Back to Journals » OncoTargets and Therapy » Volume 12
Optimal postoperative adjuvant treatment strategy for HBV-related hepatocellular carcinoma with microvascular invasion: a propensity score analysis
Authors Wang L , Chen B , Li Z, Yao X , Liu M, Rong W, Wu F, Lin S, Liu Y, Zheng Y, Li Y, Wang W, Wu J
Received 6 July 2018
Accepted for publication 13 January 2019
Published 15 February 2019 Volume 2019:12 Pages 1237—1247
DOI https://doi.org/10.2147/OTT.S179247
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Yao Dai
Liming Wang,1,* Bo Chen,2,* Zhuo Li,3 Xuesong Yao,4 Mei Liu,5 Weiqi Rong,1 Fan Wu,1 Shengtao Lin,1 Yunhe Liu,1 Yiling Zheng,1 Yexiong Li,2 Weihu Wang,6 Jianxiong Wu1
1Department of Hepatobiliary Surgery, National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China; 2Department of Radiation Oncology, National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China; 3Department of Pathology, National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China; 4Department of Interventional Therapy, National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China; 5Laboratory of Cell and Molecular Biology & State Key Laboratory of Molecular Oncology, National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China; 6Department of Radiation Oncology, Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education/Beijing), Peking University Cancer Hospital & Institute, Beijing, China
*These authors contributed equally to this work
Background: Microvascular invasion (MVI) is the most important risk factor associated with early postoperative recurrence in patients with hepatocellular carcinoma (HCC). However, the efficacy of postoperative adjuvant treatment for preventing recurrence in HCC patients with MVI has not been assessed. This study investigated the efficacy of postoperative adjuvant radiotherapy (RT) and transcatheter arterial chemoembolization (TACE) in HCC patients with MVI.
Materials and methods: From July 2008 to December 2016, 117 hepatitis B virus (HBV)-related HCC patients with MVI were retrospectively divided into two groups based on postoperative adjuvant treatments. Propensity score matching (PSM) was performed to adjust for significant differences in baseline characteristics. Relapse-free survival (RFS) and overall survival (OS) of the two groups were analyzed before and after PSM.
Results: Of all patients, the RT group had significantly smaller tumor size and milder MVI classification. PSM analysis created 46 pairs of patients. After matching, the two groups of patients were similar in baseline characteristics. Multivariate analysis indicated that tumor size, MVI classification, and postoperative treatment strategies were independently associated with RFS; tumor size and MVI classification were independently associated with OS. Similar multivariate analysis results were demonstrated after matching propensity score. Survival analysis revealed that the estimated median RFS and OS of patients with RT and TACE were 25.74±8.12 vs 9.18±1.67 months (P=0.003) and 60.69±7.36 vs 36.53±5.34 months (P=0.262), respectively. The RT group had significantly longer RFS than the TACE group.
Conclusion: Postoperative adjuvant RT offers better RFS for HCC patients with MVI than TACE.
Keywords: hepatocellular carcinoma, microvascular invasion, radiotherapy, TACE, relapse-free survival
Introduction
Hepatocellular carcinoma (HCC) accounts for 745,000 deaths worldwide and is the second most common cause of cancer mortality.1 Liver resection (LR) is the best radical treatment and well perceived as a curative treatment for patients with HCC.2 However, the high cumulative 5-year postoperative recurrence rate of HCC in the remnant liver, which reaches an incidence of >70%,3 results in an unsatisfactory 5-year survival rate of <50%.4
Microvascular invasion (MVI), also known as intravascular cancer thrombus, is likely to develop in the branches of the portal vein.5 A recent study has shown that about 15%–57.1% of LRs include MVI.6 MVI may promote metastasis in the liver parenchyma by giving rise to micrometastases, thereby initiating the process.7 Its presence is definitely regarded as the most important risk factor that is significantly associated with early postoperative recurrence within 2 years8,9 and is repeatedly confirmed as a poor prognostic factor of long-term survival after R0 resection.6,10 MVI increases the rate of tumor recurrence and dramatically shortens long-term survival for patients with small HCC.2,10,11 As MVI can be confirmed only by postoperative histological examination, effective postoperative treatment becomes an essential requirement.
In the recent decades, numerous cohort investigations and clinical randomized controlled trials, including several approaches such as transcatheter arterial chemoembolization (TACE), radiotherapy (RT), or sorafenib, have been performed to prevent postoperative recurrence of HCC. It is worth mentioning that a few studies take MVI into consideration. A retrospective study showed that postoperative adjuvant TACE is safe in preventing tumor recurrence rate significantly (P=0.004) and can result in better survival outcomes for early or intermediate-stage HCC patients with MVI.12 TACE has also been shown to reduce early recurrence rate for HCC patients with MVI in a single-center retrospective trial.13 However, adjuvant RT following hepatectomy could efficiently prevent early recurrence and delay the progression of recurrent tumors, and thereby improve the relapse-free survival (RFS) (P=0.011) and overall survival (OS) (P=0.034) in HCC patients with MVI compared with TACE in a single-center retrospective study.14 Additionally, adjuvant RT was also found to be feasible and safe for centrally located HCCs.14,15 Thus, the mode of postoperative adjuvant treatment beneficial for HCC patients with MVI is still uncertain.
In order to address the issue, the present study aims to evaluate the impacts of postoperative adjuvant treatment (RT or TACE) on long-term survival outcomes after curative resection for patients with MVI. To minimize potential bias caused by patients’ backgrounds in a retrospective, nonrandomized cohort study, a propensity score matching (PSM) analysis was adopted to select subjects and to determine the survival benefit between two groups. The prognostic factors associated with survival were also investigated. This is the first study to compare RT and TACE as the postoperative adjuvant treatments for HCC patients with MVI on their long-term survival after PSM.
Materials and methods
Selection of patients
A total of 1,563 patients with HCC received hepatic resection at the Cancer Hospital, Chinese Academy of Medical Sciences, between July 2008 and December 2016. Among them, 117 patients were considered eligible for the study based on the following criteria: 1) primary HCC patients treated with curative surgical LR; 2) surgical margin was microscopically free of tumor; 3) MVI was proven by postoperative pathology but macrovascular invasion was absent; 4) there was no tumor fracture and hemorrhage before and during resection; 5) postoperative liver failure or severe complications/adverse events did not happen within 1 month; 6) absence of previous or simultaneous malignant tumor/diseases; 7) hepatitis B virus (HBV) infection was confirmed by serological detection; 8) preoperative liver function was Child–Pugh A degree; 9) RT or TACE was performed as postoperative adjuvant treatment; and 10) patients had continuous follow-up records until death or censored time. Patients’ informed consent was not required because of the retrospective nature of the study. The primary endpoint was RFS; the secondary endpoint was OS. RFS is increasingly being used as the reliable primary endpoint for cancer clinical trials due to a shorter event time. OS has been found to be extremely good in early stages of breast cancer but not in the later stages. However, for such reasons, OS is not the preferred practical endpoint. Therefore, RFS was chosen as the primary endpoint and OS as the secondary endpoint from the practical and clinical standpoint.16
This study was approved by Ethics Committee (Institutional Review Board) of Cancer Hospital, Chinese Academy of Medical Sciences. As a retrospective noninterventional study that does not interfere with diagnosis and treatment, the results of the study will be published as statistically analyzed data and do not contain any identifiable patient’s information. Thus, patients’ data confidentiality was protected properly and the study was done in accordance with the principles of the Declaration of Helsinki. The Ethics Committee waived the informed consent of all the patients in this study.
Pathologic review and clinical grouping
H&E stained microscopic sections from all the 117 patients were retrospectively collected and reviewed by professional pathologists from our center due to the lack of consensus in definition, grading and risk features of MVI.6,14 The pathological diagnosis and classification of MVI were identified according to the 2015 clinicopathological evidence-based practice guidelines for standardized pathological diagnosis of primary liver cancers in China.17 The classification of MVI is defined as follows: M1 (low risk): the number of MVI is ≤5 and the distance of MVI is ≤1 cm from the tumor capsule; M2 (high risk): the number of MVI is >5 or the distance of MVI is >1 cm from the tumor capsule.17
In all, 117 patients were divided into the following two groups according to postoperative treatments: 1) TACE group, which consisted of 71 patients treated with TACE within 2 months after surgery and 2) RT group, which consisted of 46 patients treated with three-dimensional conformal or intensity-modulated RT within 2 months after surgery. Nutritional therapy and anti-HBV therapy were performed as basic treatments in both groups.
Procedures of TACE and RT
Nutritional therapy and postoperative anti-HBV therapy were given to all the patients during a long time period as initial therapy to improve liver function, block the process of liver cirrhosis, and prevent recurrence.14 Arterial embolization was administered with Seldinger’s technique as the standard TACE procedure.18 Following identification of suspicious residual tumor stain, infusion of a mixture of 20–30 mg of doxorubicin (Adriamycin®) and 5–10 mL of lipiodol were performed after catheterization of the arteries supplying the area of tumor. Emulsion and 2- to 3-mm strips of Gelfoam were delivered sufficiently to the suspicious residual tumor area until complete flow stagnation was achieved. RT procedure included three-dimensional conformal or intensity-modulated RT plans. The clinical treatment volume included a tumor cutting bed expansion of 1 cm margin, and 0.51 cm was added to it for the final planning treatment volume. The target total dose of 54–60 Gy was delivered by 2 Gy/fraction with five fractions per week.
TACE could not find any invisible microlesion such as MVI. As MVI has been proved to be a high risk factor of recurrence due to high possibility of metastasis, the main purpose of TACE was not to identify any residual MVI but to find possible intrahepatic metastasis lesion that was not detected by preoperative imaging or intraoperative exploration. Unfortunately, reviewed digital subtraction angiography images of patients in the TACE group showed that a few patients have definite lesion stain during the TACE procedure. It means that the area of MVI cannot be clearly stained through arteriography. As a result, for the overwhelming majority of patients without definite residual tumor stain during the procedure of arteriography, TACE has been given to tumor bed area or suspicious area with under-stain in prophylaxis. Consequently, patients with MVI have more possibility of recurrence in the TACE group because definite elimination of micrometastasis foci could not be made by TACE.
Follow-up
All patients were followed-up quarterly in the first 2 years and at 6-month intervals thereafter, following discharge from the hospital. Alpha-fetoprotein (AFP), chest X-ray, enhanced computed tomography, liver function, and/or enhanced MRI were performed as the follow-up tests. The diagnosis of oncologic recurrence was depended on typical imaging findings and/or continually increased serum AFP. Histopathology or cytopathology evidence was assessed by biopsies but not necessarily for the assessment of recurrences.
The primary outcome measures were RFS and OS. RFS was defined as the time interval between the surgery date and the date of the first detection of recurrence or censored on the date of the last follow-up. OS was recorded as time period from the surgery date to death or censored on the date of the last follow-up. The last follow-up was in December 2017.
Further treatment for recurrence
The treatment strategy for recurrence of HCC was determined based on the comprehensive consideration of tumor characteristics, liver function, and general condition by a multidisciplinary team. Local or regional curative treatment consisting of reoperation-hepatectomy, radiofrequency ablation, and stereotactic body radiation therapy was undertaken for nodular recurrence. Systemic palliative treatment, such as TACE, molecular targeted therapy, and chemotherapy, was performed as the alternative method for diffuse recurrence.
Statistical and survival analyses
Continuous variable data that are normally distributed are expressed as the mean ± SD. Categorical variables data are expressed as N (proportion). Continuous variables were compared using independent samples t-test. Comparisons between categorical variables were performed using Pearson’s chi-squared test or Fisher’s exact test where appropriate.
Univariate and multivariate Cox proportional hazards regression analyses were performed on clinicopathological parameters to identify the independent prognostic factors to RFS and OS. For the multivariable regression model, only the variables that showed statistically significant association in univariate analysis were included as covariates in the multivariable analysis. The Wald test was used to calculate P-values. The Kaplan–Meier estimator was used to calculate the median survival time and the rates of survival (RFS and OS) and to describe the survival curve. A comparison of survival analysis was performed, and the P-value was calculated using the log-rank test.
IBM SPSS 22.0 (IBM Corporation, Armonk, NY, USA) software was used for the statistical analysis. P-values (two-tailed) <0.05 were regarded as statistically significant.
PSM analysis
It was a retrospective study wherein the postoperative treatment approach was based on the clinical condition of the patients as assessed by the physician which could have introduced potential selection bias. The potential confounders causing the selection bias between the RT and TACE groups include demographic variables, preoperative liver serological parameters, surgery characteristics, and tumor variables. Therefore, a PSM analysis was conducted to generate a matched pair of patients in an attempt to reduce bias in patient selection prior to comparing long-term survival between the RT and the TACE propensity score-matched groups. Possible variables associated with the selection of postoperative treatment and variables potentially affecting the survival outcomes were comprehensively selected for propensity score generation.19 A logistic regression model with the selected variables was employed to generate a continuous propensity score from 0 to 1, using baseline characteristics tumor size, MVI classification, preoperative AFP level, surgical margin as covariates and age, gender, operative procedure, operative method, tumor number, differentiation, envelope invasion, and cirrhosis as additional covariates in the model. Subsequently, a one-to-one match without replacement between the RT group and the TACE group was obtained by optimal matching with a caliper width of 0.2 without replacement in order to minimize the conditional bias.20
All statistical analyses were conducted with SPSS for Windows version 22, Propensity Score Matching for SPSS version 3.03, and R software version 2.15.1 (IBM Corporation).
Results
Demographic and clinicopathological characteristics of the study patients
Before PSM, a total of 117 patients (103 male patients and 14 female patients) with a mean age of 51.35±10.68 (range: 27–79) years were included in the analysis (TACE group, N=71; RT group, N=46). The baseline demographic and the clinicopathological characteristics of the two groups of patients are summarized and compared in Table 1. Most of the characteristics of the two groups were similar and comparable. There were no significant differences between the two groups in the following variables, including age, gender, operative time, operative procedure, operative method, blood loss, surgical margin, number of tumors, differentiation, envelope invasion, cirrhosis, viral hepatitis, preoperative serum AFP, alanine aminotransferase, total bilirubin, albumin, and prothrombin time. Patients in the TACE group had significantly bigger tumor size (P=0.048) and higher rate of M1 in MVI classification (P=0.005) than the RT groups.
After PSM, a total of 92 patients (80 male patients and 12 female patients) with a mean age of 51.25±10.92 (range: 27–79) years were included in the analysis (TACE group, N=46; RT group, N=46). The baseline demographic and the clinicopathological characteristics of the two groups of patients with MVI are summarized and compared in Table 1. All the characteristics of the two groups were similar and comparable.
Univariate and multivariable analyses for independent prognostic factors
Before PSM, according to univariate analysis, tumor size, MVI classification, envelope invasion, serum AFP level, and postoperative treatment strategies were the factors associated with worse RFS, whereas tumor size, MVI classification, envelope invasion, serum AFP level, and post operative treatment strategies were identified as factors that influenced OS. The multivariate Cox proportional hazard regression analysis revealed that tumor size (HR=1.083, 95% CI: 1.013–1.158, P=0.019), MVI classification (HR=3.525, 95% CI: 2.161–5.749, P<0.001), and postoperative treatment strategies (HR=0.509, 95% CI: 0.309–0.840, P=0.008) were the independent prognostic factors associated with RFS, and tumor size (HR=1.169, 95% CI: 1.076–1.269, P<0.001) and MVI classification (HR=3.151, 95% CI: 1.629–6.097, P=0.001) were the independent prognostic factors associated with OS (Table 2).
After matching for propensity score, according to univariate analysis, tumor size, MVI classification, envelope invasion, and postoperative treatment strategies were the factors associated with worse RFS, whereas tumor size, MVI classification, and envelope invasion were identified as factors that influenced OS. The multivariate Cox proportional hazard regression analysis revealed that tumor size (HR=1.104, 95% CI: 1.011–1.205, P=0.027), MVI classification (HR=4.533, 95% CI: 2.612–7.869, P<0.001), and postoperative treatment strategies (HR=0.447, 95% CI: 0.264–0.757, P=0.003) were the independent prognostic factors associated with RFS and tumor size (HR=1.175, 95% CI: 1.048–1.317, P=0.006), MVI classification (HR=5.083, 95% CI: 2.249–11.485, P<0.001), and serum AFP level (HR=1.704, 95% CI: 1.015–2.861, P=0.044) were the independent prognostic factors associated with OS (Table 3).
Survival analysis of the study patients
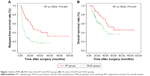
Before PSM, the cumulative 1-, 2-, and 3-year RFS rates of all 117 patients were 47.0%, 34.5%, and 27.8%, respectively, and the cumulative 1-, 2-, and 3-year OS rates of all 117 patients were 86.2%, 69.1%, and 58.5%, respectively. The median RFS times of the TACE group vs the RT group were 6.66±1.24 and 25.74±8.12 months, respectively. The 1-, 2-, and 3-year RFS rates were 31.0%, 20.1%, and 17.3% for patients in the TACE group, and 71.7%, 56.2%, and 44.0% for patients in the RT group, respectively. The RT group showed a significantly longer RFS than the TACE group (P<0.001). All of the above data are shown in Figure 1A. Median OS times of the TACE group vs the RT group were 34.46±5.28 vs 60.69±7.36 months, respectively. The 1-, 2-, and 3-year OS rates were 81.4%, 61.3%, and 48.4% for patients in the TACE group, and 93.4%, 80.6%, and 70.7% for patients in the RT group, respectively. The RT group showed a significantly longer OS than the TACE group (P=0.037). All of the above data are shown in Figure 1B.
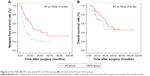
After matching propensity score, the cumulative 1-, 2-, and 3-year RFS rates of all 92 patients were 55.4%, 40.8%, and 32.5%, respectively; the cumulative 1-, 2-, and 3-year OS rates of all 92 patients were 90.1%, 74.3%, and 63.6%, respectively. RFS rate, median RFS times, and OS of the RT group were the same as that of before PSM. The median RFS time of the matched TACE group was 9.18±1.67 months. The 1-, 2-, and 3-year RFS rates were 39.1%, 25.0%, and 20.8% for patients in the matched TACE group. The RT group still showed a significantly longer RFS than the TACE group (P=0.003) as before. All of the above data are shown in Figure 2A. Median OS time of the TACE was 36.53±5.34 months. The 1-, 2-, and 3-year OS rates were 86.9%, 68.1%, and 54.5% for patients in the matched TACE group. There was no significant difference between the matched TACE group and the RT group (P=0.262). All of the above data are shown in Figure 2B.
Recurrence pattern in the TACE and RT groups
Recurrence was observed in 81 of 117 patients. Before matching propensity score, the incidence of nodular recurrence and the incidence of diffuse recurrence were 16 and 9, respectively, in the RT group and 18 and 38, respectively, in the TACE group. The TACE group had more significantly (P=0.007) diffuse recurrence; the incidence of intrahepatic recurrence and incidence of extrahepatic recurrence were 19 and 6, respectively, in the RT group and 48 and 8, respectively, in the TACE group. There was no significant difference between the two groups (P=0.285). The incidence of marginal recurrence and the incidence of nonmarginal recurrence were 4 and 21, respectively, in the RT group and 9 and 47, respectively, in the TACE group. There was no significant difference between the two groups (P=1.000). After matching propensity score, the incidence of nodular recurrence and diffuse recurrence were 15 and 19, respectively, and the incidence of intrahepatic recurrence and extrahepatic recurrence were 30 and 4, respectively, and the incidence of marginal recurrence and nonmarginal recurrence were 7 and 27, respectively. There was no significant difference in the recurrent pattern between the two groups. The details of pattern of recurrent tumor were shown in Table 4.
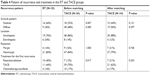  | Table 4 Pattern of recurrence and treatment in the RT and TACE groups |
The initial treatments used for recurrent HCC between the two groups were found to be significant and nonsignificant for before and after PSM, respectively, as shown in Table 4 (before matching, P=0.017; after matching, P=0.253).
Discussion
To the authors’ knowledge, this study is the first to investigate the efficacy of postoperative adjuvant RT and TACE in HCC patients with MVI after a PSM analysis in order to minimize potential bias caused by patients’ backgrounds. In the current study, multivariate analysis indicated that tumor size, MVI classification, and postoperative treatment strategies were independently associated with RFS and tumor size and MVI classification were independently associated with OS. Survival analysis revealed that the estimated median RFS and OS of patients who underwent RT and TACE were 25.74±8.12 vs 9.18±1.67 months (P=0.003) and 60.69±7.36 vs 36.53±5.34 months (P=0.262), respectively. The RT group had significantly longer RFS than the TACE group.
MVI has been reported to be the most significant independent risk factor affecting RFS and OS following curative resection,21–24 the OR reach the level as high as 28.40.25 In the patients with or without MVI, the 1-year RFS is 12% vs 69%.26 In HCC, MVI is regarded as the anatomic prerequisite for tumor spread in circulation.11,27 The feature of MVI encompasses a wide spectrum, such as distance from the invaded vessel to tumor edge, the number of invaded microscopic vessels, intravascular floating tumor clusters, and small vascular intratumoral spaces. Each feature had different prognostic significance. Recently, based on the invasion of vessels ≥1 cm from the tumor capsule9 and the number of invaded vessels ≥5,28 a classification system has been proposed to classify MVI patients into three categories that were individually associated with an inverse correlation with time to recurrence and survival.17 In our study, whether before or after PSM, univariate and multivariate analyses showed that MVI classification was the independent factor either for RFS or for OS. These results suggested that classification systems could distinguish risk features accurately.
Since MVI disseminate mainly via portal venous branches and spread along as well as against the direction of the portal venous flow, an anatomic LR according to intrahepatic distribution of portal vein theoretically gives a higher potential for cure. Conversely, a few studies had found that the incidence of MVI was closely related to the distance from the tumor capsule,29 a wider resection margin is preferable to eradicate microscopic lesions30,31 and theoretically gives a higher potential for reducing recurrence. Some other studies even suggested to ensure a safe resection margin (>2 or >1 cm) for both anatomic and nonanatomic hepatectomy.32–34 However, in this study, irrespective of PSM status, univariate and multivariate analyses showed that anatomical resection and the width of surgical margin had no influence on survival. The likely explanation is that the majority of patients in the cohort had HBV-related cirrhosis and centrally located HCC lesions preserving as much non-tumorous liver parenchyma as possible. A very important consideration for patients with cirrhosis is to prevent postoperative liver failure. In these patients, anatomical resection cannot be performed thoroughly as centrally located HCC lesions with adjoining main vasculatures make the wide margin hepatectomy impossible. Thus, nonanatomic resection with narrow margin may be a better option35,36 and the addition of effectual postoperative treatment was essentially and clinically required to reduce recurrence and improve OS. Postoperative adjuvant treatments can be designed to eliminate exfoliated tumor cells, preexisting microscopic tumor foci, and micrometastases.14
Many postoperative procedures have been investigated as strategies to reduce recurrence, including TACE, RT, and molecular targeted therapy. However, the outcomes of these interventions are variable and controversial.37–42 RT had seldom been used in HCC because of the low tolerance dose of liver. The advance external RT technology, such as three-dimensional conformal or intensity-modulated RT, can deliver tumoricidal radiation doses to the specified liver area,43 while limiting radiation adverse effect.44 Recent clinical studies showed that post operative conformal RT provided promising survival outcomes in HCC patients who underwent hepatectomy.15,45 The effects of postoperative TACE and range of applications are still topics to debate.46 A retrospective study with 2,436 patients with HCC, which had the maximum cases to date, showed that postoperative adjuvant TACE was not effective on postponing recurrence.47 A meta-analyses including 10 RCTs found that postoperative TACE did not improve RFS and OS for curative resection of HCC, except when tumor size was >5 cm.48 A most recent meta-analyses including 3,191 patients found that postoperative adjuvant TACE could achieve higher OS and RFS than surgical resection alone,49 but the conclusion is flawed as 8 RCTs and 12 retrospective studies were included in analysis. In our analysis, RFS in patients who underwent postoperative adjuvant TACE was significantly shorter than in the patients who underwent RT, both before and after PSM. These results suggested that postoperative adjuvant RT could be more effective than TACE in eliminating residual micrometastasis foci in the remnant liver.
The possible explanations for adjuvant RT rather than TACE in improving postoperative long-term survival outcomes of HCC with MVI are complicated. MVI cannot be stained clearly during the TACE procedure as supplying vessels are lacking; thus, it would be difficult to identify definite target area. Extended TACE to all liver subsegments relative to tumor bed is an alternative solution, but it might severely damage liver function, and the adverse effects of TACE would not be acceptable for a postoperative patient with cirrhosis. The conformal or intensity-modulated RT involving concentrated irradiation precisely to tumor bed area prevents normal liver tissues from irradiation at the same time. Adjusting clinical treatment volume based on MVI classification and other clinical pathology factors of patients individually can therefore limit the adverse effect when tumor bed with residual micrometastasis foci receives sufficient radiation. In this study, the recurrence pattern, which showed that the TACE group had more diffuse recurrence and the RT group had similar nonmarginal recurrence, also implies postoperative adjuvant RT could eliminate residual micrometastasis foci in the remnant liver.
As a limitation, in our retrospective study, the postoperative treatment selection was not randomized, which may introduce bias between the groups, although the patients’ baseline was similar among the two groups through PSM. PSM is not the best substitute for randomization as a small overlap in propensity scores makes the two groups incomparable requiring further statistical adjustments for evaluation. However, PSM is being used increasingly in perioperative research with a large number of confounders and a low number of events ensuring balanced treatment groups.50,51 The second limitation was the relatively small sample size, which limited further stratification analysis. However, the data of our study do provide rationale for developing a prospective study. Thus, our results should be validated in a large sample size, randomized, controlled trial in order to make a definitive conclusion. Finally, in our study, patients who underwent RT had significantly longer OS than the patients who underwent TACE before matching, but the difference was not significant after matching. This result could be due to insufficient follow-up time and limited cases. However, more factors are associated with long-term survival of HCC patients rather than just MVI.
Conclusion
Our study revealed that RT following hepatectomy could result in better survival outcomes for HCC patients with MVI than postoperative TACE based on RFS rates. This treatment strategy might especially be effective for patients with nonanatomy or narrow surgical margin.
Acknowledgments
This work was supported by Beijing Hope Run Special Fund of Cancer Foundation of China (LC2015A12) and PUMC Youth Fund/Fundamental Research Funds for the Central Universities (3332016031).
Disclosure
The authors report no conflicts of interest in this work.
References
Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136(5):E359–E386. | ||
Fan ST, Poon RT, Yeung C, et al. Outcome after partial hepatectomy for hepatocellular cancer within the Milan criteria. Br J Surg. 2011;98(9):1292–1300. | ||
Colecchia A, Schiumerini R, Cucchetti A, et al. Prognostic factors for hepatocellular carcinoma recurrence. World J Gastroenterol. 2014;20(20):5935. | ||
Fan ST, Mau Lo C, Poon RT, et al. Continuous improvement of survival outcomes of resection of hepatocellular carcinoma: a 20-year experience. Ann Surg. 2011;253(4):745–758. | ||
Quencer KB, Friedman T, Sheth R, Oklu R. Tumor thrombus: incidence, imaging, prognosis and treatment. Cardiovasc Diagn Ther. 2017;7(Suppl 3):S165–S177. | ||
Rodríguez-Perálvarez M, Luong TV, Andreana L, Meyer T, Dhillon AP, Burroughs AK. A systematic review of microvascular invasion in hepatocellular carcinoma: diagnostic and prognostic variability. Ann Surg Oncol. 2013;20(1):325–339. | ||
Hirokawa F, Hayashi M, Asakuma M, Shimizu T, Inoue Y, Uchiyama K. Risk factors and patterns of early recurrence after curative hepatectomy for hepatocellular carcinoma. Surg Oncol. 2016;25(1):24–29. | ||
Bruix J, Llovet JM. Major achievements in hepatocellular carcinoma. Lancet. 2009;373(9664):614–616. | ||
Roayaie S, Blume IN, Thung SN, et al. A system of classifying microvascular invasion to predict outcome after resection in patients with hepatocellular carcinoma. Gastroenterology. 2009;137(3):850–855. | ||
Du M, Chen L, Zhao J, et al. Microvascular invasion (MVI) is a poorer prognostic predictor for small hepatocellular carcinoma. BMC Cancer. 2014;14:38. | ||
Lim KC, Chow PK, Allen JC, et al. Microvascular invasion is a better predictor of tumor recurrence and overall survival following surgical resection for hepatocellular carcinoma compared to the Milan criteria. Ann Surg. 2011;254(1):108–113. | ||
Ye JZ, Chen JZ, Li ZH, et al. Efficacy of postoperative adjuvant transcatheter arterial chemoembolization in hepatocellular carcinoma patients with microvascular invasion. World J Gastroenterol. 2017;23(41):7415–7424. | ||
Sun JJ, Wang K, Zhang CZ, et al. Postoperative adjuvant transcatheter arterial chemoembolization after R0 hepatectomy improves outcomes of patients who have hepatocellular carcinoma with microvascular invasion. Ann Surg Oncol. 2016;23(4):1344–1351. | ||
Wang L, Wang W, Yao X, et al. Postoperative adjuvant radiotherapy is associated with improved survival in hepatocellular carcinoma with microvascular invasion. Oncotarget. 2017;8(45):79971–79981. | ||
Yu W, Wang W, Rong W. Adjuvant radiotherapy in centrally located hepatocellular carcinomas after hepatectomy with narrow margin. J Am Coll Surg. 2014;218(3):381–392. | ||
Korn RL, Crowley JJ. Overview: progression-free survival as an endpoint in clinical trials with solid tumors. Clin Cancer Res. 2013;19(10):2607–2612. | ||
Cong WM, Bu H, Chen J, et al. Practice guidelines for the pathological diagnosis of primary liver cancer: 2015 update. World J Gastroenterol. 2016;22(42):9279–9287. | ||
Seldinger SI. Catheter replacement of the needle in percutaneous arteriography; a new technique. Acta Radiol. 1953;39(5):368–376. | ||
Brookhart MA, Schneeweiss S, Rothman KJ, Glynn RJ, Avorn J, Stürmer T. Variable selection for propensity score models. Am J Epidemiol. 2006;163(12):1149–1156. | ||
Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46(3):399–424. | ||
Andreou AA, Vauthey J-N, Cherqui D. Improved long-term survival after major resection for hepatocellular carcinoma: a multicenter analysis based on a new definition of major hepatectomy. J Gastrointest Surg. 2013;17(1):66–77. | ||
Barreto SG, Brooke-Smith M, Dolan P, Wilson TG, Padbury RTA, Chen JWC. Cirrhosis and microvascular invasion predict outcomes in hepatocellular carcinoma: outcomes of hepatocellular carcinoma. ANZ J Surg. 2013;83(5):331–335. | ||
Moon JI, Kwon CH, Joh JW, et al. Primary versus salvage living donor liver transplantation for patients with hepatocellular carcinoma: impact of microvascular invasion on survival. Transplant Proc. 2012;44(2):487–493. | ||
Fan LF, Zhao WC, Yang N, Yang GS. Alpha-fetoprotein: the predictor of microvascular invasion in solitary small hepatocellular carcinoma and criterion for anatomic or non-anatomic hepatic resection. Hepatogastroenterology. 2013;60(124):825–836. | ||
McHugh PP, Gilbert J, Vera S, Koch A, Ranjan D, Gedaly R. Alpha-fetoprotein and tumour size are associated with microvascular invasion in explanted livers of patients undergoing transplantation with hepatocellular carcinoma. HPB (Oxford). 2010;12(1):56–61. | ||
Zhao WC, Fan LF, Yang N, Zhang HB, Chen BD, Yang GS. Preoperative predictors of microvascular invasion in multinodular hepatocellular carcinoma. Eur J Surg Oncol. 2013;39(8):858–864. | ||
Toyosaka A, Okamoto E, Mitsunobu M, Oriyama T, Nakao N, Miura K. Pathologic and radiographic studies of intrahepatic metastasis in hepatocellular carcinoma; the role of efferent vessels. HPB Surg. 1996;10(2):97–104. | ||
Sumie S, Nakashima O, Okuda K, et al. The significance of classifying microvascular invasion in patients with hepatocellular carcinoma. Ann Surg Oncol. 2014;21(3):1002–1009. | ||
Shi M, Zhang CQ, Zhang YQ, Liang XM, Li JQ. Micrometastases of solitary hepatocellular carcinoma and appropriate resection margin. World J Surg. 2004;28(4):376–381. | ||
Hu RH, Lee PH, Chang YC, Ho MC, Yu SC. Treatment of centrally located hepatocellular carcinoma with central hepatectomy. Surgery. 2003;133(3):251–256. | ||
Hirokawa F, Hayashi M, Miyamoto Y, et al. Outcomes and predictors of microvascular invasion of solitary hepatocellular carcinoma. Hepatol Res. 2014;44(8):846–853. | ||
Ikai I, Arii S, Kojiro M, et al. Reevaluation of prognostic factors for survival after liver resection in patients with hepatocellular carcinoma in a Japanese nationwide survey. Cancer. 2004;101(4):796–802. | ||
Shi M, Guo RP, Lin XJ, et al. Partial hepatectomy with wide versus narrow resection margin for solitary hepatocellular carcinoma: a prospective randomized trial. Ann Surg. 2007;245(1):36–43. | ||
Shimada K, Sakamoto Y, Esaki M, Kosuge T. Role of the width of the surgical margin in a hepatectomy for small hepatocellular carcinomas eligible for percutaneous local ablative therapy. Am J Surg. 2008;195(6):775–781. | ||
Matsui Y, Terakawa N, Satoi S. Postoperative outcomes in patients with hepatocellular carcinomas resected with exposure of the tumor surface: clinical role of the no-margin resection. Arch Surg Chic Ill 1960. 2007;142(7):596–602. | ||
Moris D, Tsilimigras DI, Kostakis ID, et al. Anatomic versus non-anatomic resection for hepatocellular carcinoma: a systematic review and meta-analysis. Eur J Surg Oncol. 2018;44(7):927–938. | ||
Zhong C, Guo RP, Li JQ, et al. A randomized controlled trial of hepatectomy with adjuvant transcatheter arterial chemoembolization versus hepatectomy alone for stage III a hepatocellular carcinoma. J Cancer Res Clin Oncol. 2009;135(10):1437–1445. | ||
Peng BG, He Q, Li JP, Zhou F. Adjuvant transcatheter arterial chemoembolization improves efficacy of hepatectomy for patients with hepatocellular carcinoma and portal vein tumor thrombus. Am J Surg. 2009;198(3):313–318. | ||
Kobayashi T, Ishiyama K, Ohdan H. Prevention of recurrence after curative treatment for hepatocellular carcinoma. Surg Today. 2013;43(12):1347–1354. | ||
Zhong J-H, Du X-K, Xiang B-D, Li L-Q. Adjuvant sorafenib in hepatocellular carcinoma: a cautionary Comment of storm trial. World J Hepatol. 2016;8(23):957–960. | ||
Jeng WJ, Lin CC, Chen WT, Sheen IS, Lin CY, Lin SM. Adjuvant therapy for hepatocellular carcinoma after curative treatment. Dig Dis. 2014;32(6):747–754. | ||
Lei J, Zhong J, Hao J, et al. Hepatocellular carcinoma cases with high levels of c-Raf-1 expression may benefit from postoperative adjuvant sorafenib after hepatic resection even with high risk of recurrence. Oncotarget. 2016;7(27):42598–42607. | ||
Cheng SH, Lin YM, Chuang VP, et al. A pilot study of three-dimensional conformal radiotherapy in unresectable hepatocellular carcinoma. J Gastroenterol Hepatol. 1999;14(10):1025–1033. | ||
Kim JY, Chung SM, Choi BO, Kay CS. Hepatocellular carcinoma with portal vein tumor thrombosis: improved treatment outcomes with external beam radiation therapy. Hepatol Res. 2011;41(9):813–824. | ||
Wang WH, Wang Z, Wu JX, et al. Survival benefit with IMRT following narrow-margin hepatectomy in patients with hepatocellular carcinoma close to major vessels. Liver Int. 2015;35(12):2603–2610. | ||
Tong Y, Li Z, Liang Y, et al. Postoperative adjuvant TACE for patients of hepatocellular carcinoma in AJCC stage I: friend or foe? A propensity score analysis. Oncotarget. 2017;8(16):26671–26678. | ||
Chen X, Zhang B, Qiu S. Effect of postoperative adjuvant transarterial chemoembolization on late recurrence of hepatocellular carcinoma after radical resection. Zhonghua Gan Zang Bing Za Zhi. 2010;18(8):599–603. | ||
Cheng X, Sun P, Hu QG, Song ZF, Xiong J, Zheng QC. Transarterial (chemo)embolization for curative resection of hepatocellular carcinoma: a systematic review and meta-analyses. J Cancer Res Clin Oncol. 2014;140(7):1159–1170. | ||
Liao M, Zhu Z, Wang H, Huang J. Adjuvant transarterial chemoembolization for patients after curative resection of hepatocellular carcinoma: a meta-analysis. Scand J Gastroenterol. 2017;52(6–7):624–634. | ||
Sainani KL. Propensity scores: uses and limitations. PM&R. 2012;4(9):693–697. | ||
Okoli GN, Sanders RD, Myles P. Demystifying propensity scores. Br J Anaesth. 2014;112(1):13–15. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.