Back to Journals » Clinical Ophthalmology » Volume 9
Ocular manifestations of rheumatoid arthritis and their correlation with anti-cyclic citrullinated peptide antibodies
Authors Vignesh APP, Srinivasan R
Received 8 November 2014
Accepted for publication 31 December 2014
Published 25 February 2015 Volume 2015:9 Pages 393—397
DOI https://doi.org/10.2147/OPTH.S77210
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Ammapati Paul Pandian Vignesh, Renuka Srinivasan
Department of Ophthalmology, Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry, India
Purpose: To study the ocular manifestations of rheumatoid arthritis and to correlate the role of anti-cyclic citrullinated peptide antibody (anti-CCP antibody) with the ocular manifestations.
Methods: Three-hundred and ninety-two eyes of the 196 rheumatoid arthritis patients who attended the ophthalmology outpatient department underwent a detailed ocular examination using slit lamp biomicroscopy and ophthalmoscopy. The tear function of all the patients was assessed using Schirmer’s test, tear film break-up time and ocular surface staining. The anti-CCP antibody titers for all the rheumatoid arthritis patients were estimated using enzyme-linked immunosorbent assay tests.
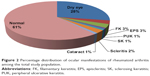
Results: Seventy-seven patients (135 eyes, 39%) out of the 196 patients studied had ocular manifestations typical of rheumatoid arthritis. Dry eye was the most common manifestation (28%, 54 patients). Of the patients, 78% was females (60 patients). The mean duration of rheumatoid arthritis in patients with ocular manifestations was 5.4±2.7 years and without ocular manifestations was 2.1±1.6years. Three percent of the patients had episcleritis (six patients). Scleritis was present in 2% of the patients (four patients). Peripheral ulcerative keratitis and sclerosing keratitis was present in 1% of the population each (two patients each). Eighty-five percent (66 patients) had bilateral manifestations 15% (eleven patients) had unilateral manifestations. There was a strong association between the presence of anti-CCP antibodies and ocular manifestations of rheumatoid arthritis which was shown by the statistically significant P-value of <0.0001.
Conclusion: Ocular manifestations are a significant part of the extra-articular manifestation of rheumatoid arthritis. Dry eye was the most common ocular manifestation. There was a statistically significant association between the presence of anti-CCP antibodies specific to rheumatoid arthritis and the ocular manifestations.
Keywords: rheumatoid arthritis, ocular manifestations, anti-CCP antibodies, dry eye, scleritis, peripheral ulcerative keratitis
Introduction
Rheumatoid arthritis (RA) is a chronic progressive, antibody mediated autoimmune disease that primarily affects small joints. It also involves other organs and ophthalmic involvement is often significant, causing varying degrees of ocular morbidity. Ocular manifestations of RA include dry eye, episcleritis, scleritis and peripheral ulcerative keratitis (PUK).1 Although rheumatoid factor (RF) is commonly used for diagnosis, anti-cyclic citrullinated peptide antibodies (anti-CCP antibodies) are a more sensitive and specific marker of systemic involvement in RA than rheumatoid factor antibody. Anti-CCP antibody is emerging as the preferred diagnostic marker for RA especially in early cases. It also predicts the future occurrence of the disease in undifferentiated arthritis. The sensitivity and specificity of anti-CCP reactivity for RA patients diagnosed based on American College of Rheumatology criteria were detected as 73.5% and 100%, respectively which shows it to be a highly sensitive and specific marker for the disease.2 In this study we correlate the presence of ocular manifestations and the presence of anti-CCP antibodies.
Methodology
The study group consisted of 196 patients who presented for the first time to the outpatient clinic of the department of ophthalmology and immunology. The study was approved by the institute’s ethics committee.
Inclusion criteria
All patients with RA undergoing routine ophthalmologic screening.
Exclusion criteria
- Presence of other autoimmune systemic disorders like systemic lupus erythematosus, graft versus host disease, and any immunosuppressive disorders.
- History of radiation.
- Drug induced ocular manifestations which includes hydroxychloroquine induced maculopathy and other effects induced by chronic immunosuppression.
- Age less than 18 years.
Parameters studied in the patient
The age, sex, and demographic data were initially collected from the patient. A detailed anterior segment examination using slit lamp was done to detect episcleritis, scleritis, and corneal changes. Dry eye examination was done using Schirmer’s test, tear film break-up time, and ocular staining score. Fundus examination was done to detect any posterior segment manifestations. The anti-CCP antibody levels were detected using enzyme-linked immunosorbent assay (ELISA); and chi-square test was used to correlate their significance to ocular manifestations.
Procedure
Patients were subjected to a thorough clinical examination to confirm the diagnosis of arthritis. Erythrocyte sedimentation rate, auto-antibodies specific to RA, and X-rays were done in all patients. The anti-CCP antibody level was detected using ELISA test (DIASTAT; Axis-Shield Diagnostics Ltd., Dundee, Scotland, UK). Serum samples collected from patients were used for the ELISA test. A positive test was considered if levels were ≥5 U/mL.2 The diagnosis of RA was made based on the American Rheumatism Association 1987 revised criteria for the diagnosis of RA.3
History of the ocular symptoms was obtained and ocular examination was done in every patient with torch light and slit lamp biomicroscopy. Schirmer’s test was done using Whatman filter paper and tear film break-up time was done using fluorescein stain in all patients to assess lacrimal function. Ocular surface involvement was assessed by fluorescein and Rose Bengal staining. The diagnosis of dry eye was based on the American-European Consensus Criteria for Sjögren’s syndrome which includes the presence of a connective tissue disorder, duration of symptoms >3 months, tear film break-up time <10 seconds, Schirmer’s test (without anesthesia) ≤5 mm/5 minutes, Van Bijsterveld score ≥4,4 the diagnosis of scleritis, episcleritis and PUK is mainly clinical. Scleritis is painful chronic inflammation of sclera which may be associated with vision loss. Episcleritis is a benign, self-limiting condition of the outer coat covering the sclera. PUK is a form of ocular inflammation that involves the outer portions of the cornea associated with progressive thinning. Dilated retinal examination was done using direct and indirect ophthalmoscopy to detect any posterior segment changes.
Observations
Age distribution
One-hundred and ninety-six patients were studied, of these 77 (39%) had ocular manifestations of RA. Most of the patients fell between 30–50 years and the average age (mean ± standard deviation) of the patients was 43.85 years ±21.54 (Table 1 and Figure 1).
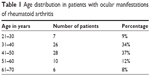  | Table 1 Age distribution in patients with ocular manifestations of rheumatoid arthritis |
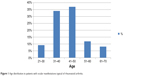  | Figure 1 Age distribution in patients with ocular manifestations typical of rheumatoid arthritis. |
Sex distribution
Of the total 196 patients studied, 150 (77%) were females and 46 (23%) were males. Among the 77 patients who had symptoms typical of RA, 60 (78%) were females and 17 (22%) were males.
Duration of disease and incidence of ocular manifestations
The mean (mean ± standard deviation) duration of RA in patients with ocular manifestations was 5.4±2.7 years and without ocular manifestations was 2.1±1.6 years.
The mean duration of RA among the patients with vision threatening complications like sclerosing keratitis and PUK was 10.5±3.1 years.
Ocular manifestations of RA
Among the 196 patients included in the study 77 (39%) had ocular manifestations typical of RA (Table 2 and Figure 2). Thirty percent (58 patients) of the patients were on immunosuppressive therapy for their systemic condition. Oral steroid was the main agent used. Around 5% (nine patients) of the patients were on other immunosuppressive agents like hydroxychloroquine.
  | Table 2 Demographic data and ocular manifestations of rheumatoid arthritis |
Laterality
Eighty-five percent (66 patients) of the manifestations was bilateral and only 15% (eleven patients) was unilateral which mostly included scleritis, episcleritis, and PUK.
Patients with more than one manifestation
Eighty percent (62 patients) of the patients with ocular involvement had only one manifestation. The remaining 20% (15 patients) had more than one manifestation which mainly included one of the vision threatening manifestations with associated dry eye or cataract.
Visual acuity in patients with ocular manifestations of RA
Eighty-six percent (67 patients) of the patients had normal visual acuity. Fourteen percent (ten patients) of the patients had decreased visual acuity due to manifestations like PUK, sclerosing keratitis, and scleritis and cataract.
Role of anti-CCP antibodies and ocular symptoms typical of RA
Chi-square test was used to analyze the results. The two-sided P-value is <0.0001, considered extremely significant. Odds ratio =4.168. Ninety-five percent confidence interval: 2.256 to 7.698. Hence there is a strong association between the presence of anti-CCP antibodies and ocular manifestations of RA (Table 3).
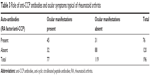  | Table 3 Role of anti-CCP antibodies and ocular symptoms typical of rheumatoid arthritis |
Discussion
Ocular manifestations were found in 77 of the 196 patients studied which is 39% of the study population. Reddy et al in their study also found the incidence of ocular manifestations in RA to be 39% in a population of 100 patients.5 This study indicates that ocular involvement is fairly common and the need for close follow-up. The rheumatologists should get an ocular examination done for all patients at diagnosis and then at periodic intervals for early detection of any ocular involvement. Punjabi et al reported that 27.3% of RA patients had dry eye in an Indian population.6 Bettero et al reported secondary Sjögren’s syndrome in 12.1% of the population with RA.7 In the present study the prevalence of dry eye was 28% and was the most common manifestation of RA. These results were similar to the previous studies mentioned above. The diagnosis of secondary Sjögren’s was made based on the American-European Consensus Criteria for Sjögren’s syndrome which was based on the duration of symptoms, Schirmer’s test, and positive vital dye staining of the eye surface. Tear film osmolarity also correlates with dry eye activity. Tong et al found in a recent study that tear film osmolarity correlated with the dry eye severity score.8 All this suggests that more research is needed on the markers of ocular surface in RA. Tong et al studied the immune factors that lead to dry eye and correlated them with systemic disease which could lead to potential treatment targets in the future showing the importance of conducting further studies on the ocular surface in RA patients.8 Villani et al studied the effect of immunosuppression on the ocular surface via confocal microscopy and cytokines level and found that immunosuppression modified the ocular surface pathology in RA patients with secondary Sjögren’s syndrome.9 Villani et al studied the corneal involvement in RA by confocal microscopy and found the corneal surface activity was more in patients with secondary Sjögren’s.10 The ocular manifestations were more common with prolonged duration of the disease. The severity was also worse with longer duration of the disease. McGavin et al studied 4,210 patients with RA and established the incidence of episcleritis as 0.I7%.11 Bhadoria et al reported episcleritis in 0.93% of the patients of the study population.12 In the present study we found episcleritis in 3% of the RA patients which is slightly higher than the above mentioned studies. Half of the patients with episcleritis had associated dry eye. In our study the vision threatening complications were scleritis, sclerosing keratitis, and PUK which affected 14% of the study population. All the patients with vision threatening complications were positive for anti-CCP antibodies. McGavin et al reported the incidence of scleritis as 0.67% in RA patients.11 In the present study scleritis was found in 2% (four patients) of the study population out of which one case was nodular scleritis and the rest were diffuse scleritis which was comparable to the previous studies. Squirrell et al reviewed the clinical and serological characteristics of the arthritis at the time of presentation of PUK. All patients had a long history of high-titer seropositive, nodular, erosive RA which on presentation of PUK had been quiescent or well controlled for many years.13 In our study the mean duration of RA among the patients with vision threatening complications like sclerosing keratitis and PUK was 10.5 years which was comparable to the abovementioned studies in which the vision threatening complications were associated with longer duration of the disease. Bettero et al reported ulcerative keratitis in 2% of the study population.7 In our study both sclerosing keratitis and PUK were found in 1% of the study population. All the patients had a long history of RA. Among the two patients with sclerosing keratitis one patient had unilateral involvement and only mild impairment of vision. Another patient with sclerosing keratitis had bilateral involvement with vision of 20/200 with associated severe dry eye. Anti-CCP antibodies are a more sensitive and specific marker of RA. Itty et al in their study found that the combined presence of anti-CCP antibodies and RA factor had more severe ocular involvement compared to those who were negative for these antibodies.1 In the present study there was a strong association between the presence of anti-CCP antibodies and the presence of ocular manifestations of RA. This will help in early detection of ocular manifestations of RA which needs corroboration by longitudinal studies.
Conclusion
Ocular manifestations are a significant part of the extra-articular manifestation of RA. Dry eye was the most common ocular manifestation. There was a significant association between the duration of the disease and ocular manifestations. The longer the duration, more common and severe are the ocular manifestations. There was a statistically significant association between the presence of anti-CCP antibodies related to RA and the ocular manifestations.
Disclosure
The authors have no conflicts of interest to disclose.
References
Itty S, Pulido JS, Bakri SJ, Baratz KH, Matteson EL, Hodge DO. Anti-Cyclic Citrullinated Peptide, Rheumatoid Factor, and Ocular Symptoms Typical of Rheumatoid Arthritis. Trans Am Ophthalmol Soc. 2008;106:75–81. | ||
El-Banna H, Jiman-Fatani A. Anti-cyclic citrullinated peptide antibodies and paraoxonase-1 polymorphism in rheumatoid arthritis. BMC Musculoskelet Disord. 2014;15:379. | ||
Arnett FC, Edworthy SM, Bloch DA, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988;31(3):315–324. | ||
Vitali C, Bombardieri S, Jonsson R, et al. Classification criteria for Sjögren’s syndrome: a revised version of the European criteria proposed by the American–European Consensus Group. Ann Rheum Dis. 2002;61(6):554–558. | ||
Reddy SC, Gupta SD, Jain IS, Deodhar SD. Ocular manifestations of rheumatoid arthritis. Indian J Ophthalmol. 1977;25(3):20–26. | ||
Punjabi OS, Adyanthaya RS, Mhatre AD, Jehangir RP. Rheumatoid arthritis is a risk factor for dry eye in the Indian population. Ophthalmic Epidemiol. 2006;13(6):379–384. | ||
Bettero RG, Cebrian RFM, Skare TL. [Prevalence of ocular manifestation in 198 patients with rheumatoid arthritis: a retrospective study]. Arq Bras Oftalmol. 2008;71(3):365–369. Portuguese. | ||
Tong L, Thumboo J, Tan YK, Wong TY, Albani S. The eye: a window of opportunity in rheumatoid arthritis? Nat Rev Rheumatol. 2014;10(9):552–560. | ||
Villani E, Galimberti D, Del Papa N, Nucci P, Ratiglia R. Inflammation in dry eye associated with rheumatoid arthritis: cytokine and in vivo confocal microscopy study. Innate Immun. 2013;19(4):420–427. | ||
Villani E, Galimberti D, Viola F, Mapelli C, Papa ND, Ratiglia R. Corneal Involvement in Rheumatoid Arthritis: An In Vivo Confocal Study. Invest Ophthalmol Vis Sci. 2008;49(2):560–564. | ||
McGavin DD, Williamson J, Forrester JV, et al. Episcleritis and scleritis. A study of their clinical manifestations and association with rheumatoid arthritis. Br J Ophthalmol. 1976;60(3):192–226. | ||
Bhadoria DP, Bhadoria P, Sundaram KR, Panda A, Malaviya AN. Ocular manifestations of rheumatoid arthritis. J Indian Med Assoc. 1989;87(6):134–135. | ||
Squirrell DM, Winfield J, Amos RS. Peripheral ulcerative keratitis “corneal melt” and rheumatoid arthritis: a case series. Rheumatol (Oxford). 1999;38(12):1245–1248. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.