Back to Journals » Clinical Ophthalmology » Volume 14
Ocular Trauma in Pediatric Age Group at a Tertiary Eye Care Center in Central Maharashtra, India
Authors Madan AH, Joshi RS , Wadekar PD
Received 3 January 2020
Accepted for publication 11 March 2020
Published 1 April 2020 Volume 2020:14 Pages 1003—1009
DOI https://doi.org/10.2147/OPTH.S244679
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Ashok Hukumchand Madan, Rajesh Subhash Joshi, Preeti Dasharath Wadekar
Department of Ophthalmology, Government Medical College, Nagpur, Maharashtra 440012, India
Correspondence: Rajesh Subhash Joshi
Government Medical College, 77, Panchtara Housing Society, Manish Nagar, Somalwada, Wardha Road, Nagpur 440012, India
Tel +91 9890131588
Email [email protected]
Purpose: To study the demographic profile and visual outcome in pediatric ocular trauma.
Study Design: Prospective and interventional study.
Setting: Tertiary eye care center in central Maharashtra.
Materials and Methods: The study included all children of age group 15 years and younger sustaining eye injuries and presented to the outpatient department or emergency services. The duration of the study was 1 year. A detailed medical history was obtained. Demographic profile was noted. A detailed ocular examination included visual acuity, slit-lamp biomicroscopy, and fundus examination. All patients were followed up to 6 months.
Results: Out of 350 children examined, 66 (18.9%) had ocular trauma. The mean age at presentation was 8.33 ± 4.03 years. Children aged 6– 10 years (39.3%) were most commonly affected followed by children from 11 to 15 years (36.1%). There were no significant differences between rural (54.1%) and urban (45.9%) children. Most (63.9%) had open and 24.6% had closed globe injuries. Perforating injuries to the cornea (n=29, 47.5%) was the most common injury. Sports-related injuries were common (n= 18) followed by wooden stick- (n = 14) and firecracker-related (n = 11) injuries. In the open and closed globe injuries, 36 (92.3%) and 5 (33.3%) patients, respectively, required immediate surgical intervention.
Conclusion: Sports-related activities were a common cause of ocular trauma in the pediatric age group in the central region of Maharashtra. We propose setting of rapid action ocular trauma team to prevent blindness occurring due to trauma.
Keywords: pediatric ocular trauma, ocular trauma study, ocular trauma, posterior segment trauma
Introduction
Ocular injury is one of the common causes of acquired blindness in children. The consequences of childhood injury are harmful as it leads to permanent blindness and visual handicap. It adds to the economic burden on the society. It also affects the psychological, social, and emotional development of a child. At the same time, parents are also worried about the future of the child.
Ocular trauma in children accounts for 8% to 14% of the total injuries.1 Childhood eye injury is different from adult ocular trauma in terms of the objects involved in causing injury, evaluation, and management protocols.2 Childhood eye trauma includes a range of corneal surface abrasions to corneal and scleral perforations. The majority of ocular injuries in children are preventable by taking minor precautions and identification of risk factors for ocular injury.3–6
Ocular injuries have been broadly classified into two types: (1) open and closed globe and (2) adnexal injuries. Open globe injury is an emergency and requires immediate attention.7
The epidemiological profile of pediatric ocular injuries varies from country to country and state wise in the same country. There have been studies on pediatric ocular injuries in the developed countries8–10 and developing countries.2,11–15 Eye trauma is more common in developing countries than in developed countries.16,17 The nature of the injury and visual outcome is different between developing and developed countries due to vast differences in social, demographic, and cultural factors. There has been a study on the epidemiological profile of ocular trauma in the pediatric age group. However, there is a sparse literature in the visual outcome in posterior segment trauma in the pediatric age group.
Therefore, the present study was carried out to identify various etiological factors involved in the causation of pediatric ocular injuries, implementation of preventive measures in the population, and the visual outcomes in pediatric ocular trauma.
Materials and Methods
The present study was a prospective, observational, and interventional case study carried out in the tertiary eye care center. The duration of the study lasted from September 2018 to August 2019. The medical ethics committee of the Government medical college and hospital, Nagpur, Maharashtra, India approved the study. The study adhered to the tenets of the Declaration of Helsinki. The data were collected after written informed consent from parents. The study included all children of age group ≤15 years who sustained eye injuries and presented to the outpatient department or emergency services. A detailed history as to the cause of the injury was obtained. Any systemic injury was noted. Demographic profiles of all patients in terms of age, sex, residential area (urban or rural), date and time of injury, and any treatment were noted. A detailed ocular examination included visual acuity, slit-lamp biomicroscopy, and fundus examination. In infants and preschool children visual acuity was evaluated using Teller Acuity Cards. In the rest of the children, visual acuity was assessed using a Snellen chart. Intraocular tension was measured in all patients, except in those having open globe injuries. Gonioscopy was performed in closed globe injury. Ultrasounds of the eye and adnexa were obtained. Radiography of the eye was advised in patients with a suspected retained intraocular foreign body. Children who did not co-operate with the examination were examined under general anesthesia before any intervention.
All patients were appropriately managed and followed up on days 1 and 7 and in the first and sixth months. Patients requiring surgical intervention were operated upon with the repair of perforation, removal of foreign body, vitrectomy. These patients were followed up on day one postoperative period and subsequently till 6 months. Surgical techniques not mentioned as it was beyond the scope of the study. At every visit, the best-corrected visual acuity, slit-lamp examination, intraocular pressure, and fundus examination were performed. Patients with minimum follow-ups of 6 months were included in the study group.
Ocular Trauma Score and Classification of Injury
Ocular trauma score was carried out according to the scoring system developed by Khun et al.17 The ocular injuries were classified using the standardized international classification of ocular trauma, the Birmingham Eye Trauma Terminology System (BETTS).18 BETTS is to depict the ocular injury terminology (open or closed globe).19 Classification of ocular trauma according to the location of the wound was defined by the Ocular Trauma Classification Group.20
Statistical Analysis
The data were entered in an Excel® sheet (Software version 14.1.0 [110310]/2011) (Microsoft Corporation, Redmond, WA, USA), and statistical analysis was performed with SPSS version 13.0 (SPSS Inc, Chicago, IL, USA). Snellen’s visual acuity was converted to LogMAR unit for the statistical analysis. Mean and standard deviation were used to describe the continuous variables, while frequencies and percentages were used to describe the categorical and binary variables. Parametric and non-parametric comparisons were performed for all variables.
Results
Demographic Characteristics
Out of 350 children examined, 66 (18.9%) presented ocular trauma. Five patients (8.2%) were lost to follow-up. Therefore, the statistics represent 61 children. Mean age at presentation was 8.33 ± 4.03 years. Children aged 6–10 years (39.3%) were most commonly affected followed by the age group consisting of 11- to 15-year-old children/adolescents (36.1%). There were 38 (62.3%) boys and 23 (37.7%) girls. There were no significant differences between rural and urban children (54.1% and 45.9%, respectively). Table 1 shows the sociodemographic characteristics of the studied ocular trauma children.
 |
Table 1 Socio-Demographic Characteristics |
Ocular Injury Details
Forty-seven children (77.1%) had uniocular and 14 children (22.9%) had binocular injuries. The nature of injuries were classified into open (63.9%) and closed globe (24.6%). Other injuries (8.2%) included adnexal and chemical injuries. Ocular injury details are shown in Table 2–4. A perforating open globe injury to the cornea (n = 29, 47.5%) was the most common injury. In a closed globe injury, corneal abrasion (n = 7, 11.5%) was the most common injury followed by hyphema (n = 04, 6.6%). Other types of closed globe injuries were lid and canalicular injuries (n = 03, 4.9%), chemical and orbital fractures (n = 01, 1.6%).
 |
Table 2 Open Globe Injury Profile |
 |
Table 3 Closed Globe Injury Profile |
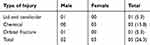 |
Table 4 Ocular Injuries (Not Included in the Birmingham Trauma Technology System [BETTS] Classification) but Included in a Closed Globe Injury |
Zone of injury: Distribution of injury according to the zone of involvement of globe is represented in Table 5. Zone I injury was common in closed (n = 33) and open (n = 15) globe injury (n = 15).
 |
Table 5 Zone of Injury in Both the Groups |
Ocular Trauma Score (OTS)
Thirty-one eyes in open globe and 15 eyes in closed globe injury fall into OTS category 2. Details of OTS are illustrated in Table 6.
 |
Table 6 Ocular Trauma Score in Both Types of Injury |
Only seven cases (11.5%) presented within 6 h after injury, 20 cases (32.8%) presented between 6 and 24 h after injury, while 34 cases (55.7%) presented 24 h after injury.
Causes of Trauma
Sports-related injury was common (n= 18) followed by those caused by wooden stick (n= 14) and firecrackers (n=11). Details of injury are shown in Table 7. During the analysis of ocular injury, most of the injuries were seen during the period of vacation of children (Summer April–June, n=14 and winter November–December, n=13).
 |
Table 7 Causes of Ocular Injury |
Treatment and Visual Outcome
In the open globe injury, 36 eyes (36/39, 92.3%) required immediate surgical intervention in the form of surgical repair of the perforation site. Three eyes had sealed corneal perforation, which were managed by medical treatment. One patient having sealed corneal perforation developed a cataract 2 months later and underwent cataract-removal surgery with implantation of intraocular lens. In the closed globe injury, five patients (33.3%) required immediate intervention. These included two patients with the removal of a corneal foreign body. One patient needed paracentesis and removal of blood from the anterior chamber, one patient required vitrectomy for endophthalmitis, and one patient required removal of dislocated lens from the anterior chamber.
In the open globe injury, 6 patients had no perception of light (NPL), while 33 patients had visual acuity from the perception of light to LogMAR 1.00 (6/60). Eight patients improved to LogMAR 0.30–0.00 while 20 improved to LogMAR 1-PL. Five patients had poor visual outcome and three patients presented with globe rupture, and presenting visual acuity was NPL. One patient each developed secondary glaucoma and panophthalmitis.
In the closed globe injury, eight children presented visual acuity LogMAR 1- PL+, and six had visual acuity LogMAR 0.30–1.00. Visual outcome in 10 children was LogMAR 0.30–-0.00. One child did not improve as his eye went into secondary glaucoma. This patient had firecracker injury. Visual outcome in types of injury is depicted in Table 8.
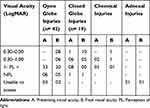 |
Table 8 Visual Outcomes in Closed and Open Globe Injury |
Discussion
The present study is the first kind of its study from the central region of Maharashtra highlighting the magnitude of the ocular injury problem in the pediatric age group. Pediatric ocular trauma forms about 20–50% of all ocular injuries reported.6,7
The incidence of pediatric ocular trauma in our study was found to be 18.9% (350/66) in a one-year period. Three hundred and fifty children presented in the outpatient department during the study period with various ocular problems. Sixty-six children had ocular injury. Singh et al noted the incidence of pediatric ocular trauma in the central Indian population as 12.8%.11 Saxena recorded the incidence in a tertiary eye care center in the duration of 6 months as 20.8%.3 Maurya (in an epidemiological study from the northern part of India) showed about 30.35% of ocular trauma occurred in the pediatric age group.21 Wadeai et al noted an increase in the childhood trauma to the extent of 49.7% in the Egyptian population.22 In the Nigerian population, the proportion of eye injuries in children was 26.4%.15 A study from an Arabian country demonstrated a high incidence of pediatric trauma to the tune of 58.5%.13 China found the incidence of pediatric ocular injury in the Chaoshan region to be 23.6%.23 Five percent of all admissions in developed countries24 and 12.9% from developing countries result from eye injuries.12 The variability in the documentation of ocular trauma incidence in pediatric population could be due to vast differences in cultural and social factors and study design. It also depends on the referral services and the facilities available for the treatment in the hospital.
Our hospital received patients from all parts of the city in addition to rural areas. Therefore, there were no differences in the referral of the cases from the rural and urban areas (54.1% and 45.9%, respectively). Chakraborti et al, in their study from eastern India, noted the majority of children were from urban populations (70%).25 However, Singh has shown a high preponderance of childhood trauma in the rural population. In their study, they demonstrated that rural area children are at 1.5 times higher risk of ocular injuries than urban children.11 Similar findings were reported by Katiyar et al in rural children, accounting for 78% of ocular trauma.26 The differences in the rural and urban population could be due to improvement in the eye care facilities in the rural areas restricting the referral to the urban centers.
We found that children aged 6–10 years (39.3%) were most commonly affected followed by those in the age range of 11 to 15 years (36.1%). This finding correlates with other studies from Indian population,3,11,25,26 and those from all over the world also show the same trend.13,22,23,27 In this age group, a child starts going to school and is often involved in many sports activities.
Studies have quoted percentage of males affected are more than the females.3,11,13,22,23,25–27 Our study also showed preponderance to males 38 (62.3%) over females 23 (37.7%). A possible reason for this finding could be that boys are more involved than females in outdoor activities. Another possible explanation given by Singh et al is the importance given to males over females in Indian society with respect to illness, a finding with which we also agree.11
In the current study, the most common cause of ocular injury was sports-related injury (spinning top, cricket ball) in a closed globe and wooden stick in the open globe. This observation correlates with Qayum et al, who also found that sports-related injuries are common with respect to closed globe injuries, and wooden stick injuries were found in open globe.28 Most of the studies demonstrate the wooden stick as a common cause of injury.11,21,26,29 Availability of wooden material in the vicinity of the house could be the reason for this finding. Nowadays, children are attracted to sports activities. They do not understand the importance of supervision by the experts. Therefore, sports-related injuries were common in our studies. Saxena et al reported bow and arrow injury (15.2%) was common in their study.3 Singh revealed only 2.1% of cases were related to bow and arrow injury.11 In our study, we did not come across any case of such an injury, suggesting a declining trend toward the use of the bow and arrow. This trend could be due to awareness about ocular injuries associated with this type of sports. Eighteen percent of the children in our study had firecracker-related injuries. Saxena et al also reported firecracker injury as a common mode of ocular injury.3 In spite of a fireworks regulation act; the trend towards ocular injury caused by fireworks is increasing. This trend could be due to firecrackers are exploded during festival seasons but also during marriages. Most of the time, parents do not supervise children’s activities, which lead to an increase in incidences of firecracker-related ocular injuries. Strict legislation and public education are needed to stop firecrackers-related injuries.
Uncommon causes of eye injury in the present study were injury caused by a bird beak, hen’s leg, dog bite, and cooker blast.
We have observed the injury trend during vacation. As many as 27 (27/61, 44.3%) children had eye trauma while on vacation. However, no seasonal predilection to injury was noted. Maurya et al observed 43.5% injuries in the summer, 31.6% in the rainy season, and 24.9% in the winter.21 The importance of performing an analysis of ocular injury during vacation periods is to strictly supervise children’s sports activities and to educate them to avoid eye injuries.
In the present study, open globe injuries (63.9%) to the eye dominated compared to the closed globe ones (24.6%). Similar trends have been observed in many studies.3,11,22,23,26 However, few studies have observed closed globe injury common than open globe injury.13,21,27,30,31 The reason for more patients with open globe injuries could be due to patients with severely injured eyes that affected their vision came to the hospital, while those with closed globe injury did not.
Open globe injuries present more potential for poor vision than the closed globe injuries.3,11,21–28 In our study, six patients presented with NPL, and five remained NPL after surgical repair of the perforation site. Poor prognosis in these patients could be due to repeated surgical interventions, development of secondary glaucoma, and/or endophthalmitis. Those children who presented with visual acuity between PL + – 6/60 (n=33) did not improve beyond 6/60. Agrawal et al demonstrated poor visual outcome in patients with posterior segment trauma.2 Singh et al reported that visual acuity presentation may suggest the extent of damage to the ocular structures.11 Delayed presentation of the patients to the hospital delays intervention thus leading to poor prognosis.11,13,22,25 In our series, 34 cases (55.7%) presented 24 h after an injury had occurred. In a study by Saxena et al, 34% of children presented 24 h after injury.3 Wadeai et al, in a pediatric Egyptian ocular trauma study, showed that 50% of children presented 24 h after injury.22 However, they did not find any clinically significant differences in the visual outcomes between patients presenting after 24 h compared to those that presented earlier than 24 h.22 Significant delays in the presentation of patients in our study could be due to lack of awareness about the severity of ocular injury in the population, late recognition of the problem, inability to bring child to the hospital due to loss of daily wages, or residing in remote areas. About half of the patients (54.1%) in our study were residing in rural areas.
In the closed globe injury group, one patient had NPL, and this patient did not improve. This patient had undergone a firecracker injury and developed secondary glaucoma. Visual outcome was better in closed group as 10 patients improved from 6/12 to 6/6 and five from 6/12 to 6/60. One patient with chemical injury had a poor vision (PL+) because he developed corneal scarring along with uncontrolled intraocular pressure. Therefore, it is important to check IOP during follow-up visits and conduct the necessary glaucoma-related investigations.
The ocular trauma score (OTS) serves to predict visual prognosis after an ocular injury has occurred. A high score suggests good visual outcome, whereas a low score suggests poor visual outcome. The maximum number of patients (n=30) had an OTS of category-2 (45–65) in the open lobe injury, suggesting poor prognosis. This finding was reflected in the visual outcome in open globe injury. This result is in agreement with Singh et al, who demonstrated that 96.2% of patients with OTS 5 could achieve good vision compared to 6.2% patients with OTS-1.11
Zone-I injuries were common in both the groups, suggesting anterior structures of the eye are vulnerable to trauma.
In order to prevent blindness due to ocular injuries and treat pediatric ocular trauma, we propose the establishment of a rapid action ocular trauma team involving a casualty medical officer, resident ophthalmic surgeon, vitreoretinal specialist, anesthetist, and medical social worker within every ophthalmic department. This setup will ensure the management of pediatric ocular injuries in addition to the education of society to prevent ocular trauma.
Conclusion
Our study concludes that ocular injuries are a major cause of pediatric blindness in the central region of Maharashtra. The age group from 6 to 10 years is susceptible for trauma. Timely referral and management can help to prevent blindness originating from ocular trauma. Follow-ups of children are important for treating complications in the long term. It is very essential to educate children, parents, and teachers regarding ocular health and hygiene in order to minimize eye injuries. Formation of a rapid action ocular trauma team may help to treat pediatric ocular trauma and create awareness and educate child, family, and society regarding ocular trauma.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Brophy M, Sinclair SA, Hostetler SG, Xiang H. Pediatric eye injury-related hospitalizations in the United States. Pediatrics. 2006;117(6):e1263–e1271. doi:10.1542/peds.2005-1950
2. Agrawal R, Rao G, Naigaonkar R, et al. Prognostic factors for vision outcome after surgical repair of open globe injuries. Indian J Ophthalmol. 2011;59(6):465–470. doi:10.4103/0301-4738.86314
3. Saxena R, Sinha R, Purohit A, et al. Pattern of pediatric ocular trauma in India. Indian J Pediatr. 2002;69(10):863–867. doi:10.1007/BF02723708
4. Shah A, Blackhall K, Ker K, et al. Educational interventions for the prevention of eye injuries. Cochrane Database Syst Rev. 2009; 4. doi:10.1002/14651858.CD006527.pub3
5. Philip SS, Hoskin AK. Children’s protective eyewear: the challenges and the way forward. Med J Aust. 2014;201(2):87–88. doi:10.5694/mja2.2014.201.issue-2
6. Hoskin AK, Philip SS, Yardley AM, et al. Eye injury prevention for the pediatric population. Asia-Pac J Ophthalmol. 2016;5(3):202–211. doi:10.1097/APO.0000000000000193
7. Desai T, Vyas C, Desai S, et al. Pattern of ocular injuries in paediatric population in western India. NHL J Med Sci. 2013;2:37–40.
8. Mela EK, Mantzouranis GA, Giakoumis AP, et al. Ocular trauma in a Greek population: review of 899 cases resulting in hospitalization. Ophthalmic Epidemiol. 2005;12(3):185–190. doi:10.1080/09286580590964801
9. Tomazzoli L, Renzi G, Mansoldo C. Eye injuries in childhood: a retrospective investigation of 88 cases from 1988 to 2000. Eur J Ophthalmol. 2003;13(8):710–713. doi:10.1177/112067210301300808
10. Loon SC, Tay WT, Saw SM, et al. Prevalence and risk factors of ocular trauma in an urban south‐east Asian population: the Singapore Malay Eye Study. Clin Exp Ophthalmol. 2009;37:362–367. doi:10.1111/j.1442-9071.2009.02035.x
11. Singh S, Sharma B, Kumar K, et al. Epidemiology, clinical profile and factors, predicting final visual outcome of pediatric ocular trauma in a tertiary eye care center of Central India. Int J Ophthalmol. 2017;65:1192.
12. Khan MD, Kundi N, Mohammad Z, et al. Eye injuries in the North West Frontier Province of Pakistan. Pak J Ophthalmol. 1988;4:5–9.
13. Al-Mahdi HS, Bener A, Hashim SP. Clinical pattern of pediatric ocular trauma in fast developing country. Int Emer Nursing. 2011;19(4):186–191. doi:10.1016/j.ienj.2011.06.008
14. Demissie BS, Demissie ES. Patterns of eye diseases in children visiting a tertiary teaching hospital: south-western Ethiopia. Ethiop J Health Sci. 2014;24(1):69–74. doi:10.4314/ejhs.v24i1.9
15. Okoye O, Ubesie A, Ogbonnaya C. Pediatric ocular injuries in a resource-deficient rural mission eye hospital in Southeastern Nigeria. J Health Care Poor Underserved. 2014;25(1):63–71. doi:10.1353/hpu.2014.0031
16. Miratashi MS. Pediatric ocular trauma. Acta Med Iran. 2006;125–130.
17. Salvin JH. Systematic approach to pediatric ocular trauma. Curr Opin Ophthalmol. 2007;18(5):366–372. doi:10.1097/ICU.0b013e3282ba54ac
18. Kuhn F, Maisiak R, Mann L, et al. The Ocular Trauma Score (OTS). Ophthalmol Clin North Am. 2002;15(2):163–165. doi:10.1016/S0896-1549(02)00007-X
19. Pieramici DJ, Sternberg P
20. Kuhn F, Morris R, Witherspoon CD, et al. The Birmingham Eye Trauma Terminology system (BETT). J Fr Ophthalmol. 2004;27(2):206–210. doi:10.1016/S0181-5512(04)96122-0
21. Maurya RP, Srivastav T, Singh VP, et al. The epidemiology of ocular trauma in Northern India: a teaching hospital study. Oman J Ophthalmol. 2019;12(2):78. doi:10.4103/ojo.OJO_149_2018
22. Al Wadeai EA, Osman AA, Macky TA, et al. Epidemiological features of pediatric ocular trauma in Egypt. J Ophthalmol. 2016;2016.
23. Cao H, Li L, Zhang M. Epidemiology of patients hospitalized for ocular trauma in the Chaoshan region of China, 2001–2010. PLoS One. 2012;7(10):e48377. doi:10.1371/journal.pone.0048377
24. Thylefors B. Epidemiological patterns of ocular trauma. Aust N Z J Ophthalmol. 1992;20(2):95. doi:10.1111/ceo.1992.20.issue-2
25. Chakraborti C, Giri D, Choudhury KP, et al. Paediatric ocular trauma in a tertiary eye care center in Eastern India. Ind J Public Health. 2014;58(4):278. doi:10.4103/0019-557X.146297
26. Katiyar V, Bangwal S, Gupta SK, et al. Ocular trauma in Indian paediatric population. J Clin Ophthalmol Res. 2016;4(1):
27. Sharifzadeh M, Rahmanikhah E, Nakhaee N. Pattern of pediatric eye injuries in Tehran, Iran. Int Ophthalmol. 2013;33(3):255–259. doi:10.1007/s10792-012-9684-4
28. Qayum S, Anjum R, Garg P. Epidemiological pattern of ocular trauma in a tertiary hospital of northern India. Int J Biomed Res. 2016;7:
29. Onakpoya OH, Adeoye AO. Childhood eye diseases in southwestern Nigeria: a tertiary hospital study. Clinics. 2009;64(10):947–951. doi:10.1590/S1807-59322009001000003
30. Armstrong GW, Kim JG, Linakis JG, et al. Pediatric eye injuries presenting to United States emergency departments: 2001–2007. Graefe’s Arch Clin Exp Ophthalmol. 2013;251(3):629–636. doi:10.1007/s00417-011-1917-0
31. Dulal S, Ale JB, Sapkota YD. Profile of pediatric ocular trauma in mid western hilly region of Nepal. Nep J Ophthalmol. 2012;4(1):134–137. doi:10.3126/nepjoph.v4i1.5865
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
