Back to Journals » Patient Related Outcome Measures » Volume 11
Oral Health Screening Status of Diabetes Patients in Selected Hospitals of Addis Ababa, Ethiopia, 2018
Authors Sahile AT , Mgutshini T, Ayehu SM
Received 25 June 2020
Accepted for publication 21 August 2020
Published 18 September 2020 Volume 2020:11 Pages 173—180
DOI https://doi.org/10.2147/PROM.S269292
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Robert Howland
Addisu Tadesse Sahile,1 Tennyson Mgutshini,2 Solomon Muluken Ayehu3
1Department of Public Health, Unity University, Addis Ababa, Ethiopia; 2Department of Public Health, University of South Africa, Pretoria, South Africa; 3Department of Emergency, Menelik II Referral Hospital, Addis Ababa, Ethiopia
Correspondence: Addisu Tadesse Sahile Tel +2519 1209 6667
Email [email protected]
Objective: The study assessed the oral health screening status of diabetes patients and its associated factors in selected public hospitals of Addis Ababa, 2018.
Patients and Methods: An institutional-based cross-sectional study was conducted on 388 diabetes patients selected on the bases of a systematic random sampling method from March to May 2018 at two selected public hospitals in Addis Ababa. Data were collected with a pre-tested, structured, and translated questionnaire. Bi-variable and multivariable logistics regression were undertaken to identify predictors of oral health screening among diabetes with their respective 95% CI and a p-value of less than 5% level of significance.
Results: The oral health screening status among diabetes patients in this study was 21.1%. The odds of having had an oral health screening was 82.4% higher in those with an educational status of college and above than those who cannot read and write and it was ten and five folds higher in participants with a monthly income of less than 750 birr than those with above 2,000 birr and those who brushed their tooth twice or more times a day than occasionally, respectively. The odds of having had an oral health screening was 17, four, and five folds higher among participants with perceived susceptibility, perceived severity, and benefit, respectively, whilst it was 8.8% lower in participants with a perceived barrier and it was as high as 19.782 times among participants with malocclusion.
Conclusion: A lower level of oral health screening was observed. A higher educational level, a lower monthly income, a higher frequency of tooth brushing per day, positive perceptions of susceptibility, severity, and benefits, and presence of malocclusions were statistically associated with a higher frequency of oral health screening. Concerned bodies were recommended to work on the identified predictors and improve the oral health screening of diabetes patients.
Keywords: oral health screening, diabetes patients, associated factors
Introduction
Globally 4.6 million deaths attributed to diabetes mellitus (DM) occurr annually.1 About 366 million people had DM, most ) of which were type 2 DM (90%)2 and found in low- and middle-income countries.3 By the year 1994, the Center for Disease Control and Preventions (CDC) declared DM as an epidemic in the US.4 Periodontal disease and DM share common risk factors and bidirectional relationships.3,5
The global burden of oral disease is predominantly periodontal disease, ranging from 20–50%6 and is the most common complication of diabetes.7 The estimated prevalence of diabetes in Ethiopia ranges from 2–5% nationally.8 Evidence suggests that its prevalence could be greater than 5% in people older than 40 years of age.9
There was a positive link between diabetes status and undertaking oral health screening.10 As the attitude of diabetes patients about oral health problems affects their oral health screening status,11 raising awareness about oral health care had a pivotal role in the improvement of the daily practice of oral health care.12
Though DM was associated with poor oral health status,13 it was evidenced that only a few proportions of DM patients were aware of their increased risk of periodontal disease,14 and hence very few utilized oral health care. Some of the reasons for lower oral health care utilization among diabetes were the perceived lack of necessity for a dental check-up, and the perception that dental problems were not serious.10
A higher cost of dental care, lower awareness among diabetes patients about oral health care, cost of transportation, and dental fears were among factors affecting oral health screening of diabetes patients.15,16
To the best of our knowledge there was a shortage of published works in Ethiopia which primarily focused on the oral health screening status of diabetes patients and its associated factors in Addis Ababa, this study was planned to assess the oral health screening status of diabetes patients and its associated factors in selected hospitals of Addis Ababa, Ethiopia, and would hopefully fill the existing gap in the literature.
Methods
Participants and Study Design
An institution-based cross-sectional study was undertaken on 388 participants at the two conveniently selected hospitals from March to May 2018. The study received ethical approval from the University of South Africa Research review ethics committee and Addis Ababa Health Bureau research and Ethics office then conducted at Menelik II Referral Hospital and Zewditu Memorial Hospital. All participants were provided written informed consent. The source population was all diabetes patients within the catchment area of the two conveniently selected Hospitals. The study population included 388 diabetes patients who were available during the data collection period at the study settings. The sample was determined based on a single population proportion with the premises of the proportion of oral health screening status to be 50%, where the final sample size was 403, inclusive of a 5% non-response rate. Diabetes participants who were on follow-up at diabetes clinics during the study period, not-admitted, not with severe complication were included in the study. Participants were selected on the bases of systematic random sampling methods with the sampling interval of K=8. The sampling frame was a medical record number of diabetes patients in both selected hospitals (N=1680 for Menelik II Hospital and N=1513 for Zewditu Memorial Hospital per three months). Data were collected with a pre-tested interviewer-administered questionnaire where a pre-test was conducted on 5% of cases at Yekatit 12 Hospital Medical College two weeks before actual the data collection period. The questionnaire was first developed by the investigators after rigorous review of literatures17–22 then given to senior researchers, and dentists for the incorporation of their inputs. Data collection was performed by five nurses after trained for two days; after which training was given by the researcher.
For this study, the outcome variable (oral health screening status) was measured as ‘yes’ or “no,” whether the diabetes patients have visited a dentist every six months or twice a year, considered as “yes” otherwise “no” as per the recommendation of CDC.23 The health belief model in line with other factors was used to identify factors affecting oral health screening.
Statistical Analysis
Descriptive statistics were used for the summarization of data. With an inter-item reliability coefficient for the health belief model constructs of perceived susceptibility, perceived severity, perceived benefits, and perceived barriers; 0.705, 0.731, 0.857, and 0.899 respectively. For the identification predictors of oral health screening, binary (bi-variable and multivariable) logistics regression was used, with their respective 95% Confidence Interval (CI) and p-value of less than 0.05 as statistically significant level.
Results
Socio-Demographic Characteristics of Participants
A total of 388 participants were enrolled in the study with a response rate of 96.3%. More than half (52.1%) of respondents were female. The mean age of participants was 52.27 years with a standard deviation of 14.797. Two hundred sixty-four (68%) of the respondents were married (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Respondents at Selected Public Hospitals in Addis Ababa, Ethiopia, May 2018 (n=388) |
Behavioral and Physical Measurements
Most (71%) of participants were type 2 diabetes patients, where most (60%) took injection and 80% of the participants had a current fasting blood glucose level of 126 g/dl and more. Most (64.4%) of respondents had no family history of DM (Table 2).
 |
Table 2 Behavioral and Physical Characteristics of Diabetes Participants at Selected Public Hospitals in Addis Ababa, Ethiopia, May 2018 (n=388) |
Perceptions of Oral Health
Less than one fifth (18.8%) of participants agreed that a person with diabetes has a higher risk of getting periodontal disease, and 25.5% of participants perceived that periodontal disease can result in heart disease. Most (64%) of participants believed complications of periodontal disease are dangerous whereas more than half (53%) of respondents perceived that oral health screening had benefits for the prevention and control of periodontal disease.
Less than one third (31.4%) of respondents agreed that there was a long waiting time to have oral health check-ups and 26.8% agreed that the long distance between diabetes clinic and dental clinic prevented them from having oral health screening.(Table 3)
 |
Table 3 Perception of Diabetes Participants at Selected Public Hospitals in Addis Ababa, Ethiopia, May 2018 (n=388) |
Oral Health Screening and its Predictors
The oral health screening level in this study was 21.1% (95% CI: 17.2–25.5%), whereas, the majority (78.9%) had less than two oral health screens per year (Figure 1).
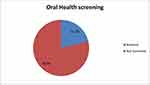 |
Figure 1 Oral health screening status of diabetes participants at selected public hospitals in Addis Ababa, Ethiopia, May 2018 (n=388). |
Marital status, perception of susceptibility, severity, benefit and barriers were independently associated with oral health screening at p<0.05.
The odds of having had an oral health screening was as higher as 82.4% in participants with an educational level of college and above, compared to those who cannot read and write (AOR: 0.176, 95CI: 0.035–0.892, P<0.05).
The odds of having had an oral health screening was ten fold higher among participants with a monthly salary of fewer than 750 birr against those with a monthly salary of 2,000 birr and more (AOR: 9.847, 95% CI:1.878–51.644, P<0.001). Possibly, this might happen due to an increase in income may lead to tightness with duties to have the follow up regularly.
The odds of having had an oral health screening was five times higher in those who brush their teeth at least twice a day compared to those who brush occasionally (AOR: 5.070, 95% CI:1.117–23.016, P<0.05).
The odds of having had oral health screening was 17.272, and 4.070 times higher in people with perceived susceptibility to, and severity of periodontal disease (AOR: 17.272, 95% CI: 4.161–71.705, P<0.001) and (AOR: 4.070, 95% CI:1.371–12.083, P<0.05) respectively.
The odds of having had an oral health screening was 4.75 times higher in participants with perceived benefits that taking preventive actions can prevent oral health problems (AOR: 4.751, 95% CI: 1.666–13.550, P<0.05).
The odds of having had an oral health screen was lower in participants with barrier perceptions (AOR: 0.088, 95% CI: 0.033–0.231, P<0.001) and the odds of having had an oral health screening was as high as 20 times among participants with malocclusion than their counterparts (AOR: 19.782, 95% CI: 6.387–61.270, P<0.001) (Table 4).
 |
Table 4 Predictors of Oral Health Screening of Diabetes Participants at Selected Public Hospitals in Addis Ababa, May 2018 (n=388) |
Discussion
In this study, one-fifth of diabetes patients reported having had two or more oral health screenings per year. Which was lower than the findings; 55% in France,24 79% in England,25 58.6% in the US,17 63.8% in Brazil,20 and 85.1% in Sweden.26 These differences might be due to the lower oral health care coverage, and awareness in Ethiopia.
One-third (33%) of diabetes patients were aware of their increased risk for periodontal disease,14 which was almost consistent with the current study. The oral health screening status in this study was almost consistent with the findings; 27% in India,22 17% and 33.3% in Malaysia, during 2016 and 2012.10,27
In this study, the level of oral health screening was higher than the findings; 12.6% and 15.1% in Saudi Arabia,28,29 and 10% in Jordan.30 This difference might be due to variations in types of population demographics and study time.
In this study, being in education, college-level and above, was associated with more oral health screening than those who cannot read and write, which was supported by a study in Nigeria which stated; a higher educational status was associated with more frequency of oral screening than their counterparts.31
In this study, the presence of malocclusion was statistically associated with higher oral health screening status, but not well investigated in other studies. In this study, tooth brushing at least twice per day was associated with a higher oral health screening status than occasional tooth brushing, and was supported by a study in India that stated a higher frequency of tooth brushing was associated with a higher frequency of dental visits.32
The more diabetes patients know about oral health problems, the more they visit dental clinics,33 but in this study knowledge of diabetes patients did not show an association with oral health screening. This might be due to variability in the application and use of available information regarding oral health in diabetes patients.
A low level of knowledge about dental problems, fear of having treatment, and financial issues were associated with lower oral health screening status.16 Whilst diabetes patients with perceived susceptibility, severity, and benefits of undertaking oral health preventive measures had a higher oral health screening experience than their counterparts.
Conclusion and Recommendation
In this study, a lower level of oral health screening was observed. A higher educational level (college and above), a lower monthly income (less than 750birr), a higher (two or more) frequency of tooth brushing per day, positive perceptions of susceptibility, severity, and benefits, and presence of malocclusions were statistically significantly associated with a higher frequency of oral health screening in the study settings. Whereas the presence of a perceived barrier was statistically significantly associated with a lower frequency of an oral health screening. Researchers were recommended to undertake a large scale community-based study. Policymakers and health professionals were also recommended to work jointly to enhance the oral health screening of diabetes patients in the study settings.
Consent for Publication
Consent for publication of the manuscript was not applicable due to the fact that there were no participant’s individual data videos or images.
Abbreviations
AOR, Adjusted Odds Ratio; CDC, Center for Disease Control; DM, Diabetes Mellitus; WHO, World Health Organization.
Data Sharing Statement
A finding of this study was generated from the data collected and analyzed on the basis of stated methods and materials hence all data were already available in the manuscript.
Ethics Approval and Consent to Participate
The study protocol was performed in accordance with the ethical principle. Ethical approval was obtained from ethics review board of the University of South Africa. The ethics approval was given in accordance with the Declaration of Helsinki. The data collectors obtained written informed consent from all participants.
Acknowledgments
The authors would like to thank the University of South Africa for the facilitation of the study. The authors would also thank study participants for their willingness in taking part in the study. Finally, the researchers would like to express their gratitude for the data collectors.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
The authors received no specific funding for this work.
Disclosure
The authors report no conflicts of interest for this work.
References
1. Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94(3):311–321. doi:10.1016/j.diabres.2011.10.029
2. Diabetes UK. Diabetes in the UK 2010: Key Statistics on Diabetes. London: Diabetes UK; 2010.
3. Taylor GW. Bidirectional interrelationships between diabetes and periodontal diseases: an epidemiologic perspective. Ann Periodontol. 2001;6(1):99–112. doi:10.1902/annals.2001.6.1.99
4. Smyth S, Heron A. Diabetes and obesity: the twin epidemics. Nat Med. 2006;12(1):75–80. doi:10.1038/nm0106-75
5. Preshaw P, Alba A, Herrera D, et al. Periodontitis and diabetes: a two-way relationship. Diabetologia. 2012;55(1):21–31. doi:10.1007/s00125-011-2342-y
6. Nazir MA. Prevalence of periodontal disease, its association with systemic diseases and prevention. Int J Health Sci. 2017;11(2):72.
7. Saini R, Saini S, Sugandha R. Periodontal disease: the sixth complication of diabetes. J Family Community Med. 2011;18(1):31. doi:10.4103/1319-1683.78636
8. Megerssa Y, Gebre M, Birru S, Goshu A, Tesfaye D. Prevalence of undiagnosed diabetes mellitus and its risk factors in selected institutions at Bishoftu Town, East Shoa, Ethiopia. J Diabetes Metab. 2013;S12:008.
9. Abebe SM, Berhane Y, Worku A, Assefa A. Diabetes mellitus in North West Ethiopia: a community based study. BMC Public Health. 2014;14(1):97. doi:10.1186/1471-2458-14-97
10. Sahril N, Aris T, Asari A, et al. Oral health seeking behaviour among Malaysians with type II diabetes. J Public Health Aspects. 2014;1(1):1–8. doi:10.7243/2055-7205-1-1
11. Poudel P, Griffiths R, Wong VW, et al. Oral health knowledge, attitudes and care practices of people with diabetes: a systematic review. BMC Public Health. 2018;18(1):577. doi:10.1186/s12889-018-5485-7
12. Mirza KM, Khan AA, Ali MM, Chaudhry S. Oral health knowledge, attitude, and practices and sources of information for diabetic patients in Lahore, Pakistan. Diabetes Care. 2007;30(12):3046–3047. doi:10.2337/dc07-0502
13. Jansson H, Lindholm E, Lindh C, Groop L, Bratthall G. Type 2 diabetes and risk for periodontal disease: a role for dental health awareness. J Clin Periodontol. 2006;33(6):408–414. doi:10.1111/j.1600-051X.2006.00929.x
14. Allen E, Ziada H, O’halloran D, Clerehugh V, Allen P. Attitudes, awareness and oral health‐related quality of life in patients with diabetes. J Oral Rehabil. 2008;35(3):218–223. doi:10.1111/j.1365-2842.2007.01760.x
15. Moore PA, Orchard T, Guggenheimer J, Weyant RJ. Diabetes and oral health promotion: a survey of disease prevention behaviors. J Am Dent Assoc. 2000;131(9):1333–1341. doi:10.14219/jada.archive.2000.0388
16. Dodd VJ, Logan H, Brown CD, Calderon A, Catalanotto F. Perceptions of oral health, preventive care, and care‐seeking behaviors among rural adolescents. J Sch Health. 2014;84(12):802–809. doi:10.1111/josh.12215
17. Yuen HK, Wolf BJ, Bandyopadhyay D, Magruder KM, Salinas CF, London SD. Oral health knowledge and behavior among adults with diabetes. Diabetes Res Clin Pract. 2009;86(3):239–246. doi:10.1016/j.diabres.2009.09.010
18. Macek MD, Tomar SL. Dental care visits among dentate adults with diabetes and periodontitis. J Public Health Dent. 2009;69(4):284–289. doi:10.1111/j.1752-7325.2009.00136.x
19. Orlando VA, Johnson LR, Wilson AR, et al. Oral health knowledge and behaviors among adolescents with type 1 diabetes. Int J Dent. 2010;2010:1–8. doi:10.1155/2010/942124
20. Alves C, Brandão M, Andion J, Menezes R. Oral health knowledge and habits in children with type 1 diabetes mellitus. Braz Dent J. 2009;20(1):70–73. doi:10.1590/S0103-64402009000100012
21. Arunkumar S, Amur S, Sambrani U, Burde KM. Survey on awareness and knowledge about the effect of diabetes mellitus on systemic and oral health in patients visiting general medicine outpatient Department in Dental Hospital. J Krishna Inst Med Sci. 2015;4(2):100–106.
22. Kejriwal S, Bhandary R, Thomas B. Assessment of knowledge and attitude of diabetes mellitus type 2 patients about their oral health in Mangalore, India. Univ Res J Dent. 2014;4(1):44–47. doi:10.4103/2249-9725.127077
23. Control CfD. The Prevention and Treatment of Complications of Diabetes: A Guide for Primary Care Practitioners. Atlanta, GA: US Department of Health and Human Services; 1991.
24. Azogui‐Lévy S, Dray‐Spira R, Attal S, Hartemann A, Anagnostou F, Azerad J. Factors associated with oral health‐related quality of life in patients with diabetes. Aust Dent J. 2018;63(2):163–169. doi:10.1111/adj.12577
25. Bowyer V, Sutcliffe P, Ireland R, et al. Oral health awareness in adult patients with diabetes: a questionnaire study. Br Dent J. 2011;211(6):E12. doi:10.1038/sj.bdj.2011.769
26. Sandberg GE, Sundberg HE, Wikblad KF. A controlled study of oral self-care and self-perceived oral health in type 2 diabetic patients. Acta Odontol Scand. 2001;59(1):28–33. doi:10.1080/000163501300035742
27. Badiah B. A preliminary survey on awareness of periodontal risk and oral health practices among diabetic patients in hospital Kuala Lumpur. Malays Dent J. 2012;34(1).
28. Bahammam MA. Periodontal health and diabetes awareness among Saudi diabetes patients. Patient Prefer Adherence. 2015;9:225. doi:10.2147/PPA.S79543
29. Al Amassi BY, Al Dakheel RS. Oral hygiene practice of adult diabetic patients and their awareness about oral health problems related to diabetes. J Dent Oral Hyg. 2017;9(2):8–14. doi:10.5897/JDOH2017.0219
30. Al Habashneh R, Khader Y, Hammad MM, Almuradi M. Knowledge and awareness about diabetes and periodontal health among Jordanians. J Diabetes Complications. 2010;24(6):409–414. doi:10.1016/j.jdiacomp.2009.06.001
31. Taiwo JO, Moronke N. Pattern of dental clinic attendance of registered diabetic patients in Ibadan. 2006.
32. DeDonnoa MA. Dental anxiety, dental visits and oral hygiene practices. Oral Health Prev Dent. 2012;10(2).
33. Wiener RC, Shockey AT. Oral health knowledge and dental visits in community living older adults in rural Appalachia-West Virginia: a cross-sectional analysis. J Stud Soc Sci. 2014;8(1):1.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
