Back to Journals » Infection and Drug Resistance » Volume 12
Oral sitafloxacin vs intravenous ceftriaxone followed by oral cefdinir for acute pyelonephritis and complicated urinary tract infection: a randomized controlled trial
Authors Lojanapiwat B, Nimitvilai S, Bamroongya M, Jirajariyavej S , Tiradechavat C , Malithong A, Predanon C, Tanphaichitra D, Lertsupphakul B
Received 25 June 2018
Accepted for publication 5 September 2018
Published 8 January 2019 Volume 2019:12 Pages 173—181
DOI https://doi.org/10.2147/IDR.S178183
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sahil Khanna
Bannakij Lojanapiwat,1 Sireethorn Nimitvilai,2 Manit Bamroongya,3 SupunNee Jirajariyavej,4 Chirawat Tiradechavat,5 Aumnat Malithong,6 Chagkrapan Predanon,7 Dan Tanphaichitra,8 Boonlert Lertsupphakul9
1Department of Surgery, Maharaj Nakorn Chiang Mai Hospital, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand; 2Department of Internal Medicine, Nakhon Pathom Hospital, Nakhon Pathom, Thailand; 3Department of Surgery, Buddasothorn Hospital, Chachoengsao, Thailand; 4Department of Medicine, Taksin Hospital, Bangkok, Thailand; 5Department of Surgery, Udon Thani Hospital, Udon Thani, Thailand; 6Department of Medicine, BMA General Hospital, Bangkok, Thailand; 7Department of Surgery, Khon Kaen Hospital, Khon Kaen, Thailand; 8Department of Internal Medicine, Anandamahidol Hospital, Lopburi, Thailand; 9Department of Surgery, Maharaj Nakorn Si Thammarat Hospital, Nakhon Si Thammarat, Thailand
Background: The conventional antibiotic regimen for community-acquired upper urinary tract infections with moderate severity in Thailand is parenteral ceftriaxone (CTRX) for several days followed by oral cephalosporin for 7–14 days. The aim of this study was to compare the efficacy and safety of oral sitafloxacin (STFX) with that of intravenous CTRX followed by oral cefdinir (CFDN) for the therapy of acute pyelonephritis (APN) and complicated urinary tract infection (cUTI).
Methods: This open-label, randomized, controlled, noninferiority clinical trial included patients from nine centers across Thailand. Adult patients with APN or cUTI were randomly assigned to receive 100 mg of oral STFX twice daily for 7–14 days, or 2 g of intravenous CTRX for several days followed by 100 mg of oral CFDN three times per day for another 4–12 days.
Results: A total of 289 adult patients with APN or cUTI (141 in the STFX group and 148 in the CTRX/CFDN group) were included in the intent-to-treat (ITT) analysis, and 211 patients (108 in the STFX group and 103 in the CTRX/CFDN group) were included in the per-protocol (PP) analysis. The baseline characteristics of patients in both groups were comparable. The causative pathogen in most patients with APN or cUTI was Escherichia coli. The clinical success rates at the end of treatment revealed the STFX regimen to be noninferior to the CTRX/CFDN regimen (86.6% vs 83.8% for ITT analysis and 97.2% vs 99.0% for PP analysis, respectively). Adverse events with mild-to-moderate severity were similar between groups.
Conclusion: Oral STFX is noninferior to intravenous CTRX followed by oral CFDN in adult patients with APN and cUTI. Lower rates of resistance compared to CTRX and/or CFDN and oral administration suggest STFX as a more attractive treatment option in this patient population.
Keywords: acute pyelonephritis, complicated urinary tract infection, sitafloxacin, ceftriaxone, cefdinir
Background
Urinary tract infection (UTI) is one of the most common community-acquired bacterial infections worldwide.1 UTIs are usually categorized as lower UTI or acute cystitis, and upper UTI or acute pyelonephritis (APN).2,3 Acute cystitis is a localized infection in the urinary bladder, whereas APN is usually an ascending infection from the lower urinary tract to the kidneys, with systemic manifestations of infection that can include sepsis. UTI in healthy individuals who have no structural or neurologic urinary tract abnormalities is most often uncomplicated UTI. In contrast, complicated UTI (cUTI) occurs in patients with urinary abnormality, urinary device, or immunocompromised condition. APN or cUTI is associated with increased morbidity and mortality, and it is the most common cause of secondary bacteremia. The most common pathogen that causes UTI is Escherichia coli (E. coli), followed by Klebsiella pneumoniae, and Proteus mirabilis.
Antibiotics with activity against Enterobacteriaceae, especially fluoroquinolones, are usually recommended for the treatment of UTIs;4 however, the prevalence of fluoroquinolone-resistant Enterobacteriaceae has been increasing worldwide.5 Sixty percent of urinary E. coli isolates from Thai patients were resistant to ciprofloxacin and levofloxacin.6 The conventional antibiotic regimen for the treatment of Thai patients with APN with moderate severity of infection is intravenous ceftriaxone (CTRX) for several days, followed by oral cephalosporin (e.g., cefdinir [CFDN] or cefixime) for 7–14 days.
Sitafloxacin (STFX), an oral antibiotic, is an advanced-generation fluoroquinolone with excellent activity against Gram-negative bacteria, including isolates that are resistant to ciprofloxacin and levofloxacin.7,8 STFX has been available in Japan for decades, and has been available in Thailand since 2012 for the treatment of respiratory tract and genitourinary tract infections. STFX was much more active than ciprofloxacin and levofloxacin against E. coli isolated from Thai patients with UTIs, and it was also active against most isolates of extended-spectrum beta-lactamase (ESBL)-producing E. coli.9,10 The bioavailability of oral STFX is 89%, and the intake of food does not significantly adversely affect the pharmacokinetics of STFX.11 STFX is primarily eliminated by the kidney, and its very high concentration in urine makes it suitable for therapy of UTI.11 Clinical studies conducted in Japan reported that STFX demonstrated good clinical efficacy and microbiological eradication of uropathogens in patients with cUTIs.12,13
The aim of this study was to compare the efficacy and safety of oral STFX with that of intravenous CTRX followed by oral CFDN for the treatment of APN and cUTI.
Methods
Study design
This prospective, open-label, randomized, controlled, noninferiority, multicenter clinical trial was conducted at nine medical centers in Thailand, including Maharaj Nakorn Chiang Mai Hospital, Nakhon Pathom Hospital, Buddasothorn Hospital, Taksin Hospital, Udon Thani Hospital, BMA General Hospital, Khon Kaen Hospital, Anandamahidol Hospital, and Maharaj Nakhon Si Thammarat Hospital during August 2013 to September 2015 study period. The Institutional Review Board or Independent Ethics Committee of each participating hospital reviewed and approved the study protocol. Written informed consent was obtained from all study participants prior to enrollment.
Study population
Eligible patients aged 18–70 years who met the diagnostic criteria for APN or cUTI, and for whom antimicrobial therapy was recommended by their responsible physicians were hospitalized. APN was defined as UTI with ≥2 of the following symptoms/signs: fever; flank pain or pelvic pain; nausea or vomiting; dysuria, urinary frequency, or urinary urgency; costovertebral area tenderness; and/or evidence of pyuria in the urine sample. cUTI was defined as APN in patients with diabetes mellitus (DM), systemic lupus erythematosus, renal diseases (eg, glomerulonephritis), or obstructive uropathy with no need for surgical procedures. The major exclusion criteria were pregnant/lactating women or women who intended to become pregnant; renal abscess requiring surgical intervention; ileal loop urinary diversion; renal transplantation; persistent indwelling urinary catheter after completing the study treatment; suspected or confirmed prostatitis or prostatic abscess; history of or current convulsive diseases; myasthenia gravis or other central nervous system diseases; hypersensitivity to fluoroquinolones, beta-lactams, or any component of the study antibiotics; history of QT interval prolongation on electrocardiogram; inability to take oral medicines; requirement for additional systemic antibiotic(s) for UTI or any other coexisting infection; had received systemic antibiotics containing activity against the bacteria causing APN or cUTI within three days prior to administration of study antibiotics, except those who had treatment failure; use of any study antibiotics within 4 weeks prior to administration of study antibiotics; documented or suspected human immunodeficiency virus infection; and/or severe heart, hepatic, or renal diseases.
Interventions
Patients were assigned to the STFX group or the CTRX plus CFDN group at a 1:1 ratio according to a simple randomization procedure. Patients in the STFX group received oral STFX (Gracevit®; Daiichi-Sankyo, Tokyo, Japan) 100 mg (two 50 mg tablets) twice a day for 7–14 days. Those in the CTRX/CFDN group received intravenous CTRX (Rocephin®; Roche, Basel, Switzerland) 2 g once a day for 2–3 days, followed by oral CFDN (Omnicef®; Pfizer, New York, NY, USA) 100 mg every 8 hours for an additional 4–12 days. The overall treatment duration of study antibiotics was at least 7–14 days depending on patient response to treatment.
Patient assessment
Patients with cUTI required at least 5 days of hospitalization. Each patient was assessed for clinical response and adverse events (AEs) during the study (4–5 days after enrollment), at the end of treatment (1–2 days after the last dose of study antibiotics), and at the end of the study (4–10 days after the end of treatment). A telephone follow-up was also performed at the test of cure (21–28 days after the end of treatment). Urine culture was performed in each patient at study enrollment, the end of treatment if the urine culture result at study enrollment was positive or when clinically indicated, and at the end of the study if the urine culture result at the end of treatment was positive or if the patient had relapse of symptoms suggestive of UTI. Blood culture was performed when clinically indicated according to the discretion of the attending physician.
The primary outcome was the clinical success rate at the end of treatment. Clinical success was defined as: 1) cure of infection (ie, resolution of the symptoms and signs of APN or cUTI that presented at study entry, no new symptoms or signs related to APN or cUTI, and no requirement for additional antimicrobial therapy); or 2) improvement of infection (ie, incomplete resolution of symptoms and signs that presented at study entry and no requirement for additional antimicrobial therapy during the study). The secondary outcomes were as follows: 1) clinical success rate at the end of the study and at the test of cure; 2) clinical cure rate at the end of treatment, the end of the study, and at the test of cure; 3) early treatment failure during therapy; 4) microbiological success rate at the end of treatment and at the end of the study; 5) clinical relapse rate at the end of the study and at the test of cure; 6) microbiological relapse rate at the end of the study; and 7) antibiotic resistance rate of new bacteria isolated from a patient during the study period.
Microbiological success was defined as reduction in the uropathogen(s) recovered from urine at study entry to <10,000 cfu/mL or the presumed absence of the uropathogen(s) recovered at study entry due to substantial clinical improvement and a urine sample was not available or cultured. Clinical relapse was defined as reappearance of symptoms/signs at the end of the study and at the test of cure. Microbiological relapse was defined as recurrence of the original uropathogen(s) ≥10,000 cfu/mL at the end of study.
Each patient was assessed for safety by one of the study investigators at each follow-up visit from study enrollment to the test of cure. AE was defined as any untoward medical occurrence in a patient that does not necessarily have a causal relationship with the study antibiotics. Serious adverse event (SAE) was defined as any untoward medical occurrence that results in death; that is life-threatening and requires hospitalization or that causes prolongation of existing hospitalization; that results in persistent or significant disability/incapacity; that is a congenital anomaly/birth defect; or that requires intervention to prevent permanent impairment or damage. Patients who developed AE and/or SAE were followed until resolution of the event or until the event was considered stable.
Sample size calculation
Postmarketing data from the manufacturer of STFX relative to the treatment outcomes of 3,225 patients with UTI revealed clinical success rates of 87.7%–94.2% (data on file at Daiichi Sankyo, Tokyo, Japan). For this study, we predicted a lower clinical success rate in UTI using STFX compared to other reported rates of clinical success, since we enrolled patients with more complex conditions such as obstructive uropathy. Assuming a clinical success rate for the treatment of APN and cUTI with STFX of 84%, which was noninferior to that of CTRX/CFDN treatment under the noninferiority margin of 15%, according to draft guidance of the US Food and Drug Administration, a one-sided significance level of 2.5% and power of 80%, the minimum study population was calculated to be 182 patients. An increase to compensate for an estimated 30% withdrawal rate for any reason increased the minimum study population to 260 patients.
Statistical methods
SPSS Statistics version 16.0 (SPSS, Inc., Chicago, IL, USA) was used to perform all data analyses. Patients who received at least one dose of study antibiotics and who had postbaseline assessment up to 4–5 days were included in the intent-to-treat (ITT) analysis. Patients who were in full compliance with the study protocol up to the test of cure follow-up were included in the per-protocol (PP) analysis. Treatment efficacy analysis was performed in both the ITT and PP patient populations. Patients who received at least one dose of study antibiotics were assessed for safety of study antibiotics. Normally distributed continuous variables were compared between groups using the two-sided Student’s t-test, and those data are presented as mean ± SD. Nonnormally distributed continuous variable were compared between groups using the Wilcoxon rank-sum test, and those data are presented as median and IQR. Categorical variables are presented as frequency and percentage, and they were compared between groups using chi-squared test or Fisher’s exact test. z-Test was used to test for noninferiority of the primary outcome between the STFX group and the CTRX/CFDN group. All statistical analyses were two-sided, and a P-value of <0.05 was regarded as being statistically significant.
Results
Flow of study patients
The flow of study patients is shown in Figure 1. Of the 305 patients who were enrolled in this study, 150 were randomized to the STFX group and 155 were allocated to the CTRX/CFDN group. Sixteen patients (9 in the STFX group and 7 in the CTRX/CFDN group) were excluded (Figure 1). The remaining 289 patients (141 in the STFX group and 148 in the CTRX/CFDN group) were included in the ITT analysis. Seventy-eight patients (33 in the STFX group and 45 in the CTRX/CFDN group) were further excluded. The remaining 211 patients (108 in the STFX group and 103 in the CTRX/CFDN group) were included in the PP analysis.
  | Figure 1 Diagram describing the flow of patients from enrollment to ITT and PP analysis. Abbreviations: CFDN, cefdinir; CTRX, ceftriaxone; ITT, intent-to-treat; PP, per-protocol; STFX, sitafloxacin. |
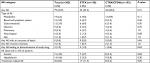
Patient demographics and baseline characteristics
The baseline characteristics of 289 enrolled patients are summarized in Table 1. The mean age of patients was 43.3 years, and the vast majority of them were female (90.3%). One hundred and two (72.3%) patients in the STFX group and 112 (75.7%) patients in the CTRX/CFDN group had APN. Thirty-nine (27.7%) patients in the STFX group and 36 (24.3%) patients in the CTRX/CFDN group had cUTI. The two most common comorbidities among patients with cUTI were DM and obstructive uropathy. There was no significant difference in demographics, types of infection, or complicating comorbidities between the two study groups.
Microbiological baseline data
Microbiological baseline data are shown in Table 2. One hundred and ninety (65.7%) patients had positive urine culture (68.8% in the STFX group and 62.8% in the CTRX/CFDN group). E. coli was the most frequently isolated bacteria, followed by K. pneumoniae and P. mirabilis. ESBL-producing Gram-negative bacteria were identified in 27 (24.5%) isolates of all Gram-negative isolates, and 24 (88.9%) of those were E. coli. The prevalence of ESBL producers among E. coli isolates was higher in the STFX group (18.6%) than in the CTRX/CFDN group (6.5%). Among 24 isolates of ESBL-producing E. coli, only one (4.2%) isolate was resistant to STFX. K. pneumoniae was isolated more often in the CTRX/CFDN group (7.5%) than in the STFX group (0.0%). Seventeen (5.9%) bacterial isolates were STFX-resistant (nine in the STFX group and eight in the CTRX/CFDN group). CTRX resistance was identified in 31 (10.7%) isolates. CTRX resistance was higher in the STFX group (16.3%) than in the CTFX/CFDN group (5.4%). CFDN resistance was identified in 35 (12.1%) isolates. CFDN resistance was higher in the STFX group (15.6%) than in the CTRX/CFDN group (8.8%). Twenty-seven (9.3%) isolates were resistant to both CTRX and CFDN. Combined CTRX and CFDN resistance was higher in the STFX group (13.4%) than in the CTRX/CFDN group (5.4%). Concomitant bacteremia was observed in 17.3% of patients, and only 3 of those had ESBL-producing E. coli bacteremia.
Duration of study antibiotics
The median (IQR) duration of antibiotic treatment in the STFX group was 10 days (IQR: 1, 14). In the CTRX/CFDN group, the median duration of CTRX and CFDN was 3 days (IQR: 1, 6) and 7 days (IQR: 1, 23), respectively.
Treatment efficacy
Primary outcome
The clinical success rates of patients in the STFX group and the CTRX/CFDN group at the end of treatment, and the results of noninferiority testing are shown in Table 3. For the ITT analysis, 86.6% of patients in the STFX group and 83.8% of patients in the CTRX/CFDN group achieved clinical success, with an absolute difference between groups of 2.8% (95% CI: –4.2% to 9.7%) in favor of the STFX regimen. The PP analysis revealed that 97.2% of patients in the STFX group and 99.0% of patients in the CTRX/CFDN group achieved clinical success, with an absolute difference of 1.8% (95% CI: –5.9% to 1.9%) in favor of the CTRX/CFDN protocol. The clinical success rate of patients with APN or cUTI in the STFX group was comparable to that of patients in the CTRX/CFDN group. The test for noninferiority revealed that the primary outcomes of patients in the STFX group were noninferior to those of the CTRX/CFDN group for both the ITT analysis and the PP analysis (P<0.025). The median time from study enrollment to clinical success at the end of treatment of the patients in both groups was 5 days for ITT and PP analyses.
Secondary outcomes
Secondary outcome data are shown in Table 4. The rates of all secondary outcomes were comparable between the STFX group and the CTRX/CFDN group.
Treatment safety
The incidence rates of various AEs that developed in both groups are shown in Table 5. At least one AE occurred in 23.3% and 28.4% of patients in the STFX group and the CTRX/CFDN group, respectively. The frequency and distribution of AEs were generally similar between groups, and most AEs were mild to moderate in severity. Only anemia and hypokalemia occurred in more than 5% of patients. AEs related to treatment were more frequent in the STFX group (11.3%) than in the CTRX/CFDN group (5.2%). AEs that resulted in discontinuation of study antibiotics were observed in only three patients (two in the STFX group and one in the CTRX/CFDN group). No phototoxicity or SAEs were observed in any study patients in either group.
Discussion
We selected STFX for comparison with parenteral CTRX followed by oral CFDN for therapy of APN and cUTI, because STFX is very active against Gram-negative bacteria that cause UTI, including isolates that are resistant to ciprofloxacin, levofloxacin, and cephalosporins. Consistent with the aforementioned, the rate of STFX resistance among the bacteria isolated from patients in this study was much lower than CTRX resistance and/or CFDN resistance, as shown in Table 2. Moreover, the fact that STFX is an oral antibiotic means that it is more convenient for the patient and less resource intensive for health care providers than parenteral CTRX. We used a dosage of 100 mg of STFX two times per day based on the results of a previous clinical trial that compared STFX 50 mg twice daily with STFX 100 mg twice daily for the treatment of cUTIs.13 The clinical efficacy of both regimens was similar; however, the microbiological eradication rate was slightly higher in the 100 mg twice daily group than in the 50 mg twice daily group.13
The efficacy of STFX for the treatment of patients with APN and cUTI was comparable to that of the CTRX/CFDN regimen, with absolute differences in clinical cure rates between treatment regimens of only 2.8% in ITT analysis and 1.8% in PP analysis. The CIs of the aforementioned differences in clinical cure rates were within 15% of the noninferiority margin. Noninferiority testing revealed the primary outcomes of patients in the STFX group to be noninferior to those of the patients in the CTRX/CFDN group for both ITT and PP analyses. The efficacy of STFX for the treatment of APN and cUTI observed in this study confirm the results of a small descriptive study in Thai patients who found oral STFX to be very effective for therapy of APN and cUTI.14 STFX was well-tolerated in this study, and the incidence of AEs was comparable between the two drug regimen groups. All observed AEs were mild to moderate in severity and they were all reversible. Although a previous study reported association between high-dose STFX and cutaneous phototoxicity in Caucasians,15 neither phototoxicity nor SAEs was observed in patients who received STFX in the present study. These findings support the safety of using a higher dose of STFX in Asian patients.
There are several oral antibiotics in addition to STFX that are active against Gram-negative bacteria that cause UTI (including ESBL-producing E. coli), such as fosfomycin and nitrofurantoin. However, these oral antibiotics are not indicated for the treatment of upper UTI due to inadequate drug concentrations in the bloodstream.16 STFX is, therefore, the most appropriate treatment option for the therapy of APN and cUTI caused by ESBL-producing E. coli, because other potential oral antibiotics, such as oral carbapenems, are not yet available in Thailand. In addition to using STFX for an entire course of treatment in APN and cUTI, STFX can also be used as a switch therapy after a patient with severe APN or cUTI has received carbapenem for few days. A small randomized controlled trial of STFX as a switch therapy after treatment with ertapenem for several days for APN caused by ESBL-producing E. coli revealed similar outcomes between the group that received ertapenem only and the group that received ertapenem followed by STFX.17 Using STFX instead of carbapenems for therapy of UTI caused by ESBL-producing Gram-negative bacteria, including carbapenem-resistant Enterobacteriaceae (CRE), may have less impact on inducing multidrug resistance in the causative bacteria and microbiomes of the patients, since carbapenems seem to be a strong risk factor associated with the development of CRE.18
Limitations
This study has some mentionable limitations. First, this study’s open-label design is susceptible to bias since the investigators were aware of the antibiotic regimen that each patient received. Second, the random allocation of patients was not stratified according to APN and cUTI. Third, urine cultures were positive in only about two-thirds of patients. Fourth, 27% of the ITT population was excluded from the PP analysis. Fifth and last, the results of this study should not be considered generalizable to pregnant women and patients with long-term indwelling urinary catheter since neither of these two subgroups were included in our study population.
Conclusion
Oral STFX was found to be noninferior to intravenous CTRX followed by oral CFDN in adult patients with APN and cUTI. Lower rates of resistance compared to CTRX and/or CFDN and oral administration suggest STFX as a more attractive treatment option in this patient population.
Data sharing statement
The information collected for each participating patient is available upon request.
Acknowledgment
The authors gratefully acknowledge Mr Suthipol Udompanthurak of the Division of Clinical Epidemiology, Department of Research and Development, Faculty of Medicine Siriraj Hospital, Mahidol University for assistance with statistical analysis. The study was supported by Daiichi-Sankyo (Thailand) Ltd. The funding agency was not involved in the execution of the study, the analysis of the collected data, or the preparation of the manuscript.
Author contributions
All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Stamm WE, Norrby SR. Urinary tract infections: disease panorama and challenges. J Infect Dis. 2001;183(Suppl 1):S1–S4. | ||
Flores-Mireles AL, Walker JN, Caparon M, Hultgren SJ. Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nat Rev Microbiol. 2015;13(5):269–284. | ||
Chenoweth CE, Gould CV, Saint S. Diagnosis, management, and prevention of catheter-associated urinary tract infections. Infect Dis Clin North Am. 2014;28(1):105–119. | ||
Gupta K, Hooton TM, Naber KG, et al. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: a 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis. 2011;52(5):e103–e120. | ||
World Health Organization. Antimicrobial resistance: global report on surveillance. 2014. Available from: http://www.who.int/drugresistance/documents/surveillancereport/en/. Accessed October 25, 2014. | ||
National Antimicrobial Resistance Surveillance, Thailand (NARST). Percentage of Susceptible Organisms Isolated from Urine, 44 hospitals, Jan–Sep 2017. Available from: http://narst.dmsc.moph.go.th/antibiograms/2017/9/Jan-Sep2017-Urine.pdf. Accessed June 5, 2018. | ||
Anderson DL. Sitafloxacin hydrate for bacterial infections. Drugs Today. 2008;44(7):489–501. | ||
Yamaguchi K, Ohno A, Ishii Y, et al. In vitro susceptibilities to levofloxacin and various antibacterial agents of 12,919 clinical isolates obtained from 72 centers in 2007. Jpn J Antibiot. 2009;62(4):346–370. | ||
Tiengrim S, Phiboonbanakit D, Thunyaharn S, et al. Comparative in vitro activity of sitafloxacin against bacteria isolated from Thai patients with urinary tract infections and lower respiratory tract infections. J Med Assoc Thai. 2012;95 Suppl 2(Suppl 2):S6–S17. | ||
Tiengrim S, Mootsikapun P, Wonglakorn L, et al. Comparative in vitro activity of sitafloxacin against bacteria isolated from Thai patients with urinary tract infections and lower respiratory tract infections in 2016. J Med Assoc Thai. 2017;100(10):1061–1072. | ||
Nakashima M, Uematsu T, Kosuge K, Umemura K, Hakusui H, Tanaka M. Pharmacokinetics and tolerance of DU-6859a, a new fluoroquinolone, after single and multiple oral doses in healthy volunteers. Antimicrob Agents Chemother. 1995;39(1):170–174. | ||
Kawada Y, Ishihara S, Matsui T, et al. Comparative study on sitafloxacin and levofloxacin in complicated urinary tract infections. Jpn J Chemother. 2008;56:81–91. | ||
Kawada Y, Yasuda M, Tanaka K. Dose-comparative study of sitafloxacin in complicated urinary tract infections. Jpn J Chemother. 2008;56:92–102. | ||
Manosuthi W, Wiboonchutikul S. Treatment outcomes of oral sitafloxacin in acute complicated urinary tract infection and pyelonephritis. Springerplus. 2016;5:410. | ||
Dawe RS, Ibbotson SH, Sanderson JB, Thomson EM, Ferguson J. A randomized controlled trial (volunteer study) of sitafloxacin, enoxacin, levofloxacin and sparfloxacin phototoxicity. Br J Dermatol. 2003;149(6):1232–1241. | ||
Auer S, Wojna A, Hell M. Oral treatment options for ambulatory patients with urinary tract infections caused by extended-spectrum-beta-lactamase-producing Escherichia coli. Antimicrob Agents Chemother. 2010;54(9):4006–4008. | ||
Malaisri C, Phuphuakrat A, Wibulpolprasert A, Santanirand P, Kiertiburanakul S. A randomized controlled trial of sitafloxacin vs. ertapenem as a switch therapy after treatment for acute pyelonephritis caused by extended-spectrum β-lactamase-producing Escherichia coli: a pilot study. J Infect Chemother. 2017;23(8):556–562. | ||
van Loon K, Voor In ‘t Holt AF, Vos MC. A systematic review and meta-analyses of the clinical epidemiology of carbapenem-resistant Enterobacteriaceae. Antimicrob Agents Chemother. 2018;62(1):e01730-17. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.