Back to Journals » Cancer Management and Research » Volume 11
Oncologic outcome of parotid mucoepidermoid carcinoma in pediatric patients
Authors Fang Q , Liu F, Seng D
Received 30 October 2018
Accepted for publication 31 December 2018
Published 29 January 2019 Volume 2019:11 Pages 1081—1085
DOI https://doi.org/10.2147/CMAR.S192788
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Kenan Onel
Qigen Fang,1 Fei Liu,2 Dongjie Seng3
1Department of Head and Neck, Affiliated Cancer Hospital of Zhengzhou University, Henan Cancer Hospital, Zhengzhou, China; 2Department of Oral Medicine, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, China; 3Department of Ear, Nose, and Throat, Affiliated Children Hospital of Zhengzhou University, Zhengzhou, China
Background: The goal of this study was to investigate the long-term oncologic outcome of parotid mucoepidermoid carcinoma (MEC) in pediatric patients.
Patients and methods: Patients <19 years old who were diagnosed with MEC from January 1990 to December 2017 were retrospectively enrolled in this study. The main analyzed indexes included intraparotid node (IPN) metastasis, neutrophil-tolymphocyte ratio (NLR), loco-regional control (LRC), and disease-specific survival (DSS) rates.
Results: A total of 73 patients were enrolled. IPN metastasis occurred in 13 (17.8%) patients; the mean value of the NLR was 2.48 (range: 1.3–6.1). Loco-regional recurrence occurred in 12 patients, and 7 patients died of the disease. The 10-year LRC and DSS rates were 83% and 88%, respectively. IPN metastasis remained significantly related to recurrence in both univariate and Cox model analyses; a high NLR was significantly associated with recurrence in the univariate analysis but not in the Cox model. IPN metastasis remained significantly related to disease-related death in both the univariate and Cox model analyses; a high NLR was not associated with the DSS in univariate analysis.
Conclusion: The long-term survival rate was relatively favorable in pediatric MEC. IPN metastasis was an independent risk factor for loco-regional recurrence and DSS. The role of the NLR in predicting survival in parotid cancer requires more research.
Keywords: pediatric cancer, salivary cancer, parotid cancer, mucoepidermoid carcinoma
Introduction
Parotid tumors are uncommon in children and adolescents, 10%–50% of which are malignant;1–3 the most common malignant lesion is MEC,4–12 and it is challenging to develop a consensus on treatment owing to the rarity of the disease. For cancers of the major salivary glands, surgical resection has been the primary treatment modality,12 but the optimal degree of surgery remains unclear. In previous reports, various surgical procedures, including superficial and total parotidectomy, have been described.4–16 Therefore, in the current study, we aimed to investigate the long-term oncologic outcome in pediatric patients with parotid MEC treated by total parotidectomy.
Patients and methods
The Zhengzhou University institutional research committee approved our study, and all the legal guardians, including the parents, provided written informed consent for any patient under the age of 18; this study was conducted in accordance with the Declaration of Helsinki. All methods were performed in accordance with the relevant guidelines and regulations.
From January 1990 to December 2017, a consecutive series of pediatric patients (age <19 years old) diagnosed with primary parotid MEC were retrospectively enrolled. All pathologic sections were re-reviewed. Related information regarding age, sex, pretreatment NLR, TNM stage (according to AJCC 2017), operative record, pathologic report, recurrence, and disease-related death was extracted and analyzed.
In our cancer center, frozen sections of primary tumors are routinely reviewed, and if malignancy is highly suspected, total parotidectomy is conducted. NLR is defined as absolute neutrophil count divided by absolute lymphocyte count within 2 weeks before the initial treatment.17,18 The cutoff value calculated from the ROC curve, tertiles, or median in previous studies varied from 1.98 to 5,17,18 and the standardized cutoff value is unknown; therefore, in the current study, the cutoff value was defined as the mean value of NLR.
The Kaplan–Meier method was used to evaluate the LRC and DSS rates. The Cox model was used to determine the independent risk factors for the LRC and DSS rates. A P<0.05 was considered to be significant, and all statistical analyses were performed in SPSS 20.0.
Results
A total of 73 pediatric patients (43 females and 30 males) were enrolled with a mean age of 14.3 (range: 8–18) years. Preoperative fine-needle biopsy of the primary tumor was conducted in 20 (27.4%) patients. Tumor stages of the patients were distributed as follows: T1 in 40 (54.8%) cases, T2 in 19 (26.0%) cases, T3 in 10 (13.7%) cases, and T4 in 4 (5.5%) cases. All patients underwent total parotidectomy with preservation of the facial nerve except in 3 cases with severe tumor invasion; negative margins were achieved in 68 (93.2%) patients. The mean value of the NLR was 2.48 (range: 1.3–6.1).
The neck status was evaluated by physical examination (ultrasound and CT or MRI) with or without fine-needle puncture biopsy. Fifteen patients were classified as having clinically positive necks, and these patients underwent neck dissection; 12 of these patients had pathologic neck disease. The mean number of metastatic nodes was 1.4 (range: 1–3).
Transient facial paralysis occurred in 29 (39.7%) patients, and permanent paralysis was noted in 5 (5.5%) patients. There were no surgical site infections. Eleven (15.1%) patients complained of the occurrence of Frey syndrome. The grades of the tumors were distributed as follows: low in 42 (57.5%) patients, moderate in 20 (27.4%) patients, and high in 11 (15.1%) patients. Perineural infiltration was reported in 11 (15.1%) patients, and lymphovascular invasion (LVI) was reported in 9 (12.3%) patients.
IPN metastasis occurred in 13 (17.8%) patients, consisting of 7 females and 6 males; the mean age was 14.2 (range: 9–17) years, and the mean value of the NLR was 2.78 (range: 1.4–6.0). The disease stages were distributed as follows: I in two cases, II in three cases, III in five cases, and IV in three cases. Perineural infiltration was reported in four patients, and LVI was reported in four patients. Negative margins were achieved in ten patients. The grade of the tumor was distributed as follows: low in five cases, moderate in five cases, and high in three cases (Table 1).
During our follow-up after a mean time of 95.4 (range: 13–286) months, 15 patients underwent postoperative radiotherapy, and 4 patients also received adjuvant chemotherapy. Seven patients died of the disease. Loco-regional recurrence was noted in 12 patients, and there were no distant metastases.
The 10-year LRC rate was 83%, and the median time to recurrence was 27 (range: 13–80) months. IPN metastasis remained significantly related to recurrence in both univariate and Cox model analyses, and a high NLR was significantly associated with recurrence in univariate analysis but not in the Cox model (Table 2).
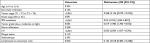  | Table 2 Risk factors for loco-regional recurrence in pediatric patients with parotid cancer Abbreviations: IPN, intraparotid node; LVI, lymphovascular invasion. |
The 10-year DSS rate was 88%. IPN metastasis remained significantly related to the disease-related death rate in both univariate and Cox model analyses; however, a high NLR was not associated with the DSS in the univariate analysis (Table 3).
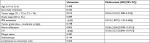  | Table 3 Risk factors for disease-related death in pediatric patients with parotid cancer Abbreviations: IPN, intraparotid node; LVI, lymphovascular invasion. |
Discussion
MEC is the most common pediatric parotid cancer,2 but because of the rarity of pediatric salivary tumors, there are hardly any large sample size studies. There is no agreement regarding the best treatment procedure; the current study was the first to focus on the long-term oncologic outcomes of pediatric parotid MEC patients.
A relatively high incidence of transient facial nerve paralysis was noted in the current study, a finding that conflicted with those of previous reports.1,2 The difference might be explained by the fact that total parotidectomy was the only surgical procedure performed, and any minor neurological dysfunction was defined as transient facial nerve paralysis in the current study.
The prognosis of pediatric salivary malignancy was reported to be favorable, but disease-specific death has also been noted.4,6,9,11,12 Nevertheless, in the current study, the 10-year DSS survival rate was as high as 88%, and only a small number of patients received postoperative radiotherapy which could increase disease control.13 This finding somewhat conflicted with other studies. Possible explanations for this conflicting finding include: first, unlike other reports, only MEC was analyzed in the current study, and most of the disease was low-grade, thus having a relatively better prognosis; second, negative margins were achieved in 93.2% of the patients, and total parotidectomy was performed in all patients; in other reports, positive margins and superficial parotidectomies were common.6,9,11,12
Loco-regional recurrence was one of the common treatment failure patterns.6,9,11,12 Cockerill et al6 reported that 14 (26.9%) out of 52 patients had a recurrence. In the current study, recurrence was noted in only 12 (16.4%) patients, slightly better than those of other reports.6,11 The favorable LRC rate was mainly attributed to the standard surgical procedure consisting of total parotidectomy only and the effort to achieve complete excision. In other studies,6,9,11,12 various surgical procedures were performed, even including enucleation, and as many as 38.1% of the patients had positive margins. In our cancer center, complete resection of the tumor is one of the main goals for cancer treatment. Otherwise, there is a higher possibility of recurrence; moreover, second surgeries have lower rates of success and higher rates of operation-related complications.
The role of IPN metastasis in survival remains unclear. Cockerill et al6 reported that 11% of their patients had positive intraparotid lymph nodes. However, in that study, only 65% of the patients underwent total parotidectomy, and there were nodes in both superficial and deep parotid glands; therefore, the data from that study may have presented an underestimation of positive intraparotid lymph nodes. In the current study, total parotidectomy was performed in all patients, and the IPN metastasis rate was 17.8%. This finding was consistent with rates reported for adult patients.15,16 Moreover, the current study was the first to evaluate how IPN metastasis may affect the prognosis. It was noted that once there is IPN metastasis, the risk for recurrence and death would increase by twofold compared to baseline levels. Similar findings were also reported by Klussmann et al,15 Lim et al,5 and Stenner et al;16 even Klussmann et al15 concluded that total parotidectomy and radical-modified neck dissection were recommended as surgical treatments for parotid cancer. We propose that total parotidectomy should be required in all pediatric MEC patients, owing to the fact that there were also nodes in the parotid deep lobe; if IPN metastases are noted, more monitoring should take place to detect neck recurrence early.
Radiotherapy has been indicated to increase LRC and DSS rates.4,7,9,12 Nevertheless, radiation-induced cancer was also reported,4 as well as such complications as dry mouth, trismus and, in particular, jaw development disorders. Generally, radiotherapy is commonly selected for patients with adverse pathologic characteristics, such as positive margins, high-grade tumors, advanced tumor stage, positive neck disease, etc. Recently, Mao et al10 reported their experience of surgery combined with postoperative 125I seed brachytherapy in pediatric MEC management, during a follow-up period of 5–13.4 years (median, 7.2 years); the overall and disease-free survival rates were both 100%. Nevertheless, the sample size was small, and more studies are needed to clarify this question.
The NLR with respect prognosis in head and neck cancer had been hotly debated. Kano et al17 analyzed the association between pretreatment inflammatory markers and the prognosis of patients with squamous cell carcinoma of the head and neck. The authors found that a high NLR was related to advanced disease stage; with respect to survival outcomes, a high NLR was significantly associated with decreases in disease-free survival and overall survival. Recently, Liu et al18 noted the NLR correlated with tumor size in thyroid cancer. The underlying mechanism might be that neutrophils produce several angiogenic factors and cytokines that participate in various steps of tumor development, and lymphocytes are responsible for immune surveillance, resulting in the elimination of cancer cells.19 However, the significance of the NLR in parotid cancer remains unclear, and the current study was the first to note that the NLR has a limited effect on the prognosis in parotid cancer patients. Nevertheless, only 73 patients were enrolled in the current study, and further large sample size studies are needed to clarify this question.
There are some limitations of this study. First, there is inherent bias in retrospective studies. Second, the sample size was relatively small, possibly reducing the statistical power. A multi-center study is needed to clarify the long-term survival in pediatric patients with parotid MEC. Third, it should be recognized that neutrophil and lymphocyte counts are non-specific parameters, and they can be influenced by concomitant conditions, such as infections or inflammation.20
Conclusion
In summary, the long-term survival rate was relatively favorable in pediatric MEC; the 10-year LRC and DSS rates were 83% and 88%, respectively. IPN metastasis was one of the most important prognostic factors. Finally, understanding the effect of the NLR on MEC prognosis requires more research.
Abbreviations
DSS, disease-specific survival; IPN, intraparotid node; LRC, loco-regional control; MEC, mucoepidermoid carcinoma; NLR, neutrophil-to-lymphocyte ratio.
Data sharing statement
All data generated or analyzed during this study are included in this published article. The primary data can be obtained from the corresponding author.
Author contributions
Study design and manuscript writing: FL, DS, and QF. Study selection and data analysis: DS, and QF. Study quality evaluation: FL and QF. Manuscript revision: QF. All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Andreasen S, Stevens E, Bjørndal K, Homøe P. Salivary gland epithelial neoplasms in pediatric population: a single-institute experience with a focus on the histologic spectrum and clinical outcome. Hum Pathol. 2018;73:193–194. | ||
Fang QG, Shi S, Li ZN, Zhang X, Liu FY, Sun CF. Epithelial salivary gland tumors in children: a twenty-five-year experience of 122 patients. Int J Pediatr Otorhinolaryngol. 2013;77(8):1252–1254. | ||
Li LJ, Li Y, Wen YM, Liu H, Zhao HW. Clinical analysis of salivary gland tumor cases in West China in past 50 years. Oral Oncol. 2008;44(2):187–192. | ||
Morse E, Fujiwara RJT, Husain Z, Judson B, Mehra S. Pediatric salivary cancer: epidemiology, treatment trends, and association of treatment modality with survival. Otolaryngol Head Neck Surg. 2018;159(3):553–563. | ||
Lim CM, Gilbert MR, Johnson JT, Kim S. Clinical significance of intraparotid lymph node metastasis in primary parotid cancer. Head Neck. 2014;36(11):1634–1637. | ||
Cockerill CC, Gross BC, Contag S, et al. Pediatric malignant salivary gland tumors: 60 year follow up. Int J Pediatr Otorhinolaryngol. 2016;88:1–6. | ||
Chiaravalli S, Guzzo M, Bisogno G, et al. Salivary gland carcinomas in children and adolescents: the Italian TREP project experience. Pediatr Blood Cancer. 2014;61(11):1961–1968. | ||
Janz TA, Camilon PR, Nguyen SA, Levi JR, Lentsch EJ. Has the management of pediatric mucoepidermoid carcinoma of the parotid gland changed? Laryngoscope. 2018;128(10):2408–2414. | ||
Radomski S, Dermody S, Harley EH. Clinical characteristics and outcomes of major salivary gland malignancies in children. Laryngoscope. 2018;128(5):1126–1132. | ||
Mao MH, Zheng L, Wang XM, et al. Surgery combined with postoperative 125I seed brachytherapy for the treatment of mucoepidermoid carcinoma of the parotid gland in pediatric patients. Pediatr Blood Cancer. 2017;64(1):57–63. | ||
Rebours C, Couloigner V, Galmiche L, et al. Pediatric salivary gland carcinomas: diagnostic and therapeutic management. Laryngoscope. 2017;127(1):140–147. | ||
Kupferman ME, de La Garza GO, Santillan AA, et al. Outcomes of pediatric patients with malignancies of the major salivary glands. Ann Surg Oncol. 2010;17(12):3301–3307. | ||
Shi S, Fang Q, Liu F, Zhong M, Sun C. Prognostic factors and survival rates for parotid duct carcinoma patients. J Craniomaxillofac Surg. 2014;42(8):1929–1931. | ||
Stodulski D, Mikaszewski B, Majewska H, Wiśniewski P, Stankiewicz C. Probability and pattern of occult cervical lymph node metastases in primary parotid carcinoma. Eur Arch Otorhinolaryngol. 2017;274(3):1659–1664. | ||
Klussmann JP, Ponert T, Mueller RP, Dienes HP, Guntinas-Lichius O. Patterns of lymph node spread and its influence on outcome in resectable parotid cancer. Eur J Surg Oncol. 2008;34(8):932–937. | ||
Stenner M, Molls C, Luers JC, Beutner D, Klussmann JP, Huettenbrink K-B. Occurrence of lymph node metastasis in early-stage parotid gland cancer. Eur Arch Otorhinolaryngol. 2012;269(2):643–648. | ||
Kano S, Homma A, Hatakeyama H, et al. Pretreatment lymphocyte-to-monocyte ratio as an independent prognostic factor for head and neck cancer. Head Neck. 2017;39(2):247–253. | ||
Liu CL, Lee JJ, Liu TP, Chang YC, Hsu YC, Cheng SP. Blood neutrophil-to-lymphocyte ratio correlates with tumor size in patients with differentiated thyroid cancer. J Surg Oncol. 2013;107(5):493–497. | ||
Trellakis S, Bruderek K, Dumitru CA, et al. Polymorphonuclear granulocytes in human head and neck cancer: enhanced inflammatory activity, modulation by cancer cells and expansion in advanced disease. Int J Cancer. 2011;129(9):2183–2193. | ||
Dell’Aquila E, Cremolini C, Zeppola T, et al. Prognostic and predictive role of neutrophil/lymphocytes ratio in metastatic colorectal cancer: a retrospective analysis of the tribe study by GONO. Ann Oncol. 2018;29(4):924–930. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

