Back to Journals » Clinical Ophthalmology » Volume 11
Ocular melanoma-when you have seen one, you have not seen them all: a clinical outcome study from the Surveillance, Epidemiology and End Results (SEER) database (1973–2012)
Authors Mahendraraj K, Shrestha S, Lau CSM, Chamberlain RS
Received 24 August 2016
Accepted for publication 20 October 2016
Published 5 January 2017 Volume 2017:11 Pages 153—160
DOI https://doi.org/10.2147/OPTH.S120530
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Krishnaraj Mahendraraj,1 Sneha Shrestha,1 Christine SM Lau,1,2 Ronald S Chamberlain1–4
1Department of Surgery, Saint Barnabas Medical Center, Livingston, NJ, USA; 2Saint George’s University School of Medicine, Grenada, West Indies; 3Department of Surgery, Banner MD Anderson Cancer Center, Gilbert, AZ, USA; 4Department of Surgery, Rutgers University, New Jersey Medical School, Newark, NJ, USA
Background: Ocular melanoma (OM) comprises <5% of all melanomas. Uveal melanoma (UM) is the most common subtype of OM, while conjunctival melanoma (CM) is rare and differs significantly from UM. The purpose of this study is to evaluate a large cohort of OM patients to differentiate demographic, pathologic, and clinical factors between these two neoplasms, which may affect treatment and outcomes.
Methods: The Surveillance, Epidemiology, and End Results database (1973–2012) was used to extract demographic and clinical data on 8,165 OM patients (92.1% UM and 7.9% CM).
Results: Both CM and UM were most prevalent among Caucasian males in the seventh decade of life. UM patients presented more often with localized disease (90.9% vs 81.2, P<0.01). Surgery (42.8%), radiation (43.0%), or combined surgery and radiation (7.0%) were used in the treatment of UM, while CM was treated almost exclusively with surgery (88.7%). Mean overall survival was longer (15.4 vs 14.6 years; P<0.01) and mortality rates were lower in patients (38.8% vs 46.1%; P<0.01) with CM.
Conclusion: Despite presenting with more advanced disease than UM, CM is associated with an increased overall survival. Surgery is the primary therapy for CM, whereas radiotherapy is the primary therapy for UM and is associated with prolonged survival.
Keywords: ocular melanoma, uveal melanoma, conjunctival melanoma, SEER
Introduction
Ocular melanoma (OM), the second most common type of melanoma after cutaneous melanoma, accounts for 3.7% of all melanoma cases.1,2 The incidence rate of OM is one per million in the United States (US), and 0.7 per 100,000 among Caucasians alone (age-standardized to the World Standard Population).2,3 There are two major subtypes of OM: those that arise from the iris, choroid, and ciliary body (uveal melanoma, UM) and those from the conjunctiva (conjunctival melanoma, CM).
UM is the most common primary intraocular malignancy among adults, and accounts for up to 85% of all cases of OM.4,5 The incidence of UM in the US is 4.9 per million and has remained stable over the last three decades.6 Although UM patients typically present with symptoms including blurred vision, visual field defect, metamorphopsia, or photopsia, 30% patients may be asymptomatic and upon routine eye examination, they are detected incidentally.7,8 Diagnosis is accurately established by clinical examination in over 99% cases.9 Modern diagnostic tools such as A and B ultrasonography, fluorescein angiography, and optical coherence tomography can significantly aid in diagnosis, making it possible to avoid biopsy in nearly all cases.10,11 Historically, UM has been treated with enucleation, radiation alone, or combination surgery and radiation; however since the late 1980s, a change in prevailing trends toward radiation has emerged.12 More recently, with growing understanding of the genetic and molecular basis of UM, therapeutic trials utilizing adjuvant therapies such as crizotinib, sunitinib, valproic acid, interferon alpha, and dacarbazine have begun to emerge.11 Regardless of the initial management method chosen, at least 30% of affected patients will develop metastatic spread to the liver, lung, bone, or skin within 10 years of successful local control of the primary neoplasm, with the liver being involved in up to 95% of cases.13,14
CM accounts for only 5% of all OM patients.15 The CM incidence in the US is 0.4 per million and has been increasing progressively.10 Among Caucasian men alone, the incidence rate increased by 295% over the last 27 years.10 CM occurs most commonly in the bulbar conjunctiva, and rarely in the palpebral and forniceal conjunctiva, plica semilunaris, or caruncula.10,13 CM typically presents in patients over 60 years of age with raised pigmented lesions on the conjunctiva, often surrounded by prominent feeder blood vessels, and these lesions may even be amelanotic.10,13 CMs are generally asymptomatic, causing only occasional pain and irritation.10 Primary treatment of CM is surgical with wide local excision.1 Additional therapies include adjuvant brachytherapy, cryotherapy, and topical chemotherapeutic agents such as mitomycin C.10 Metastasis in CM typically involves the salivary lymph nodes, lungs, liver, skin, and brain, with the brain being the most common site of distant metastasis (involved in up to 25% of cases).10
At present, data detailing survival trends among OM patients are based primarily on rare population-based studies involving small groups of patients from high volume melanoma centers.10,16 Demographic and clinical factors influencing clinical outcomes in OM patients, particularly CM, are not well understood. The current study examines a large cohort of OM patients (both UM and CM) to evaluate demographic, pathologic, and clinical factors that affect patient outcomes and alter therapeutic approaches.
Methods
Data for the current study were extracted from the National Cancer Institute’s Surveillance, Epidemiology, and End Result (SEER) database between 1973 and 2012. Data from 17 SEER registries (Alaska Native Tumor Registry, Arizona Indians, Cherokee Nation, Connecticut, Detroit, Georgia Center for Cancer Statistics, Greater Bay Area Cancer Registry, Greater California, Hawaii, Iowa, Kentucky, Los Angeles, Louisiana, New Jersey, New Mexico, Seattle-Puget Sound, and Utah) were extracted into SEER Stat software version 8.0.4. There were 277,120 cases of histologically confirmed melanoma. A total of 8,165 cases with a primary diagnosis of OM were identified using the SEER International Classification of Disease for Oncology (ICD-O-3) codes, code C69.0 (CM) for the CM group, and C69.3 (choroid) and C69.4 (ciliary body and iris) for the UM group. The demographic and clinical data that were extracted were age, sex, ethnicity, geographic location, prior malignancy status, tumor stage, laterality, and type of treatment received (surgery, radiation, both surgery and radiation, or no treatment/unknown). Patients with in situ cancers were excluded from the study. The endpoints and outcomes that were examined included overall survival, mortality, and 1-, 2-, and 5-year cancer-specific survival. Chi-square test was used to compare categorical data, while Student’s t-test and analysis of variance were used to compare continuous data. To determine independent factors that affect survival and mortality, a multivariate analysis using the “backward wald” method was conducted, and odds ratios (OR) were calculated. Long-term actuarial survival between conjunctival and UM was performed using Kaplan–Meier curves. Unknown and missing data were not included in the multivariate analysis. A P-value of <0.05 was utilized to determine statistical significance. All data analyses were performed with IBM SPSS®v20.2. Ethics board approval to conduct the study was obtained from Saint Barnabas Medical Center who deemed patient consent was not required as the current study is a retrospective study utilizing data from the SEER database and no specific patient identifiable information was utilized.
Results
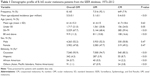
The study cohort consisted of 8,165 OM cases, which represented 2.9% of all melanomas in the SEER database (1973–2012). UM accounted for 92.1% (N=7,516) and CM accounted for 7.9% (N=649) of all OM cases (Table 1), P<0.01.
Demographic characteristics
Mean age-adjusted incidence of OM was 5.5 per million, while mean age-adjusted CM incidence was 0.4 per million, P<0.001. The mean age of all OM patients was 61.4±15.3 years (Table 1). CM and UM patients had a similar mean age (61.7±18.6 years vs 61.4±15.0 years, P=0.63). Among all OM patients, 21.0% (N=1,717) were <50 years of age, 67.7% (N=5,529) were between 50–79 years of age, and 11.3% (N=919) were ≥80 years of age. Although most CM and UM patients were between 50–79 years old (59.4% vs 68.4%, P<0.01), more CM patients were under the age of 50 years (24.0% vs 20.8%, P=0.05) and ≥80 years (16.6% vs 10.8%, P<0.01) compared to UM patients. The male-to-female ratio for OM was 1.09:1 with 52.2% male (N=4,263) and 47.8% female (N=3,902), P<0.01. Male-to-female ratio was similar for both CM and UM (1.03:1.0 vs 1.1:1.0, P=0.47). OM, UM, and CM were all more common among Caucasians (93.9% in OM, 94.7% in UM, and 85.3% in CM, P<0.01). The highest incidence of OM was among Caucasians (93.9%; N=7,540), followed by Hispanics (4.3%; N=342), African-Americans (0.7%; N=54), and other ethnicities including Asian, Pacific Islanders, and Native Americans (1.1%; N=91), P<0.01. CM had a significantly lower incidence among Caucasians (85.3% vs 94.7%, P<0.01) and higher incidence in non-Caucasian groups compared to UM, including African Americans (2.2% vs 0.5%, P<0.01), Hispanics (8.7% vs 3.9%, P<0.01), and Asian/Pacific Islanders/Native Americans (3.8% vs 0.9%, P<0.01).
Tumor characteristics
Among OM patients, 50.1% (N=4,049) had right eye involvement, 49.8% (N=4,025) had left eye involvement, and 0.1% (N=3) had bilateral involvement (Table 2). CM had significantly less right eye involvement (45.5% vs 50.5%, P<0.01) and more left involvement (54.3% vs 49.4%, P<0.01), but comparable bilateral involvement (0.15% vs 0.03%, P=0.08) compared to UM.
In all, 90.1% (N=6,602) of all OM patients presented with localized disease, 8.2% (N=601) with regional disease, and 1.7% (N=124) exhibited distant metastasis. Significantly fewer CM patients had localized disease compared to UM patients (81.2% vs 90.9%, P<0.01). Conversely, CM patients had more regional (16.2% vs 7.5%, P<0.01) and distant diseases (2.6% vs 1.6%, P=0.09).
Treatment
In all, 47.1% (N=3,769) of OM patients were treated surgically, while 39.9% of patients (N=3,192) were treated with primary radiotherapy (Table 3). In all, 6.7% of patients (N=538) received both surgery and radiotherapy, while 6.3% of patients (N=504) had no treatment. Surgery was the primary treatment in CM (88.7%, N=565) and was used significantly more often than for UM (42.8%, N=3,218), P<0.01. UM patients underwent radiation therapy (43.0%, N=3,232) and radiation combined with surgery (7.0%, N=527) more frequently than CM patients in whom 0.9% (N=6) underwent radiation therapy and 2.4% (N=15) underwent combination therapy, P<0.01. More CM patients did not receive treatment (8.0% vs 7.2%), P=0.44.
Outcomes
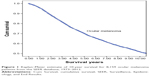
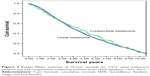
Mean overall survival for all OM patients was 14.6±0.2 years (Table 3), P<0.01. Overall survival for CM patients was higher than for UM patients (15.4±0.9 years vs 14.6±0.2 years), P<0.01 (Figures 1 and 2). Overall and cancer-specific mortality was 45.5% and 21.5%, respectively, for OM. Overall mortality was 46.1% among UM patients and 38.8% among CM patients, while overall cancer-specific mortality was 24.9% among UM patients and 20.0% among CM, P<0.01.
Mean cancer-specific relative survival at 1, 2, and 5 years for all OM patients was 96%, 89%, and 71%, respectively. Similar mean cancer-specific survival at 1, 2, and 5 years was observed in UM (96%, 89%, and 70%) and CM (95%, 88%, and 73%), P>0.05.
Multivariate analysis
Multivariate analysis identified male sex (OR 1.1, CI =1.0–1.3), age over 50 years (OR 4.0, CI =3.4–4.6), and distant metastases (OR 8.6, CI =4.7–15) as independently associated with increased overall and cancer-specific mortality for OM patients, P<0.005. Surgical treatment alone was independently associated with increased mortality in UM (OR 2.6, CI =2.0–3.3, P<0.005), while primary radiation treatment was independently associated with reduced mortality (OR 0.5, CI =0.4–0.7), P<0.005. No variables were associated with a statistically significant higher risk of mortality for CM.
Discussion
The incidence of OM is considerably lower than cutaneous melanoma; however, UM is the most common primary intraocular malignancy in adults, with a mean age-adjusted incidence of 5.1 per million in the US population.1,4 UM accounts for 85%–90% of all OMs in the published literature, while CM accounts for only 5%–10% of cases.10,17 The current study reports a CM incidence of 0.4 per million over the study period from 1973 to 2012, which is relatively low compared to the UM incidence of 5.1 per million. McLaughlin et al and Singh et al reported age-adjusted UM incidence rates of 4.9–5.1 per million in the US, with the incidence remaining relatively unchanged over the last 35 years.2,4 Yu et al and Tuomaala et al reported CM incidence rates of 0.2–0.8 per million; however, unlike UM, the incidence of CM has been rising over the last 40 years in tandem with a rising cutaneous melanoma incidence.16,18,19 Yu et al reported a 295% increase in the incidence of CM among Caucasian males between 1973 and 1999, while Tuomaala et al reported a rising incidence from 0.4 to 0.8 per million between 1967 and 2000 in a Danish population.18,19
The incidence of UM and CM between sexes is approximately 1:1, which is consistent with most prior population-based studies.2,4,7 Singh et al studied 4,070 UM patients and noted that 51.8% of patients were males.4 In contrast, Graell et al noted that 55.8% of their 303 UM patients were females, while Yu et al reported that 41% of their 206 CM patients were females.18,20 A higher incidence in females (55%) was also reported in a study of 194 Dutch CM patients.14 Lack of consensus implies there is no clear sex predominance for either CM or UM, and both the sexes should be considered equally at risk.
OM most commonly affects Caucasians in the seventh decade of life, with CM patients being slightly older than UM patients. These results are similar to large retrospective studies by Graell et al and Damato and Damato who reported a mean age of 60.1 and 62.1 years for UM patients, respectively, and Anastassiou et al and Kimura et al who reported a mean age of 60 and 62.3 years for CM patients, respectively.7,20–22 McLaughlin et al conducted a large population-based retrospective study including 4,885 OM patients and reported that the incidence of OM was 8–10 times higher among Caucasians compared to African Americans.2 Similarly, Singh et al conducted a retrospective SEER study and found that 97.8% of the 4,070 UM patients were Caucasians.4 Caucasians in their seventh decade of life and older should be considered for fundoscopic screening examinations for OM during regular health visits, with further workup warranted for patients presenting with visual symptoms.18
Hispanics constituted the second largest ethnicity affected by OM (4.2%), particularly CM (8.5%) in the current study. Similarly, Hu et al conducted a retrospective SEER study involving 168 CM patients and reported that 8.33% were Hispanics, also comprising the second largest affected group.23 In terms of UM, Margo reported that Hispanics were the most common ethnic group affected after Caucasians, constituting 5.4% of the 873 UM patients in his study.24 Although Caucasians are at the greatest risk, Hispanic patients should also be considered a high-risk group, and periodic as well as symptomatic screening for OM should be considered.
UM is diagnosed far more often than CM and at earlier, localized stages, while CM has relatively higher rates of advanced disease stage at presentation. McLaughlin et al reported that 67.2% of the 4,885 OM (both UM and CM) patients in their study had localized tumors at the time of diagnosis.2 Missotten et al conducted a retrospective study involving 194 Dutch CM patients and reported that 78.9% of patients had localized tumor, 4.64% had regional metastasis, and 16.5% had distant metastasis.14 Regional metastasis of CM to preauricular and submandibular lymph nodes was very common and occurred in one-third of CM patients.15,21,25
UM is routinely treated with primary radiation therapy, while CM is almost exclusively treated surgically. The majority of CM patients in the current study were treated with surgery only (87.1%), while radiation alone was used in 0.9% and combination therapy in 2.3%. CM was previously believed to be one of the most malignant tumors and enucleation was historically the mainstay of therapy.26 Currently, surgical en bloc excisional biopsy of the tumor, infrequently with adjuvant brachytherapy or chemotherapy like mitomycin C or cryotherapy, has become the preferred treatment for CM and preserves the eye.26 CM is far more surgically accessible given its external location, making it easier to resect than its uveal counterpart, resulting in excellent long-term prognosis and oncologic outcomes if resected early enough.26
Enucleation was the mainstay of treatment for UM until the results of the landmark Collaborative Ocular Melanoma Study (COMS) involving 1,310 UM patients was published and concluded that mortality rates following iodine (I)-125 brachytherapy did not differ significantly from enucleation (27% vs 28%, P=0.48).4,9,27 The COMS centers also reported an increased trend toward diagnosing smaller UMs with advances in diagnostic modalities. As a result, there has been a switch toward eye and vision sparing treatment for smaller tumors.27
In addition to the eye sparing and associated aesthetic benefits associated with avoiding enucleation, vision is preserved in up to 43% of patients receiving radiation therapy. Furthermore, patients with UM who receive radiation therapy experience longer survival than patients who undergo surgical treatment.24,28 The COMS study reported longer survival rates for medium sized melanomas when treated with I-125 brachytherapy compared to enucleation, with comparable 5-year all-cause mortality (19% vs 18%) and 5-year tumor-related mortality (11% vs 9%).24 Despite this, radiotherapy as the primary treatment modality for UM has been slow to take effect and, therefore, may be confounded by other factors such as earlier detection of UM with improved diagnostic modalities allowing for earlier detection and treatment.
External beam radiation (EBRT) has been increasingly used in recent years. Techniques such as proton beam radiotherapy and gamma knife radiosurgery have been increasingly investigated, with variable success.29 In a SEER study involving 1,004 UM patients, Abrams et al reported similar 5-year overall survival (83.3% vs 82.5%, P=0.69) and 5-year cause-specific survival (88.3% vs 88.3%, P=0.92) with EBRT and brachytherapy.29 Brachytherapy appeared more beneficial for early stage tumors, whereas EBRT was more favorable in late stage tumors, likely because it is more difficult to deliver prescriptive doses to tumors of advanced stages.29
In the current study, overall survival was longer for CM patients than UM patients (15.4±0.9 years vs 14.6±0.2 years), and overall mortality for CM patients was lower than for UM patients (38.8% vs 46.1%). In prior studies on UM, the 5-year survival rates after enucleation, brachytherapy, and other methods have ranged from 25% to 66%.30–34 Isager et al studied 2,504 Danish OM patients and observed a 5-year mean cancer-specific mortality of 55%.10 The 5-year mean cancer-specific mortality for CM was noted to be 70%, which is comparable to the current study (73%).10 Isager et al also noted that patients with iris melanomas had the highest observed and relative survival, patients with choroid and ciliary body melanoma had the lowest, and patients with CM had intermediate survival.10 These findings suggest that early management of CM is crucial to maximize survival as it has a relatively better prognosis than UM. Given the difficulty in diagnosing UM and the poor prognosis, periodic ophthalmologic screening of high-risk patients is required for earlier detection and treatment of UM. More research and interest from the clinicians must take place in order to provide the best possible care as well as to improve the prognosis for UM and CM.
With the increasing knowledge of molecular and genetic biology on OM, the optimal management for OM is continually evolving.35–38 To spare the need for surgery and radiation, transpupillary thermotherapy was introduced to conservatively treat small UM tumors.39 Alternative therapies including ipilimumab, kinase inhibitors, and histone deacetylase (HDAC) inhibitors are beginning to be investigated. In a recent study with 746 UM patients, Moser et al reported improved survival with the use of ipilimumab (28 months vs 13 months, P=0.07), compared to those receiving only local therapy.40 Similar improvements in survival were seen with bevacizumab (25 months vs 12 months, P=0.09).40 Genetic counseling to identify BAP1 mutations are also currently under investigation.41 A 15-panel genetic assay has also been developed, which helps to risk stratify tumors and can be used to recommend participation in therapeutic trials. Epigenetic drugs, including DNA methyltransferase (DNMT) inhibitors and HDAC inhibitors, have been shown to have anticancer properties and are beginning to be investigated for ocular tumors with hopes of restoring normal control of neoplastic genomes.42,43 Vidaza (5-azacytidine), a DNMT inhibitor, has been shown to reduce ocular metastasis to the lung in murine xenograft models.42,44 Tenovin-6, which inhibits the class 3 HDAC sirtuin 1 and 2, has shown promise in eliminating UM tumor cells and cancer stem cells.45
Despite the results of this study, several limitations should be taken into consideration. Factors such as tumor size, tumor depth, and socioeconomic status were not included in the SEER database. Furthermore, data on diagnostic imaging and long-term follow-up were not reported. Data on whether or not surgery and radiation were utilized were available in the SEER database; however, specific details pertaining to the surgical procedure, such as surgical margins and the drugs and dosages utilized for chemotherapy, were not reported. This ultimately limits the ability to evaluate the impact of adjuvant or neoadjuvant therapy. Lastly, since SEER registries are more likely to sample from urban than from rural areas, there may also be a degree of selection bias. However, despite these limitations, the SEER database contains data obtained from 26% of the US population, and these findings can be generalized to the overall population.
Conclusion
OM is a rare variant of melanoma. Although UM and CM are variants of OM, they have different clinical behaviors. Both UM and CM are most common in the seventh decade of life and most often found in Caucasians and Hispanics. Both UM and CM present most commonly as localized tumors, with CM more likely to have regional and distant metastasis at presentation. UM has higher overall mortality and cancer-specific mortality than CM. Surgery is the primary therapy for CM, while radiotherapy is the primary therapy for UM and results in prolonged survival compared to surgery alone. Males, older age, and distant disease are all associated with an increased risk of mortality in OM, with primary surgical treatment being an additional risk factor in UM. The optimal management of OM continues to evolve. Novel therapies such as transpupillary thermotherapy and targeted therapy were introduced to manage tumors conservatively without the need for invasive surgery. Although a variety of alternative modalities have been used to treat UM with varying degrees of success, it remains uncertain how these therapies will impact future management and clinical outcomes. A deeper understanding of these rare tumors among clinicians is vital to guide therapeutic decision making in terms of the choice and timing of management.
Disclosure
The authors report no conflicts of interest in this work.
References
Jovanovic P, Mihajlovic M, Djordjevic-Jocic J, Vlajkovic S, Cekic S, Stefanovic V. Ocular melanoma: an overview of the current status. Int J Clin Exp Pathol. 2013;6:1230–1244. | ||
McLaughlin CC, Wu XC, Jemal A, Martin HJ, Roche LM, Chen VW. Incidence of noncutaneous melanomas in the U.S. Cancer. 2005;103:1000–1007. | ||
Isager P, Osterlind A, Engholm G, et al. Uveal and conjunctival malignant melanoma in Denmark, 1943–1997: incidence and validation study. Ophthalmic Epidemiol. 2005;12:223–232. | ||
Singh AD, Turell ME, Topham AK. Uveal melanoma: trends in incidence, treatment, and survival. Ophthalmology. 2011;118:1881–1885. | ||
Nichols EE, Richmond A, Daniels AB. Disparities in uveal melanoma: patient characteristics. Semin Ophthalmol. 2016;31:296–303. | ||
Eskelin S, Kivela T. Mode of presentation and time to treatment of uveal melanoma in Finland. Br J Ophthalmol. 2002;86:333–338. | ||
Damato EM, Damato BE. Detection and time to treatment of uveal melanoma in the United Kingdom: an evaluation of 2,384 patients. Ophthalmology. 2012;119:1582–1589. | ||
Accuracy of diagnosis of choroidal melanomas in the Collaborative Ocular Melanoma Study. COMS report no. 1. Arch Ophthalmol. 1990;108:1268–1273. | ||
Pereira PR, Odashiro AN, Lim LA, et al. Current and emerging treatment options for uveal melanoma. Clin Ophthalmol. 2013;7:1669–1682. | ||
Isager P, Engholm G, Overgaard J, Storm H. Uveal and conjunctival malignant melanoma in Denmark 1943–1997: observed and relative survival of patients followed through 2002. Ophthalmic Epidemiol. 2006;13:85–96. | ||
Blum ES, Yang J, Komatsubara KM, Carvajal RD. Clinical management of uveal and conjunctival melanoma. Oncology (Williston Park). 2016;30:29–32,34–43,48. | ||
Singh AD, Turell ME, Topham AK. Uveal melanoma: trends in incidence, treatment, and survival. Ophthalmology. 2011;118:1881–1885. | ||
Paridaens AD, McCartney AC, Hungerford JL. Multifocal amelanotic conjunctival melanoma and acquired melanosis sine pigmento. Br J Ophthalmol. 1992;76:163–165. | ||
Missotten GS, Keijser S, De Keizer RJ, De Wolff-Rouendaal D. Conjunctival melanoma in the Netherlands: a nationwide study. Invest Ophthalmol Vis Sci. 2005;46:75–82. | ||
Esmaeli B, Wang X, Youssef A, Gershenwald JE. Patterns of regional and distant metastasis in patients with conjunctival melanoma: experience at a cancer center over four decades. Ophthalmology. 2001;108: 2101–2105. | ||
Seregard S. Conjunctival melanoma. Surv Ophthalmol. 1998;42:321–350. | ||
Chang AE, Karnell LH, Menck HR. The National Cancer Data Base report on cutaneous and noncutaneous melanoma: a summary of 84,836 cases from the past decade. The American College of Surgeons Commission on Cancer and the American Cancer Society. Cancer. 1998;83:1664–1678. | ||
Yu GP, Hu DN, McCormick S, Finger PT. Conjunctival melanoma: is it increasing in the United States? Am J Ophthalmol. 2003;135:800–806. | ||
Tuomaala S, Eskelin S, Tarkkanen A, Kivela T. Population-based assessment of clinical characteristics predicting outcome of conjunctival melanoma in whites. Invest Ophthalmol Vis Sci. 2002;43:3399–3408. | ||
Graell X, Caminal JM, Masuet C, et al. Age distribution of uveal melanoma and its relationship to survival. Arch Soc Esp Oftalmol. 2007;82:343–347. | ||
Anastassiou G, Heiligenhaus A, Bechrakis N, Bader E, Bornfeld N, Steuhl KP. Prognostic value of clinical and histopathological parameters in conjunctival melanomas: a retrospective study. Br J Ophthalmol. 2002;86:163–167. | ||
Kimura K, Usui Y, Goto H. Clinical findings and prognosis of 11 cases of conjunctival malignant melanoma. Nippon Ganka Gakkai Zasshi. 2012;116:503–509. | ||
Hu DN, Yu G, McCormick SA, Finger PT. Population-based incidence of conjunctival melanoma in various races and ethnic groups and comparison with other melanomas. Am J Ophthalmol. 2008;145:418–423. | ||
Margo CE. The Collaborative Ocular Melanoma Study: an overview. Cancer Control. 2004;11:304–309. | ||
Shields CL. Conjunctival melanoma: risk factors for recurrence, exenteration, metastasis, and death in 150 consecutive patients. Trans Am Ophthalmol Soc. 2000;98:471–492. | ||
Lim LA, Madigan MC, Conway RM. Conjunctival melanoma: a review of conceptual and treatment advances. Clin Ophthalmol. 2013;6:521–531. | ||
Diener-West M, Earle JD, Fine SL, et al. The COMS randomized trial of iodine 125 brachytherapy for choroidal melanoma, III: initial mortality findings. COMS Report No. 18. Arch Ophthalmol. 2001;119:969–982. | ||
Singh AD, Shields CL, Shields JA. Prognostic factors in uveal melanoma. Melanoma Res. 2001;11:255–263. | ||
Abrams MJ, Gagne NL, Melhus CS, Mignano JE. Brachytherapy vs. external beam radiotherapy for choroidal melanoma: survival and patterns-of-care analyses. Brachytherapy. 2016;15:216–223. | ||
The Collaborative Ocular Melanoma Study (COMS) randomized trial of pre-enucleation radiation of large choroidal melanoma II: initial mortality findings. COMS report no. 10. Am J Ophthalmol. 1998;125:779–796. | ||
Diener-West M, Hawkins BS, Markowitz JA, Schachat AP. A review of mortality from choroidal melanoma. II. A meta-analysis of 5-year mortality rates following enucleation, 1966 through 1988. Arch Ophthalmol. 1992;110:245–250. | ||
Kroll S, Char DH, Quivey J, Castro J. A comparison of cause-specific melanoma mortality and all-cause mortality in survival analyses after radiation treatment for uveal melanoma. Ophthalmology. 1998;105:2035–2045. | ||
Seddon JM, Gragoudas ES, Egan KM, et al. Relative survival rates after alternative therapies for uveal melanoma. Ophthalmology. 1990;97:769–777. | ||
Seregard S. Long-term survival after ruthenium plaque radiotherapy for uveal melanoma. A meta-analysis of studies including 1,066 patients. Acta Ophthalmol Scand. 1999;77:414–417. | ||
Oosterhuis JA, Journee-de Korver HG, Kakebeeke-Kemme HM, Bleeker JC. Transpupillary thermotherapy in choroidal melanomas. Arch Ophthalmol. 1995;113:315–321. | ||
Journee-de Krver H, Schalij-Delfos N, Imhof S. Uveal malignant melanoma: management options – thermotherapy. In: Singh A, Damato B, Pe’er J, editors. Clinical Ophthalmic Oncology. Philadelphia, PA: Saunders Elsevier; 2007:232–240. | ||
Shields CL, Shields JA, Perez N, Singh AD, Cater J. Primary transpupillary thermotherapy for small choroidal melanoma in 256 consecutive cases: outcomes and limitations. Ophthalmology. 2002;109: 225–234. | ||
Robertson DM, Buettner H, Bennett SR. Transpupillary thermotherapy as primary treatment for small choroidal melanomas. Arch Ophthalmol. 1999;117:1512–1519. | ||
Harbour JW, Chao DL. A molecular revolution in uveal melanoma: implications for patient care and targeted therapy. Ophthalmology. 2014;121:1281–1288. | ||
Moser JC, Pulido JS, Dronca RS, McWilliams RR, Markovic SN, Mansfield AS. The Mayo Clinic experience with the use of kinase inhibitors, ipilimumab, bevacizumab, and local therapies in the treatment of metastatic uveal melanoma. Melanoma Res. 2015;25:59–63. | ||
Triozzi P. Dacarbazine and Recombinant Interferon Alfa-2b in Treating Patients With Primary Uveal Melanoma With Genetic Imbalance. ClinicalTrials.gov Identifier: NCT01100528; 2016. | ||
Wen X, Lu L, He Z, Fan X. Orchestrating epigenetic roles targeting ocular tumors. Onco Targets Ther. 2016;9:1001–1009. | ||
Venza M, Visalli M, Beninati C, Biondo C, Teti D, Venza I. Role of genetics and epigenetics in mucosal, uveal, and cutaneous melanomagenesis. Anticancer Agents Med Chem. 2016;16(5):528–538. | ||
Rajaii F, Asnaghi L, Enke R, Merbs SL, Handa JT, Eberhart CG. The demethylating agent 5-Aza reduces the growth, invasiveness, and clonogenicity of uveal and cutaneous melanoma. Invest Ophthalmol Vis Sci. 2014;55:6178–6186. | ||
Dai W, Zhou J, Jin B, Pan J. Class III-specific HDAC inhibitor Tenovin-6 induces apoptosis, suppresses migration and eliminates cancer stem cells in uveal melanoma. Sci Rep. 2016;6:22622. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.