Back to Journals » International Medical Case Reports Journal » Volume 9
Optical coherence tomography findings of bilateral foveal leukemic infiltration
Authors Le J, Braich P, Brar V
Received 6 January 2016
Accepted for publication 9 March 2016
Published 8 August 2016 Volume 2016:9 Pages 237—240
DOI https://doi.org/10.2147/IMCRJ.S103723
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
John Q Le,1 Puneet S Braich,2 Vikram S Brar2
1Department of Internal Medicine, 2Department of Ophthalmology, Virginia Commonwealth University, Richmond, VA, USA
Abstract: We report a case of a 59-year-old man with a history of atypical chronic myelogenous leukemia who presented with a several-week history of decreased vision in both eyes. His clinical examination revealed bilateral foveal infiltration, which was also demonstrated on optical coherence tomography. After a failed induction with imatinib (Gleevec®), he was treated with omacetaxine (Synribo®) with an appropriate hematologic response. As his leukemia improved with chemotherapy, his retinal lesions regressed as demonstrated by serial optical coherence tomography and fundus photographs, with near complete restoration of foveal architecture.
Keywords: leukemia, leukemic retinopathy, leukemic infiltration, OCT
Introduction
Leukemic retinopathy refers to numerous, abnormal fundoscopic findings that stem from complications of leukemia, such as anemia, thrombocytopenia, and hyperviscosity.1,2 The most prevalent of such findings include intraretinal hemorrhages, cotton-wool spots, and white-centered hemorrhages. These hemorrhages are typically found in the posterior pole and particularly in the inner layers with focal destruction.1 While ocular involvement can range from 39% to 53% of cases in patients with acute leukemia,1 only a small portion of these findings are a result of direct leukemic infiltration. In this case report, we present a rare scenario of bilateral, foveal leukemic infiltration, and vision loss in a patient with atypical chronic myelogenous leukemia who eventually had regression of these foveal lesions and recovered vision after chemotherapy. The clinical response was documented on serial spectral domain optical coherence tomography (OCT) imaging, with image registration.
Case report
A 59-year-old man with a history of asthma, hypertension, and newly diagnosed atypical chronic myelogenous leukemia, which was BCR-ABL receptor-negative, presented to the eye clinic with a several-week history of decreased vision, floaters and photopsia, and central scotomas. His best corrected visual acuity was 20/80 oculus uterque (OU), and intraocular pressures were 13 and 14 mmHg, respectively. His pupils were symmetric and reacted briskly to light without a relative afferent pupillary defect. His external slit-lamp examination was remarkable only for nuclear sclerosis OU. His dilated fundus exam revealed a posterior vitreous detachment in his right eye without vitreous hemorrhage. His cup-to-disk ratio was 0.85 with healthy rims and bilateral peripapillary atrophy. Scattered white-centered hemorrhages were present throughout the fundus. Focal areas of leukemic infiltration were present in the fovea OU (Figure 1) with larger leukemic lesions temporally in right eye and inferotemporally in the left eye. OCT scans of the macula revealed hyperreflective lesions in the inner retina as well as a separate outer retinal lesion in the right eye (Figure 2). The left eye demonstrated a larger inner retinal lesion with smaller adjacent lesions, without an outer retinal component. There was no evidence of choroidal involvement or subretinal fluid.
The patient was diagnosed with chronic phase chronic myelogenous leukemia (BCR-ABL-negative) by bone marrow aspiration and biopsy with an overall cellularity of 95%. The myeloid series was increased and left shifted with full maturation. Flow cytometry with CD34 staining showed <5% blasts. Cytogenetic studies showed 47, XXY. Unlike acute lymphoblastic leukemia, central nervous system involvement in chronic myelogenous leukemia is rare,3 and in the absence of headaches or other focal neurological findings, he did not undergo further analysis of his cerebrospinal fluid. The patient’s white blood cell count was noted to be 265.7×109/L (reference range 4,500–10,000×109/L) with a hemoglobin of 7.8 g/dL (reference range 13.3–17.2 g/dL) and platelets of 199×109/L (reference range 179×109/L–373×109/L). Differential revealed 31% neutrophils, 5% bands, 48% myelocytes, 2% metamyelocytes, 1% basophils, 1% eosinophils, 2% monocytes, 4% promyelocytes, and 5% blasts.
One month into his induction therapy with imatinib (Gleevec®; Novartis International AG., Basel, Switzerland) 400 mg daily, he developed lower extremity edema and failed to show response to therapy; his white blood cell count remained elevated at 395.3×109/L. His oncologist subsequently initiated therapy with omacetaxine (Synribo®; Teva Pharmaceutical Industries., Petah Tikva, Israel) and demonstrated a rapid and effective hematologic response. As his white blood cell decreased, he was noted to have improved vision at subsequent ophthalmologic visits. His dilated fundus examinations demonstrated a gradual regression of his leukemic lesions at his 2 and 3 month follow up visits (Figure 1B and Figure 1C respectively). At 12 months from his initial presentation, there was complete resolution of his bilateral foveal infiltration, cotton-wool spots, and retinal hemorrhages (Figure 1D). OCT scans revealed restored foveal contour with focal defects at the photoreceptor outer segments (Figure 2C). By this point, the patient had successfully completed his induction therapy and was undergoing maintenance therapy. His best corrected visual acuity was 20/30 OU. The Virginia Commonwealth University (VCU) Institutional Review Board (IRB) does not require approval for this case report as it does not constitute a human research subject that involves an investigational article. Written patient consent was obtained in compliance with VCU Health System, to use ophthalmic imaging and data in the publication of this case report.
Comment
Regardless of the type of leukemia, ocular manifestations can be found in up to half of the cases.1 Most of these manifestations, such as retinal hemorrhages, represent conditions associated with leukemia as opposed to direct leukemic infiltration. A prior report has demonstrated the time domain OCT findings of leukemic infiltration of the choroid with overlying serous detachment of the neurosensory retina, which resolved following successful treatment.4 Further in another report, spectral domain OCT revealed the presence of choroidal thickening in addition to associated serous retinal detachment in a patient with recurrent leukemia.5
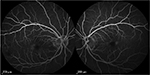
Our case is the first to demonstrate leukemic infiltration of the retina using OCT. It describes not only resolution of retinal hemorrhages associated with leukemia but also resolution of leukemic infiltration of the macula as well, following successful systemic treatment. Leukemic infiltration, as demonstrated in our scans, represents lesions of uniform reflectivity and can involve all layers of the retina. At month 3, there are persistent hemorrhages present in the foveal regions in both eyes (Figure 1C), with complete resolution of the infiltrates and the corresponding hyperreflective lesions on OCT on the right (Figure 2C). This indicates that the leukemic lesions are distinct entities from retinal hemorrhages on OCT. Finally, there was no consecutive atrophy of the inner retinal layers upon resolution, but there were focal disruptions of the photoreceptor outer segments where there was initial leukemic involvement. This was supported by fluorescein angiography, which was performed at 3 months from presentation, where there was preservation of the perifoveal capillary bed (Figure 3).
This report demonstrates a rare case of leukemic infiltration of the macula, documented with serial OCTs. Infiltration of the retina can be identified and monitored using OCT and should be employed in cases of suspected leukemic retinopathy.
Disclosure
The authors report no conflicts of interest in this work.
References
Schachat AP, Andrew PS, Jan A. Markowitz, JA. Graham. Ophthalmic manifestations of leukemia. Arch Ophthalmol. 1989;107(5):697–700. | ||
Carraro MC, Rossetti L, Gerli GC. Prevalence of retinopathy in patients with anemia or thrombocytopenia. Eur J Haematol. 2001;67(4):238–244. | ||
Lindhorst SM, Lopez RD, Sanders RD. An unusual presentation of chronic myelogenous leukemia: a review of isolated central nervous system relapse. J Natl Compr Canc Netw. 2013;11(7):745–750. | ||
Candoni A,Simeone E,Bandello F,Fanin R. Leukaemic infiltration of the retina at onset of Philadelphia-positive acute lymphoblastic leukaemia revealed by stratus optical coherence tomography. Br J Haematol. 2006;133(5):45. | ||
Chalam K, Patel CJ, Edwards J, Murthy RK. T-cell leukemia. Ophthalmology. 2012;119(8):1713–1714.e1. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.