Back to Journals » Clinical Ophthalmology » Volume 14
Outcomes of Pre-Early Treatment for Retinopathy of Prematurity (Pre-ETROP)
Authors Titawattanakul Y , Kulvichit K, Varadisai A , Mavichak A
Received 16 July 2020
Accepted for publication 24 September 2020
Published 16 October 2020 Volume 2020:14 Pages 3393—3397
DOI https://doi.org/10.2147/OPTH.S268997
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Yothin Titawattanakul, Kittisak Kulvichit, Adisai Varadisai, Apivat Mavichak
Vitreo-retina Research Unit, Department of Ophthalmology, Faculty of Medicine, King Chulalongkorn Memorial Hospital, Chulalongkorn University, Bangkok, Thailand
Correspondence: Kittisak Kulvichit
Department of Ophthalmology, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand
Tel +66 2 2564000
Email [email protected]
Introduction: The earlier treat stage 3 ROP is more likely to achieve better outcomes.
Primary Purpose: To study the unfavorable outcomes and regression after pre-early treatment for ROP.
Secondary Purpose: To evaluate the progression and recurrence of ROP requiring retreatment after pre-early treatment for ROP.
Patients and Methods: The data were retrieved retrospectively from the medical records of all infants who were screened and treated for ROP from January 2009 to January 2014 at a tertiary care facility. The outcomes measured the following: 1. unfavorable outcomes; 2. regression of ROP; 3. progression of ROP and 4. recurrence of ROP requiring retreatment. We treated all stage 3 ROP in any zone, with or without plus. The study also compared the outcomes between the pre-ETROP and the ETROP subgroups.
Results: There were 91 eyes with stage 3 ROP. Of the total of 91 eyes, there were 63 eyes with the pre-ETROP group and 28 eyes of the ETROP group. The unfavorable outcomes after treatment occur 6 eyes from 28 eyes (21.43%) in the ETROP group but no unfavorable outcomes in the pre-ETROP group (P=0.001). The pre-ETROP group who were treated with laser LIO alone had 100% regression, while the ETROP group who were treated with LIO (26 eyes) had 88.46% regression. There were 2 eyes of this group who were treated with a combination of LIO and IVT Bevacizumab. Both of them did not have regression. The recurrence of ROP requiring retreatment occurred in 2 eyes (7.14%) of the ETROP group, but no recurrence in the pre-ETROP group (P=0.092). The progression after treatment occurred in 3 eyes (10.71%) in the ETROP group, but no progression in the pre-ETROP group (P=0.027).
Conclusion: The pre-ETROP treatment is useful for reducing unfavorable outcomes and increasing the regression of ROP. Further, the treatment can reduce the recurrence of neovascularization and progression after treatment.
Keywords: retinopathy of prematurity, pre-early treatment for retinopathy of prematurity, outcomes, regression
Introduction
Retinopathy of prematurity (ROP) is one of the leading causes of blindness and severe visual impairment worldwide in preterm infants, especially in middle-income countries such as China, India, Vietnam, and Thailand.1–3 The incidence of ROP is increasing globally mainly because of the advancement of neonatal care, and therefore the survival rate of premature infants has also increased.4 In 2010, on average 13.0 million of 15.0 million preterm born infants were estimated to have survived after one month of life.5 At least 184,700 infants were found to have ROP and 53,800 infants progressed to potent visual impairment and required treatment.6 In Thailand, the incidence of ROP is about 3402 infants per year.7 The amount of blindness and low vision in Thai children was approximately 13,101 cases in 2006–2007.8 One of the major causes of blindness in Thai children is retinopathy of prematurity (66.67%).8 ROP is an important problem in public health. However, visual impairment from ROP can be significantly reduced with early detection and timely treatment.
Retinopathy of prematurity is a disease of abnormal retinal vascular development in prematurity. The major risk factors are low birth weight and low gestational age (GA).9 The incomplete vascularization of the immature retina causes local ischemia, with subsequent retinal neovascularization, and after that fibrovascular proliferation (stage 3 ROP) occurs. The end stages of the disease involve retinal detachment, which is the main cause of blindness from ROP.
There has not been a specific treatment for ROP in the past. Until 1988, Cryotherapy for Retinopathy of Prematurity (CRYO-ROP) study suggested treatment for threshold ROP (stage 3 ROP in zone I or II with plus disease extending for 5 contiguous clock hours [150 degrees] or 8 cumulative clock hours [240 degrees]) with cryotherapy, ie ablation of the peripheral avascular retina. The study showed a reduction in unfavorable outcomes by about 50% (21.8% with unfavorable outcomes in the treatment group compared to 43.0% in the control group).10 However, the long-term outcomes of treated patients have been frequently poor. A recent report from the CRYO-ROP study found that, when the children were 15 years old, almost half of the treated eyes (44%) had visual acuity of 6/60 or worse despite their improved retinal outcomes after treatment.11 In 2003, the benefits of earlier treatment of ROP infants were studied in a Multicenter Early Treatment for Retinopathy of Prematurity (ETROP) study. This study was randomly allocated the patients to early laser treatment or conventional management. The outcomes demonstrated reduction in unfavorable visual acuity outcomes (from 19.5% to 14.5%, P = 0.01) and unfavorable structural outcomes in the earlier treatment group (from 15.6% to 9.1%, P < 0.001).12 The analysis of previous studies found that the earlier treatment for ROP yields both better structural and visual outcomes; however, in the early treatment of ROP infants in the ETROP study were still found to have some unfavorable visual and structural outcomes. For the management of ROP infants at King Chulalongkorn Memorial Hospital (KCMH), we have been routinely treating ROP infants earlier than seen in previous studies. We treated all infants that had stage 3 ROP in any zone with or without plus disease. In this study, we analyze the outcomes of the practice in terms of unfavorable outcomes, regression of ROP after the treatment, progression of ROP after the treatment, and recurrence of ROP requiring retreatment.
Patients and Methods
The institutional review boards (IRB) of Faculty of Medicine, Chulalongkorn University approved the study, which followed the WMA Declaration of Helsinki. A patient informed consent to review their medical records was not required by the IRB since the study was retrospective design and the data were extracted from medical records. Moreover, the patient data confidentiality was strictly protected and all the case record forms were anonymised.
The medical records of all infants that were screened and treated for ROP at the Clinic, the Neonatal Intensive Care Unit (NICU), and the Prematurity Unit between January 2009 and January 2014 were reviewed retrospectively. Subjects were included if they were diagnosed with ROP. Case recording forms were used to collect the data, which were divided into 4 parts: general data, Ante-, Peri-, and Post-natal data, ROP associated data, sequelae, and outcomes.
The primary outcomes were unfavorable outcomes and the regression of ROP. The secondary outcomes were progression after the treatment and the recurrence of ROP requiring retreatment.
The operational definitions used in this study are as follows:
- Pre-Early Treatment for ROP (Pre-ETROP) was the treatment, using either Cryoretinopexy or Laser Indirect Ophthalmoscope (LIO), for any stage 3 ROP in any zone with or without plus disease within 48 hours of diagnosis.
- Standard treatment was the treatment according to ETROP study guidelines.13
- The unfavorable outcomes were defined as posterior retinal fold involving the macula, retinal detachment involving the macula, and retrolental tissue or mass obscuring the view of the posterior pole.
- The regression of ROP was defined as retinal vessel growth into the retinal avascular area; the decrease of the height and width of the intraretinal ridge; the regression of the neovascularization membrane.
- The progression of ROP was defined as the increasing extent of neovascularization or progression to the next stage.
- The recurrence of ROP was defined as the recurrence of neovascularization after the regression of ROP.
After collecting the data, the researcher analyzed it using descriptive statistics on various aspects, such as demographic data for frequency, and percentage, mean, and standard deviation. The results of the unfavorable outcomes, the regression of ROP after the treatment, the progression of ROP after the treatment, and the recurrence of ROP requiring retreatment were collected and analyzed for frequency, percentage, and comparison between subgroups using Chi-square test and Fisher’s exact test in order to compare the 2 independent groups.
Results
We found and collected the records on 183 eyes from 96 patients with any ROP and in any zone. The demographic data are shown in Table 1. There were 91 eyes with stage 3 ROP in any zone and with or without plus that needed LIO treatment according to our pre-ETROP protocol. The majority of these 91 eyes were females (57.1% in both groups).
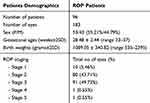 |
Table 1 Demographic Data of All ROP Infants |
Among these treated 91 eyes, 28 fit the criteria for treatment in the ETROP study. The other 63 eyes had pre-ETROP findings, eg stage 3 zone 2 without plus or pre plus. All 28 eyes that fit the ETROP criteria were those of the prethreshold type 1 ROP. The mean gestational ages and birth weights of the pre-ETROP subgroup were 28.02 ± 2.69 weeks and 983.14 ± 299.40 grams respectively. The ETROP subgroup had mean gestational ages and birth weights of 28.79 ± 2.35 weeks and 1211.43 ± 295.00 grams respectively (Table 2). Most of the eyes in the ETROP subgroup were referral cases.
 |
Table 2 Comparison Characteristics Between the Pre-ETROP and the ETROP Subgroups |
The unfavorable outcomes occurred in 6 eyes in the ETROP group but there were none in the pre-ETROP group and were statistically significant using Fisher’s exact test (P=0.001) (Table 3). All 6 eyes with unfavorable outcomes were at stage 3 ROP in zone 2 with plus. There were 4 eyes treated with laser LIO and that had developed retinal detachment involving the macula in one eye and fibrovascular traction at the macula in 3 eyes. Only 2 eyes were treated with combined laser LIO and intravitreous Bevacizumab. Both developed retinal detachment involving macula. A subgroup analysis of the eyes with unfavorable outcomes found that 2 eyes had a recurrence of neovascularization after regression. There were 3 eyes progressed after treatment without regression and subsequently caused unfavorable outcomes. Only 1 eye had fibrovascular traction at the macula after regression. The pre-ETROP group revealed 100% regression after the treatment (63 eyes). On the other hand, the ETROP group achieved 88.46% regression (23 eyes) and 11.54% non-regression (3 eyes) and 2 eyes of this group that were treated with combined laser LIO and intravitreous Bevacizumab did not regress. The pre-ETROP group exhibited greater regression after treatment than the ETROP group, and this was found to be statistically significant using Fisher’s exact test (P=0.002) (Table 3).
 |
Table 3 Comparison of Outcomes Between the Pre-ETROP and the ETROP Subgroups |
The recurrence of neovascularization after regression ROP and requiring retreatment occurred in 2 eyes (7.14%) of the ETROP group, but there was no recurrence in the pre-ETROP group (P=0.092). The progression after ROP treatment without regression ROP occurred in 3 eyes (10.71%) in the ETROP group, but there was none in the pre-ETROP group (P=0.027). Two eyes progressed to the proliferation of more neovascularization and led to the development of retinal detachment (1 eye had ROP stage 4 and the other had stage 5). These eyes were treated with combined LIO and intravitreal Bevacizumab. There was 1 eye at stage 5 ROP that was treated with only LIO without intravitreal Bevacizumab.
Discussion
The Cryotherapy for Retinopathy of Prematurity (CRYO-ROP) study suggested treatment for threshold ROP.10 The results of the study revealed that unfavorable outcomes occurred in the treatment group at around 21.8%. The Multicenter Early Treatment for Retinopathy of Prematurity (ETROP) study, which considered a treatment earlier, found unfavorable visual outcomes at 14.5% and unfavorable structural outcomes at 9.1% in the treatment group. The question remains whether the ETROP criteria for treatment are early enough. At King Chulalongkorn Memorial Hospital, we did not follow either CRYO-ROP or ETROP guidelines. Instead, we regarded all the ROP stage 3 the same, ie, the existence of neovascularization. Consequently, we treated all stage 3 ROP regardless of zone or plus disease. All of the cases were treated with either cryotherapy or LIO within 48 hours of diagnosis. However, since we are a tertiary center, we also had some cases that fit the ETROP criteria at the first visit. Therefore in this study, we compare the results between those in the pre-ETROP and the ETROP group. The birth weight was lower in the pre-ETROP group. No unfavorable outcomes occurred in the pre-ETROP group, while the ETROP group had 21.43% unfavourable outcomes, similar to previous study.
The data from the Bevacizumab Eliminates the Angiogenic Threat of Retinopathy of Prematurity (BEAT-ROP) study showed that the intravitreous Bevacizumab was significantly more effective than conventional laser therapy for stage 3 ROP with plus in zone 1 but not zone 2.14 The rate of recurrence ROP with zone 1 disease was 42% in the laser group compared with 6% in the intravitreous Bevacizumab group (P=0.003), but with zone 2 posterior disease was not differ significantly between the laser group and the Bevacizumab group, with 12% in laser group and 5% in the intravitreous Bevacizumab group (P=0.27).14 The results of this study showed no recurrence in the pre-ETROP group, compared to 7.14% in the ETROP group.
In the ETROP study, it was found that the progression from prethreshold type 2 ROP to prethreshold type 1 ROP occurred 22.1%.15 We found that if the prethreshold type 2 that had stage 3 in zone 2 without plus or pre plus in this study received treatment by laser LIO, there would be no progression to prethreshold type 1 ROP. The recurrence after regression occurred in 7.14% of the ETROP group, but there was no recurrence in the pre-ETROP group.
The results from this study suggest that the earlier we treat stage 3 ROP, the more likely it is to achieve better outcomes. A prospective well-controlled study would provide more solid evidence to proposal.
Conclusion
The pre-ETROP treatment is useful for reducing unfavorable outcomes and increasing the regression of ROP after treatment. Further, the pre-ETROP treatment can reduce the recurrence of neovascularization after regression ROP and progression after treatment.
Acknowledgments
The authors would to thanks the scholarship from the graduate school, Chulalongkorn University to commemorate the 72nd anniversary of his majesty King Bhumibala Aduladeja.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Gilbert C, Fielder A, Gordillo L, et al. Characteristics of infants with severe retinopathy of prematurity in countries with low, moderate, and high levels of development: implications for screening programs. Pediatrics. 2005;115(5):518–525. doi:10.1542/peds.2004-1180
2. Gilbert C, Rahi J, Eckstein M, et al. Retinopathy of prematurity in middle-income countries. Lancet. 1997;350(9070):12–14. doi:10.1016/S0140-6736(97)01107-0
3. Chen Y, Feng J, Gilbert C, et al. Time at treatment of severe retinopathy of prematurity in China: recommendations for guidelines in more mature infants. PLoS One. 2015;10(2). doi:10.1371/journal.pone.0116669
4. Quinn GE. Retinopathy of prematurity blindness worldwide: phenotypes in the third epidemic. Eye Brain. 2016;8:31–36. doi:10.2147/EB.S94436
5. Blencowe H, Lee A, Cousens S, et al. Preterm birth–associated neurodevelopmental impairment estimates at regional and global levels for 2010. Pediatr Res. 2013;74(S1):17–34. doi:10.1038/pr.2013.204.
6. Blencowe H, Lawn JE, Vazquez T, et al. Preterm-associated visual impairment and estimates of retinopathy of prematurity at regional and global levels for 2010. Pediatr Res. 2013;74(S1):35–49. doi:10.1038/pr.2013.205
7. Department of medical services, Ministry of public health, Thailand. Guideline for the Screening and Treatment of Retinopathy of Prematurity. The Agricultural Cooperative Federation of Thailand., LTD. 2004: 1–11.
8. Wongkittirux K. Blindness, low vision and eye diseases in Thai children 2006–2007. J Health Serv Res. 2012;6(4):501–512.
9. Hellström A, Smith L, Dammann O. Retinopathy of prematurity. Lancet. 1991;337(8733):83–84.
10. Cryotherapy for Retinopathy of Prematurity Cooperative Group. Multicenter trial of cryotherapy for retinopathy of prematurity. Preliminary results. Arch Ophthalmol. 1988;106(4):471–479. doi:10.1001/archopht.1988.01060130517027.
11. Palmer EA, Hardy RJ, Dopson V, et al. 15-year outcomes following threshold retinopathy of prematurity: final outcomes from the multicenter trial of cryotherapy for retinopathy of prematurity. Arch Ophthalmol. 2005;123(3):311–318. doi:10.1001/archopht.123.3.311
12. Good WV. Early treatment for Retinopathy of prematurity cooperative group. Final results of the early treatment for retinopathy of prematurity (ETROP) randomized trial. Trans Am Ophthalmol Soc. 2004;102:233–248.
13. American Academy of Pediatrics Section on Ophthalmology. Screening examination of premature infants for retinopathy of prematurity. Pediatrics. 2013;131(1):189–195. doi:10.1542/peds.2012-2996
14. Mintz-Hittner HA, Kennedy KA, Chuang AZ. Efficacy of intravitreal bevacizumab for stage 3+ retinopathy of prematurity. N Engl J Med. 2011;364(7):603–615. doi:10.1056/NEJMoa1007374
15. Christiansen SP, Dobson V, Quinn GE, et al. Progression of type 2 to type 1 retinopathy of prematurity in the early treatment for retinopathy of prematurity study. Arch Ophthalmol. 2010;128(4):461–465. doi:10.1001/archophthalmol.2010.34
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
