Back to Journals » Orthopedic Research and Reviews » Volume 12
Optimal Management of Acromioclavicular Dislocation: Current Perspectives
Authors Nolte PC , Lacheta L, Dekker TJ, Elrick BP, Millett PJ
Received 16 January 2020
Accepted for publication 19 February 2020
Published 5 March 2020 Volume 2020:12 Pages 27—44
DOI https://doi.org/10.2147/ORR.S218991
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Clark Hung
Philip C Nolte,1,2 Lucca Lacheta,1,3 Travis J Dekker,1,4 Bryant P Elrick,1 Peter J Millett1,5
1Steadman Philippon Research Institute, Vail, CO, USA; 2Department of Trauma and Orthopedic Surgery, BG Trauma Center Ludwigshafen, Ludwigshafen, Germany; 3Center for Musculoskeletal Surgery, Charité Universitaetsmedizin Berlin, Berlin, Germany; 4Eglin Air Force Base, 96th Medical Group, United States Air Force, Eglin, FL, USA; 5The Steadman Clinic, Vail, CO, USA
Correspondence: Peter J Millett
Steadman Philippon Research Institute, 181 W Meadow Dr, Ste 400, Vail, CO 81657, USA
Tel +1 970 479-5871
Email [email protected]
Abstract: Injuries to the acromioclavicular (AC) joint are common and mostly involve younger, male individuals. Whereas the majority of AC joint dislocations can be treated nonoperatively with a trial of immobilization, pain medication, cryotherapy, and physiotherapy, there are patients that do not respond well to conservative management and may require surgical treatment. Identifying and treating these patients according to the type and chronicity of AC joint dislocation is paramount. To date, a myriad of surgical techniques have been proposed to address unstable AC joint dislocations and are indicative of the uncertainty that exists in optimal management of these injuries. Historically research has focused on the restoration of the coracoclavicular ligament complex. However, recently the importance of the acromioclavicular capsule and ligaments has been emphasized. This review aims to provide the reader with an overview of current treatment strategies and research, as well as future perspectives.
Keywords: AC capsule, AC joint, coracoclavicular, reconstruction, stabilization, shoulder surgery
Anatomy
The acromioclavicular (AC) joint is a diarthrodial joint formed by the distal clavicle and scapula (acromion). Opposing articulating surfaces are covered in hyaline cartilage and a fibrocartilaginous disk is present intraarticularly that undergoes rapid degeneration between the 2nd and 4th decades of life1 and varies in size, shape and completeness.2 The AC joint serves as the link between the shoulder girdle and axial skeleton and facilitates both gliding and rotational motion. More specifically, it serves as a coordinating link between the scapulothoracic (ST), glenohumeral (GH), and sternoclavicular (SC) joints and allows for physiological movement.3 Stabilization of the AC joint is achieved via dynamic and static contributions. Important anatomic structures that provide static stabilization to the joint include the joint capsule, acromioclavicular (AC) and coracoclavicular (CC) ligament complex.
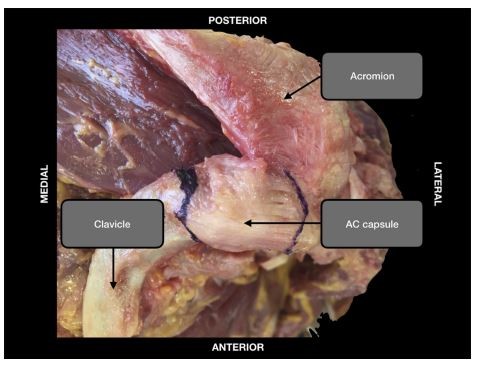
The AC joint capsule is relatively thin, but contributes directly to AC joint stability, along with a capsular thickening known as the AC ligament (Figure 1). The AC ligament complex spans between the acromion and the distal clavicle and has been described by multiple authors as having anterior, posterior, superior, and inferior components;4,5 however, numerous cadaveric studies have failed to identify the inferior ligament up to 50% of the time.6–8 Nakazawa et al9 divided the ligament into 2 parts: superoposterior (SP) and anteroinferior (AI). Despite consistent presence of the SP bundle, the AI bundle varied in thickness and location, spanning the inferior part of the joint in only 42% of the investigated shoulders. Biomechanically, the AC ligament is primarily responsible for resisting anterior-posterior AC joint translation,10–13 while providing additional restraint against posterior axial rotation of the clavicle.12 In comparison to the CC ligament complex, the AC ligament complex usually fails first, signifying it may be responsible for resisting relatively small moments of displacement while the CC ligament resists larger displacement moments.14
 |
Figure 1 Superior view of a cadaveric left shoulder specimen showing the acromioclavicular capsule. |
The coracoclavicular ligament complex is made out of two components: the conoid and trapezoid ligaments, which are positioned anteromedial and posterolateral, respectively, and span between the inferior, distal clavicle and the base of the coracoid process. Together these ligaments provide superoinferior static AC joint stabilization, with the trapezoid being the stronger ligament.15 Additionally, they also provide rotational stability and stability with protraction and retraction of the scapula. The conoid ligament originates on the superomedial coracoid base and courses superolateral to insert broadly on the clavicular conoid tubercle. Similarly, the trapezoid originates on the superomedial surface of the coracoid, anterior to the conoid, and travels superolateral to insert narrowly on the clavicular trapezoid line, anterior to the conoid tubercle.16 The diverging course and distinct attachments of both ligaments argues individual function that must be considered during surgical reconstruction. Rios et al determined that reliable CC ligament clavicular insertions could be calculated as percentages of total clavicular length—the trapezoid and conoid attaching 17% and 31% of the total clavicular length from the distal end, respectively. Chahla et al16 quantitatively found that the CC ligament clavicular insertion is on average 15.7 mm from the lateral joint line and the footprint spans an average length of 25.6 mm on the clavicle. Additionally, mean distances from the coracoid apex to the center of the trapezoid and conoid ligaments are 27.0 ± 3.3 mm and 33.9 ± 3.3 mm, respectively.
Epidemiology
AC injuries are common with as many as 9% of all shoulder girdle injuries involving the AC joint.17 The estimated incidence of AC joint injuries is 1.8 per 1000 per year, with the majority of injuries occurring between ages 20 to 40 and men being 8.5 times more likely to suffer injury compared to women. The cause for disparity is most likely due to life-style differences and men being more apt to participate in high-risk activity.18 Additionally, AC joint injuries are more common in the sports-participating population, particularly during contact sports like hockey, wrestling, and rugby, among others.17 Notably, a recent study evaluating injuries in American professional football players found that almost 30% of all National Football League (NFL) shoulder injuries were AC joint-related.19
The mechanism of AC joint injury can occur as a result of either direct or indirect trauma, although direct blows to the lateral shoulder are the most common precipitating event. The characteristic strength of the SC joint transmits contact forces to the AC joint, distal clavicle, and supporting ligaments, causing disruption.3 Indirect injury is generally position-related and can occur after a fall onto the ipsilateral extremity in either an adducted or outstretched position, which makes AC and CC ligaments more vulnerable to injury.20
Classification
Tossy et al21 was among the first to propose a classification system for AC joint injuries in 1963. Since then, numerous classifying schemes have been suggested by various authors. In 1984, Rockwood22 expanded on the original system to develop a six-part classification that is the most adopted and widely used classifying method to date (Table 1).
 |
Table 1 Acromioclavicular Injuries: Rockwood Classification |
The Rockwood classification system utilizes radiographs of the shoulder (AP, axillary, and Zanca views) to characterize the direction and displacement of the injured shoulder, in relation to the contralateral side. Type I injuries involve a sprain or partial tear to the AC ligament without clinical or radiographic evidence of joint instability or CC ligament injury. Type II injuries include a complete tear of the AC ligament, with only a sprain or partial tear to the CC ligaments. Intact CC ligaments prevent drastic acromial depression and aid in maintaining the normal relationship of the joint, thus, identifying these injuries radiographically can be challenging. Complete rupture of the AC ligaments may lead to horizontal instability. Type III injuries involve complete tears of the AC and CC ligament complexes.23 Disruption of these ligaments can cause both vertical and horizontal instability that can be grossly appreciated, as well as an increased coracoclavicular (CC) distance up to 100% the uninjured side (Figure 2). The CC distance is defined as the length from superior cortex of the coracoid process to the undersurface of the clavicle where the CC ligaments insert. Type IV injuries also require complete tears of the AC and CC ligaments, but are specifically characterized by distal clavicle posterior displacement, which commonly results in buttonholing of the trapezius. Type V injuries are simply more severe Type III injuries. These injuries similarly result in complete tears of the AC and CC ligament complexes, but the CC distance is increased between 100–300% of normal (Figure 3). Type VI injuries are characterized by inferior displacement of the distal clavicle, either inferior to the acromion or coracoid, with complete disruption of ligamentous complexes and likely damage to the trapezial fascia and/or deltoid.
The Rockwood classification is meant to serve as a treatment guide. Type I and II injuries are typically managed non-operatively, while type IV–VI injuries are treated with surgical reduction and stabilization. There remains controversy over the management of type III injuries without consensus. Although historically these injuries are treated non-operatively, some patients respond poorly and may benefit from surgical intervention. Recently, the International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine Upper Extremity Committee (ISAKOS) has suggested a more specific classification that subdivides type III injuries into IIIA and IIIB. Type IIIA injuries present as stable, while grade IIIB injuries are thought to be unstable with positive radiological and clinical findings pointing to additional horizontal instability (Figure 4).23 The authors agree that type III injuries must be evaluated carefully and managed individually since unstable injuries (type IIIB) are more likely to result in continued morbidity. Furthermore, remembering to address co-pathologies is essential in achieving optimal outcomes with over 50% of patients with AC joint dislocations type III and V present with concomitant intra-articular glenohumeral injury.24
Nonoperative Treatment
Optimal treatment of AC joint injuries remains controversial. In general, it is accepted that Rockwood type I and II AC joint dislocations are treated non-operatively.25 Treatment of these injuries typically consists of pain medication, cryotherapy and the use of a sling for comfort for one to two weeks with the encouragement of early range of motion activities and weaning of the sling as pain permits. In contrast, type IV–VI injuries have classically been treated in an operative manner.15 Controversy remains about optimal treatment of type III injuries20 as well as new evidence of trials of non-operative management even for type V AC separations.26
As studies have shown good to excellent outcomes in 80% of patients treated non-operatively in the setting of a type III AC injury,27 authors are now advocating for initial conservative management in type III injuries and only resorting to surgery when the trial of non-operative management fails.28 Identifying those that may fail has been the key to determining more aggressive options of treatment to include early surgical intervention as there is some evidence to suggest that chronic injuries do worse than those that are treated acutely.29 Patient lifestyle and demand has been a determining factor in advocating for surgery in the setting of type III injuries in patients that are considered high demand, athletic and laborers.30 Additionally, patients that perform routine activities such as bench press or push-ups may warrant surgical treatment in order to obtain optimal clinical outcomes (ie military population).27,31 In these population groups who may be less tolerant to persistent AC instability, a variety of radiographic techniques have been described to evaluate dynamic instability of the AC joint. Bontempo et al described using a cross arm-adduction radiograph to identify horizontal AC instability by evaluating clavicular overlap on the acromion.32 Alexander et al describes obtaining scapular Y radiographs of bilateral shoulders with cross arm adduction to allow for direct comparison of AC overlap.33,34 These stress radiographs can be used to determine when early operative intervention in an at-risk population is warranted.
Interestingly, patients with type V injuries may be offered a trial of non-operative management. Even in the high demand population such as the military, Krul et al demonstrated that when treated initially with conservative management, patients with type V AC injuries return to duty at equivalent rates and time.26 They also found that total clavicle displacement was a more reliable indicator compared to change in CC distance in determining patients that went on to fail non-operative management.26 Figure 5 illustrates an approach to the management of AC joint dislocations.
 |
Figure 5 Flowchart illustrating the management of acromioclavicular joint dislocation. |
Operative Treatment
Timing to Surgery
The AC joint ligaments lose their potential to heal after three weeks following injury.35 Therefore, in AC joint dislocations acuity is commonly defined as < 3 weeks and chronicity as > 6 weeks.36 However, as previously discussed, type III injuries may require an initial course of non-operative treatment that usually extends one month;37 therefore, defining acute as < 3 weeks is unrealistic in some circumstances. For this reason, some authors propose a threshold of six months for terming AC joint injuries chronic.37 Indeed, the debate regarding chronicity is ongoing.
When surgery has been determined as the optimal treatment, there is moderate evidence to support early operative intervention compared to that of delayed surgical reconstruction. Rolf et al compared outcomes of early versus delayed AC joint stabilization with improvement in Constant scores, maintenance of surgical reduction, improvement in patient satisfaction and less overall complications in the early treatment cohort.38 Similarly, a systematic review of eight studies by Song et al demonstrated improvement in Constant scores and overall functional outcomes in early versus delayed operative intervention.39 In contrast, Krul et al showed in their series of active duty military patients with type V AC dislocations, that those that undergo reconstruction in a delayed fashion show no statistical delay in return to duty.26 Higher powered studies with randomization of groups when determining timing of surgery is required to truly determine the effect of early versus delayed treatment.
AC-Stabilization in Acute Cases
Stabilization with Metallic Devices
Several techniques for the reduction of acute AC dislocations have been published. Table 2 summarizes outcomes and complications from the most recent literature. Historically, metal implants such as the Bosworth screw, which has shown to be effective in surgical stabilization of grade III, IV and V AC joint dislocations, have been technically easy to implant in a short surgical time. Biomechanically, Ammon et al40 showed that the Bosworth screw restored the strength close to the native AC joint with intact coracoclavicular ligaments. Clinical long-term results suggest that the Bosworth screw technique is reliable and provides adequate reduction and similar outcomes in terms of function and pain level when compared to minimally-invasive K-wire fixation.41 Compared to K-wires the Bosworth screw has shown to be superior in early infection rates and lower rates of AC joint osteoarthritis (intra- vs extraarticular fixation) after 8 years.41 However, compared to newer suspensory device techniques the Bosworth screw presented with less patient satisfaction and more inconveniences.42 Furthermore, in all patients treated with the Bosworth screw, a second surgical intervention with known associated risks was necessary to remove the implant.42
 |  |  |
Table 2 Summary of the Most Recent Literature (< 10 Years) Regarding Surgical Treatment of AC Joint Dislocation |
The hook plate metallic device showed early promise as an alternative implant to treat unstable AC injuries. In direct comparison to the Bosworth screw, Kezunovìc et al43 observed a lower, yet not significant, complication rate in patients treated with the hook plate and significantly higher Constant scores and patient satisfaction when compared to the Bosworth screw. However, this difference diminished over time as reported in the long-term study by Broos et al44 Koukakis et al suggests removal of the hook plate within 3 months to avoid the possibility of plate related subacromial impingement. This may lead to lower postoperative pain and complication rates when compared to suspensory device fixations, however, suspensory device fixations have higher shoulder function scores as summarized by Arirachakaran et al in a systematic review and meta-analysis.45
Suspensory Devices
Over time, surgical treatment of relevant acute AC joint dislocations has become more minimal-invasive using low-profile suspensory devices (Figure 6). One of the advantages of suspensory devices are that the hardware does not need to be removed. This advantage was shown by Wang et al in their clinical comparison of suspensory device fixation with additional tendon allograft compared to hook plating.46 Additionally, Millett et al47 described the advantage of suspensory device fixation in relation to its arthroscopically assisted approach, which allows for the detection of concomitant glenohumeral pathologies associated with acute and chronic acromioclavicular joint injuries.24
 |
Figure 6 Conventional anteroposterior radiographic images of a left shoulder following stabilization with a suspensory button device (circle). |
Clinical short-term results after suspensory device fixation showed excellent postoperative outcome scores (mean ASES score of 93.8 points) and no further revision surgery, however, complications occurred in 23%.48 A closer look at complications following cortical button fixation or additional tendon graft fixation by Martetschlaeger and Millett detected a construct survivorship of 86% at 12 months and 83% at 24 months postoperatively.48 To further reveal risk factors for failure of suspensory devices, Spiegl et al investigated the influence of bone tunnel diameter on construct strength and the risk for clavicle fractures in their biomechanical study comparing two common CC reconstruction techniques.49 While the use of an additional allograft increased construct strength, it also increased tunnel diameter and the associated risk for clavicle fractures.48
To keep the advantage of increased strength after incorporation of an additional tendon graft, which is theorized to generate an increase in both primary and secondary stability due to its biologic component, the arthroscopic acromioclavicular joint reconstruction technique using a suspensory device with an additional tendon graft was modified by Menge et al50 with the graft looped around the clavicle and coracoid process instead of using bone tunnels. This technique allows for smaller bone drilling and decreased fracture risk. At the same time a knotless fixation was introduced to avoid knot and hardware irritation while maintaining excellent stability.
Furthermore, reducing anatomic CC ligament reconstruction from double- to single-bundle reconstruction for the treatment of acute AC joint dislocations resulted in less drilling-associated fracture risk and successful long-term clinical and radiographic outcomes as demonstrated by Mori et al51.
AC-Reconstruction in Chronic Cases
Chronic ACJ instability is a challenging injury to treat for orthopedic surgeons. It can occur from delayed initial or failed non-operative or operative treatment of AC joint dislocations. It is widely accepted that the AC and CC ligaments lose their potential to heal greater than 3 weeks after the injury35 however, as discussed previously, the debate on defining chronicity is ongoing.36,37 When comparing the outcomes following operative treatment of acute (< 3 weeks) vs chronic (> 3 weeks) ACJ injuries, it has been demonstrated that for chronic injuries, poorer results can be expected.35,38,39,52 While acute treatment of AC joint dislocations aims to approximate the ends of the AC and CC ligaments in order to achieve healing, the biological capabilities are compromised in chronic cases.35,53,54 Therefore, mechanical stabilization of the dislocated joint alone without the use of biological augmentation may be insufficient. The next paragraphs aim to provide an overview of historical and current treatment concepts of chronic AC joint instability.
Ligament and Tendon Transfers
The transposition of the coracoacromial (CA) ligament to the distal clavicle has first been introduced by Weaver and Dunn in 1972 to stabilize AC joint dislocations.55 A distal clavicle excision was performed as an adjunct to the ligament transfer.55 Rauschning et al reported on excellent clinical outcomes following the Weaver-Dunn procedure in 18 patients.56 Kawabe et al treated 41 patients and achieved favorable results in Rockwood type III dislocations.57
To further improve healing and initial stability of the construct, numerous changes to the original technique such as additional augmentation (e.g. sutures, screws, suspensory button devices, plates)58–62 and fixation techniques (e.g. bone chip from the acromion)63,64 were introduced. This altered design was referred to as a “modified Weaver-Dunn procedure”. However, the coracoacromial ligament as a graft source represents only 25% of the native biomechanical strength of the CC ligaments.65,66 In the absence of other biological structures, which is the case in chronic AC joint dislocations, the CA ligament transfer and its modifications are more susceptible to failure, even after complete healing of the construct. This can potentially lead to recurrent instability in up to 30% of patients.35,55 Furthermore, another potential downside of the Weaver-Dunn technique is sacrificing the CA ligament, which is part of the coracoacromial arc and acts as a static restraint against anterosuperior migration of the humeral head, especially in patients with massive rotator cuff tears.67–69 Additionally, the vector of the transferred CA ligament does not represent the vector of the native CC ligaments.65
With the advent of autogenic and allogenic tendons in orthopedics, as well as newer implants, the Weaver-Dunn procedure is losing its role in the treatment of chronic AC joint dislocations. Tauber et al demonstrated in a prospective comparative study on chronic AC joint dislocations, that a semitendinosus graft resulted in significantly superior clinical and radiological outcomes compared to the modified Weaver-Dunn procedure.64 Hegazy et al also demonstrated superior outcomes in comparison to the modified Weaver-Dunn procedure by using a semitendinosus tendon in chronic AC joint injuries.70 Kocaoglu et al compared an autogenic palmaris longus graft to a modified Weaver-Dunn procedure in chronic dislocations and postulated benefits for the graft group with significantly better outcome scores.60 When comparing the modified Weaver-Dunn procedure to synthetic ligaments for the treatment of chronic dislocations, the synthetic ligament resulted in better outcome scores as well as earlier return to work and sport.71 In a systematic review by Borbas et al tendon or ligament transfers, such as the Weaver-Dunn procedure, showed inferior clinical and radiological outcomes when compared to non-biological (e.g. synthetic ligaments and suture loops) and biological (e.g. allograft or autograft) fixation techniques.53 Furthermore, ligament and tendon transfers resulted in the highest overall complication rate (17.3%) with infections being the most common complication (7.4%).53
Dynamic Fixation with Conjoined Tendons
In order to avoid harvesting the CA ligament with the possibility of weakening the coracoacromial arc, the idea of utilizing the short head of the biceps was first introduced in 1942.72 Sloan et al postulated that the lateral half of the conjoined tendon is a viable and slightly more stable alternative (265 N) to the CA ligament transfer (246 N).73 However, the native CC ligaments where still 250% stronger (621 N).73 In a retrospective study involving 38 patients with an average follow up of 38.7 months, good clinical results according to the Constant score (90.6 points) and good to excellent satisfaction in 89% of patients was achieved with this technique.69 However, radiological evaluation at the time of final follow up showed loss of reduction in 21% of cases.69 Kim et al combined the lateral half of the conjoined tendon with a CA ligament transfer in chronic AC joint dislocations with the additional use of Steinman pins for trans-fixation and reported their results of 12 patients with a follow up of 2 years.74 No loss of reduction at final follow up was observed, and 11 out of 12 patients showed excellent results (18.5 points) according to the UCLA score.74 However, the additional use of Steinman pins required secondary removal, and due to the CA ligament transfer the coracoacromial arc was interrupted. Le Hanneur et al described a technique using a split short head of the biceps tendon in addition to a CA ligament transfer.75 The split tendon was fixed to the clavicle in an anatomic position to account for the individual position of the conoid and trapezoid ligaments. A biomechanical comparison utilizing the above mentioned technique showed significantly lower displacements after cyclic loading in the axial plane compared to a modified Weaver-Dunn procedure.76 However, clinical results are not yet available for this technique and CA ligament harvesting again poses the risk for anterosuperior migration of the humeral head.67–69
Synthetic Ligaments
Numerous synthetic materials such as carbon fiber, polytetrafluoroethylene (GoreTex®) and polyethyleneterephthalate (LARS®; Dacron®) have been used as artificial ligaments for the treatment of chronic AC joint dislocations. These materials aim to provide primary stability and induce healing through colonization of fibroblasts into their interwoven and porous fibers.77 Fraschini et al reported on a success rate (good to excellent results) in 93.3% of patients when using the LARS® ligament, with a complication rate of only 3.3%.78 Using a Dacron® vascular prosthesis a success rate of only 53.3% was achieved. Furthermore, a high complication rate (43.3%) in the Dacron® group was observed, mostly due to rupture of the neoligament (23.3%).78 Tiefenboeck et al reported on good to excellent outcomes in all 47 patients after a mean follow up of 7.4 years with the use of the LARS® ligament.79 Complications occurred in 5 patients (11%), necessitating surgical revision in 4 patients.79 Also, the use of a vascular graft (GorePropaten®) showed acceptable results in chronic ACJ dislocations with no infections, a mean DASH score of 6.42 points and Constant score of 82 points at 24 months follow up.80
However, when comparing the use of a semitendinosus graft with the use of a LARS® ligament in chronic AC joint dislocations Rockwood type III or higher, a significantly better Constant score was demonstrated at 1 and 4 years follow up in the “biological” group.77 Despite relatively good results, synthetic ligaments are still associated with a significant degree of foreign body reactions and should be used with caution.81
Reconstruction with Allo- and Autografts
Although, allografts and autografts such as palmaris longus,60,82 flexor carpi radialis,82 peroneus longus,83 and tibialis anterior tendons84 have been utilized for the treatment of AC joint dislocations, hamstring tendons are most commonly used.53,64,77,84–87 Tendon grafts are used in both acute and chronic AC joint dislocations, however, they are most beneficial in chronic AC joint injuries, since in order to facilitate healing, biological augmentation is needed.88
Free tendon grafts have been shown to provide superior biomechanical strength compared to the Weaver-Dunn procedure65,82,87,89 and similar biomechanical strength to suspensory button devices.88 Also, clinical studies focusing on the reconstruction of chronic AC joint dislocations have yielded favorable results when using tendon grafts. Fauci et al demonstrated better clinical and radiographic outcomes for semitendinosus grafts compared to a synthetic ligament.77 Performing an anatomic reconstruction using a tibialis anterior allograft or semitendinosus graft, Carofino and Mazzocca reported on good clinical outcomes in their case series of 17 patients with significant improvements in pre- to postoperative SST, Constant and ASES scores.84 However, they experienced a revision rate of 17.6% due to AC joint pain, infection, and loss of reduction.84 When using a semitendinosus graft to reconstruct both the AC and CC ligaments, Kibler et al reported on good clinical outcomes with a DASH score of 13 points after a minimum follow up of 1.5 years with no complications related to the surgical procedure.90 In a systematic review on surgical management of chronic AC joint dislocations, biological fixation with tendon grafts proved to result in better postoperative outcomes compared to nonbiological fixation and ligament/tendon transfers (e.g. Weaver-Dunn).53 Also, the reported complication rate was relatively low (15.5%) when considering the highest rate (33.8%) of previous AC joint reconstructions in the tendon graft group.53
Current literature focusses on “anatomic” reconstruction of the CC ligaments, to best restore the native CC and AC ligaments.82,87,89,91 However, it is hard to determine which AC joint reconstruction is truly anatomical. Wellmann et al postulated, that reconstructions should only be referred to as “anatomic” if they address the native CC ligament insertions on the coracoid and clavicle, thus necessitating two points of fixations on both the clavicle and coracoid.88 Some authors argue, that a truly anatomic AC joint reconstruction must include the AC ligaments as well.90,91 However, when aiming to perform an anatomic AC joint reconstruction care should be taken to find a compromise between anatomic reconstruction using multiple points of fixation (e.g. drill holes/tunnels) and increasing the risk for coracoid and clavicle fractures.49 Milewski et al reported two coracoid and three clavicle fractures in a series of 27 patients following anatomic reconstruction of the CC ligaments when using a coracoid bone tunnel or two clavicular bone tunnels. Millett et al reported a 6.5% clavicle fracture rate following anatomic CC reconstruction using two clavicular bone tunnels for graft fixation.92 Martetschläger et al reported on a clavicle fracture rate of 4.6% in patients treated with a tendon graft.48
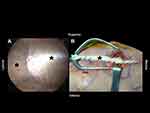
Senior Authors Preferred Technique
The senior author of this manuscript (blinded for review) prefers an arthroscopic reconstruction technique using a knotless CC fixation and soft-tissue anatomic CC ligament reconstruction for both acute and chronic AC joint dislocations.50 Indications include acute and chronic Rockwood type IV to VI injuries, horizontally unstable type IIIB and symptomatic type IIIA injuries that have failed a course of non-operative management.23,93 A standard diagnostic arthroscopy is performed, and concomitant injuries are treated accordingly.24 The subcoracoid space is then debrided and the inferior aspect of the coracoid is prepared (Figure 7A). A 2 to 3cm skin incision and subsequent subcutaneous dissection are performed over the distal end of the clavicle perpendicular to its long axis. A cannula of appropriate size to fit an AC aiming device is inserted through an anteroinferolateral portal. The aiming device is then placed centered on the undersurface of the coracoid (Figure 7B). A 2.4 mm cannulated drill bit is drilled through the distal clavicle and coracoid under arthroscopic visualization. Subsequently, a unicortical reamer is utilized to drill a centered bone socket into the superior aspect of the distal clavicle to avoid soft tissue irritation of the later placed fixation device. A suture is passed from superior through the cannulated drill and retrieved through the anteroinferolateral portal with an arthroscopic grasper (Figure 8A). After removing the drill, a double-loaded knotless CC fixation device (Dog Bone; Arthrex, Naples, FL, USA) is then inserted through the shuttling suture and passed through the coracoid and clavicular bone tunnels. The cortical button is positioned flush on the coracoid undersurface (Figure 8B). The AC joint is then reduced, and the fixation device is pulled securely followed by cutting of the suture ends.
For anatomic reconstruction, an allograft (hamstrings or tibialis anterior) or an autograft (hamstrings) can be used. Two soft tissue tunnels are created for soft-tissue passage with the use of a dilator. Under direct arthroscopic visualization, the first tunnel is created from the posterior aspect of the clavicle to the medial aspect of the coracoid, and the second tunnel is placed from the anterior aspect of the clavicle to the lateral aspect of the coracoid, recreating the conoid and the trapezoid vector respectively. The graft is then passed through the soft-tissue tunnels and looped around the coracoid with the help of shuttling sutures (Figure 9A). The ends of the graft are secured to each other on top of the clavicle with nonabsorbable suture, thus re-creating the anatomical position of the CC ligaments (Figure 9B). This technique combines the benefits of a high primary stability due to the CC fixation device with cortical buttons with the long-term advantages of a biologic graft augmentation and negates the need for larger bone tunnels in the clavicle or coracoid for graft fixation, thus reducing fracture risk.48,92
The Role of the AC Capsule and Ligaments
The contribution of the AC capsule and AC ligaments to translational as well as posterior rotational stability of the AC joint is generally accepted and has been proven in various biomechanical studies reaching back 20 years.12,94 However, scientific interest in the AC capsule and ligaments has substantially grown during the last decade.95–98 Scheibel et al were among the first to demonstrate that clinical outcomes were poorer when horizontal instability persisted, as opposed to persistent vertical instability, when performing AC joint stabilization.99 They concluded, that more attention should be paid to the posterior component of AC joint instability. In the following years, a multitude of techniques were developed to address this issue, mainly focusing on restoring the integrity of the AC capsule and ligaments.90,91,97,100
The addition of an AC cerclage to the CC stabilization lead to superior radiological results with a lower incidence of dynamic posterior instability and improved clinical outcomes in a study performed by Hann et al101. Furthermore, reconstruction of both the AC and CC ligaments proved to be beneficial in a study conducted by Tauber et al in which a single-bundle technique was compared to a triple-bundle technique using hamstring autografts in 26 patients.91 The triple-bundle technique resulted in no significant differences in the Constant and ASES scores after a minimum follow-up of 2 years, yet the AC joint specific scores (ACJI and Taft score) where significantly superior compared to the single-bundle technique.91 Also, the ACJ instability recurrence rate was higher in the single-bundle group (21%) in comparison to the triple-bundle group (8%).91
In a systematic review, CC stabilization with additional augmentation of the AC joint has been shown to improve horizontal stability in both biomechanical and clinical studies compared to CC stabilization alone.102 However, so far no clinical advantage was demonstrated for the additional AC augmentation with respect to the ASES and Constant scores.102
Perspective
In the authors’ opinion, future research regarding AC joint dislocations will need to focus on evaluation, diagnosis and treatment of acute and chronic horizontal instability considering there is no consensus to date.103 Various techniques have been described to address both the AC capsule and ligaments, using different fixation techniques as well as biological augmentation.90,91,101 In a biomechanical study, Dyrna et al demonstrated that all investigated techniques of AC augmentation significantly improved the stability against translational and rotational loading, however, all tested suture constructs were unable to restore the properties of the native AC capsule and ligaments.97 This is plausible, since most techniques involve only 2 points of fixation and can rotate around their own axis at the level of the AC joint. Morikawa et al proposed that the integrity of the AC capsule and ligament is best restored when the entire acromioclavicular ligament complex is repaired (acute) or reconstructed (chronic).98 The same working group recently published a biomechanical study using patch augmentation to reconstruct the AC capsule and ligaments in addition to reconstruction of the CC ligaments.104 They found that the reconstruction of the AC capsule and ligaments with dermal allograft in addition to CC reconstruction restored posterior translational and rotational stability closest to normal.104 However, to date a gold standard has not yet been established.
Conclusion
Treating acute and chronic ACJ injuries is still a challenging task for orthopedic surgeons. Considering these injuries mostly affect younger patients, long-term consequences involving cosmesis and shoulder dysfunction are not yet well understood, and therefore must be anticipated.
The myriad of existing techniques is indicative for the uncertainty regarding this topic and a gold standard has not yet been determined. However, when diagnosed correctly and treated accordingly, results are overall satisfactory.
Disclosure
The position of PCN and LL at the Steadman Philippon Research Institute is supported by Arthrex. PJM is a consultant for and receives royalties from Arthrex, Medbridge, and Springer; owns stock in GameReady and VuMedi; receives support from the Steadman Philippon Research Institute and Vail Valley Medical Center; and has corporate sponsorship from the Steadman Philippon Research Institute, Smith & Nephew, Arthrex, Siemens. The authors report no other conflicts of interest in this work.
References
1. The role of the discs of the sternoclavicular and acromioclavicular joints. DePalma, AF: Clin Orthop Relat Res. 1959;13:7–12.
2. Tillmann BPW. Clinical Anatomy. Stanford (CT): Appleton and Lange; 1998.
3. Warth RJ, Martetschlager F, Gaskill TR, Millett PJ. Acromioclavicular joint separations. Curr Rev Musculoskelet Med. 2013;6(1):71–78. doi:10.1007/s12178-012-9144-9
4. Collins DN. Disorders of the acromioclavicular join. In: Rockwood CA, Wirth MA, Lippitt SB, editors. The Shoulder.
5. Stine IA, Vangsness CT
6. Branch TP, Burdette HL, Shahriari AS, Carter FM
7. Renfree KJ, Wright TW. Anatomy and biomechanics of the acromioclavicular and sternoclavicular joints. Clin Sports Med. 2003;22(2):219–237. doi:10.1016/S0278-5919(02)00104-7
8. Salter EG
9. Nakazawa M, Nimura A, Mochizuki T, Koizumi M, Sato T, Akita K. The orientation and variation of the acromioclavicular ligament: an anatomic study. Am J Sports Med. 2016;44(10):2690–2695. doi:10.1177/0363546516651440
10. Klimkiewicz JJ, Williams GR, Sher JS, Karduna A, Des Jardins J, Iannotti JP. The acromioclavicular capsule as a restraint to posterior translation of the clavicle: a biomechanical analysis. J Shoulder Elbow Surg. 1999;8(2):119–124. doi:10.1016/S1058-2746(99)90003-4
11. Oki S, Matsumura N, Iwamoto W, et al. The function of the acromioclavicular and coracoclavicular ligaments in shoulder motion: a whole-cadaver study. Am J Sports Med. 2012;40(11):2617–2626. doi:10.1177/0363546512458571
12. Fukuda K, Craig EV, An KN, Cofield RH, Chao EY. Biomechanical study of the ligamentous system of the acromioclavicular joint. J Bone Joint Surg Am. 1986;68(3):434–440. doi:10.2106/00004623-198668030-00019
13. Lee KW, Debski RE, Chen CH, Woo SL, Fu FH. Functional evaluation of the ligaments at the acromioclavicular joint during anteroposterior and superoinferior translation. Am J Sports Med. 1997;25(6):858–862. doi:10.1177/036354659702500622
14. Willimon SC, Gaskill TR, Millett PJ. Acromioclavicular joint injuries: anatomy, diagnosis, and treatment. Phys Sportsmed. 2011;39(1):116–122. doi:10.3810/psm.2011.02.1869
15. Mazzocca AD, Spang JT, Rodriguez RR, et al. Biomechanical and radiographic analysis of partial coracoclavicular ligament injuries. Am J Sports Med. 2008;36(7):1397–1402. doi:10.1177/0363546508315200
16. Chahla J, Marchetti DC, Moatshe G, et al. Quantitative assessment of the coracoacromial and the coracoclavicular ligaments with 3-dimensional mapping of the coracoid process anatomy: a cadaveric study of surgically relevant structures. Arthroscopy. 2018;34(5):1403–1411. doi:10.1016/j.arthro.2017.11.033
17. Mazzocca AD, Arciero RA, Bicos J. Evaluation and treatment of acromioclavicular joint injuries. Am J Sports Med. 2007;35(2):316–329. doi:10.1177/0363546506298022
18. Chillemi C, Franceschini V, Dei Giudici L, et al. Epidemiology of isolated acromioclavicular joint dislocation. Emerg Med Int. 2013;2013:171609. doi:10.1155/2013/171609
19. Lynch TS, Saltzman MD, Ghodasra JH, Bilimoria KY, Bowen MK, Nuber GW. Acromioclavicular joint injuries in the National Football League: epidemiology and management. Am J Sports Med. 2013;41(12):2904–2908. doi:10.1177/0363546513504284
20. Johansen JA, Grutter PW, McFarland EG, Petersen SA. Acromioclavicular joint injuries: indications for treatment and treatment options. J Shoulder Elbow Surg. 2011;20:S70–S82. doi:10.1016/j.jse.2010.10.030
21. JD MN T, Sigmond HM. Acromioclavicular separations: useful and practical classification for treatment. Clin Orthop Relat Res. 1963;28:111–119.
22. Rockwood CAJ. Fractures and Dislocations of the Shoulder. Philadelphia (PA): Lippincott; 1984.
23. Beitzel K, Mazzocca AD, Bak K, et al. ISAKOS upper extremity committee consensus statement on the need for diversification of the Rockwood classification for acromioclavicular joint injuries. Arthroscopy. 2014;30(2):271–278. doi:10.1016/j.arthro.2013.11.005
24. Jensen G, Millett PJ, Tahal DS, Al Ibadi M, Lill H, Katthagen JC. Concomitant glenohumeral pathologies associated with acute and chronic grade III and grade V acromioclavicular joint injuries. Int Orthop. 2017;41(8):1633–1640. doi:10.1007/s00264-017-3469-3
25. Beitzel K, Cote MP, Apostolakos J, et al. Current concepts in the treatment of acromioclavicular joint dislocations. Arthroscopy. 2013;29(2):387–397. doi:10.1016/j.arthro.2012.11.023
26. Krul KP, Cook JB, Ku J, Cage JM, Bottoni CR, Tokish JM. Successful conservative therapy in rockwood type V acromioclavicular dislocations. Orthop J Sports Med. 2015. doi:10.1177/2325967115S00017
27. Schlegel TF, Burks RT, Marcus RL, Dunn HK. A prospective evaluation of untreated acute grade III acromioclavicular separations. Am J Sports Med. 2001;29(6):699–703. doi:10.1177/03635465010290060401
28. Ceccarelli E, Bondi R, Alviti F, Garofalo R, Miulli F, Padua R. Treatment of acute grade III acromioclavicular dislocation: a lack of evidence. J Orthop Traumatol. 2008;9(2):105–108. doi:10.1007/s10195-008-0013-7
29. Cook JB, Shaha JS, Rowles DJ, Bottoni CR, Shaha SH, Tokish JM. Clavicular bone tunnel malposition leads to early failures in coracoclavicular ligament reconstructions. Am J Sports Med. 2013;41(1):142–148. doi:10.1177/0363546512465591
30. Korsten K, Gunning AC, Leenen LP. Operative or conservative treatment in patients with Rockwood type III acromioclavicular dislocation: a systematic review and update of current literature. Int Orthop. 2014;38(4):831–838. doi:10.1007/s00264-013-2143-7
31. Mulier T, Stuyck J, Fabry G. Conservative treatment of acromioclavicular dislocation. Evaluation of functional and radiological results after six years follow-up. Acta Orthop Belg. 1993;59(3):255–262.
32. Bontempo NA, Mazzocca AD. Biomechanics and treatment of acromioclavicular and sternoclavicular joint injuries. Br J Sports Med. 2010;44(5):361–369. doi:10.1136/bjsm.2009.059295
33. Alexander OM. Dislocation of the acromioclavicular joint. Radiography. 1949;15(179):260,illust.
34. Alexander OM. Radiography of the acromioclavicular articulation. Med Radiogr Photogr. 1954;30(2):34–39.
35. Weinstein DM, McCann PD, McIlveen SJ, Flatow EL, Bigliani LU. Surgical treatment of complete acromioclavicular dislocations. Am J Sports Med. 1995;23(3):324–331. doi:10.1177/036354659502300313
36. Flint JH, Wade AM, Giuliani J, Rue JP. Defining the terms acute and chronic in orthopaedic sports injuries: a systematic review. Am J Sports Med. 2014;42(1):235–241. doi:10.1177/0363546513490656
37. Muench LN, Kia C, Jerliu A, et al. Functional and radiographic outcomes after anatomic coracoclavicular ligament reconstruction for type III/V acromioclavicular joint injuries. Orthop J Sports Med. 2019;7(11):2325967119884539. doi:10.1177/2325967119884539
38. Rolf O, Hann von Weyhern A, Ewers A, Boehm TD, Gohlke F. Acromioclavicular dislocation Rockwood III-V: results of early versus delayed surgical treatment. Arch Orthop Trauma Surg. 2008;128(10):1153–1157. doi:10.1007/s00402-007-0524-3
39. Song T, Yan X, Ye T. Comparison of the outcome of early and delayed surgical treatment of complete acromioclavicular joint dislocation. Knee Surg Sports Traumatol Arthrosc. 2016;24(6):1943–1950. doi:10.1007/s00167-014-3225-9
40. Ammon JT, Voor MJ, Tillett ED. A biomechanical comparison of Bosworth and poly-L lactic acid bioabsorbable screws for treatment of acromioclavicular separations. Arthroscopy. 2005;21(12):1443–1446. doi:10.1016/j.arthro.2005.09.005
41. Cetinkaya E, Arikan Y, Beng K, Mutlu H, Yalcinkaya M, Uzumcugil O. Bosworth and modified Phemister techniques revisited. A comparison of intraarticular vs extraarticular fixation methods in the treatment of acute Rockwood type III acromioclavicular dislocations. Acta Orthop Traumatol Turc. 2017;51(6):455–458. doi:10.1016/j.aott.2017.09.002
42. Darabos N, Vlahovic I, Gusic N, Darabos A, Bakota B, Miklic D. Is AC TightRope fixation better than Bosworth screw fixation for minimally invasive operative treatment of Rockwood III AC joint injury? Injury. 2015;46(Suppl 6):S113–S118. doi:10.1016/j.injury.2015.10.060
43. Kezunovic M, Bjelica D, Popovic S. Comparative study of surgical treatment of acromioclavicular luxation. Vojnosanit Pregl. 2013;70(3):292–297. doi:10.2298/VSP1303292K
44. Broos P, Stoffelen D, Van de Sijpe K, Fourneau I. Surgical management of complete Tossy III acromioclavicular joint dislocation with the Bosworth screw or the Wolter plate. A critical evaluation. Unfallchirurgie. 1997;23(4):
45. Arirachakaran A, Boonard M, Piyapittayanun P, et al. Post-operative outcomes and complications of suspensory loop fixation device versus hook plate in acute unstable acromioclavicular joint dislocation: a systematic review and meta-analysis. J Orthop Traumatol. 2017;18(4):293–304. doi:10.1007/s10195-017-0451-1
46. Wang G, Xie R, Mao T, Xing S. Treatment of AC dislocation by reconstructing CC and AC ligaments with allogenic tendons compared with hook plates. J Orthop Surg Res. 2018;13(1):175. doi:10.1186/s13018-018-0879-x
47. Millett PJ, Warth RJ, Greenspoon JA, Horan MP. Arthroscopically assisted anatomic coracoclavicular ligament reconstruction technique using coracoclavicular fixation and soft-tissue grafts. Arthrosc Tech. 2015;4(5):e583–e587. doi:10.1016/j.eats.2015.06.007
48. Martetschlager F, Horan MP, Warth RJ, Millett PJ. Complications after anatomic fixation and reconstruction of the coracoclavicular ligaments. Am J Sports Med. 2013;41(12):2896–2903. doi:10.1177/0363546513502459
49. Spiegl UJ, Smith SD, Euler SA, Dornan GJ, Millett PJ, Wijdicks CA. Biomechanical consequences of coracoclavicular reconstruction techniques on clavicle strength. Am J Sports Med. 2014;42(7):1724–1730. doi:10.1177/0363546514524159
50. Menge TJ, Tahal DS, Katthagen JC, Millett PJ. Arthroscopic acromioclavicular joint reconstruction using knotless coracoclavicular fixation and soft-tissue anatomic coracoclavicular ligament reconstruction. Arthrosc Tech. 2017;6(1):e37–e42. doi:10.1016/j.eats.2016.08.035
51. Mori D, Yamashita F, Kizaki K, Funakoshi N, Mizuno Y, Kobayashi M. Anatomic coracoclavicular ligament reconstruction for the treatment of acute acromioclavicular joint dislocation: minimum 10-year follow-up. JB JS Open Access. 2017;2(3):e0007. doi:10.2106/JBJS.OA.16.00007
52. von Heideken J, Bostrom Windhamre H, Une-Larsson V, Ekelund A. Acute surgical treatment of acromioclavicular dislocation type V with a hook plate: superiority to late reconstruction. J Shoulder Elbow Surg. 2013;22(1):9–17. doi:10.1016/j.jse.2012.03.003
53. Borbas P, Churchill J, Ek ET. Surgical management of chronic high-grade acromioclavicular joint dislocations: a systematic review. J Shoulder Elbow Surg. 2019. doi:10.1016/j.jse.2019.03.005
54. Cisneros LN, Reiriz JS. Management of chronic unstable acromioclavicular joint injuries. J Orthop Traumatol. 2017;18(4):305–318. doi:10.1007/s10195-017-0452-0
55. Weaver JK, Dunn HK. Treatment of acromioclavicular injuries, especially complete acromioclavicular separation. J Bone Joint Surg Am. 1972;54(6):1187–1194. doi:10.2106/00004623-197254060-00005
56. Rauschning W, Nordesjo LO, Nordgren B, Sahlstedt B, Wigren A. Resection arthroplasty for repair of complete acromioclavicular separations. Arch Orthop Trauma Surg. 1980;97(3):161–164. doi:10.1007/BF00389721
57. Kawabe N, Watanabe R, Sato M. Treatment of complete acromioclavicular separation by coracoacromial ligament transfer. Clin Orthop Relat Res. 1984;185:222–227.
58. Pavlik A, Csepai D, Hidas P. Surgical treatment of chronic acromioclavicular joint dislocation by modified Weaver-Dunn procedure. Knee Surg Sports Traumatol Arthrosc. 2001;9(5):307–312. doi:10.1007/s001670100222
59. Wellmann M, Lodde I, Schanz S, Zantop T, Raschke MJ, Petersen W. Biomechanical evaluation of an augmented coracoacromial ligament transfer for acromioclavicular joint instability. Arthroscopy. 2008;24(12):1395–1401. doi:10.1016/j.arthro.2008.06.008
60. Kocaoglu B, Ulku TK, Gereli A, Karahan M, Turkmen M. Palmaris longus tendon graft versus modified Weaver-Dunn procedure via dynamic button system for acromioclavicular joint reconstruction in chronic cases. J Shoulder Elbow Surg. 2017;26(9):1546–1552. doi:10.1016/j.jse.2017.01.024
61. Wilson DR, Moses JM, Zilberfarb JL, Hayes WC. Mechanics of coracoacromial ligament transfer augmentation for acromioclavicular joint injuries. J Biomech. 2005;38(3):615–619. doi:10.1016/j.jbiomech.2004.04.015
62. Bostrom Windhamre HA, von Heideken JP, Une-Larsson VE, Ekelund AL. Surgical treatment of chronic acromioclavicular dislocations: a comparative study of Weaver-Dunn augmented with PDS-braid or hook plate. J Shoulder Elbow Surg. 2010;19(7):1040–1048. doi:10.1016/j.jse.2010.02.006
63. Hedtmann A, Fett H, Ludwig J. Treatment of old neglected dislocations of the AC-joint with residual instability and/or secondary osteoarthrosis. Orthopade. 1998;27(8):556–566.
64. Tauber M, Gordon K, Koller H, Fox M, Resch H. Semitendinosus tendon graft versus a modified Weaver-Dunn procedure for acromioclavicular joint reconstruction in chronic cases: a prospective comparative study. Am J Sports Med. 2009;37(1):181–190. doi:10.1177/0363546508323255
65. Lee SJ, Nicholas SJ, Akizuki KH, McHugh MP, Kremenic IJ, Ben-Avi S. Reconstruction of the coracoclavicular ligaments with tendon grafts: a comparative biomechanical study. Am J Sports Med. 2003;31(5):648–655. doi:10.1177/03635465030310050301
66. Harris RI, Wallace AL, Harper GD, Goldberg JA, Sonnabend DH, Walsh WR. Structural properties of the intact and the reconstructed coracoclavicular ligament complex. Am J Sports Med. 2000;28(1):103–108. doi:10.1177/03635465000280010201
67. Lee TQ, Black AD, Tibone JE, McMahon PJ. Release of the coracoacromial ligament can lead to glenohumeral laxity: a biomechanical study. J Shoulder Elbow Surg. 2001;10(1):68–72. doi:10.1067/mse.2001.111138
68. Arrigoni P, Randelli P, Filiputti M, Cabitza P, Vaienti L. The CARE technique: arthroscopic CoracoAcromial ligament RE-attachment. Musculoskelet Surg. 2010;94(Suppl 1):S65–S69. doi:10.1007/s12306-010-0067-6
69. Jiang C, Wang M, Rong G. Proximally based conjoined tendon transfer for coracoclavicular reconstruction in the treatment of acromioclavicular dislocation. J Bone Joint Surg Am. 2007;89(11):2408–2412. doi:10.2106/JBJS.F.01586
70. Hegazy G, Safwat H, Seddik M, Al-Shal EA, Al-Sebai I, Negm M. Modified Weaver-Dunn procedure versus the use of semitendinosus autogenous tendon graft for acromioclavicular joint reconstruction. Open Orthop J. 2016;10:166–178. doi:10.2174/1874325001610010166
71. Kumar V, Garg S, Elzein I, Lawrence T, Manning P, Wallace WA. Modified Weaver-Dunn procedure versus the use of a synthetic ligament for acromioclavicular joint reconstruction. J Orthop Surg (Hong Kong). 2014;22(2):199–203. doi:10.1177/230949901402200217
72. Vargas L. Repair of complete acromioclavicular dislocation, utilizing the short head of the biceps. J Bone Joint Surg Am. 1942;24:772–773.
73. Sloan SM, Budoff JE, Hipp JA, Nguyen L. Coracoclavicular ligament reconstruction using the lateral half of the conjoined tendon. J Shoulder Elbow Surg. 2004;13(2):186–190. doi:10.1016/j.jse.2003.12.002
74. Kim SH, Lee YH, Shin SH, Lee YH, Baek GH. Outcome of conjoined tendon and coracoacromial ligament transfer for the treatment of chronic type V acromioclavicular joint separation. Injury. 2012;43(2):213–218. doi:10.1016/j.injury.2011.08.003
75. Le Hanneur M, Delgrande D, Lafosse T, Werthel JD, Hardy P, Elhassan B. Triple-bundle anatomical reconstruction using the coracoacromial ligament and the short head of biceps tendon to stabilize chronic acromioclavicular joint dislocations: a cadaver feasibility study. Orthop Traumatol Surg Res. 2018;104(1):27–32. doi:10.1016/j.otsr.2017.11.003
76. Le Hanneur M, Thoreson A, Delgrande D, et al. Biomechanical comparison of anatomic and extra-anatomic reconstruction techniques using local grafts for chronic instability of the acromioclavicular joint. Am J Sports Med. 2018;46(8):1927–1935. doi:10.1177/0363546518770603
77. Fauci F, Merolla G, Paladini P, Campi F, Porcellini G. Surgical treatment of chronic acromioclavicular dislocation with biologic graft vs synthetic ligament: a prospective randomized comparative study. J Orthop Traumatol. 2013;14(4):283–290. doi:10.1007/s10195-013-0242-2
78. Fraschini G, Ciampi P, Scotti C, Ballis R, Peretti GM. Surgical treatment of chronic acromioclavicular dislocation: comparison between two surgical procedures for anatomic reconstruction. Injury. 2010;41(11):1103–1106. doi:10.1016/j.injury.2010.09.023
79. Tiefenboeck TM, Boesmueller S, Popp D, et al. The use of the LARS system in the treatment of AC joint instability - Long-term results after a mean of 7.4 years. Orthop Traumatol Surg Res. 2018;104(6):749–754. doi:10.1016/j.otsr.2018.02.010
80. Vitali M, Pedretti A, Naim Rodriguez N, Franceschi A, Fraschini G. Vascular graft employment in the surgical treatment of acute and chronic acromio-clavicular dislocation. Eur J Orthop Surg Traumatol. 2015;25(7):1205–1211. doi:10.1007/s00590-015-1672-8
81. Sinagra ZP, Kop A, Pabbruwe M, Parry J, Clark G. Foreign body reaction associated with artificial LARS ligaments: a retrieval study. Orthop J Sports Med. 2018;6(12):2325967118811604. doi:10.1177/2325967118811604
82. Grutter PW, Petersen SA. Anatomical acromioclavicular ligament reconstruction: a biomechanical comparison of reconstructive techniques of the acromioclavicular joint. Am J Sports Med. 2005;33(11):1723–1728. doi:10.1177/0363546505275646
83. Zhu Y, Hsueh P, Zeng B, et al. A prospective study of coracoclavicular ligament reconstruction with autogenous peroneus longus tendon for acromioclavicular joint dislocations. J Shoulder Elbow Surg. 2018;27(6):e178–e188. doi:10.1016/j.jse.2017.12.009
84. Carofino BC, Mazzocca AD. The anatomic coracoclavicular ligament reconstruction: surgical technique and indications. J Shoulder Elbow Surg. 2010;19(2 Suppl):37–46. doi:10.1016/j.jse.2010.01.004
85. Baran S, Belisle JG, Granger EK, Tashjian RZ. Functional and radiographic outcomes after allograft anatomic coracoclavicular ligament reconstruction. J Orthop Trauma. 2018;32(4):204–210. doi:10.1097/BOT.0000000000001079
86. Lee SJ, Keefer EP, McHugh MP, et al. Cyclical loading of coracoclavicular ligament reconstructions: a comparative biomechanical study. Am J Sports Med. 2008;36(10):1990–1997. doi:10.1177/0363546508324284
87. Thomas K, Litsky A, Jones G, Bishop JY. Biomechanical comparison of coracoclavicular reconstructive techniques. Am J Sports Med. 2011;39(4):804–810. doi:10.1177/0363546510390482
88. Wellmann M, Kempka JP, Schanz S, et al. Coracoclavicular ligament reconstruction: biomechanical comparison of tendon graft repairs to a synthetic double bundle augmentation. Knee Surg Sports Traumatol Arthrosc. 2009;17(5):521–528. doi:10.1007/s00167-009-0737-9
89. Mazzocca AD, Santangelo SA, Johnson ST, Rios CG, Dumonski ML, Arciero RA. A biomechanical evaluation of an anatomical coracoclavicular ligament reconstruction. Am J Sports Med. 2006;34(2):236–246. doi:10.1177/0363546505281795
90. Kibler WB, Sciascia AD, Morris BJ, Dome DC. Treatment of symptomatic acromioclavicular joint instability by a docking technique: clinical indications, surgical technique, and outcomes. Arthroscopy. 2017;33(4):696–708 e692. doi:10.1016/j.arthro.2016.08.023
91. Tauber M, Valler D, Lichtenberg S, Magosch P, Moroder P, Habermeyer P. Arthroscopic stabilization of chronic acromioclavicular joint dislocations: triple- versus single-bundle reconstruction. Am J Sports Med. 2016;44(2):482–489. doi:10.1177/0363546515615583
92. Millett PJ, Horan MP, Warth RJ. Two-year outcomes after primary anatomic coracoclavicular ligament reconstruction. Arthroscopy. 2015;31(10):1962–1973. doi:10.1016/j.arthro.2015.03.034
93. Petri M, Warth RJ, Greenspoon JA, et al. Clinical results after conservative management for grade III acromioclavicular joint injuries: does eventual surgery affect overall outcomes? Arthroscopy. 2016;32(5):740–746. doi:10.1016/j.arthro.2015.11.024
94. Costic RS, Labriola JE, Rodosky MW, Debski RE. Biomechanical rationale for development of anatomical reconstructions of coracoclavicular ligaments after complete acromioclavicular joint dislocations. Am J Sports Med. 2004;32(8):1929–1936. doi:10.1177/0363546504264637
95. Hislop P, Sakata K, Ackland DC, Gotmaker R, Evans MC. Acromioclavicular joint stabilization: a biomechanical study of bidirectional stability and strength. Orthop J Sports Med. 2019;7(4):2325967119836751. doi:10.1177/2325967119836751
96. Dyrna FGE, Imhoff FB, Voss A, et al. The integrity of the acromioclavicular capsule ensures physiological centering of the acromioclavicular joint under rotational loading. Am J Sports Med. 2018;46(6):1432–1440. doi:10.1177/0363546518758287
97. Dyrna F, Imhoff FB, Haller B, et al. Primary stability of an acromioclavicular joint repair is affected by the type of additional reconstruction of the acromioclavicular capsule. Am J Sports Med. 2018;46(14):3471–3479. doi:10.1177/0363546518807908
98. Morikawa D, Dyrna F, Cote MP, et al. Repair of the entire superior acromioclavicular ligament complex best restores posterior translation and rotational stability. Knee Surg Sports Traumatol Arthrosc. 2018;27:3764–3770.
99. Scheibel M, Droschel S, Gerhardt C, Kraus N. Arthroscopically assisted stabilization of acute high-grade acromioclavicular joint separations. Am J Sports Med. 2011;39(7):1507–1516. doi:10.1177/0363546511399379
100. Haber DB, Golijanin P, Stone GL, et al. Primary acromioclavicular-coracoclavicular reconstruction using 2 allografts, tightrope, and stabilization to the acromion. Arthrosc Tech. 2019;8(2):e147–e152. doi:10.1016/j.eats.2018.10.006
101. Hann C, Kraus N, Minkus M, Maziak N, Scheibel M. Combined arthroscopically assisted coraco- and acromioclavicular stabilization of acute high-grade acromioclavicular joint separations. Knee Surg Sports Traumatol Arthrosc. 2018;26(1):212–220. doi:10.1007/s00167-017-4643-2
102. Jordan RW, Malik S, Bentick K, Saithna A. Acromioclavicular joint augmentation at the time of coracoclavicular ligament reconstruction fails to improve functional outcomes despite significantly improved horizontal stability. Knee Surg Sports Traumatol Arthrosc. 2018;27:3747–3763.
103. Aliberti GM, Kraeutler MJ, Trojan JD, Mulcahey MK. Horizontal instability of the acromioclavicular joint: a systematic review. Am J Sports Med. 2019;48:504–510.
104. Morikawa D, Mazzocca AD, Obopilwe E, et al. Reconstruction of the acromioclavicular ligament complex using dermal allograft: a biomechanical analysis. Arthroscopy. 2020;36(1):108–115. doi:10.1016/j.arthro.2019.07.021
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.