS, mainly for white cataracts. Intraoperative complications occurred in two (9.1%) eyes. The most common postoperative complication was transient increased intraocular pressure (two eyes, 9.1%). Mean preoperative best-corrected visual acuity (BCVA) was approximately 20/4,000. The large majority (95.2%) of eyes experienced improved BCVA following SICS, with a mean postoperative BCVA of 20/138 over an average follow-up of 4.2 months. Forty-seven programs responded to the survey (40.1% response rate). Residents were trained in SICS in 66.7% of these programs. However, more than half of all the programs did not have SICS-oriented educational resources available for residents.
Conclusion: Resident-performed SICS was found to be a safe and effective technique for cataract management. Considering the limited surgical volume for SICS in the USA, training programs might instead consider implementing SICS-oriented content in their surgical curriculum, including wet labs.
Keywords: resident, cataract, mature, SICS, surgical training
Introduction
Cataracts account for 47.8%–51.0% of all global blindness.1 Obtaining proficiency in cataract extraction techniques therefore comprises one of the most important elements of ophthalmology resident training. In the USA, while the Accreditation College of Graduate Medical Education requires residents to have performed a minimum of 86 cataract cases at the time of graduation,2 it does not specify a required division of surgical volume between the different surgical techniques. The advent of phacoemulsification as the preferred method for cataract extraction in the developed world has subsequently influenced how residents learn cataract surgery, with training programs placing greater emphasis on the learning of phacoemulsification. While phacoemulsification remains the more common method for cataract extraction in the USA, there is still value in teaching residents other techniques. Indeed, exposure of ophthalmology residents in the USA to techniques such as extracapsular cataract extraction (ECCE) and small incision cataract surgery (SICS) remains limited.3 In 2017, ophthalmology residents in the USA performed, on average, only two cases of ECCE, while only 26% of residents in the USA Veterans Health Administrations reported being trained in SICS.4
Although less commonly utilized inside the USA, ECCE and manual SICS still represent useful techniques for residents to learn. Manual surgical techniques require a skill set different than that of phacoemulsification. Prior exposure is thus particularly important considering that at any point during a surgeon’s career, a conversion from phacoemulsification to manual cataract extraction might be required. SICS has additionally been shown to be comparable to phacoemulsification in terms of both its safety and efficacy and may especially be useful for removal of mature cataracts, where the high phacoemulsification power often needed for nuclear disassembly increases the risk for corneal edema and postoperative inflammation.5 Learning SICS could be of additional benefit to those desiring to spend time at international locations, especially in the developing world where phacoemulsification equipment might not always be available and SICS remains a popular surgical technique owing to its cost-effectiveness and faster surgical times.6
Although other authors have assessed the efficacy and safety of resident-performed manual SICS, most of these studies were conducted abroad6–10 and, to date, there has only been one study, which assessed the outcomes of manual SICS performed in residency training in the USA.11 The purpose of our study was therefore to determine the complication rates and visual outcomes of resident-performed SICS at our institute. Secondly, we aimed to assess the current surgical training curriculum for SICS-related content in ophthalmology residency programs across the USA through a national survey.
Materials and methods
Retrospective review
We conducted a retrospective chart review of all patients who underwent resident-performed manual SICS at the Wilmer Eye Institute between January 2014 and January 2018. The designated primary surgeon for all cases were postgraduate year 4 (PGY-4) resident physicians (14 in total). Although the exact surgical number might vary, PGY-4 residents can perform SICS after they have performed at least 20 phacoemulsification cases and are deemed ready by the cataract surgery educator. Except for one case, the remaining procedures were performed under the supervision of the same attending surgeon. Any case that required conversion from phacoemulsification to SICS was excluded.
Recorded data included information on patient demographics (age, sex, race/ethnicity), past ocular history (presence of ocular comorbidities, laterality of the eye being operated upon, grade of cataract, degree of astigmatism), presence of preoperative risk factors (small pupil, preexisting zonular weakness), anesthesia plan, and the length of follow-up. Data on best-corrected visual acuity (BCVA) and intraocular pressure were collected preoperatively as well as on postoperative day 1, week 1, month 1, and the last follow-up visit. In addition to any intraoperative complication, the occurrence of postoperative complications during the follow-up period was also noted.
Surgical technique
A superior 3-o’clock conjunctival peritomy was performed to expose the bare sclera. Hemostasis was achieved with gentle cautery to the scleral bed. A 6–8 mm frown partial thickness scleral incision was created approximately 2 mm posteriorly to the limbus. A partial thickness scleral tunnel was carried anteriorly into the clear cornea with a crescent blade, widening the tunnel anteriorly. The anterior chamber was filled with an ophthalmic viscosurgical device and a 2.75 mm keratome was used to enter the anterior chamber at the center of the corneoscleral tunnel.
A continuous curvilinear capsulorhexis of ~6.5 mm was initiated with a cystotome and completed using Utrata forceps. The cataractous lens was dialed out of the capsular bag and into the anterior chamber using an iris sweep. The internal opening of the scleral tunnel was widened and the nucleus was removed from the anterior chamber using irrigating vectis. Cortical remnants were removed using bimanual irrigation/aspiration. A three-piece acrylic intraocular lens (IOL) (Alcon AcrySof® 3-piece MA50BM) was placed in the capsular bag. In cases with anterior capsular tear or insufficient zonular support, the three-piece lens was inserted in the ciliary sulcus. If the scleral tunnel was not watertight, interrupted 10–0 nylon sutures were used to close the wound.
Survey
A four-question survey (Qualtrics, Provo, UT, USA) was emailed to all ophthalmology program directors in the USA on April 28, 2018. Information related to resident training in SICS and on the SICS-oriented surgical curriculum offered by the residency programs was collected from the survey.
Participants were made aware that all data would be kept confidential and only aggregate data would be shared. They were also informed that completion of the survey indicated their consent for participation in the study. Two reminder emails were sent during the study period, with response collection ending on June 10, 2018.
Statistical analyses
All statistical analyses were performed using SPSS version 23 (IBM Corporation, Armonk, NY, USA). Mean with SD was computed to describe continuous data. Frequencies and percentages were calculated to describe categorical data.
Ethics statement
The study adhered to the tenets of the Declaration of Helsinki and was conducted after approval from the Institutional Review Board of the Johns Hopkins Hospital. Since this was a retrospective study and all patient data were de-identified, individual patient consent was not required.
Results
Retrospective study
During the 5-year period, a total of 17 patients (22 eyes) underwent manual SICS at our institute. Mean age of the patients was 73.3±11.0 years and 70.6% were female (Table 1). The left eye (12/22, 54.5%) was more commonly operated upon and white or brunescent cataracts were identified in 77.3% (17/22 eyes) of the cases. Preoperative zonular weakness was identified in two (9.1%) eyes.
  | Table 1 Baseline demographic information of patients undergoing resident-performed small incision cataract surgery |
Most cases (9/22, 40.9%) were performed under sub-Tenon’s anesthesia followed closely by general anesthesia (7/22, 31.8%) and retrobulbar block (6/22, 27.2%).
Intraoperative complications occurred in two eyes (9.1%), with one case (4.5%) each of vitreous loss and of anterior capsule tear resulting in sulcus-placed IOL.
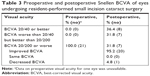
The mean follow-up duration was 4.2±6.4 months. Postoperative complications were observed in four eyes (18.2%) (Table 2) and one patient experienced more than one complication. The most frequently observed complication was transient raised intraocular pressure (two eyes), which was managed conservatively.
  | Table 2 Postoperative complications of eyes undergoing resident-performed small incision cataract surgery |
Other complications included hyphema formation on postoperative day 1 in one eye, which also developed hypotony, and one case of postoperative corneal decompensation in a patient with preexisting Fuchs’ corneal endothelial dystrophy. There were no cases of endophthalmitis, retinal detachment, or surgery-induced cystoid macular edema in our series.
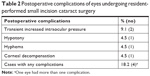
The mean preoperative BCVA in our sample was 2.31±0.74 logarithm of the minimum angle of resolution (logMAR) units (approximately 20/4,000) (Table 3). BCVA was 1.18±0.93 at postoperative day 1, 0.99±0.83 at 1 week, 0.87±0.90 at month 1, and 0.84±0.90 (20/138) at the last follow-up visit. Although an improvement in BCVA was noted for 95.2% (20/21) of the cases, one eye suffered from decreased BCVA, which was attributed to the development of retinal hemorrhage of unclear etiology and neovascular glaucoma (change from 20/200 to no light perception). Eight (57.1%) of the 14 eyes with BCVA worse than 20/40 at the last follow-up visit were deemed to have vision limited by other ocular pathologies (diabetic retinopathy = four eyes; glaucoma = two eyes; macular scarring = one eye; and Fuchs’ dystrophy = one eye) and almost all eyes (6/7, 100.0%) with postoperative BCVA 20/200 or worse had underlying ocular comorbidity (mainly diabetic retinopathy and glaucoma). Astigmatism measurements were available for seven eyes (31.8%), with a mean measurement of 1.50±1.50 D.
Survey
The survey was emailed to 117 program directors and 47 responses were received (40.1% response rate). The geographical regions were relatively equally distributed, with 33.3% from the Northeast, 30.6% from the Midwest, 19.4% from the South, and 16.7% from the West. Of the 47 participants that responded, the large majority (28/47, 66.7%) had formal training in SICS available for residents. In 17 of these 28 programs (60.0%) residents were performing SICS as the primary surgeon in PGY-4, in eight (28.0%) programs during PGY-3, and in three (12%) programs, residents undertook SICS surgeries starting in PGY-2.
Table 4 shows whether any of the surgical training elements were available and/or required at the residency programs. More than half of all the programs did not have SICS-oriented classroom lectures (53.2%) or formal wet lab courses (57.4%) available for residents. Furthermore, 48.9% of the programs did not have any supervised wet lab sessions on SICS.
  | Table 4 Availability and requirement of surgical training curriculum elements on small incision cataract surgery in the residency programs surveyed |
Discussion
We found resident-performed SICS at our institute to be both safe and efficacious for cataract extraction, especially for white or brunescent cataracts. Vision improved in >90.0% of all our patients, increasing from an average of 2.31 logMAR units preoperatively (approximately 20/4,000) to 0.84 (20/138) at the last postoperative follow-up visit.
Demographics
Females accounted for 71.0% of our study population. A similar sex disparity was also reported by Lynds et al,11 who to the best of our knowledge are currently the only other group to have assessed the outcomes of resident-performed SICS inside the USA.11 Although females are known to account for two-thirds of all people living with cataracts,12 studies from developing countries have consistently shown female patients to access cataract care at much lower rates than men,13 potentially resulting in later presentation with more advanced cataracts. This gender-based inequity in underutilization of eye care services is believed to result from a combination of factors that are more commonly known to affect women and include financial costs, transport limitations, and socioeconomic status.12,13 The relatively higher proportion of females in our sample could potentially also be attributable to sex differences in longevity and the possibility of selective survival.14
African Americans made up 64.7% of our patient population, while Hispanics accounted for 46.2% of the population in the study by Lynds et al.11 As age-specific cataract prevalence rates among Hispanics and African Americans are comparable to other races as well as to USA national estimates,15 we believe this racial distribution may be more reflective of poor uptake of eye care resources among these populations.
Operative outcomes
The intraoperative complication rate for resident-performed SICS at our institute was 9.1%. Vitreous loss was observed in one case, with our incidence rate comparable to that of previously reported literature. Studies from developing nations have reported vitreous loss rates of between 0.67% and 8.2% for resident-performed SICS,6–9 which is comparable to the vitreous loss rate of 4.5% at our institute. In the USA, Lynds et al11 had a vitreous loss rate of 1.9%, with relatively higher frequencies for other intraoperative complications, including iris prolapse (9.6%) and zonular dialysis (7.7%). Our observed vitreous loss rate was also well within the 1.8%–14.7% range reported across several different resident-performed phacoemulsification studies.16–18
Postoperative complications were observed in 18.2% of our cases over a mean follow-up duration of over 4 months. A similar rate (23.1%) was also reported by Lynds et al.11 The large majority of postoperative complications observed in our sample were, however, of minor clinical significance and were successfully managed through conservative measures.
Visual outcomes achieved with SICS are comparable to those of phacoemulsification,19 with 71.0%–95.2% of all patients undergoing resident-performed SICS achieving a BCVA of 20/40 or better.6–8,10,11 In our sample, 38.1% of all patients achieved a BCVA of 20/40, which improved to 61.5% when those with preexisting ocular pathologies were removed. Based on presenting visual acuity, improved vision was noted in 95.2% patients. We believe that in addition to the presence of preexisting ocular pathology, which has been shown to be a strong independent predictor of visual outcomes after cataract surgery,20 the final visual acuity in our sample could potentially also have been limited by the increased age of our patients. Indeed, studies have shown increasing patient age to be associated with poor visual outcomes following cataract surgery.20–22 In their evaluation of >3,500 cataract surgeries, Matta et al found that the risk for poor visual outcomes was increased by 4.63-fold among patients aged ≥70 years,22 whereas Schein et al showed that people aged 75–95 years were 3.6 times more likely not to show improvement in cataract surgery-related outcomes than people aged 50–64 years, even after adjustment for ocular comorbidities.23
Survey
In a recent survey-based study, it was found that most ophthalmologists practicing in the USA believed that manual cataract extraction was an important skill that should be taught to residents. We found 67.0% of the 47 programs that responded were training their residents in SICS. SICS-specific educational resources were, however, offered at less than half of all these programs. Considering the limited opportunities USA resident ophthalmologists may have for performing SICS over the course of their training, residency programs can instead consider placing emphasis on improving training outside the operating room. Wet lab is one such training resource that has been associated with improving technical proficiency of the residents and surgical skill acquisition. In a recent study by Ramani et al, resident-performed manual SICS was in fact associated with significantly decreased intraoperative complication rates and improved postoperative visual outcomes, after implementation of a structured curriculum for wet lab practice.24 Planned training can potentially also result in greater resident comfort level for performing SICS, especially during cases needing conversion from phacoemulsification. Furthermore, SICS can be a useful technique to learn for ophthalmologists who may want to work in developing countries where standard phacoemulsification equipment may not always be available. Learning SICS can also teach residents good scleral tunnel construction, which can be beneficial in certain settings such as anterior chamber IOL placement. Thus, while phacoemulsification remains the standard of care in the USA, SICS should be considered a viable technique, particularly for dense cataracts.
Limitations
Our study has several limitations, including its retrospective nature, which may have limited the quality of our data. Secondly, 18.2% of our cases were lost to early follow-up, which may have resulted in the loss of patients who potentially had room for visual improvement. Furthermore, these patients might have been at risk of developing late postoperative complications. Thirdly, because of our small sample size, even small changes in patient-related outcomes made substantial changes in the frequency. Another limitation of our study is the absence of resident-performed phacoemulsification cases as the control group. The reason we did not have a control group was because the cataracts assessed in our sample were deemed too dense for safe removal through phacoemulsification. Larger studies are needed to assess outcomes of resident-performed SICS with that of phacoemulsification.
Conclusion
Manual SICS is an important technique that USA ophthalmology residents should gain exposure to during their training. The technique is especially useful for white or brunescent cataracts that are likely to cause difficulty with phacoemulsification. Our findings showed SICS to be an efficacious surgical technique that can safely be performed by residents. We also found that more than half of all residency programs surveyed in our study did have SICS-specific educational resources available for residents. Because of the limited surgical volume, training programs should consider placing SICS-related content in their current surgical curriculum, including wet lab practice sessions.
Acknowledgments
The authors would like to acknowledge the Mitchell Trust for its continued support of their work and Wilmer Biostatistical Department (Core Grant EY01765) for assistance with data analysis.
Disclosure
The authors report no conflict of interest in this work.
References
Khairallah M, Kahloun R, Bourne R, et al. Number of people blind or visually impaired by cataract worldwide and in world regions, 1990 to 2010. Invest Ophthalmol Vis Sci. 2015;56(11):6762–6769. | ||
Education ACfGM. Required minimum number of procedures for graduating residents in ophthalmology. 2013. Available from: https://www.acgme.org/Portals/0/PFAssets/ProgramResources/240_Oph_Minimum_Numbers.pdf. Accessed March 06, 2019. | ||
Pershing S, Kumar A. Phacoemulsification versus extracapsular cataract extraction: where do we stand? Curr Opin Ophthalmol. 2011;22(1):37–42. | ||
Chen CK, Tseng VL, Wu WC, Greenberg PB. A survey of the current role of manual extracapsular cataract extraction. J Cataract Refract Surg. 2010;36(4):692–693. | ||
Riaz Y, de Silva SR, Evans JR, Cochrane Eyes and Vision Group. Manual small incision cataract surgery (MSICS) with posterior chamber intraocular lens versus phacoemulsification with posterior chamber intraocular lens for age-related cataract. Cochrane Database Syst Rev. 2013;102(6):CD008813. | ||
Haripriya A, Chang DF, Reena M, Shekhar M. Complication rates of phacoemulsification and manual small-incision cataract surgery at Aravind Eye Hospital. J Cataract Refract Surg. 2012;38(8):1360–1369. | ||
Garima A, Hansa T, Kamini A. Visual outcome and major surgical complications of manual small incision cataract surgery versus extra capsular cataract extraction performed by resident doctors in a regional institute of ophthalmology. Gujarat Medical J. 2015;70(2):31–36. | ||
Decroos FC, Chow JH, Garg P, Sharma R, Bharti N, Boehlke CS. Analysis of resident-performed manual small incision cataract surgery (MSICS): an efficacious approach to mature cataracts. Int Ophthalmol. 2012;32(6):547–552. | ||
Gupta SK, Kumar A, Kumar D, Agarwal S. Manual small incision cataract surgery under topical anesthesia with intracameral lignocaine: study on pain evaluation and surgical outcome. Indian J Ophthalmol. 2009;57(1):3–7. | ||
Khanna RC, Kaza S, Palamaner Subash Shantha G, Sangwan VS. Comparative outcomes of manual small incision cataract surgery and phacoemulsification performed by ophthalmology trainees in a tertiary eye care hospital in India: a retrospective cohort design. BMJ Open. 2012;2(5):e001035. | ||
Lynds R, Hansen B, Blomquist PH, Mootha VV. Supervised resident manual small-incision cataract surgery outcomes at large urban United States residency training program. J Cataract Refract Surg. 2018;44(1):34–38. | ||
Abou-Gareeb I, Lewallen S, Bassett K, Courtright P. Gender and blindness: a meta-analysis of population-based prevalence surveys. Ophthalmic Epidemiol. 2001;8(1):39–56. | ||
Lewallen S, Courtright P. Gender and use of cataract surgical services in developing countries. Bull World Health Organ. 2002;80(4):300–303. | ||
Kochanek KD, Murphy SL, Xu J, Arias E. Mortality in the United States, 2016. NCHS Data Brief, No 293. National Center for Health Statistics; 2017. Available from: https://www.cdc.gov/nchs/data/databriefs/db293.pdf. Accessed March 06, 2019. | ||
Grober ED, Jewett MAS. The concept and trajectory of “operative competence” in surgical training. Can J Surg. 2006;49(4):238–240. | ||
Corey RP, Olson RJ. Surgical outcomes of cataract extractions performed by residents using phacoemulsification. J Cataract Refract Surg. 1998;24(1):66–72. | ||
Bhagat N, Nissirios N, Potdevin L, et al. Complications in resident-performed phacoemulsification cataract surgery at New Jersey Medical School. Br J Ophthalmol. 2007;91(10):1315–1317. | ||
Allinson RW, Metrikin DC, Fante RG. Incidence of vitreous loss among third-year residents performing phacoemulsification. Ophthalmology. 1992;99(5):726–730. | ||
Gogate P, Optom J, Deshpande S, Naidoo K. Meta-analysis to compare the safety and efficacy of manual small incision cataract surgery and phacoemulsification. Middle East Afr J Ophthalmol. 2015;22(3):362–369. | ||
Wong TY. Effect of increasing age on cataract surgery outcomes in very elderly patients. BMJ. 2001;322(7294):1104–1106. | ||
Venkatesh R, Muralikrishnan R, Balent LC, Prakash SK, Prajna NV. Outcomes of high volume cataract surgeries in a developing country. Br J Ophthalmol. 2005;89(9):1079–1083. | ||
Matta S, Park J, Palamaner Subash Shantha G, Khanna RC, Rao GN. Cataract surgery visual outcomes and associated risk factors in secondary level eye care centers of L V Prasad Eye Institute, India. PLoS One. 2016;11(1):e0144853. | ||
Schein OD, Steinberg EP, Cassard SD, Tielsch JM, Javitt JC, Sommer A. Predictors of outcome in patients who underwent cataract surgery. Ophthalmology. 1995;102(5):817–823. | ||
Ramani S, Pradeep TG, Sundaresh DD. Effect of wet-laboratory training on resident performed manual small-incision cataract surgery. Indian J Ophthalmol. 2018;66(6):793–797. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.