Back to Journals » Therapeutics and Clinical Risk Management » Volume 16
Optimal Courses of Chemotherapy Combined with Radiotherapy for Low-Risk Extranodal Natural Killer/T-Cell Lymphoma, Nasal Type: A Propensity Score Matching Analysis
Authors Li J, Li Y, Zeng R, Lin J, Zhong M, Liu X, He Y, He J, Ouyang Z, Huang L, Xiao L, Zhou H
Received 20 March 2020
Accepted for publication 21 August 2020
Published 2 December 2020 Volume 2020:16 Pages 1151—1163
DOI https://doi.org/10.2147/TCRM.S254246
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Deyun Wang
Jin Li,1 Yajun Li,2 Ruolan Zeng,2 Jingguan Lin,1 Meizuo Zhong,3 Xianling Liu,4 Yizi He,2 Junqiao He,2 Zhou Ouyang,2 Lijun Huang,2 Ling Xiao,5 Hui Zhou2
1Department of Comprehensive Chemotherapy/Daytime Chemotherapy, Hunan Cancer Hospital, Changsha, Hunan, People’s Republic of China; 2Department of Lymphoma and Hematology, Hunan Cancer Hospital, Changsha, Hunan, People’s Republic of China; 3Department of Oncology, Xiangya Hospital, Central South University, Changsha, Hunan, People’s Republic of China; 4Department of Oncology, The Second Xiangya Hospital, Central South University, Changsha, Hunan, People’s Republic of China; 5Department of Histology and Embryology, School of Basic Medical Science, Central South University, Changsha, Hunan, People’s Republic of China
Correspondence: Hui Zhou
Department of Lymphoma and Hematology, Hunan Cancer Hospital, Changsha, Hunan, People’s Republic of China
Tel +86 731 89762281
Email [email protected]
Purpose: This retrospective study compared effectiveness between ≤ 4 cycles and ≥ 5 cycles of L-asparaginase/pegaspargase-based chemoradiation in newly diagnosed low-risk extranodal natural killer/T-cell lymphoma (ENKTL), nasal type classified according to the Prognostic Index of Natural Killer (PINK) lymphoma model.
Patients and Methods: Patients were categorized into ≤ 4-cycle (2– 4 chemotherapy cycles, n = 166) and ≥ 5-cycle groups (5– 6 cycles, n = 86). Propensity score matching analysis was used to reduce potential confounding bias between the two groups. Treatment responses, adverse events, and survival outcomes between the two groups were analyzed.
Results: No matter before or after matching (65 in the ≤ 4-cycle group, 65 in the ≥ 5-cycle group), response rates and survival outcomes were similar between the ≤ 4-cycle and ≥ 5-cycle groups. Incidences of grade 1– 2 anemia and transaminase elevation were higher in the ≥ 5-cycle group. After matching, for stage IE disease, there were no differences in response rates and survival outcomes between the two groups. For stage IIE disease, the complete response rate was higher in the ≥ 5-cycle group (72.4% vs 92.6%, p = 0.049), and the 3-year overall survival (65.5% vs 85.2%, p = 0.024) and 3-year progression-free survival (58.6% vs 81.5%, p = 0.027) rates were significantly extended in the ≥ 5-cycle group.
Conclusion: When chemoradiotherapy strategies with L-asparaginase/pegaspargase-based regimens are applied to modern low-risk ENKTL patients classified according to the PINK model, it may be better to moderately extend chemotherapy courses in patients with stage IIE disease.
Keywords: extranodal natural killer/T-cell lymphoma, nasal type, chemotherapy courses, low-risk
Introduction
Extranodal natural killer/T-cell lymphoma (ENKTL), nasal type, is an aggressive subtype of non-Hodgkin lymphoma with a low incidence and is much more prevalent in Asia and Latin America.1 Approximately 70%-80% of patients exhibit lesions within nasal cavities and adjacent structures of the upper aerodigestive tract,2 while others present with skin, gastrointestinal tract, pancreas and lung involvement.3–5 In terms of treatment, chemotherapy combined with radiotherapy is recommended for Ann Arbor stage IE/IIE patients, and stage III/IV patients are mainly treated with systemic chemotherapy.2 Traditional anthracycline-containing regimens for lymphoma, such as CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone) or CHOP-like regimens, are ineffective in ENKTL because P-glycoprotein is expressed on the surface of ENKTL cell membranes and pumps anthracycline out of tumor cells.6–8 The emergence of L-asparaginase has changed the treatment of ENKTL. The GELOX/P-GEMOX regimen (gemcitabine, oxaliplatin, and L-asparaginase/pegaspargase) showed promising complete response (CR) rates of 60%-88% for newly diagnosed ENKTL9–12 and 52%-62% for relapsed/refractory patients.11,13 When the GELOX/P-GEMOX regimen combined with radiotherapy in early-stage patients, CR rates reached 70%-88%.11,14,15 The SMILE regimen (dexamethasone, methotrexate, ifosfamide, L-asparaginase/pegaspargase, and etoposide) reached CR rates of 45%-80%,16,17 and the VLP regimen (vincristine, L-asparaginase/pegaspargase, and prednisone) achieved CR rates of 59%-68% and overall response rates (ORR) of 86%-89% in stage IE-IIE patients with combined modality therapy.18,19
At present, predicting the prognosis of lymphoma patients mainly relies on risk stratification models. Risk stratification is one of the main strategies for the treatment of lymphoma. Currently, there are three main risk stratification systems to predict the prognosis of ENKTL, including the International Prognostic Index (IPI), Korean Prognostic Index (KPI) and Prognostic Index of Natural Killer lymphoma (PINK)/Prognostic Index of Natural Killer lymphoma-EBV (PINK-E). The IPI was derived from diffuse large B-cell lymphoma (DLBCL) and is not suitable for ENKTL because the molecular phenotype, cytogenetics, clinical presentation, disease development and treatment of ENKTL are very different from those of DLBCL.20 The KPI was obtained from patients treated with anthracycline-based regimens and thus cannot be applied in L-asparaginase-era patients.21,22 The PINK/PINK-E model was proposed in 2016 from several non-anthracycline-based retrospective studies and contains the criteria of age >60-year-old, stage III–IV disease, distant lymph node involvement, and non-nasal type disease for the PINK model, with the addition of positive plasma EBV-DNA titer for the PINK-E model.23 The PINK or PINK-E model categorizes ENKTL into 3 risk groups, low-, intermediate- and high-risk, which have corresponding scores of 0, 1, and ≥2 for PINK or 0–1, 2, and ≥3 for PINK-E, respectively, and these groups are correlated with a 3-year overall survival (OS) rates of 81%, 62%, and 25% or 81%, 55%, and 28%, respectively.23 This model has been the unique prognostic model recommended by the National Comprehensive Cancer Network (NCCN) guidelines.24
The population with low-risk score held around half proportion in the PINK/PINK-E model.23 Patients in low-risk ENKTL according to the PINK model belonged to Ann Arbor stage IE-IIE. The NCCN guidelines recommend that stage IE-IIE ENKTL requires 2–6 cycles of chemotherapy combined with radiotherapy, and 4–6 cycles with or without radiation are required for the stage III–IV patients.24 However, few studies have used risk stratification to develop a suitable treatment plan for ENKTL. Hence, we carried out this retrospective study to explore the appropriate chemotherapy course in combination with radiotherapy in low-risk ENKTL according to the PINK model.
Methods
Patients
We enrolled ENKTL patients between 2010 and 2018 from the Hunan Cancer Hospital, the Xiangya Hospital of Central South University and the Second Xiangya Hospital of Central South University. The entry criteria are as follows: (1) a diagnosis of ENKTL by two pathologists according to the current WHO classification of mature B cell, T cell, and NK cell neoplasms;25,26 (2) newly diagnosed ENKTL; (3) low-risk ENKTL according to the PINK model, which meant that the patient’s clinical characteristics must have met the four conditions of age ≤60-year-old, stage IE/IIE disease, no distant lymph node involvement, and nasal type disease; (5) first-line treatment with chemotherapy and radiotherapy; (6) chemotherapy with L-asparaginase/pegaspargase without anthracycline; and (7) receipt of 2–6 cycles of chemotherapy according to the NCCN guidelines’ recommendation.
All enrolled patients were tested with physical examinations, blood routine, blood chemistry, electrocardiogram, bone marrow biopsies and imaging examination. The endoscopy examination included a conchoscope and a nasopharyngolaryngoscope. The imaging examination included enhanced computer tomography (CT) of the neck, chest, abdomen and pelvic cavity, enhanced magnetic resonance imaging (MRI) of the involved sites or whole-body positron emission tomography (PET-CT). Information on sex, primary tumor location, ECOG score, Ann Arbor stage, lactate dehydrogenase (LDH) level, plasma EBV DNA titer, B symptoms, primary tumor invasion (PTI), chemoradiotherapy pattern, chemotherapy regimen, the number of chemotherapy cycles, radiation dose, date of diagnosis, and date of first disease progression or death was collected.
Primary tumor location referred to the initial site of the main symptoms at the time of diagnosis. Nasal site indicated that the primary tumor location was the nasal cavity, with or without other sites or organ involvement. Extranasal site indicated that the primary tumor location involved the upper aerodigestive tract, except for the nasal cavity. PTI was defined as lesions invading adjacent structures or tissues (such as bone or skin) or single or multiple anatomical sites of the upper aerodigestive tract (such as the paranasal sinus, nasopharynx, oropharynx, laryngopharynx, tonsil, and larynx).
This study was approved by the Ethics Committees of Hunan Cancer Hospital, Xiangya Hospital of Central South University and Second Xiangya Hospital of Central South University. All patients’ clinical data were anonymized. All participants signed informed consent. This research abided by the 2008 Declaration of Helsinki.
Treatment, Response and Toxicity Criteria
The selected patients received three chemotherapy regimens containing GELOX, SMILE and VLP. The drugs and dosages of the regimens are listed in Table 1. Radiotherapy was given in a “sequential” pattern – at the initial of treatment, following the completion of chemotherapy, or in a “sandwich” pattern – between cycles of chemotherapy. Patients who received 2–4 cycles of chemotherapy were categorized into the ≤4-cycle group, and patients who received 5–6 cycles were categorized into the ≥5-cycle group. Efficacy evaluation with enhanced CT, enhanced MRI or whole-body PET-CT was conducted after every 2 cycles of chemotherapy, before and after radiotherapy, and after the completion of chemoradiotherapy. The response criteria were evaluated in accordance with the Lugano Response Criteria for non-Hodgkin’s lymphoma.27
 |
Table 1 Chemotherapy Regimens |
Treatment toxicities were evaluated according to the National Cancer Institute’s Common Toxicity Criteria (version 3).28
Statistical Analysis
The differences in baseline clinical features and adverse events between the ≤4-cycle group and the ≥5-cycle group were assessed by the chi-squared test or the Kruskal–Wallis test for categorical variables and two-sided t-tests for continuous variables. Continuous variables were displayed as mean ± standard deviation. Propensity score matching (PSM) analysis was used to effectively balance confounding bias between the ≤4-cycle group and the ≥5-cycle group. PSM accounted for age, sex, ECOG score, primary tumor location, Ann Arbor stage, LDH level, B symptoms, PTI, radiation dose, chemotherapy regimen and chemoradiotherapy pattern. A nearest‐neighbor matching method with a caliper width of 0.10 to generate a ratio of 1:1 matching.
OS was defined as the period from the date of initial diagnosis to the date of follow-up or death. Progression-free survival (PFS) was defined as the interval from the date of initial diagnosis to the date of first progression, first recurrence, or death. The associations between clinical features or chemotherapy cycles and OS and PFS were evaluated by the Kaplan–Meier method and a Log rank test. Univariate and multivariate analyses of prognostic factors for OS and PFS were conducted by Cox regression analysis.
All statistical analyses were calculated by SPSS 24.0 software (IBM Corp., New York, NY, USA). P<0.05 was designated as the level of significance.
Results
Characteristics of the Original Patients
A total of 252 ENKTL patients of low-risk group with PINK model were enrolled in this retrospective study from May 2009 to June 2018, including 166 patients allocated to the ≤4-cycle group and 86 to the ≥5-cycle group. The patient baseline features are listed in Table 2. The median age of all patients was 41-year-old (range 13–60-year-old). The male: female ratio was 2:1. One-hundred and twenty-nine patients were tested with plasma EBV DNA titer at the time of diagnosis, involving 88 in the ≤4-cycle group (27 patients were positive for plasma EBV DNA titer) and 41 in the ≥5-cycle group (22 patients were positive). All these patients belonged to PINK-E low-risk group. Seventy-six, 19, and 4 patients received PET-CT before, during and at the end of treatment, respectively.
 |
Table 2 Patient Characteristics Before and After Propensity Score Matching |
The primary tumor location was more common in nasal cavity, including 191 patients presented with nasal cavity and 61 with extranasal site (nasopharynx n = 43, larynx n = 6, oropharynx n = 5, paranasal sinus n = 4, tonsil n = 3). Patients in the ≤4-cycle group were slightly older (41.0 ± 10.4-year-old vs 36.2 ± 11.6-year-old, p = 0.001) and were much more in sequential pattern (55.4% vs 15.1%, p < 0.001) than those in the ≥5-cycle group. Moreover, compared with the ≤4-cycle group, patients in the ≥5-cycle group presented with more unfavorable prognostic features, including stage IIE (25.3% vs 38.4%, p = 0.031), elevated LDH (19.3% vs 31.4%, p = 0.031), and B symptoms (34.9% vs 47.7%, p = 0.05)
Three different chemotherapy regimens (GELOX, SMILE and VLP) were given to the entire cohort. The median number of chemotherapy cycles was 4 (range 2–6 cycles). In the ≤4-cycle group, 115 patients were assigned to the GELOX regimen, 15 were assigned to the SMILE regimen and 36 were assigned to the VLP regimen. Twenty-eight patients underwent 2 cycles, 29 patients underwent 3 cycles, and 109 patients underwent 4 cycles. In the ≥5-cycle group, 66 patients were allocated to the GELOX regimen, 12 were allocated to the SMILE regimen, and 8 were allocated to the VLP regimen. Twenty patients underwent 5 cycles, and 66 underwent 6 cycles. The median radiation dose was 55 Gy (range 40.0–62.7 Gy).
Characteristics of the Matched Patients
PSM analysis was conducted between the ≤4-cycle and ≥5-cycle groups to balance the potential confounding bias. After matching, a total of 144 patients were matched (72 in the ≤4-cycle group, 72 in the ≥5-cycle group). All baseline clinical characteristics between the ≤4-cycle and ≥5-cycle groups were well balanced (Table 2).
Adverse Events and Response to Treatment Before and After Matching
All patients tolerated treatment-related adverse events, and no one died due to treatment toxicities. Adverse events were classified as hematologic and nonhematologic (Table 3). The most common adverse event was neutropenia and radio-mucositis in the hematologic and nonhematologic categories, respectively. In the original samples, incidences of grade 1–2 anemia and transaminase elevation were higher in the ≥5-cycle group (33.3% vs 61.0%, p < 0.001; 27.1% vs 51.9%, p < 0.001, respectively). After matching, higher rate of grade 1–2 anemia and transaminase elevation were also observed in the ≥5-cycle group (30.2% vs 59.4%, p = 0.002; 24.5% vs 51.6%, p = 0.003, respectively).
 |
Table 3 Adverse Events Before and After Propensity Score Matching |
In the original patient samples, after the completion of chemoradiotherapy, a CR was observed in 227 (90.1%) patients, a partial response (PR) was observed in 9 (3.6%) patients, and progressive disease (PD) was observed in 16 (6.3%) patients. The CR rate was slightly higher in the ≥5-cycle group than that in the ≤4-cycle group (87.3% vs 95.4%, p = 0.044). After matching, the CR rate was higher in the ≥5-cycle group (84.7% vs 95.8%, p = 0.024).
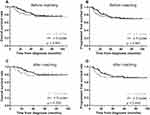
Treatment Failure and Survival Before and After Matching
In the overall study population, as of July 2019, the median follow-up time was 34.6 months (range 2.7–109.6 months). Up to the follow-up time, 48 patients died. Forty-four patients eventually relapsed, of which 13 patients had local recurrence, and 31 patients had systemic recurrence. The 3-year OS rate, 3-year PFS rate and 3-year cumulative recurrence rate were 84.1%, 77.8% and 14.7%, respectively. The 3-year OS rate (82.5% vs 87.2%, p = 0.500) and 3-year PFS rate (77.1% vs 79.1%, p = 0.567) were not significantly different in the ≤4-cycle group and the ≥5-cycle group (Figure 1A and B). The 3-year cumulative recurrence rate was 13.4% and 16.3% in the ≤4-cycle group and the ≥5-cycle group, respectively (p = 0.850).
After matching, the 3-year cumulative recurrence rate (13.9% vs 15.3%, p = 0.886), 3-year OS rate (81.9% vs 88.9%, p = 0.309) and 3-year PFS rate (76.4% vs 80.6%, p = 0.449) were similar in the ≤4-cycle group and the ≥5-cycle group (Figure 1C and D).
Cox Regression Analyses Before and After Matching
For the entire cohort, in the multivariate analysis, a primary tumor location in an extranasal site (OS: HR 1.811, 95% CI 1.008–3.252, p = 0.047; PFS: HR 1.953, 95% CI 1.174–3.250, p = 0.010, respectively), Ann Arbor stage IIE (OS: HR 1.879, 95% CI 1.053–3.352, p = 0.033; PFS: HR 1.723, 95% CI 1.037–2.860, p = 0.036, respectively) and PTI (OS: HR 2.628, 95% CI 1.356–5.091, p = 0.004; PFS: HR 2.609, 95% CI 1.472–4.624, p = 0.001, respectively) were correlated with decreased OS and PFS (Table 4). After matching, PTI independent adversely affected OS (HR 8.362, 95% CI 1.953–35.808, p = 0.004). A primary tumor location in an extranasal site (HR 2.223, 95% CI 1.096–4.507, p = 0.027) and PTI (HR 4.270, 95% CI 1.644–11.089, p = 0.003) were negative predictor factors for PFS (Table 4).
 |
Table 4 Univariate and Multivariate Analyses for Factors Affecting Survival Outcomes Before and After Propensity Score Matching |
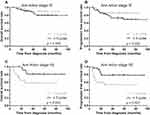
Subgroup Analysis of Ann Arbor Stage After Matching
To examine the response rate and survival outcome between chemotherapy courses and Ann Arbor stage, we further assessed CR rates and Kaplan–Meier curves according to the number of chemotherapy courses stratified by the status of stage. For stage IE ENKTL patients, the CR rate (93.0% vs 97.8%, p = 0.284), 3-year cumulative recurrence rate (9.3% vs 15.6%, p = 0.240), 3-year OS rate (93.0% vs 91.1%, p = 0.336) and 3-year PFS rate (88.4% vs 80.0%, p = 0.220) were similar in the ≤4-cycle group and the ≥5-cycle group (Figure 2A and B). For patients with stage IIE disease, the 3-year cumulative recurrence rate (20.7% vs 14.8%, p = 0.284) was similar in the two groups. While the CR rate was higher in the ≥5-cycle group than in the ≤4-cycle group (72.4% vs 92.6%, p = 0.049). Moreover, the 3-year OS and 3-year PFS rates were significantly extended in the ≥5-cycle group (OS: 65.5% vs 85.2%, p = 0.024; PFS: 58.6% vs 81.5%, p = 0.027) (Figure 2C and D).
Analysis of GELOX/P-GEMOX Patients After Matching
The analysis was separately done for GELOX/P-GEMOX group as this constituted the largest group of patients. The baseline characteristics were comparable between the ≤4-cycle and ≥5-cycle groups (data not shown). The CR rate was higher in the ≥5-cycle group than that in the ≤4-cycle group (88.7% vs 98.2%, p = 0.042). The 3-year cumulative recurrence rate (15.1% vs 16.1%, p = 0.972), 3-year OS rate (81.1% vs 89.3%, p = 0.336) and 3-year PFS rate (77.4% vs 80.4%, p = 0.613) were similar in the ≤4-cycle group and the ≥5-cycle group. For stage IE ENKTL patients, the CR rate (94.1% vs 97.2%, p = 0. 522), 3-year cumulative recurrence rate (11.8% vs 16.7%, p = 0.428), 3-year OS rate (91.2% vs 91.7%, p = 0.586) and 3-year PFS rate (85.3% vs 77.8%, p = 0.375) were similar between the two groups. For patients with stage IIE disease, the 3-year cumulative recurrence rate (21.1% vs 15.0%, p = 0.372) was similar in the two groups. While the CR rate was higher in the ≥5-cycle group than in the ≤4-cycle group (78.9% vs 100.0%, p = 0.030). Moreover, the 3-year OS rate was significantly prolonged in the ≥5-cycle group (63.2% vs 85.0%, p = 0.046). There was an extension trend of the 3-year PFS rate in the ≥5-cycle group (63.2% vs 85.0%, p = 0.077).
Discussion
The optimal courses of chemotherapy for low-risk ENKTL patients who received combined modality therapy have not been well defined. In this multicenter retrospective study, we demonstrated that no matter before or after matching, there were no significant differences in response rates, recurrence rates, and survival outcomes between the ≤4-cycle and the ≥5-cycle groups of low-risk ENKTL patients classified according to the PINK model. After matching, long courses of chemotherapy showed better survival in patients with stage IIE disease than short courses.
Patients in low-risk ENKTL according to the PINK model belonged to stage IE-IIE. Yong Yang et al29 proposed a prognostic model for previously untreated early-stage ENKTL patients in low- and high-risk groups based on 5 factors, including Ann Arbor stage, age, ECOG score, LDH level and presence of PTI. Yong Yang et al developed a risk-adapted therapy model including radiotherapy alone for the low-risk group and radiotherapy followed by chemotherapy for the high-risk group. Another retrospective multicenter study explored radiotherapy for early-stage ENKTL in elderly patients based on the age-adjusted prognostic model (4 risk factors including Ann Arbor stage II, ECOG score ≥2, elevated LDH, and presence of PTI) from the study of Yong Yang et al.30 After receiving radiotherapy, regardless of if patients were treated with radiation alone or in combination with chemotherapy, low-risk and high-risk patients showed a good prognosis in terms of PFS within 24 months, and their survival rates were the same as those of the average Chinese population. In our study, we adopted the PINK model because 81% of patients who received chemotherapy in the study of Yong Yang et al received anthracycline-based regimens. Second, the PINK prognostic model is currently the only recommended model in the NCCN guidelines.24 In contrast to patients with other lymphomas, ENKTL patients have poor responses to anthracycline-containing regimens. L-asparaginase/pegaspargase is effective for ENKTL and shows outstanding efficiency in relapsed or refractory patients.31,32 Radiotherapy is a core part of the treatment strategy for early-stage ENKTL. However, radiotherapy alone is not sufficient to improve survival because a large number of patients will suffer local and systemic recurrence after radiotherapy alone.33,34 Therefore, the combination of L-asparaginase/pegaspargase chemotherapy with radiotherapy has been proposed as a first-line treatment for previously untreated limited-stage ENKTL. Moreover, the NCCN guidelines also propose that patients with stage IE-IIE disease undergo combined modality therapy (concurrent, sequential or sandwich chemoradiation).24 Hence, patients who received radiotherapy alone or chemotherapy alone were not included in our study. In the future, we need larger retrospective studies or prospective studies to establish more complete prognostic models and risk-adapted therapy strategies.
Table 5 lists retrospective and prospective studies on ≤4 cycles or ≥5 cycles of chemotherapy combined with chemotherapy in stage IE-IIE ENKTL. Our results were comparable with the previous studies except for two by Jieun Lee et al,35 and Jian Zang et al.36 In Jieun Lee et al’s study, 9 of 27 patients were administered only concurrent chemoradiotherapy without consolidation chemotherapy. In Jian Zang et al’s research, more than half of patients received anthracycline-containing regimens. Moreover, when combined with radiation, excessive courses of chemotherapy did not improve survival might be due to the potential increasing toxicities. These speculations might be the reasons why the CR rates and survival outcomes of above two studies were much inferior than ours. X. Wu et al’s study37 showed that there was no significant difference in survival between patients receiving <4 cycles of chemotherapy and those receiving ≥4 cycles. All patients in X. Wu et al’s study received CHOP regimen. Furthermore, the study cohort included stage III–IV patients, and the treatment manners covered chemoradiotherapy, radiotherapy alone and palliative therapy. Another retrospective study cohort of ENKTL patients was grouped into >8 courses (n=37), 6–8 courses (n=18) and <6 courses (n=14) of chemotherapy, the corresponding 5-year OS rate was 63.5%, 45.1% and 22.9%, respectively (p = 0.030).38 The early-stage patients in this study received combined modality therapy. While the majority of patients were given CHOP or CHOP-like regimens, and advanced stage patients consisted the proportion of 15%.
 |
Table 5 Chemoradiotherapy for Stage IE-IIE Extranodal NK/T Cell Lymphoma, Nasal Type |
There were several limitations in this study. Firstly, this was a retrospective study to provide relatively lower power evidence than a prospective study. Secondly, the study population scale was comparatively small. The patients’ data were not collected from multicenter in a practical sense, which meant the institutions from different provinces and countries. Thirdly, the chemotherapy regimens and radiation doses in the study were heterogeneous. Lastly, PET-CT scan was not used as a regular examination method to assess the baseline lesions and response efficacy.
Conclusion
When chemoradiotherapy strategies with L-asparaginase/pegaspargase-based regimens are applied to modern low-risk ENKTL patients classified according to the PINK model, it may be better to moderately extend chemotherapy courses in patients with stage IIE disease. Prospective clinical studies and larger retrospective studies are required to further determine applicable early-stage risk stratification models and the appropriate number of cycles of chemotherapy for low-risk ENKTL patients.
Acknowledgments
This study was supported by grants from the Hunan Provincial Key Research and Development Program for Social Development (2017SK2133), the Science and Technology Program of Changsha, China (kq1706041), and the Science and Technology Program of Health Commission of Hunan Province (B20180496).
Disclosure
The authors have no conflicts of interest to declare.
References
1. Vose J, Armitage J, Weisenburger D. International peripheral T-cell and natural killer/T-cell lymphoma study: pathology findings and clinical outcomes. J clin oncol. 2008;26(25):4124–4130.
2. Suzuki R. NK/T cell lymphoma: updates in therapy. Current Hematologic Malignancy Reports. 2018;13(1):7–12. doi:10.1007/s11899-018-0430-5
3. Kwong YL. Natural killer-cell malignancies: diagnosis and treatment. Leukemia. 2005;19(12):2186–2194. doi:10.1038/sj.leu.2403955
4. Haverkos BM, Pan Z, Gru AA, et al. Extranodal NK/T cell lymphoma, nasal type (ENKTL-NT): an update on epidemiology, clinical presentation, and natural history in North American and European cases. Current Hematologic Malignancy Reports. 2016;11(6):514–527. doi:10.1007/s11899-016-0355-9
5. Yamaguchi M, Suzuki R, Oguchi M. Advances in the treatment of extranodal NK/T-cell lymphoma, nasal type. Blood. 2018;131(23):2528–2540. doi:10.1182/blood-2017-12-791418
6. Yamaguchi M, Kita K, Miwa H, et al. Frequent expression of P-glycoprotein/MDR1 by nasal T-cell lymphoma cells. Cancer. 1995;76(11):2351–2356. doi:10.1002/1097-0142(19951201)76:11<2351::AID-CNCR2820761125>3.0.CO;2-1
7. Wang B, Lu JJ, Ma X, et al. Combined chemotherapy and external beam radiation for stage IE and IIE natural killer T-cell lymphoma of nasal cavity. Leukemia Lymphoma. 2007;48(2):396–402. doi:10.1080/10428190601059795
8. Kim BS, Kim TY, Kim CW, et al. Therapeutic outcome of extranodal NK/T-cell lymphoma initially treated with chemotherapy–result of chemotherapy in NK/T-cell lymphoma. Acta oncologica. 2003;42(7):779–783.
9. Guo HQ, Liu L, Wang XF, et al. Efficacy of gemcitabine combined with oxaliplatin, L-asparaginase and dexamethasone in patients with newly-diagnosed extranodal NK/T-cell lymphoma. Molecular Clinical Oncology. 2014;2(6):1172–1176. doi:10.3892/mco.2014.368
10. Wang JH, Wang H, Wang YJ, et al. Analysis of the efficacy and safety of a combined gemcitabine, oxaliplatin and pegaspargase regimen for NK/T-cell lymphoma. Oncotarget. 2016;7(23):35412–35422. doi:10.18632/oncotarget.8643
11. Jing XM, Zhang ZH, Wu P, et al. Efficacy and tolerance of pegaspargase, gemcitabine and oxaliplatin with sandwiched radiotherapy in the treatment of newly-diagnosed extranodal nature killer (NK)/T cell lymphoma. Leuk Res. 2016;47:26–31. doi:10.1016/j.leukres.2016.05.004
12. Li JW, Li YJ, Zhong MZ, Liu XL, Li J. Efficacy and tolerance of GELOXD/P-GEMOXD in newly diagnosed nasal-type extranodal NK/T-cell lymphoma: A multicenter retrospective study. Eur J Haematol. 2018;100(3):247–256.
13. Wang JH, Wang L, Liu CC, et al. Efficacy of combined gemcitabine, oxaliplatin and pegaspargase (P-gemox regimen) in patients with newly diagnosed advanced-stage or relapsed/refractory extranodal NK/T-cell lymphoma. Oncotarget. 2016;7(20):29092–29101. doi:10.18632/oncotarget.8647
14. Wang H, Wuxiao ZJ, Zhu J, et al. Comparison of gemcitabine, oxaliplatin and L-asparaginase and etoposide, vincristine, doxorubicin, cyclophosphamide and prednisone as first-line chemotherapy in patients with stage IE to IIE extranodal natural killer/T-cell lymphoma: a multicenter retrospective study. Leukemia Lymphoma. 2015;56(4):971–977.
15. Bi XW, Xia Y, Zhang WW, et al. Radiotherapy and PGEMOX/GELOX regimen improved prognosis in elderly patients with early-stage extranodal NK/T-cell lymphoma. Ann Hematol. 2015;94(9):1525–1533. doi:10.1007/s00277-015-2395-y
16. Yang L, Liu H, Xu XH, et al. Retrospective study of modified SMILE chemotherapy for advanced-stage, relapsed, or refractory extranodal natural killer (NK)/T cell lymphoma, nasal type. Medical Oncol. 2013;30(4):720. doi:10.1007/s12032-013-0720-7
17. Qi S, Yahalom J, Hsu M, et al. Encouraging experience in the treatment of nasal type extra-nodal NK/T-cell lymphoma in a non-Asian population. Leukemia Lymphoma. 2016;57(11):2575–2583. doi:10.1080/10428194.2016.1180689
18. Huang L, Yuan B, Wu H, et al. Comparative study of l-asparaginase-based lop regimen over chop regimen before radiotherapy for stage iie extranodal nasal type NK/T cell lymphoma: a study of 2 centers. Clin Lymphoma Myeloma Leuk. 2017;17(3):152–158. doi:10.1016/j.clml.2016.12.003
19. Hu Y, Chen M, Song Y, et al. Study of l-asparaginase, vincristine, and dexamethasone combined with intensity-modulated radiation therapy in early-stage nasal NK/T-cell lymphoma. Am J Clin Oncology. 2019.
20. Chim CS, Ma SY, Au WY, et al. Primary nasal natural killer cell lymphoma: long-term treatment outcome and relationship with the International Prognostic Index. Blood. 2004;103(1):216–221. doi:10.1182/blood-2003-05-1401
21. Lee J, Suh C, Park YH, et al. Extranodal natural killer T-cell lymphoma, nasal-type: a prognostic model from a retrospective multicenter study. J clin oncol. 2006;24(4):612–618. doi:10.1200/JCO.2005.04.1384
22. Yamaguchi M, Takata K, Yoshino T, et al. Prognostic biomarkers in patients with localized natural killer/T-cell lymphoma treated with concurrent chemoradiotherapy. Cancer Science. 2014;105(11):1435–1441. doi:10.1111/cas.12526
23. Kim SJ, Yoon DH, Jaccard A, et al. A prognostic index for natural killer cell lymphoma after non-anthracycline-based treatment: a multicentre, retrospective analysis. Lancet Oncology. 2016;17(3):389–400. doi:10.1016/S1470-2045(15)00533-1
24. NCCN guidelines version 2. 2019 T-cell lymphomas. Availbale from: https://www.nccn.org/professionals/physician_gls/default.aspx.
25. Campo E, Swerdlow SH, Harris NL, et al. The 2008 WHO classification of lymphoid neoplasms and beyond: evolving concepts and practical applications. Blood. 2011;117(19):5019–5032. doi:10.1182/blood-2011-01-293050
26. Cazzola M. Introduction to a review series: the 2016 revision of the WHO classification of tumors of hematopoietic and lymphoid tissues. Blood. 2016;127(20):2361–2364. doi:10.1182/blood-2016-03-657379
27. Cheson BD, Fisher RI, Barrington SF, et al. Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: the Lugano classification. J clin oncol. 2014;32(27):3059–3068. doi:10.1200/JCO.2013.54.8800
28. Trotti A, Colevas AD, Setser A, et al. CTCAE v3.0: development of a comprehensive grading system for the adverse effects of cancer treatment. Semin Radiat Oncol. 2003;13(3):176–181. doi:10.1016/S1053-4296(03)00031-6
29. Yang Y, Zhu Y, Cao JZ, et al. Risk-adapted therapy for early-stage extranodal nasal-type NK/T-cell lymphoma: analysis from a multicenter study. Blood. 2015;126(12):
30. Chen B, Zhu SY, Shi M, et al. Risk-dependent curability of radiotherapy for elderly patients with early-stage extranodal nasal-type NK/T-cell lymphoma: A multicenter study from the China Lymphoma Collaborative Group (CLCG). Cancer Med. 2018;7(12):5952–5961.
31. Yong W, Zheng W, Zhu J, et al. L-asparaginase in the treatment of refractory and relapsed extranodal NK/T-cell lymphoma, nasal type. Ann Hematol. 2009;88(7):647–652. doi:10.1007/s00277-008-0669-3
32. Jaccard A, Gachard N, Marin B, et al. Efficacy of L-asparaginase with methotrexate and dexamethasone (AspaMetDex regimen) in patients with refractory or relapsing extranodal NK/T-cell lymphoma, a Phase 2 study. Blood. 2011;117(6):1834–1839. doi:10.1182/blood-2010-09-307454
33. Cheung MM, Chan JK, Lau WH, Ngan RK, Foo WW. Early stage nasal NK/T-cell lymphoma: clinical outcome, prognostic factors, and the effect of treatment modality. Int J Radiat Oncol Biol Phys. 2002;54(1):182–190. doi:10.1016/S0360-3016(02)02916-4
34. Kim GE, Lee SW, Chang SK, et al. Combined chemotherapy and radiation versus radiation alone in the management of localized angiocentric lymphoma of the head and neck. Radiother Oncol. 2001;61(3):261–269. doi:10.1016/S0167-8140(01)00428-5
35. Lee J, Kim CY, Park YJ, Lee NK. Sequential chemotherapy followed by radiotherapy versus concurrent chemoradiotherapy in patients with stage I/II extranodal natural killer/T-cell lymphoma, nasal type. Blood Res. 2013;48(4):274–281. doi:10.5045/br.2013.48.4.274
36. Zang J, Li C, Luo SQ, et al. Early radiotherapy has an essential role for improving survival in patients with stage I-II nasal-type of NK/T cell lymphoma treated with L-asparaginase-containing chemotherapy–a single institution experience. Ann Hematol. 2015;94(4):583–591. doi:10.1007/s00277-014-2244-4
37. Wu X, Li P, Zhao J, et al. A clinical study of 115 patients with extranodal natural killer/T-cell lymphoma, nasal type. Clinical Oncology. 2008;20(8):619–625. doi:10.1016/j.clon.2008.05.011
38. Xu Y, Wang J, Zhang W, et al. Extended course and increased dose of initial chemotherapy for extranodal nasal type natural killer/t (nk/t)-cell lymphoma in patients <60 years old: a single-center retrospective cohort study. Medical Science Monitor. 2016;22:4297–4311.
39. Ma X, Guo Y, Pang Z, et al. A randomized Phase II study of CEOP with or without semustine as induction chemotherapy in patients with stage IE/IIE extranodal NK/T-cell lymphoma, nasal type in the upper aerodigestive tract. Radiother Oncol. 2009;93(3):492–497. doi:10.1016/j.radonc.2009.08.045
40. Kim SJ, Yang DH, Kim JS, et al. Concurrent chemoradiotherapy followed by L-asparaginase-containing chemotherapy, VIDL, for localized nasal extranodal NK/T cell lymphoma: CISL08-01 phase II study. Ann Hematol. 2014;93(11):1895–1901. doi:10.1007/s00277-014-2137-6
41. Ke QH, Zhou SQ, Du W, et al. Concurrent IMRT and weekly cisplatin followed by GDP chemotherapy in newly diagnosed, stage IE to IIE, nasal, extranodal NK/T-Cell lymphoma. Blood Cancer J. 2014;4:e267. doi:10.1038/bcj.2014.88
42. Oh D, Ahn YC, Kim SJ, Kim WS, Ko YH. Concurrent chemoradiation therapy followed by consolidation chemotherapy for localized extranodal natural killer/t-cell lymphoma, nasal type. Int J Radiat Oncol Biol Phys. 2015;93(3):677–683. doi:10.1016/j.ijrobp.2015.07.2267
43. Michot JM, Mazeron R, Danu A, et al. Concurrent etoposide, steroid, high-dose ara-c and platinum chemotherapy with radiation therapy in localised extranodal natural killer (NK)/T-cell lymphoma, nasal type. European j Cancer. 2015;51(16):2386–2395. doi:10.1016/j.ejca.2015.07.009
44. Yoon DH, Kim SJ, Jeong SH, et al. Phase II trial of concurrent chemoradiotherapy with L-asparaginase and MIDLE chemotherapy for newly diagnosed stage I/II extranodal NK/T-cell lymphoma, nasal type (CISL-1008). Oncotarget. 2016;7(51):85584–85591. doi:10.18632/oncotarget.11319
45. Dong LH, Zhang LJ, Wang WJ, et al. Sequential DICE combined with l-asparaginase chemotherapy followed by involved field radiation in newly diagnosed, stage IE to IIE, nasal and extranodal NK/T-cell lymphoma. Leukemia Lymphoma. 2016;57(7):1600–1606. doi:10.3109/10428194.2015.1108415
46. Jiang M, Zhang L, Xie L, et al. A phase II prospective study of the “Sandwich” protocol, L-asparaginase, cisplatin, dexamethasone and etoposide chemotherapy combined with concurrent radiation and cisplatin, in newly diagnosed, I/II stage, nasal type, extranodal natural killer/T-cell lymphoma. Oncotarget. 2017;8(30):50155–50163.
47. Qi F, Wang WH, He XH, et al. Phase 2 study of first-line intensity modulated radiation therapy followed by gemcitabine, dexamethasone, and cisplatin for high-risk, early stage extranodal nasal-type nk/t-cell lymphoma: the green study. Int J Radiat Oncol Biol Phys. 2018;102(1):61–70. doi:10.1016/j.ijrobp.2018.05.046
48. Qi F, Chen B, Wang J, et al. Upfront radiation is essential for high-risk early-stage extranodal NK/T-cell lymphoma, nasal type: comparison of two sequential treatment modalities combining radiotherapy and GDP (gemcitabine, dexamethasone, and cisplatin) in the modern era. Leukemia Lymphoma. 2019;60(11):2679–2688. doi:10.1080/10428194.2019.1599111
49. Lee KW, Yun T, Kim DW, et al. First-line ifosfamide, methotrexate, etoposide and prednisolone chemotherapy ± radiotherapy is active in stage I/II extranodal NK/T-cell lymphoma. Leukemia Lymphoma. 2006;47(7):1274–1282. doi:10.1080/10428190600562823
50. Lin N, Song Y, Zheng W, et al. A prospective phase II study of L-asparaginase- CHOP plus radiation in newly diagnosed extranodal NK/T-cell lymphoma, nasal type. J Hematol Oncol. 2013;6:44. doi:10.1186/1756-8722-6-44
51. Aviles A, Neri N, Fernandez R, Huerta-Guzman J, Nambo MJ. Combined therapy in untreated patients improves outcome in nasal NK/T lymphoma: results of a clinical trial. Medical Oncol. 2013;30(3):637. doi:10.1007/s12032-013-0637-1
52. Zheng W, Gao Y, Ke X, et al. PEG-L-CHOP treatment is safe and effective in adult extranodal NK/T-cell lymphoma with a low rate of clinical hypersensitivity. BMC Cancer. 2018;18(1):910. doi:10.1186/s12885-018-4782-y
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.