Back to Journals » Clinical Ophthalmology » Volume 17
Open Globe Injury in a Tertiary Hospital of Northern Thailand: No Vision Survival and Ocular Trauma Score
Authors Porapaktham T, Choovuthayakorn J , Nanegrungsunk O, Phinyo P , Tanasombatkul K, Watanachai N , Kunavisarut P, Chaikitmongkol V, Patikulsila D
Received 15 December 2022
Accepted for publication 19 January 2023
Published 25 January 2023 Volume 2023:17 Pages 365—373
DOI https://doi.org/10.2147/OPTH.S401643
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Tuangprot Porapaktham,1 Janejit Choovuthayakorn,1 Onnisa Nanegrungsunk,1 Phichayut Phinyo,2– 4 Krittai Tanasombatkul,2,3 Nawat Watanachai,1 Paradee Kunavisarut,1 Voraporn Chaikitmongkol,1 Direk Patikulsila1
1Department of Ophthalmology, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand; 2Clinical Epidemiology and Clinical Statistics Center, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand; 3Department of Family Medicine, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand; 4Musculoskeletal Science and Translational Research (MSTR), Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand
Correspondence: Janejit Choovuthayakorn, Department of Ophthalmology, Faculty of Medicine, Chiang Mai University, 110 Intavaroros Road, Maung, Chiang Mai, 50200, Thailand, Tel +66 53 935512, Fax +66 53 936121, Email [email protected]
Purpose: To determine characteristics and factors associated with no vision survival (included no light perception, enucleation, and evisceration) following open globe injury (OGI) and to correlate the proportion of final vision to predictive values of ocular trauma score (OTS).
Patients and Methods: The medical records of consecutive patients diagnosed as OGI between January 2015 and December 2020 were retrospectively reviewed. Data collected included demographics, mechanisms and modes of injuries, ophthalmic presentations, managements, and visual outcomes at the final visit.
Results: Three hundred and seventy-one patients with a mean (standard deviation, SD) age of 44.0 (17.4) years were included. Male with workplace injury was the most frequent scenario. High-velocity metallic objects were the predominant causative materials. Following treatments, fifty-six eyes (14.9%) obtained no vision survival. Factors associated with no vision survival following OGI were low presenting vision, globe perforation, larger wound, presence of relative afferent pupillary defect, retinal detachment, and vitreous hemorrhage. Compared to OTS predictive values, eyes in OTS categories 1 and 2 had a lower proportion of no vision survival.
Conclusion: This study identified the importance of workplace injuries. Overall, there were comparable final visions between OTS and this study. However, a reduced proportion of no vision survival among severely injured eyes signifies the challenges of OGI management.
Keywords: open globe injury, visual outcomes, characteristics, no vision survival
Introduction
Globally, eye injury remains a major etiology of acquired visual impairments.1–4 As a consequence, its magnitude and trend have been evaluated over time in numerous publications.5–14 Based on a recent meta-analysis that combined information from 20 population-based studies, an annual prevalence of 7.5 per 100 persons for eye injury and 4.5 per 1000 persons for eye injury-related visual impairment were shown.15 Furthermore, in a recent analysis using the Korean National Health Insurance claims database, an annual incidence of 1.99 per 100,000 persons for primary closure of cornea or sclera and 0.39 per 100,000 persons for intraocular foreign body (IOFB) removal were noted.16
Following management, a number of open globe injury (OGI) patients attain unfavorable vision or no vision survival. These impairments not only lead to limitations in visual tasks but also impact other aspects of their lives, including quality of life, psychological distress, and mental health.17–19 Therefore, several studies have been performed to determine factors and/or models for predicting eye injury-related visual outcomes.22,23 Given the changing trends of daily life behaviors, information regarding the pattern, characteristics, and visual outcomes following OGI in each geographic location should be updated.
This study aimed to explore the characteristics and related factors for having no vision survival following OGI in a tertiary referral center located within a non-industrial area. The data would be valuable for determining, counselling, and decision-making for OGI management and prevention.
Materials and Methods
This retrospective medical chart review was conducted in accordance with the tenets of the Declaration of Helsinki. The protocol was approved by Chiang Mai University Hospital ethics committee, Faculty of Medicine, Thailand (Study code: OPT 2564-07933). Due to anonymized data collection, the need for informed consent was waived. The data accessed complied with all relevant data protection and data privacy regulations.
Consecutive OGI patients who presented and were managed at this hospital between January 2015 and December 2020 identified from the operation lists. The retrieved data included demographics, circumstances causing injury, presenting ophthalmic findings, management, and visual status at the most recent visits. Patients who had follow-up visits less than 3 months (except those who underwent eye removal procedures or had no indication for further visits) and had pre-existing ophthalmic diseases precluding OGI-related visual impairment estimation were excluded. All datasets were de-identified and gathered in Microsoft Excel Spreadsheet.
Mechanisms of OGI were classified according to a Standardized Classification of Ocular Trauma as rupture (caused by a blunt-object injury) and penetration, perforation and retained IOFB (caused by a sharp-object injury).24 Locations of injury were defined by the most posterior part of the eye wall with a full-thickness opening into 3 zones according to a System for Classifying Mechanical Injuries of the Eye (zone I: wound involving cornea and limbus, zone II: wound involving anterior 5 mm of sclera from the limbus, and zone III: wound involving sclera beyond 5 mm from the limbus).25
During the study period, 376 OGI patients were identified; however, 5 patients did not return at their follow-up visits and were excluded. Demographics and presenting ophthalmic characteristics of the excluded patients were similar to the study group, except for smaller wound sizes and more anterior wound locations.
Statistical Analysis
Descriptive analyses were expressed as mean (SD) for continuous data and percentage for categorical data. Visual acuity (VA) at the final visit was categorized as vision survival (eyes having Snellen VA from 20/20 to the light perception (LP)), and no vision survival (eyes having no light perception (NLP) or eyes that were removed). The associations between final vision status and predictors including demographics (gender, age) and ophthalmic presentations (presenting VA, wound location and extent, lens injury, presence of relative afferent pupillary defect (RAPD), retinal detachment (RD), vitreous hemorrhage (VH), IOFB, endophthalmitis, and eyelid laceration) were explored using multivariable logistic regression. Generalized estimating equations were performed to correct the correlation between two eyes. Snellen VA was converted to the Logarithm of the Minimum Angle of Resolution (LogMAR) VA for an analysis. Based on the OTS scoring system, the actual and predicted final VA in each category was assessed by testing for equality of proportion. Statistical analysis was calculated using the STATA program and a P value less than 0.05 was considered significant.
Results
Overall, three hundred and seventy-one patients (377 eyes) with a mean (SD) age of 44.0 (17.4) years (ranged 4 to 81 years) and a median (interquartile range, IQR) follow-up of 8 (4 to 13) months were included in the study. Three hundred and thirty-five (90.3%) patients were males and six (1.6%) had bilateral eye injuries (three related to fireworks, two related to traffic accidents, and one related to a blasting injury). The majority of the patients (257 patients, 69.3%) were injured at their workplaces, and most injuries were associated with agricultural activities (135 patients (36.4%) related to lawn mowing and 55 patients (14.8%) related to gardening/farming). A high-velocity metallic object (133 patients, 35.9%) represented the most frequent causative material. In each year, there were no differences in the number of injuries by month (p = 0.148) as shown in Figure 1. The median (IQR) time interval from injury to the hospital was 48 (9 to 96) hours. Table 1 summarizes demographics and details of circumstances causing OGI.
 |
Table 1 Patients’ Demographics and Circumstances Causing Open Globe Injury by Final Vision Status |
 |
Figure 1 Distribution of open globe injury by month and year. |
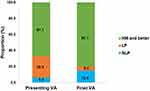
Regarding presenting ocular characteristics, most injuries were confined within zone I (249 eyes, 66.1%) and IOFB (162 eyes, 43.0%) was the most prevalent mechanism of injury. A mean (SD) presenting VA was 2.2 (0.7) LogMAR (Snellen equivalent of 20/3170) with 253 eyes (67.1%) had VA of HM and better, and 23 eyes (6.1%) had NLP. Other presenting ocular characteristics are described in Table 2. Of note, RAPD could not be determined in 4 cases (8 eyes) with bilateral involvement (2 eyes with no vision survival and 6 eyes with vision survival).
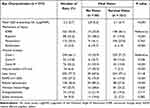 |
Table 2 Characteristics of Eyes Sustaining Open Globe Injury by Final Vision Status |
Regarding surgical interventions, with a mean (SD) of 2.1 (0.9) operations per eye, 289 (76.7%) eyes required pars plana vitrectomy (PPV). Due to severe structural damage, 10 eyes (10/377, 2.7%) that had presenting vision of NLP could not be successfully repaired and underwent primary enucleation/evisceration. Following treatments, due to pain and/or severe infection, subsequent enucleations/eviscerations were also performed in 22/377 (5.8%) eyes with NLP vision (7 with presenting NLP, 12 worsening from LP, and 3 worsening from HM). The final vision of the study population improved to a mean (SD) of 1.4 (1.1) LogMAR (Snellen equivalent of 20/500). Three hundred and two eyes (80.1%) achieved final vision of HM and better, whereas 56 (14.9%) eyes had no vision survival (32 eyes were removed, 20 worsened to NLP, and 4 remained NLP despite treatments). The distribution of presenting and final vision is illustrated in Figure 2. During follow-up, none developed sympathetic ophthalmia.
By an exploratory multivariable analysis (Table 3), presenting VA worse than HM, perforation, wound extent ≥10 mm, presence of RAPD, RD, and VH were significant factors related to no vision survival following OGI. Following OTS categories, the distribution of visual outcomes for patients in this study compared to those in the OTS study is demonstrated in Table 4. Of note, the lower proportion of no vision survival for eyes having OTS categories 1 and 2 and a concordance in proportion for eyes having OTS categories 3 and 4 to predictive values of OTS were observed.
 |
Table 3 Multivariable Exploratory Analysis for Factors Associated with No Vision Survival Following Open Globe Injury |
 |
Table 4 Distribution of Eyes with No Vision Survival at Final Follow Up Compared Between Ocular Trauma Score Study and This Study |
Discussion
This study, consistent with others, described that male and workplace settings were the major risks for the occurrence of OGI in a tertiary hospital-based setting. Interestingly, the main circumstances of injury in this study population were exposed to activities involving projectile metallic objects, particularly lawn mowing. For visual consequences, approximately one-fifth of injured eyes had no vision survival. In addition, a reduction in the proportion of no vision survival for eyes having OTS categories 1 and 2 was observed. This information supports the practical importance for clinicians and patients to carefully assess and determine the management for severe eye injuries.
Several studies have evaluated the characteristics of OGI and similarly described a more likelihood of OGI in working males.23,26–28 Nevertheless, a wide range of injury settings and circumstances were observed across publications. In a study that evaluated OGI in rural West India, the authors found the most prevalent injuries occurred in young workers who had been struck by wooden sticks or flying stones during agricultural work, whereas a study from central India reported a predominant injury in young workers who had been injured from industrial work.26,27 In a recent multicenter study, a distinct distribution of mechanisms, locations, and objects causing OGI varied between different geographical centers.29 Similar to our study, Beshay et al reported the majority of OGI occurred in middle-aged adults who were exposed to work involving high-velocity metallic objects.30 The three main activities related to no vision survival in this study were construction, gardening/farming, and mowing. This information is valuable to establish more effective educational and/or preventive strategies among this specific population. Educational programs to increase an awareness of using safety eye protection in hazardous environments, as well as training programs to improve compliance with using these protections during work at all times, are important issues to be emphasized.
Predictors for vision survival following OGI have been explored in previous studies.31–35 Ocular trauma score (OTS), proposed in 2002, is one of the most commonly used systems to estimate the probability of vision survival following closed and open globe injuries. The influencing factors used to estimate OTS categories and the likelihood of vision are presenting VA, mechanism of injury, endophthalmitis, RD, and presence of RAPD.34 Additionally, Schmidt et al proposed that by using the classification and regression tree analysis model, presenting VA, presence of RAPD, eyelid laceration, and wound location were significant predictive factors for no vision survival following OGI.31 Another study by Han et al found that presenting VA, wound length, and RD were significant independent factors for no vision survival.35 Further exploration in a cohort of severe OGI presenting with NLP vision provided evidence that choroidal and ciliary body damage, and close-funneled RD were predictors for no vision survival.36 By an exploratory analysis, this study found that presenting VA, mechanism of injury, larger wound size, RD, presence of RAPD, and VH were influencing factors associated with no vision survival. The diversities of predictive factors between publications may be partly attributed to differences in the nature of injuries, study domains, and duration of follow-up. In addition, the development of ophthalmic microsurgical instruments might lead to these variations. Due to the retrospective design and the long period of this study, further prospective studies that collect data from similar time points and surgical techniques may help clarify these associations.
More than half of OGI in this study were classified as having OTS categories 1 or 2 which carried worse visual prognoses. The use of OTS for predicting visual outcomes has been reported in many OGI situations.20,37–39 Some studies described similar proportions of no vision survival by each category to those in the OTS study.20,39,40 However, some reports revealed a lower proportion of no vision survival compared to OTS, particularly for eyes in the more severe OTS categories.35,41–43 In agreement, this study noted a lower proportion of no vision survival for eyes in OTS categories 1 and 2, while a concordance in proportions was observed in eyes in OTS categories 3 and 4. In a recent study, the authors proposed that by using a modified OTS with the addition of orbital fracture as another predictive factor, the accuracy of visual prediction for eyes with OTS category 1 improved.43 Nevertheless, with a retrospective design and a small sample size, this modified OTS system requires further validation. As there was a reduction in no vision survival for severe eye injuries, careful decision-making for the management of OGI should be highlighted.
Limitations of this study included data extraction based on a tertiary center setting; therefore, it might not represent OGI in other settings. Furthermore, based on retrospective analysis, the bias of data incompleteness such as drug and/or alcohol use and the use of eye protection could not be extracted in every case. In addition, a number of patients were sent back to their primary physicians if no further eye injury-related interventions were required, which might affect the estimation of long-term injury-related complications. The exploration using prospective data collection and/or standardized ocular trauma registry in further studies might overcome these limitations.44 Nonetheless, information from this study supports the evidence of no vision survival following OGI in agricultural settings and defines some potential points that are essential for preventing eye injuries and their visual prognoses.
Conclusion
This study identifies that activities involving high-velocity objects remain a potential cause of OGI. Poor presenting vision, perforation mechanism, larger wound size, presence of RAPD, RD, and VH were important for predicting no vision survival following OGI. A reduction in the proportion of no vision survival in severely injured eyes after OGI signifies the impact of OGI management on visual outcomes.
Acknowledgments
We would like to thank Barbara Metzler, a director of the Chiang Mai University English Language Team, for helping with manuscript editing.
Funding
The authors did not receive any funding for this study.
Disclosure
Dr Onnisa Nanegrungsunk is speaker for Allergan and Roche; reports support for meeting registration and traveling from Bayer and Novartis; advisory board and speaker for Santen, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Négrel AD, Thylefors B. The global impact of eye injuries. Ophthalmic Epidemiol. 1998;5:143–169. doi:10.1076/opep.5.3.143.8364
2. Zhou J, Wang FH, Lu H, Liang YB, Wang NL; Group HES. Ocular trauma in a rural population of North China: the Handan eye study. Biomed Environ Sci. 2015;28:495–501. doi:10.3967/bes2015.071
3. Keel S, Xie J, Foreman J, Taylor HR, Dirani M. The prevalence of vision loss due to ocular trauma in the Australian national eye health survey. Injury. 2017;48(11):2466–2469. doi:10.1016/j.injury.2017.09.020
4. Wong MY, Man RE, Gupta P, et al. Prevalence, subtypes, severity and determinants of ocular trauma: the Singapore Chinese eye study. Br J Ophthalmol. 2018;102:204–209. doi:10.1136/bjophthalmol-2017-310564
5. Wong TY, Tielsch JM. A population-based study on the incidence of severe ocular trauma in Singapore. Am J Ophthalmol. 1999;128:345–351. doi:10.1016/s0002-9394(99)00167-1
6. Loon SC, Tay WT, Saw SM, Wang JJ, Wong TY. Prevalence and risk factors of ocular trauma in an urban South-East Asian population: the Singapore Malay eye study. Clin Exp Ophthalmol. 2009;37:362–367. doi:10.1111/j.1442-9071.2009.02035.x
7. Morris DS, Willis S, Minassian D, Foot B, Desai P, MacEwen CJ. The incidence of serious eye injury in Scotland: a prospective study. Eye. 2014;28:34–40. doi:10.1038/eye.2013.213
8. Chang YS, Teng YT, Huang YH, et al. Author correction: major ocular trauma in Taiwan: 2002–2004 versus 2012–2014. Sci Rep. 2018;8:13566. doi:10.1038/s41598-018-31648-3
9. Iftikhar M, Latif A, Farid UZ, Usmani B, Canner JK, Shah SMA. Changes in the incidence of eye trauma hospitalizations in the United States from 2001 through 2014. JAMA Ophthalmol. 2019;137:48–56. doi:10.1001/jamaophthalmol.2018.4685
10. Lee JS, Chen WM, Huang LH, et al. Epidemiology of outpatient and inpatient eye injury in Taiwan: 2000, 2005, 2010, and 2015. PLoS One. 2020;15:e0235208. doi:10.1371/journal.pone.0235208
11. Ojuok E, Uppuluri A, Langer PD, Zarbin MA, Thangamathesvaran L, Bhagat N. Demographic trends of open globe injuries in a large inpatient sample. Eye. 2021;35:2270–2276. doi:10.1038/s41433-020-01249-4
12. Wang W, Zhou Y, Zeng J, Shi M, Chen B. Epidemiology and clinical characteristics of patients hospitalized for ocular trauma in South-Central China. Acta Ophthalmol. 2017;95:e503–e510. doi:10.1111/aos.13438
13. Okamoto Y, Morikawa S, Okamoto F, et al. Clinical characteristics and outcomes of open globe injuries in Japan. Jpn J Ophthalmol. 2019;63:109–118. doi:10.1007/s10384-018-0638-x
14. Court JH, Lu LM, Wang N, McGhee CNJ. Visual and ocular morbidity in severe open-globe injuries presenting to a regional eye centre in New Zealand. Clin Exp Ophthalmol. 2019;47:469–477. doi:10.1111/ceo.13439
15. Swain T, McGwin G. The prevalence of eye injury in the United States, estimates from a meta-analysis. Ophthalmic Epidemiol. 2020;27(3):186–193. doi:10.1080/09286586.2019.1704794
16. Kwon JW, Choi MY, Bae JM. Incidence and seasonality of major ocular trauma: a nationwide population-based study. Sci Rep. 2020;10:10020. doi:10.1038/s41598-020-67315-9
17. Keles A, Karayagmurlu A, Yetkin E, Sonmez K, Karatepe MS, Karaman SK. Development of posttraumatic stress disorder and depression after open globe injury in adults. Graefes Arch Clin Exp Ophthalmol. 2022. doi:10.1007/s00417-022-05792-6
18. Yüksel H, Türkcü FM, Ahin M, et al. Vision-related quality of life in patients after ocular penetrating injuries. Arq Bras Oftalmol. 2014;77:95–98. doi:10.5935/0004-2749.20140024
19. Karaman S, Ozkan B, Gok M, et al. Effect of eye trauma on mental health and quality of life in children and adolescents. Int Ophthalmol. 2017;37:539–544. doi:10.1007/s10792-016-0301-9
20. Sobaci G, Akin T, Erdem U, Uysal Y, Karagül S. Ocular trauma score in deadly weapon-related open-globe injuries. Am J Ophthalmol. 2006;141:760–761. doi:10.1016/j.ajo.2005.11.002
21. Agrawal R, Rao G, Naigaonkar R, Ou X, Desai S. Prognostic factors for vision outcome after surgical repair of open globe injuries. Indian J Ophthalmol. 2011;59:465–470. doi:10.4103/0301-4738.86314
22. Acar U, Tok OY, Acar DE, Burcu A, Ornek F. A new ocular trauma score in pediatric penetrating eye injuries. Eye. 2011;25:370–374. doi:10.1038/eye.2010.211
23. Ustaoglu M, Karapapak M, Tiryaki S, et al. Demographic characteristics and visual outcomes of open globe injuries in a tertiary hospital in Istanbul, Turkey. Eur J Trauma Emerg Surg. 2020;46(3):549–556. doi:10.1007/s00068-018-1060-2
24. Kuhn F, Morris R, Witherspoon CD, Heimann K, Jeffers JB, Treister G. A standardized classification of ocular trauma. Ophthalmology. 1996;103:240–243. doi:10.1016/S0161-6420(96)30710-0
25. Pieramici DJ, Sternberg P, Aaberg TM, et al. A system for classifying mechanical injuries of the eye (globe). The Ocular Trauma Classification Group. Am J Ophthalmol. 1997;123(6):820–831. doi:10.1016/S0002-9394(14)71132-8
26. Toh ZH, Shah SM, Chua CH, Hoskin AK, Agrawal R, Shah M. International Globe and Adnexal Trauma Epidemiology Study (IGATES): visual outcomes in open globe injuries in rural West India. Eye. 2022;37(1):88–96. doi:10.1038/s41433-021-01895-2
27. Toh ZH, Agrawal S, Raje D, Hoskin A, Agrawal R, Khandelwal R. International globe and adnexal trauma epidemiology study (IGATES): a report from Central India on visual outcome in open globe injuries and correlation with ocular trauma score. Int Ophthalmol. 2020;40(11):2797–2806. doi:10.1007/s10792-020-01429-x
28. Cro S, Partington G, Cornelius VR, et al. Presenting clinical characteristics of open globe injuries in ocular trauma: baseline analysis of cases in the ASCOT national clinical trial. Eye. 2022. doi:10.1038/s41433-022-02206-z
29. Hoskin AK, Low R, Sen P, et al. Epidemiology and outcomes of open globe injuries: the international globe and adnexal trauma epidemiology study (IGATES). Graefes Arch Clin Exp Ophthalmol. 2021;259(11):3485–3499. doi:10.1007/s00417-021-05266-1
30. Beshay N, Keay L, Dunn H, Kamalden TA, Hoskin AK, Watson SL. The epidemiology of open globe injuries presenting to a tertiary referral eye hospital in Australia. Injury. 2017;48(7):1348–1354. doi:10.1016/j.injury.2017.04.035
31. Schmidt GW, Broman AT, Hindman HB, Grant MP. Vision survival after open globe injury predicted by classification and regression tree analysis. Ophthalmology. 2008;115(1):202–209. doi:10.1016/j.ophtha.2007.04.008
32. Feng K, Hu YT, Ma Z. Prognostic indicators for no light perception after open-globe injury: eye injury vitrectomy study. Am J Ophthalmol. 2011;152(4):654–662.e2. doi:10.1016/j.ajo.2011.04.004
33. Han YS, Kavoussi SC, Adelman RA. Visual recovery following open globe injury with initial no light perception. Clin Ophthalmol. 2015;9:1443–1448. doi:10.2147/OPTH.S87852
34. Kuhn F, Maisiak R, Mann L, Mester V, Morris R, Witherspoon CD. The Ocular Trauma Score (OTS). Ophthalmol Clin North Am. 2002;15(2):163–165, vi. doi:10.1016/S0896-1549(02)00007-X
35. Han SB, Yu HG. Visual outcome after open globe injury and its predictive factors in Korea. J Trauma. 2010;69(5):E66–E72. doi:10.1097/TA.0b013e3181cc8461
36. Feng K, Shen L, Pang X, et al. Case-control study of risk factors for no light perception after open-globe injury: eye injury vitrectomy study. Retina. 2011;31:1988–1996. doi:10.1097/IAE.0b013e318213d8c7
37. Man CY, Steel D. Visual outcome after open globe injury: a comparison of two prognostic models--the ocular trauma score and the classification and regression tree. Eye. 2010;2:84–89. doi:10.1038/eye.2009.16
38. Guven S. Verification of ocular trauma score for intraocular foreign bodies in lethal-weapon-related ocular injuries. Mil Med. 2020;185(7–8):e1101–e1105. doi:10.1093/milmed/usaa042
39. Shrestha SM, Anthony CL, Justin GA, et al. Factors affecting final functional outcomes in open-globe injuries and use of ocular trauma score as a predictive tool in Nepalese population. BMC Ophthalmol. 2021;21:69. doi:10.1186/s12886-021-01819-4
40. Unal MH, Aydin A, Sonmez M, Ayata A, Ersanli D. Validation of the ocular trauma score for intraocular foreign bodies in deadly weapon-related open-globe injuries. Ophthalmic Surg Lasers Imaging. 2008;39(2):121–124. doi:10.3928/15428877-20080301-15
41. Agrawal R, Wei HS, Teoh S. Prognostic factors for open globe injuries and correlation of ocular trauma score at a tertiary referral eye care centre in Singapore. Indian J Ophthalmol. 2013;61:502–506. doi:10.4103/0301-4738.119436
42. Unver YB, Kapran Z, Acar N, Altan T. Ocular trauma score in open-globe injuries. J Trauma. 2009;66:1030–1032. doi:10.1097/TA.0b013e3181883d83
43. Zhou Y, Chang P, Abdelmalik B, Mayer Z, Shah A, Steigleman WA. Prognosis of open globe injuries at a tertiary referral center: the modified Florida ocular trauma score. Am J Ophthalmol. 2022;244:152–165. doi:10.1016/j.ajo.2022.08.015
44. Ng SMS, Low R, Hoskin AK, et al. The application of clinical registries in ophthalmic trauma-the International Globe and Adnexal Trauma Epidemiology Study (IGATES). Graefes Arch Clin Exp Ophthalmol. 2022;260:1055–1067. doi:10.1007/s00417-021-05493-6
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.