Back to Journals » Risk Management and Healthcare Policy » Volume 14
Observation of the Effectiveness of a Diagnostic Model for Acute Abdominal Pain Based on the Etiology Checklist and Process Thinking
Authors Pan H, Li H, Shen Z, Guo H, Zhao Q, Li J
Received 1 December 2020
Accepted for publication 27 January 2021
Published 26 February 2021 Volume 2021:14 Pages 835—845
DOI https://doi.org/10.2147/RMHP.S295142
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Marco Carotenuto
Hong-ming Pan,1,* Hong-ling Li,2,* Zhang-shun Shen,2 Hui Guo,2 Qian Zhao,2 Jian-guo Li2
1Graduate School of Hebei Medical University, Shijiazhuang, 050051, People’s Republic of China; 2Department of Emergency Medicine, Hebei General Hospital, Shijiazhuang, 050051, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jian-guo Li
Department of Emergency Medicine, Hebei General Hospital, No. 348 Heping West Road, Shijiazhuang, 050051, People’s Republic of China
Tel +86 31185988361
Email [email protected]
Objective: The present study aimed to explore the effectiveness of the etiology checklist and process thinking in the differential diagnosis for acute abdominal pain.
Methods: A retrospective design was used to include 5,403 patients with acute abdominal pain in the Emergency Department of Hebei Provincial People’s Hospital. The patients with acute abdominal pain between July and December 2017 in whom the etiology checklist and process thinking were not implemented were selected as the traditional group. Those with acute abdominal pain between July and December 2018 in whom the etiology checklist and process thinking were implemented were selected as the process thinking group. The clinical data, such as the emergency length of stay, hospitalization expenses, hospitalization length of stay, diagnostic accuracy, and outcome, were compared between the two groups.
Results: For patients at emergency level 2 and above, the average emergency length of stay was shorter in the process thinking group than in the traditional group, while the average emergency length of stay was longer for patients at emergency level 3. For hospitalized patients at emergency level 2 and above and patients at emergency level 3, those in the process thinking group had improved diagnostic accuracy, shorter average hospitalization length of stay, reduced average hospital expenses, and improved outcomes. In the comparison among six physicians, the results in the traditional group were inconsistent and statistically different in terms of the average emergency length of stay and diagnostic accuracy, while the results in the process thinking group tended to be consistent. The differences were not statistically different.
Conclusion: The diagnostic model for acute abdominal pain based on the etiology checklist and process thinking could improve the diagnostic accuracy and outcomes for patients with acute abdominal pain.
Keywords: acute abdominal pain, emergency diagnosis, lateral thinking, process thinking
Introduction
Acute abdominal pain is caused by diseases inside the abdominal cavity, together with some extra-abdominal, thoracic, and systemic diseases, with an onset of less than one week. These diseases may require urgent intervention, such as surgery.1 As one of the most common diseases in the emergency room, there are about five million patients with acute abdominal pain in the United States yearly. The number of cases constitutes around 30% of the total number of patients in the emergency departments,2 and it has increased year by year.3 In China, patients with abdominal pain account for more than 20% of the emergency cases, with a mortality rate of 0.5%–5.0%.4
Acute abdominal pain often involves different specialties, such as internal medicine, surgery, gynecology, and pediatrics. It often originates from diseases of the digestive system, but it may also be caused by extra-abdominal diseases, such as acute myocardial infarction and pneumonia. Moreover, acute abdominal pain may also be a clinical manifestation in neurological and psychiatric diseases. Although research on the thinking and process of diagnosing acute abdominal pain has continued at the national and international level, there is a lack of high-quality evidence to guide the diagnosis of acute abdominal pain. The first worldwide English-language practice guidelines on the management of acute abdominal pain, the Basic Clinical Practice Guidelines for Acute Abdominal Care, were published in 2015 after three years’ research by five medical research teams.5 However, owing to the complexity of acute abdominal pain, the guidelines do not play a positive role in the actual clinical practice. Many domestic models for the diagnosis and treatment of abdominal pain are only empirical summaries, and most of the models have not been recognized.
As the misdiagnosis rate of abdominal pain is high, it is important to diagnose and treat acute abdominal pain comprehensively and accurately within a specific duration in emergency medicine. The present study aimed to explore the effectiveness of the etiology checklist and process thinking in the differential diagnosis for acute abdominal pain.
Materials and Methods
Research Subjects and Design
A diagnostic model of process thinking of the etiology for acute abdominal pain was developed in the authors’ department in March 2018. Through a retrospective comparative analysis during the study period from July 1 to December 31, 2018, a more mature application of process thinking was selected. Adult patients with a principal complaint of abdominal pain for the first time during this period were chosen as the study subjects and enrolled in the process thinking group (the process thinking diagnostic model). Patients in whom process thinking was not used for the etiology of acute abdominal pain between July 1 and December 31, 2017 were enrolled in the traditional group (the traditional diagnostic model). A total of 11 physicians were involved in the consultation in both periods. Patients seen by the six physicians who were involved in the entire consultation in both periods were selected for the study to reduce the confounding factors. The diagnosis and treatment were completed independently. This study was approved by the Ethics Committee of Hebei General Hospital, and all patients signed informed consent.
The Inclusion Criteria
The Neusoft Medical Information System emergency triage platform was adopted with “acute abdominal pain, abdominal pain, abdominal distension, abdominal discomfort, abdominal ache, stomach pain, stomach-ache, peri-umbilical pain” as the search terms to fuzzily retrieve the emergency patients.
The Exclusion Criteria
Patients aged under 14, patients with abdominal pain caused by trauma, patients transferred from other medical institutions, patients who had attended the emergency department previously, patients with an emergency length of stay of fewer than five minutes or more than six hours,6,7 patients at level 4 of the non-emergency rating, patients who left the hospital voluntarily, and patients with incomplete data.
The Traditional Diagnostic Model
According to the guidelines for classifying the emergency patients published by the Ministry of Health in August 2011,8 the patients were classified by the attending physician based on the severity of the disease. Patients with different classifications were assigned to corresponding examinations by the attending physician according to the traditional diagnostic pattern. This was disease-oriented, following the rule that common and frequent diseases had priority, then rare diseases. Organic diseases had priority, followed by functional diseases. If the preliminary diagnosis was rejected, other possible diseases were considered and verified until the diagnosis was confirmed. In the second evaluation and dynamic observation, all the information was integrated, and the patients were kept under observation if life-threatening diseases could not be excluded.
The Process Thinking Diagnostic Model
The Establishment of the Etiology Checklist for Acute Abdominal Pain
The textbooks on diagnostics, internal medicine, and emergency medicine were collected to list the symptomatological etiologies for abdominal pain. The etiologies of non-traumatic acute abdominal pain in adults were reorganized with the combination of anatomy and diagnostics. The concept of “the whole person” was introduced, and the etiologies of abdominal pain were reclassified. The easy-to-remember etiology checklist for abdominal pain that could guide the direction of diagnosis for abdominal pain was established as follows: 1) local diseases: the abdominal cavity (inflammation, rupture, obstruction, torsion, vascular diseases), and the abdominal wall; 2) adjacent organs; 3) systematic diseases; 4) functional diseases; 5) gynecological diseases. Since gynecological diseases have a special place in the etiology of abdominal pain, we listed those diseases in a separate category to facilitate memory and differential diagnosis. The diseases associated with each category were listed at the next level of the etiological classification of the anatomical or pain mechanism, as shown in Table 1.
 |
Table 1 The Etiology Checklist for Abdominal Pain |
The Triaged Diagnosis and Treatment Based on the Checklist
For patients with critical abdominal pain, the principle of step-down thinking was followed9 to quickly screen for possible life-threatening diseases on the etiology checklist. Safe, appropriate, and inexpensive laboratory and bedside examinations were conducted to understand the pathophysiological state and clarify the direction of diagnosis earlier. Subsequently, the sequence of priority, prevalence, and ease of implementation was followed to facilitate the screening process (Figure 1). For patients with non-critical abdominal pain, the checklist was used as a guide to collect information through historical inquiry and physical examinations to perform stratified and titrated screening together with targeted laboratory and imaging examinations.
 |
Figure 1 The emergency flow chart of diagnosis and treatment. |
Data Collection
The detailed information concerning each patient was collected from the emergency triage platform. This included general information, such as age, gender, time of onset, and level of classification. Clinical data, such as the emergency length of stay (the time difference between the point when the physician was attending the patient and the point when the patient left the emergency room), was also included. Hospitalization expenses, hospitalization length of stay, diagnostic accuracy (measured by whether the emergency diagnosis in the admission notification was the same as the inpatient diagnosis at discharge), and outcome (cured, improved, not cured, died), was also collected from the emergency triage platform. According to the disease classification, the differences in the emergency length of stay, hospitalization expenses, hospitalization length of stay, outcome, and emergency diagnostic accuracy for patients at level 2 or above or level 3 were compared, respectively. The differences in the emergency length of stay and emergency diagnostic accuracy were compared between the traditional group and the process thinking group among the six attending physicians.
Statistical Analysis
SPSS 21.0 software (International Business Machines Corporation, Armonk, New York, USA) was used for the data analysis. The measurable data, including the age, time of onset, emergency length of stay, average hospitalization length of stay, and average hospitalization expenses for patients, were expressed as mean ± standard deviation (x ± SD) for those who met the normal distribution, and median (interquartile interval) for those who did not meet the normal distribution. Chi-square tests were used for comparisons between groups. The Chi-square test was used for countable data, including the male/female ratio, level of classification, and diagnostic accuracy. P < 0.05 was considered statistically significant.
Results
A total of 2,662 patients comprising 1,394 males and 1,268 females were included in the traditional group, and 2,741 patients comprising 1,403 males and 1,338 females were included in the process thinking group. The average age was 42.42 ± 18.38 years in the traditional group and 41.73 ± 18.49 years in the process thinking group. The average time of onset was 21.12 ± 29.71 hours in the traditional group and 22.15 ± 31.00 hours in the process thinking group. There was no significant difference in general characteristics, such as time of onset, male/female ratio, and age, between the two groups (p > 0.05), indicating that the two groups’ data were comparable.
The Evaluation of the Emergency Length of Stay
The Comparative Analysis of Emergency Length of Stay in Patients at Emergency Level 2 and Above Between the Traditional and Process Thinking Groups
The results of the analysis revealed that there were no statistically significant differences in the proportion of patients at level 1 and level 2, male/female ratio, average age, and average time of onset between the two groups. The average emergency length of stay was shorter in the process thinking group than in the traditional group, and the difference was statistically significant (p < 0.05, as shown in Table 2).
 |
Table 2 The Comparative Analysis of the Emergency Length of Stay of Patients at the Level Above 2 Between the Traditional Group and the Process Thinking Group |
The Comparative Analysis of Emergency Length of Stay in Patients in Emergency Level 3 Between the Traditional and Process Thinking Groups
There were no statistically significant differences in the male/female ratio, average age, and average time of onset between the two groups. The average emergency length of stay was longer in the process thinking group than in the traditional group, and the difference was statistically significant (p < 0.05, as shown in Table 3).
 |
Table 3 The Comparative Analysis of the Emergency Length of Stay of Patients at Level 3 Between the Traditional Group and the Process Thinking Group |
The Comparative Analysis of the Diagnostic Accuracy, Average Hospitalization Length of Stay, Average Hospitalization Expenses, and Outcome in the Hospitalized Patients
The Hospitalized Patients at Emergency Level 2 and Above
There were no statistically significant differences between the two groups in male/female ratio, average age, the average time of onset, proportion of the level of disease classification, and proportion of medical and surgical patients. The process thinking group had higher diagnostic accuracy, shorter average emergency length of stay, fewer hospitalization expenses, shorter hospitalization length of stay, and a more improved outcome than the traditional group. The differences between the two groups were statistically significant (p < 0.05, as shown in Table 4).
The Hospitalized Patients at Emergency Level 3
There were no statistically significant differences in the male/female ratio, average age, average onset time, proportion of the level of disease classification, and proportion of medical and surgical patients between the two groups. The process thinking group had higher diagnostic accuracy, longer average emergency length of stay, fewer hospitalization expenses, shorter hospitalization length of stay, and a more improved outcome than the traditional group. The differences between the two groups were statistically significant (p < 0.05, as shown in Table 5).
Comparison of Emergency Length of Stay and Diagnostic Accuracy of Patients Admitted Before and After the Establishment of Process Thinking of the Etiology for Abdominal Pain Among Physicians
Among the six physicians in the present study, physician 1, physician 2, physician 3, and physician 4 were the attending physicians, and physician 5 and physician 6 were the deputy chief physicians. All had several years of professional experience in emergency medicine.
There was a statistical difference in average emergency length of stay and diagnostic accuracy in hospitalized patients in the traditional group among different physicians (p < 0.05, as shown in Table 6).
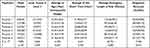 |
Table 6 The Comparative Analysis of the Emergency Length of Stay and the Diagnostic Accuracy of Patients in the Traditional Group Among Different Physicians |
There was no statistical difference in emergency length of stay and diagnostic accuracy in hospitalized patients in the process thinking group among different physicians. The results tended to be consistent (p < 0.05, as shown in Table 7).
 |
Table 7 The Comparative Analysis of the Emergency Length of Stay and the Diagnostic Accuracy of Patients in the Process Thinking Group Among Different Physicians |
Discussion
The diagnostic model for acute abdominal pain based on the etiology checklist and process thinking in the present study was different from the previous traditional diagnostic methods. Currently, courses on acute abdominal pain are disease-centered, ranging from the disease, etiology, and pathophysiology to clinical manifestations, auxiliary examinations, and treatment principles. The real clinical practice begins with symptoms, which is the opposite of those in the textbooks. Clinicians must redigest and summarize the disease-oriented theory of “etiology-clinical manifestation-diagnosis” and translate it into the symptom-oriented application in clinical practice, which increases the complexity of clinical practice. Generally, it takes years of study and experience to explain the knowledge structure of diagnosis. Only the expert can establish a complete differential diagnosis in a short period with the help of symptoms. This is difficult for inexperienced young doctors, and even senior doctors may make mistakes.10 Moreover, the traditional diagnostic process is in line with the hypothesis-based deductive reasoning proposed by Barrows and Picknell (1991),11 that is, from the symptoms directly to the disease, first putting forward the hypothesis of one or more possible diseases, and then verifying it through a variety of examinations. The traditional way of thinking belongs to homeopathic thinking, which saves time and effort and is simple and fast but with insufficient lateral thinking. Consequently, clinical decisions rely on personal experience. The present study was oriented with the symptoms of abdominal pain, with all the possible etiologies of abdominal pain being integrated. This not only conformed to the real-life consultation process but also worked backward from the etiology of abdominal pain to screen possible diseases by severity and prevent misdiagnosis and missed diagnosis. The results revealed that the diagnostic accuracy was higher in the process thinking group than in the traditional group for the patients at both level 2 and level 3. As early as 1991, this “symptom-oriented model of diagnosis and treatment” was introduced into clinical teaching and achieved good results in the University of Calgary Faculty of Medicine, Canada, with a symptom-oriented course structure.12,13 This model confirmed the results of the present study.
The first information an emergency physician obtains from a patient with acute abdominal pain is a complaint of an acute onset of abdominal pain, not a particular disease. The symptoms in a patient are often not directly derived from the original disease. One clinical manifestation does not represent a single disease, and a group of clinical manifestations cannot represent one disease. One etiology may have multiple symptoms, and multiple symptoms may be the etiology of one disease.14 The complexity of the clinical presentation is a challenge for the emergency physician. The diagnostic list of differential diagnoses is extremely extensive, and each physician must memorize hundreds of diseases together with the manifestations, making it an onerous task for any physician and a challenge for the time-pressed emergency physician. How to deal with this task has been a challenge for emergency physicians. In the present study, the etiologies of non-traumatic acute abdominal pain in adults were reorganized with the combination of anatomy and diagnostics. The concept of “holistic medicine” was introduced, and the etiologies of abdominal pain were reclassified. The easy-to-remember etiology checklist for abdominal pain that could guide the diagnosis direction of abdominal pain was established as follows: 1) local diseases: the abdominal cavity (inflammation, rupture, obstruction, torsion, vascular diseases), and the abdominal wall; 2) adjacent organs; 3) systematic diseases; 4) functional diseases; 5) gynecological diseases, which acted as the top layer in a modular differential diagnosis program. Since gynecological diseases have a special place in the etiology of abdominal pain, this item was listed in a separate category to facilitate memory and differential diagnosis.
Concerning the effectiveness of the “checklist,” Artur Govender describes it as follows. The application of a checklist had reduced the percentage of infections of central venous intubation from 11% to zero across the hospital, avoided 43 cases of infection and eight cases of fatality, and saved $2 million in costs in the hospital.15 Hales et al16 suggested that the checklist was important for reducing the risk of costly errors and improving the overall outcomes. In an 18-month study, Pronovost et al17 showed that the application of the checklist in critical care medicine reduced the rate of catheter-related bloodstream infections by 66%. The Mayo Clinic in the United States designed and used the Critical Illness Early Identification and Treatment Checklist (CERTAIN) and has demonstrated the reliability and validity of CERTAIN.18,19 Despite the demonstrated benefits of the checklist in medicine and critical care, its incorporation into clinical applications has not been as rapid and widespread as in other areas. There is currently no national or international report concerning its application in the diagnosis of acute abdominal pain.
For critically ill patients, time is one of the vital factors for successful treatment. Therefore, in the area of emergency, there is a saying of “shoot first and aim later,” which means that for critically ill patients with abdominal pain, “preemptive” treatment will be given according to the pathophysiological changes to save lives, which is the core content of step-down thinking.9 Preemptive examination guided by process thinking is the use of safe, appropriate, and inexpensive examinations and bedside examinations for potentially life-threatening illnesses on the thinking checklist. This is in addition to the initial assessment and treatment of critically ill patients, which will complement the step-down thinking. However, “preemptive” examination is not the same as “blind” examination, nor is it a “full set” of examinations. It is based on the critical status. All the potentially fatal diseases on the checklist for abdominal pain need to be screened in a process, which is also a targeted examination. The comparison with the traditional group showed that the emergency length of stay for patients at level 2 and above was shorter in the checklist group than in the traditional group. This might be due to the early targeted examinations for possible risk factors under the guidelines of the checklist, avoiding multiple trips between the emergency room and the Computed Tomography (CT) room, reducing the waiting time for repeated blood sampling and laboratory results, and effectively reducing the emergency length of stay for patients with critical abdominal pain (as shown in Table 2). Furthermore, the conditions concerning the hospitalization were analyzed in patients at level 2 and above (Table 4). In addition to the shorter emergency length of stay compared with the traditional group, the “preemptive” examination under the guidelines in the checklist led to an increase in emergency diagnostic accuracy in the process thinking group, as well as a significant advantage in terms of hospitalization length of stay, hospitalization expenses, and outcome. This is consistent with the findings of Yang et al20 that timely diagnosis and treatment of acute pulmonary embolism in the emergency room improved the therapeutic effect and prognosis. Although the implementation of the “preemptive” examination included some negative examination results that might increase the expense, “preemptive” examination was not only a necessary means of implementing the step-down thinking but also a concrete manifestation of “life first” medical humanism. For patients in level 3 with non-critical abdominal pain, since no life-threatening changes occur within a short period and time urgency is not emphasized, a “titrated” triaged diagnosis guided by the etiology checklist was implemented to improve the diagnostic accuracy. Moreover, since the preliminary diagnosis is often subjective, secondary assessment and dynamic observation must continually be conducted following process thinking of abdominal pain, especially in disorders where early symptoms are not obvious in the list of abdominal pain.21 This is also a reflection of the dynamic nature of clinical thinking.22 The results of the present study revealed that for patients in level 3 with non-critical abdominal pain, the “titrated” triaged diagnosis and dynamic observation under the guidance of the thinking checklist led to a longer emergency length of stay (as shown in Table 3). This might be due to the lack of a more effective process of differential diagnosis and dynamic observation in the traditional thinking mode of direct diagnosis based on the clinical experience and targeted examination for patients with relatively mild illnesses, such as suspected acute gastroenteritis and urinary stones, resulting in shorter diagnosis time and reduced diagnostic accuracy. Many clinical diseases with nausea, vomiting, abdominal pain, diarrhea, and other manifestations similar to acute gastroenteritis can be misdiagnosed or lead to a missed diagnosis.23 A Korean study on primary cerebellar hemorrhage showed that in around 9% of patients, cerebellar hemorrhage was misdiagnosed as gastroenteritis since the early cerebellar hemorrhage might be accompanied by nausea or vomiting without other neurological signs or symptoms, and the neurological examinations were ignored by the attending physician.24 In addition, for urinary stones, a misdiagnosis analysis was performed as early as 1983,25 and related case reports are even more frequently published.26–28 Process thinking requires the attending physician to use the checklist as a guide for “titrated” triaged diagnosis and dynamic observation. Even for patients with mild abdominal pain, such as gastroenteritis and urinary stones, examinations should be screened according to the checklist, and the possibility of other diseases should be considered. Although this will take more time, it can improve diagnostic accuracy. The results of the present study revealed that the hospitalized patients at level 3 had a relative reduction in hospitalization expenses and hospitalization length of stay and an improved prognosis (as shown in Table 5). This was probably due to the improved diagnostic accuracy in the emergency department, which led to a clearer and more effective treatment plan after hospitalization.
Emergency medicine is an interdisciplinary clinical discipline with a wide spectrum of diseases, which requires rapid and correct diagnosis and timely and reasonable treatment with great unpredictability and uncertainty. Although experience can bring us closer to the diagnostic goal quickly, it can also lead to inertia,29 which might result in “the benevolent see benevolence, the wise see the wisdom,” and there is a tendency for different doctors to treat the patients differently. Even under the same conditions, the treatment of the same disease varies greatly from hospital to hospital and doctor to doctor. One of the focal issues in emergency medicine is how to be “fast and accurate,” ensure patient safety, and achieve homogeneous results in emergency diagnosis and treatment. In the present study, a comparison was conducted among six physicians of different levels of seniority. It revealed that there was a difference in diagnostic accuracy and emergency length of stay among six physicians in the traditional group (as shown in Table 6), which meant that different levels of seniority and experience produced different decisions. With the establishment of the etiology checklist for acute abdominal pain, it was found that there was no difference in the length of stay and diagnostic accuracy among the same six physicians in the process thinking group (as shown in Table 6) together with improved diagnostic accuracy in general when compared with those in the traditional group. In the present study, the etiology checklist for abdominal pain was concise and flexible. When emergency physicians were faced with patients with acute abdominal pain, they no longer needed to consider “what’s the disease and how to treat it,” but only needed to follow the checklist, thus avoiding the difference in clinical judgment caused by different levels of experience. Of course, we could not ignore the role of clinical experience, and process thinking might be the summation and sublimation of expert experience. The etiology checklist for abdominal pain provided direction for the preliminary diagnosis, but some clinical experience was also required in the determination of specific diseases. However, relying too much on experience may lead to empirical myths and inertia, which is risky. Historically, the process of disease diagnosis, differential diagnosis, and treatment has been an evolving process of thinking and decision-making, as empirical medicine and medical technology have evolved over the decades.
One of the limitations in the present study is that owing to the lack of strong support in the information system, the per capita expenses of outpatients were not compared with the overall expenses of patients with abdominal pain. There was also a lack of persuasion regarding whether it might lead to overmedication. The present study was a single-center retrospective study, and therefore, the impact of practices, process improvements, and the progress of physicians in our hospital on the outcomes needs to be confirmed by a multicenter study.
Conclusion
The core of emergency medicine is the priority of diagnosing and treating the critically ill patient, and the treatment of acute abdominal pain should be in line with this principle. The establishment of the abdominal pain etiology checklist and process thinking might capture the diagnostic direction from the local to the whole and form a holistic and systematic fixed structured plan.30 This might lead to rapid treatment, shorten the average emergency length of stay for patients with abdominal pain, improve the diagnostic accuracy, shorten the average hospitalization length of stay, reduce the average hospitalization expenses, realize systematic clinical decision-making, and improve the overall safety. The establishment of the checklist might provide the emergency physicians with a common starting point for the diagnosis and treatment of acute abdominal pain, which could be conducive to the eventual homogenization of the initial practice of emergency medicine.
Ethics Approval and Consent to Participate
I confirm that I have read the Editorial Policy pages. This study was conducted with approval from the Ethics Committee of our hospital. This study was conducted in accordance with the declaration of Helsinki. Written informed consent was obtained from all participants.
Acknowledgments
We would like to acknowledge the hard and dedicated work of all the staff that implemented the intervention and evaluation components of the study.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
1. Hustey FM, Meldon SW, Banet GA, Gerson LW, Blanda M, Lewis LM. The use of abdominal computed tomography in older ED patients with acute abdominal pain. Am J Emerg Med. 2005;23(3):259–265. doi:10.1016/j.ajem.2005.02.021
2. Lyon C, Clark DC. Diagnosis of acute abdominal pain in older patients. Am Fam Physician. 2006;74(9):1537–1544.
3. Hastings RS, Powers RD. Abdominal pain in the ED: a 35 year retrospective. Am J Emerg Med. 2011;29(7):711–716. doi:10.1016/j.ajem.2010.01.045
4. Zhang Y, Wang Y, Li X, et al. Analysis on the regularity of emergency disease spectrum of 106 551 patients. Chin J Critical Care Med. 2016;36(3):254–257.
5. Mayumi T, Yoshida M, Tazuma S, et al. Practice guidelines for primary care of acute abdomen 2015. J Hepatobiliary Pancreat Sci. 2016;23(1):3–36. doi:10.1002/jhbp.303
6. McCaig LF, Nawar EW. National hospital ambulatory medical care survey: 2004 emergency department summary. Adv Data. 2006;372:1–29.
7. Henneman PL, Nathanson BH, Li H, et al. Emergency department patients who stay more than 6 hours contribute to crowding. J Emerg Med. 2010;39(1):105–112. doi:10.1016/j.jemermed.2008.08.018
8. Ministry of Health of the People’s Republic of China. Guiding Principles for grading the condition of emergency patients (draft for comments). Chin J Crit Care Med. 2011;04(4):241–243.
9. Wang P. Unique clinical thinking in emergency - ladder differential diagnosis. Int J Emerg Critical Care Med. 2007;3:1828.
10. Li L, Li B, Wang M. Misdiagnosis and misdiagnosis of acute abdomen. Chin J Emerg Resuscitat Disaster Med. 2019;14(6):598–600.
11. Tibbles A. Developing clinical problem-solving skills a guide to more effective diagnosis and treatment. J Can Chiropr Assoc. 1992;36(3):173.
12. Mandin H, Harasym P, Eagle C, Watanabe M. Developing a “clinical presentation” curriculum at the University of Calgary. Acad Med. 1995;70(3):186–193. doi:10.1097/00001888-199503000-00008
13. Roh H, Lee K, Eo E, et al. Development of guide to clinical performance and basic clinical skills for medical students. Korean J Med Educ. 2015;27(4):309. doi:10.3946/kjme.2015.27.4.309
14. Fan D. My view on holistic integrative medical education. Negative. 2018;9(01):1–8.
15. Gervinder A. translated by Wang J. Checklist Revolution. Vol. 10. Beijing: Beijing United Press; 2017:46–56.
16. Hales BM, Pronovost PJ. The checklist–a tool for error management and performance improvement. J Crit Care. 2006;21(3):231–235. doi:10.1016/j.jcrc.2006.06.002
17. Pronovost P, Needham D, Berenholtz S, et al. An intervention to decrease catheter-related bloodstream infections in the ICU. N Engl J Med. 2006;355(26):2725–2732. doi:10.1056/NEJMoa061115
18. Erdogan A, Dong Y, Chen X, et al. Development and validation of clinical performance assessment in simulated medical emergencies: an observational study. BMC Emerg Med. 2016;16:4. doi:10.1186/s12873-015-0066-x
19. Kogan A, Pennington KM, Vallabhajosyula S, et al. Reliability and validity of the checklist for early recognition and treatment of acute illness and injury as a charting tool in the medical intensive care unit. Indian J Crit Care Med. 2017;21(11):746–750. doi:10.4103/ijccm.IJCCM_209_17
20. Yang Z, Huang T. The effect of timely diagnosis and treatment of acute pulmonary embolism on the curative effect and prognosis of patients. Chin J Crit Care Med. 2015;35(s2).
21. Irvin TT. Abdominal pain: a surgical audit of 1190 emergency admissions. Br J Surg. 2010;76(11):1121–1125. doi:10.1002/bjs.1800761105
22. Zhao Q, Guo H, Shen Z, Li J. On the nature and principle of clinical thinking. Med Philos. 2019;40(12):15–19.
23. Locascio EJ, Mahler SA, Arnold TC. Intestinal angioedema misdiagnosed as recurrent episodes of gastroenteritis. West J Emerg Med. 2010;11(4):391–394.
24. Lee SH, Stanton V, Rothman RE, et al. Misdiagnosis of cerebellar hemorrhage - features of ‘pseudo-gastroenteritis’ clinical presentations to the ED and primary care. Diagnosis (Berl). 2017;4(1):27–33. doi:10.1515/dx-2016-0038
25. Li YK. [Clinical analysis of misdiagnosed urolithiasis]. Zhonghua Wai Ke Za Zhi. 1983;21(12):764–766. Chinese.
26. Singh G, Dhawan R, Potteiger CE, Bedi A, Modesto TA, Gutknecht DR. Acute renal infarction secondary to left ventricular thrombus, masquerading as a renal calculus–a case report and brief review of literature. Angiology. 2001;52(10):717–720. doi:10.1177/000331970105201009
27. Alicioglu B, Kaplan M, Aktoz T, Atakan IH. A case of calcified ureteritis cystica: an indiscernible condition from ureterolithiasis. Prague Med Rep. 2009;110(3):245–249.
28. Niwa N, Kobayashi H, Hatakeyama N, Hasegawa S. An enostosis may be misdiagnosed as a ureteral stone. Intern Med. 2013;52(12):1441. doi:10.2169/internalmedicine.52.0401
29. Wu D. Principles of clinical decision-making and ability cultivation. Chin J Diagnostics Electron. 2015;4:235–239.
30. Huang Y. Operating light 2.0. Chinese Drugstore. 2017;08:108.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


