Back to Journals » Journal of Multidisciplinary Healthcare » Volume 14
Nurse–Physician Communication in Patient Care and Associated Factors in Public Hospitals of Harari Regional State and Dire-Dawa City Administration, Eastern Ethiopia: A Multicenter-Mixed Methods Study
Authors Jemal M, Kure MA , Gobena T , Geda B
Received 20 May 2021
Accepted for publication 16 August 2021
Published 27 August 2021 Volume 2021:14 Pages 2315—2331
DOI https://doi.org/10.2147/JMDH.S320721
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Mehammedamin Jemal,1 Mohammed Abdurke Kure,2 Tesfaye Gobena,3 Biftu Geda2
1Department of Nursing, Hiwot Fana Specialized University Hospital, Haramaya University, Harar, Ethiopia; 2School of Nursing and Midwifery, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia; 3School of Public Health, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
Correspondence: Mohammed Abdurke Kure P. O. Box: 235, Harar, Ethiopia
Tel +251919231736
Fax +251256668081
Email [email protected]
Background: Nurse–physician communication remains a public health challenge in the health care setting of developing countries. Clear and respectful nurse–physician communication is very crucial for the health of the patients. Numerous studies have shown that inter-professional communication gaps are the leading cause of adverse medical events that compromise the quality of patient care in the clinical setting. Although it has negative consequences and wider effects on patient care, nurse–physician communication in patient care is rarely studied in Africa. In eastern Ethiopia, predictors of nurse–physician communication in patient care have not been studied. Therefore, this study was aimed to assess nurse–physician communication in patient care in public hospitals of Harari Regional State and Dire-Dawa city administration, Eastern Ethiopia.
Methods: The multicenter-mixed methods (a quantitative cross-sectional and phenomenological qualitative) were conducted from March 07 to April 07, 2019 in public Hospitals of Eastern Ethiopia. A total of 440 nurses and physicians working in public hospitals in the Harari Regional State and Dire-Dawa administration were enrolled in the study. Participants were approached through a simple random sampling technique. Data were collected using a pretested, self-administered questionnaire and entered into Epi-Data version 3.1, and exported to STATA software (version SE 14) for further analysis. Descriptive statistics were carried out using frequency tables, proportions, and summary measures. Multivariable logistic regression analysis was carried out to identify the true effects of the selected predictor variables on the outcome variable after controlling for possible confounders. Statistical significance was declared at p-value < 0.05. Qualitative data were collected from 10 key informants using a semi-structured questionnaire and analyzed using statistical software, Open Code (version 4.2) by thematic analysis method.
Results: Overall, the magnitude of the level of nurse–physician communication in patient care was found to be 53.2% [95% CI (48.9– 58.0)]. In the final model of multivariable analysis, being in the age group of 31– 40 [(AOR=0.42, 95% CI (0.25– 0.72)], ever married nurse or physician [(AOR=2.28, 95% CI(1.41– 3.69)], being a nurse professional [AOR=2.36, 95% CI (1.23– 4.54)], a salary class of 2250– 3562ETB [(AOR=0.25, 95% CI (0.08– 0.84)], higher score for organizational related factors [(AOR=0.58, 95% CI (0.36– 0.92)], and higher score for work-related attitude behaviors [(AOR=0.62, 95% CI(0.39– 0.984)] were factors independently associated with the poor level of nurse–physician communication in patient care. In the qualitative findings, unattractive working environments and negative attitudes of professionals were found to be barriers to nurse–physician communication in patient care.
Conclusion: In this study, the nurse–physician communication in patient care was relatively low because more than half of the level of nurse–physician communication was found to be poor. Increasing in age, getting a lower monthly salary, higher report for work-related attitude, and organizational related factors were the potential predictors that would decrease the good level of nurse–physician communication in patient care. This result provides cue due attention to improving nurse–physician communication in patient care through various techniques.
Keywords: nurse–physician, communication, patient care, predictors, associated factors, Eastern Ethiopia
Introduction
Nurse–Physician communication (NPC) is a process by which Nurses and Physicians share and discuss, correct, timely based, frequent and problem-solving nature of information about the patient to provide patient care.1 Effective communication in the health care setting is not only about the exchanging of information but also about creating a common understanding among health care professionals to improve safety and quality of patient care.2,3 Globally, NPC continues to be a public health problem in a clinical setting. Studies have shown that NPC gaps are the leading cause of adverse medical events that can compromise the quality of patient care in hospital environments.4–6 Likewise, these communication gaps can cause serious breakdowns in the continuity of patient care and medication errors, which potentially compromise the quality and safety of the patient care.7,8 Many of these adverse medical events are preventable; however, if neglected by professionals, they may result in serious complications and long-term disabilities.6,9,10
Worldwide, nurses and physicians have experienced a complicated working relationship in patient care.11,12 Moreover, researchers have identified that nurses and doctors had been on collegial, collaborative, student-teacher, friendly stranger, and hostile types of relationships in their working environment.4,13,14 In developing regions like sub-Saharan Africa and Asian countries, the situation is far worse because of non-conducive clinical environments.15–18
Furthermore, numerous studies have shown that communication gaps between nurses and physicians are the leading cause of adverse medical events, such as hospital-acquired infections,19 increased length of hospital stay,6 medication administration errors,7,8,20 unnecessary health-related cost,21 and other negative consequences that could compromise the quality of patient care.22,23 On the contrary, effective NPC has been associated with an increased quality of patient outcomes by reducing hospital-acquired infections,19 length of hospitalization,24 patient readmission,6 hospital death rates22,25 and decreasing medication administration errors.9
Although it is known that the status of NPC has a significant association with the quality of patient care, the way that nurses and physicians experience is becoming increasingly difficult due to the different professional and organizational features of the healthcare facilities. For instance, researchers have indicated that nurses and physicians are more autonomous, solution-oriented, problem identifiers, and patient advocators in a setting where hospital administrators are more towards working in collaboration, plan-oriented organizational identification, and organizational advocate.5,26–28
Although a limited number of studies have been reported in Africa, there is little information about NPC in patient care in sub-Saharan Africa,16,29,30 and even all previous studies were limited to the use of quantitative cross-sectional methods. Most importantly, although mixed methods are very helpful to identify and explore the true features of NPC in patient care, there is still a gap in assessing the level of NPC in patient care using mixed-methods study designs in order to triangulate and explore the results of quantitative findings with that of a qualitative one. In Ethiopia, although few studies have been conducted in the last five years, almost all previous researchers were selective to Northern part (Amhara and Tigray Regions),17,31 rarely Southwestern (Oromia Region),28 but neglecting other parts of the country, particularly Afar, Harari, and Somali Regions. In addition, to the extent knowledge of the researchers, the level of NPC in patient care is not well known in eastern Ethiopia, particularly in the study area. Therefore, this study aimed to assess the level of NPC in patient care and its associated factors using mixed-methods study designs among nurses and physicians working in public hospitals of Harari Regional State and Dire-Dawa city administration, Eastern Ethiopia.
Methods and Materials
Study Setting and Design
Multicenter-mixed methods (a quantitative cross-sectional and phenomenological qualitative) were conducted from March 07 to April 07, 2019 in four public hospitals of Eastern Ethiopia. These public hospitals are Hiwot Fana Specialized University Hospital (HFSUH), Jugal Regional Hospital (JRH), Dilchora Referral Hospital (DRH), and Sabian Primary Level Hospital (SPLH). HFSUH and JRH are found in Harari Regional State Eastern Ethiopia. Harari Regional State is one of the 10 Regions of Ethiopia, which is located 526 km away from the capital city Addis Ababa. According to the 2007 national census conducted by the Central Statistics Agency (CSA) of Ethiopia, the total population of the Harari Region was 183,415 (92,316 males and 91, 099 females).32 In the Region, there are 45 health facilities (34 health posts, 8 health centers, 5 hospitals, and 1 Family guidance Association). Of the five hospitals found in the region, only two are providing services as public hospitals. The two public hospitals are HFSUH with a total of 332 nurses and physicians, and JRH with a total of 127 nurses and physicians. Moreover, DRH and SPLH are found in Dire-Dawa administration, Eastern Ethiopia. Dire-Dawa administration is one of the two federal city administrations in Ethiopia, which is located at 515 Km from the capital Addis Ababa, to the East. Dire-Dawa administration has a total population of 341,834 (171,461 males and 170,373 females). It has 56 health facilities (38-health posts, 15-health centers, and 3 hospitals). There were 143 nurses and 42 physicians working in DRH, and 48 nurses and 17 physicians working in the SPLH.32
Population and Sampling Procedure
All nurses and physicians working in public hospitals of Harari Regional State and Dire-Dawa city administration were considered as source population. All randomly selected nurses and physicians (licensed and employed), who had more than six months of working experience, and currently working in the selected public hospitals of Harari Regional State and Dire Dawa city administration were enrolled in the study. However, nurses and physicians who were not on the job (those who were on annual leave, study leave, sick leave, and on training) during the data collection period were excluded from the study.
In this study, the sample size was independently calculated for both objectives. The sample size for the first objective was calculated using Epi-info version 7.0 (USA, 2018) by considering the following assumptions. Taking the proportion of perceived NPC in patient care to the good level of NPC in Ethiopia (p = 49.7%),28 a 95% confidence level (Z=1.96), 5% tolerable margin of error (d=0.05), and by adding 10% contingency for the non-response rate, the final sample size for the first objective was 422. Similarly, the sample size for the second specific objective was determined using the double population proportion formula by considering different factors associated with NPC. It was calculated using statistical software of EPI-Info version 7.0 (USA, 2018). Accordingly, participants’ age was considered because it produced a maximum sample size. This was taken from a previous study report conducted elsewhere.33 Thus, nurses and physicians of the 26 to 29 years of age category were considered as the unexposed group, and those who were in the age category of above 50 years were considered as the exposed group. Based on this information, the following assumptions were made. The proportion of 85% outcome among unexposed (P1= 0.85), 94% outcome among exposed (P2=0.94), a two-sided confidence level of 95%, a tolerable margin of error 5%, power of 80%, a ratio of unexposed to exposure of 1.0, and by taking 10% contingency for non-response rate, the final sample size for the second specific objective was 447. Hence, the sample size for the second objective was larger than that of the first objective; we considered the larger sample size for the second objective (n=447). The sample size for the qualitative data was determined based on the saturation of ideas from the interview of key informants who were selected by the purposive sampling technique. Accordingly, a total of 10 key informants (6 nurses and 4 physicians) were selected and interviewed.
Four public hospitals (HFSUH, JRH, DRH, and SPLH) found in Harari Regional State, and Dire-Dawa city administration were selected purposely. A total of 709 licensed nurses and physicians employed in these public hospitals were identified. Accordingly, the sampling frame was developed, and the total sample size (n=447) was proportionally allocated to each hospital. The study participants were categorized into two strata according to their professions (as nurses and physicians). Then, the study participants were selected using a simple random sampling technique from the sample frame. Finally, the data were collected until the required sample size was obtained (Figure 1).
Data Collection Tools and Procedures
The quantitative data at the level of NPC were collected using English version of structured, pre-tested and self-administered questionnaires adopted from a study conducted in Iran and Jimma, Ethiopia.25,28 Further, it was developed by reviewing peer-reviewed published literature16,34–36 to include factors associated with the level of NPC. The questionnaire was categorized as socio-demographic characteristics of nurses and physicians (age, sex, marital status, professional category, work experience, educational level, current salary, and working unit), level of communication between Nurses and Physicians in patient care with 19 items, and participants were asked to rate each item on a 5-point Likert scale, which ranges from never (1) to always (5), and factors associated with the level of NPC in patient care, which has 15 items, and participants were asked to rate each factor on a 5-point Likert scale, which ranges from strongly disagree (1) to strongly agree (5). The internal consistency and reliability of the tool was established. The Cronbach’s alpha coefficient for the level of NPC tool was 0.93, while the factors tool was 0.821. The overall Cronbach's alpha of the tool was 0.862. A separate in-depth interview for the qualitative part was collected using semi-structured English version questions prepared in accordance with the review of different related literature and personal experiences of the investigators. The in-depth interview guide includes general information about the respondents and other open-ended questions. The data were transcribed via Amharic language and then translated into the English language.
The data were collected over a month for both the quantitative and qualitative methods. The quantitative part of the data was collected by trained twelve nurses (4 Diploma nurses (10+3) and 8 Bachelors of Sciences nurses), and supervised by eight Masters of Science (MSc) nurses. Accordingly, twelve (12) data collectors were assigned to collect the quantitative data for the period of 30 days. The supervisors were supervising the data collectors throughout the study period. More specifically, the qualitative data were collected by a trained BSC nurse with the supervision of the principal investigator using in-depth interview questions regarding the reasons that could affect the level of NPC in patient care among nurses and physicians. The data were collected targeting as supplementary information for the quantitative part of the study in order to explore the issues that could not be addressed by the quantitative method. This qualitative method was conducted among 10 key informants (6 nurses and 4 physicians) until the saturation of ideas was reached. The interviews were started through open-ended questions and later, probing questions were asked as long as more clarifications were needed. The interviewing processes were stopped when data saturations were reached. It was collected during the last 10 days of the planned month of the data collection period. A minimum of 12 minutes and a maximum of 54 minutes were allocated for each interview. The whole interviews were tape-recorded and personal notes were taken. Overall, the interviews were conducted in a private place to avoid any distractions and disturbances.
Study Variables and Measurements
In this study, the dependent variable was the level of Nurse–Physician communication. This level of NPC was dichotomized as “good outcome” and “poor outcome”. Thus, in the STATA software analysis, this outcome variable was recoded into binary outcomes as zero and one. Accordingly, “Good level of NPC was recoded as 0 and Poor level of NPC was recoded as 1. Good level of NPC: means the level of NPC, where respondents have a score of greater than or equal to the mean scores (x =55.19) of items from the components of NPC in the questionnaire. Poor level of NPC: the level of NPC where respondents have a score of less than the mean scores (x =55.19) of items from the components of NPC in the questionnaire.
In this study, the independent variables were developed and customized after reviewing different related literature in order to visualize factors associated with the level of NPC. These predictor variables were categorized into socio-demographic, organizational, and individual-related factors. In addition, all these predictor variables were summarized in the conceptual framework that was submitted as supplementary file one (Supplementary file-1). These predictor variables were categorized as socio-demographic factors (age, sex, marital status, professional category, work experience, educational level), individual factors: Personal behavior-related factors (disruptive behavior, unfavorable attitude towards other professions, unsatisfactory interpersonal communication skill, and conflicting orders), work attitude related factors (non-compliance with advice, negligence to duty, abusive behavior to other professions, poor attitude towards work, and uncooperativeness at work), organizational related factors (working hospital, working unit, employee’s monthly salary, roles and responsibilities, hospital management, communication forum, differential treatment of nurses or physicians, and lack of shared vision between nurses and physicians in the hospital).
Operational Definitions
Nurse: A licensed registered nurse educated at least the diploma level (10+3) or above, and who is providing direct patient care. Physician: a medical doctor who has completed his/her medical school, and providing direct patient care including those residents and specialists. Guest Physicians: are specialist doctors who are not formally employed, but they are giving a service for temporary as a contract. Disruptive behavior: is the bad behavior of professionals characterized by raising the voice, disrespect, condescension, berating colleagues and patients. Differential treatment: is treatment or care given by professionals with the making of distinction between patients. Communication: any verbal and/or non-verbal interaction that occurs between the nurses and physicians to provide care to patients in hospital settings. Nurse–Physician communication (NPC): is a professional interaction, working together, shared decision-making around health issues, formulating collaborative patient care plan in which the actual team’s (Nurses and Physicians) performance is going to be measured. Level of NPC: Measured by 19-items of 5-score Likert scales (1= never, 2= rarely, 3=Sometimes, 4= usually and 5= always) containing statements related to NPC in patient care where the total score ranges from 19 to 95. The responses of each participant were first added up, and their means were computed. Then, levels of NPC were categorized and recoded as good and poor. Good level of NPC: the level of NPC where respondents have a score of greater than or equal to the mean scores (x =55.19) of items from the components of NPC in the questionnaire. Poor level of NPC: the level of NPC where respondents have a score of less than the mean scores (x =55.19) of items from the components of NPC in the questionnaire. Work attitude-related personal individuals’ factors: are factor scores that include noncompliance with advice, negligence of duty, abusive (verbal, physical, and sexual) behavior, poor attitude to one’s work, and uncooperativeness at work.28 High score of work attitude related personal individual factors: for those participants who have scored of greater than or equal to the mean score (x =16.15) of work attitude related personal individual factors. Low Score of work attitude-related personal individual factors: for participants who have scored less than the mean score (x =16.15) of work attitude related personal individual factors. Personal behavior-related individual factors: are factor scores that include disruptive behaviors, unfavorable attitude toward other professionals (Nurse or Physician), and inappropriate inter-professional communication skill.28 High score of personal behavior-related individual factors: for participants who have scored greater than or equal to the mean score (x =12.61) of personal behavior-related factors. Low Score of Personal behavior-related individual factors: for those participants who have scored less than the mean score (x =12.61) of personal behavior-related individual factors. Organizational related factors: are factor scores that include differential treatment of nurses or physicians in the hospital, absence of forum regarding NPC, lack of shared vision between nurses and physicians in the hospital, conflicting orders from physicians, lack of clarity of roles and responsibilities, and disorganized hospital management system.28 High score of organizational related factors: for those participants who have scored greater than or equal to the mean score (x =16.15) of organizational related factors. The low score of organizational factors: for those participants who have scored less than the mean score (x = 16.15) of organizational related factors.
Data Quality Control
Data collectors and supervisors were trained for one day regarding the following: the purpose of the study, study tools, data collection procedures, and data handling techniques. The questionnaire pretest was conducted on 22 participants (5% of the total samples) in Bisidemo General Hospital before the actual data collection. The returned questionnaires were reviewed and checked daily, by supervisors and principal investigators. Moreover, immediate measures were undertaken if any missing values or incomplete questionnaires were found. Double data entry was done by two independent data clerks, and the consistency of data was checked. For the qualitative study, an in-depth interview was transcribed verbatim in Amharic audios, and translated into the English language. Data were analyzed using the thematic analysis approach with the help of Open Code version 4.02 software. Each transcript data was carefully screened and triangulated with the quantitative data.
Data Processing and Analysis
Before the analysis, data were coded, cleaned, and checked for any missing value. Then, they were entered into Epi-Data version 3.1 and exported to STATA software (SE version 14) for further analysis. Descriptive analyses were done using proportions and summary statistics. Results were then presented using frequency tables, figures, and summary measures. The responses for the outcome variable were first added and the overall mean was computed. Then, it was categorized and recoded as good and poor for the respective values of greater than or equal to the mean and less than the mean. The working attitude-related personal behaviors and organizational related factors were computed after recoding the Likert scale of their respective components as 0 and as 1.37 Then, the recoded scores were added up for each participant and an overall mean was computed. Finally, they were categorized and recoded as high and low. Thus, “high category” was considered if the score of greater than or equals to the mean value, and “low category” was considered for a score of less than the mean value. Bi-variable analyses were computed to see the association between each independent variable and the outcome variable using binary logistic regression analysis. All variables with a p-value ≤0.25 in the bivariate analysis were entered into the final model of multivariable analysis to control for any possible confounders and the variables were selected by backward stepwise technique. Multicollinearity test was checked using the variance inflation factor (VIF) and tolerance. The model adequacy was checked using Hosmer-Lemeshow goodness-of-fit tests. The odds ratio with a 95% confidence interval was used to determine the strength of association between dependent and independent variables. Finally, the significance of the association was declared at a p-value of less than 0.05. For the qualitative part, data collection and analysis were preceded concurrently. The data were analyzed using thematic/content analysis methods with the help of Open Code (version 4.2), statistical software for qualitative study. First, the interviews were transcribed, and carefully read several times in order to obtain a general sense of the entire interview. Then, the texts were divided into condensed meaningful units. Later, these condensing units were abstracted and labeled with the codes at the Open Code software. Following this stage, the codes were sorted into categories and then subcategories38 based on their similarities and differences in the software. Finally, themes were formulated as their presentation of the latent content of the text.39
Ethical Considerations and Consent to Participate
The study protocol was approved by the Institutional Health Research Ethics Review Committee (IHRERC) of the College of Health and Medical Sciences, Haramaya University. Letters of cooperation were submitted to authorized bodies of all study sites (HFSUH, JRH, DRH, and SPLH.) The study participants were informed about the following: The purpose of the study, and their rights to withdraw at any time, potential risks and benefits of the study. In addition, informed, voluntary, written, and signed consent was obtained from all respondents before the data collection. Confidentiality of the information was assured since their names were not written in every part of the questionnaires. Permission to tape-record was taken from the selected participants for the interview questions. Data confidentiality was maintained through anonymity by removing any personal identifiers. In addition, informed consent was included the publication of anonymized responses of the study participants. Confidentiality of information and privacy of the participants were respected and their names were not disclosed to anyone at any time. This study was conducted following the Declaration of Helsinki.
Results
Socio-Demographic Characteristics of the Study Participants
A total of 447 study participants were enrolled in the study with a response rate of 98.43%. More than half, 241 (54.8%) of the study participants were males. The participants’ age ranged from 21 to 58 years with a mean age of 31.36 (SD= ± 6.58) years. Nearly two-thirds, 265 (60.2%) of the participants were within the age group of 20–30 years old. Out of the 440 study participants, nearly three-fourths, 325 (73.9%), and more than half, 234 (54.1%) of them were nurses by professional category and married by marital status, respectively. The length of service years of the participants ranged from one year to thirty-two years with a mean of 6.01 (SD= ±6.481) service years. The majority, 294 (67%) of the participants were found within the service category of 1–5 years. Regarding the educational qualification, more than half (266; 60.5%) of the participants were Bachelor of Science (BSc) nurses followed by General Practitioners (GPs) (66; 15%) (Table 1).
 |
Table 1 Socio-Demographic Characteristics of the Nurses and Physicians Working in Public Hospitals of Harari Regional State and Dire-Dawa City Administration, Eastern Ethiopia, 2019 |
General Characteristics of Working Institutions
Regarding employees’ monthly salary, the average salary of the participants were 5943.80 (± 2138.437 SD) ETB with nearly half, 192 (44%) of respondents’ salary was in the salary classification range of 3563–5328 ETB followed by 143 (32.8%) within 5329–7411 ETB. Nearly three-fourths, 320 (72.7%) of the respondents were working in the referral hospitals. Concerning the hospital working unit, nearly half, 210 (47.7%) of the study participants were working in Inpatient Departments (IPD) followed by cold Outpatient Departments (COPD) (92; 21.1%) (Table 2).
 |
Table 2 General Characteristics of Working Institutions for Nurses and Physicians Working in Public Hospitals of Harari Regional State and Dire-Dawa Administration, Eastern Ethiopia, 2019 |
Level of NPC in Patient Care
In this study, the mean (± SD) score for the level of NPC in patient care was 55.19 (SD= ±15.930). Moreover, the level of NPC in patient care at public Hospitals of Harari Regional State and Dire-Dawa city administration was found to be 53.2% [95% CI (48.6–58.0)] (Figure 2).
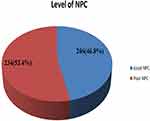 |
Figure 2 Magnitude of level of NPC in patient care among nurses and physicians working in public hospitals of Harari Regional State and Dire-Dawa city Administration, Eastern Ethiopia, 2019. |
Organizational Related Factors of NPC in Patient Care
Regarding the items for the measurement of the level of NPC in patient care, participants who usually and always asked for clarification were about 27.5% of the time (15.5% +12.0%). More specifically, the participants reported that 55% (25.9% + 18.6% + 10.5%) of them were adhered to the discussion mechanism to maintain the patient safety at least sometimes. Likewise, the participants’ report indicated that they usually or always do not feel angry [44.1% (27.5% + 16.6%)], and frustrated [39.5 (22.5% + 17.0%)]. Similarly, the participants reported that they usually or always felt understood [33.2% (22.3% + 10.9%)], respected [35.7% (20.2% + 15.5%)], pleased [32.5% (18.4% + 14.1%)], and satisfied [34.8% (20.9% + 13.9%)] after nurse and physician interaction. The report for patient discharge confirmation by signature of nurses and physicians was at most 74.5% (15.7% + 15.2% + 43.6%) times (Table 3).
 |
Table 3 Level of Measuring Items for Communication Between Nurses and Physicians in Patient Care in Public Hospitals of Harari Regional State and Dire Dawa City Administration, Eastern Ethiopia, 2019 |
Organizational Related Factors Affecting the Level of NPC in-Patient Care
Regarding the predicting factors that could affect the effectiveness of level of NPC in patient care, the most commonly reported reasons in the quantitative study were organizational-related factors like disorganized Hospital management system (260; 59.1%), absence of communication forum between nurses and physicians (253; 57.5%), and lack of clarity in roles and responsibilities of professionals (261; 59.3%). In addition, personal behavior-related factors like unfavorable attitude towards other professions (216; 49.1%), unsatisfactory inter-professional communication skills (223; 50.7%), disruptive behavior of nurses (208; 47.3%), and disruptive behavior of physicians (188; 42.7%) were reported as the reasons that affect the effectiveness of NPC in-patient care. Likewise, from the perspective of work attitude related individual factors of the study participant; negligence of duty (260; 59.1%), uncooperativeness (245; 55.7%), and poor attitude towards one’s work (236; 3.6%) were reported to be predictors that would affect NPC, which accounts for and respectively (Table 4).
Factors Associated with the Level of NPC in Patient Care
In the final model of multivariable analysis, participants’ age, marital status, professional categories, participants’ monthly salary, and high score for organizational-related and work attitude-related factors were independently associated with a poor level of NPC. Accordingly, nurses and physicians who were in the age group of 31–40 years were 58% times less likely to have a good level of NPC in patient care than those in the age group of 20–30 years [AOR=0.42, 95% CI(0.25, 0.72)]. Similarly, those participants whose age ≥40 years old were 69% times less likely to have a good level of NPC in patient care as compared to the participants in the age group of 20–30 years [AOR= 0.31, 95% CI(0.14, 0.68)]. Likewise, ever-married nurses and physicians were 2.28 times more likely to have a good level of NPC in patient care [AOR=2.28, 95% CI(1.41, 3.69)]. Regarding the professional categories of the participants, nurses were greater than two times more likely to have a good level of NPC in patient care as compared to the physicians [AOR= 2.36, 95% CI (1.23, 4.54)]. According to employees’ salary classification, those study participants who were paid 3563–5328 ETB were 75% times less likely to have a good level of NPC in patient care as compared to those in the salary category of greater than or equal to 7412 ETB [AOR= 0.25, 95% CI (0.08, 0.84)]. In addition, those study participants who had high scores for organizational related factors were 42% times less likely to have a good level of NPC in patient care as compared to those who reported low scores [AOR= 0.58, 95% CI (0.36, 0.92]. Similarly, the likelihood of having a good level of NPC inpatient care was 38% times lower among those participants who had high scores for work attitude-related individual factors compared to their counterparts (those who reported low score) [AOR= 0.62, 95% CI (0.39, 0.98)] (Table 5).
Results of Qualitative Method
Reasons/Predictors for the Level of NPC from the Qualitative Part of the Study
In this study, a qualitative part was conducted with in-depth interview questions from a total of 10 participants (6 Nurses and 4 Physicians). Their average ages were 30.2 years and the majority, 7 (70%) of them were males. All the participants were key informants who had the position of department head in their respective assigned units. The findings from this qualitative part of the study were identified as a group of four themes and eleven categories that determine the level of NPC in patient care (Supplementary file-2).
Working Environment/ Organizational Related Factors
Non-Professional Duties
A qualitative study report finding revealed that professionals’ trend of doing and being ordered for non-professional activities is one of the reasons mentioned for ineffective NPC in patient care.
A 29-year-old Emergency OPD head, BSc nurse said and shared his experience as follows:
… But there are some trends in which some physicians are ordering nurses to do things out of their responsibilities because they may not know the job description of Nurses. In this regard, we nurses feel discomfort and may not have approached that physician. As a result, there could be a negative influence on effective NPC in patient care. I had one experience; once upon a time the floor at emergency OPD was contaminated with blood, then the physician said ‘why don’t you clean it?’ then, I responded saying I know my job better than you and you could not enforce me to do what is not my responsibility. (Nurse-4)
Shortage of Staff
A qualitative study report revealed that the work overload and tiredness of the professionals because of a shortage of professional staff is one of the reasons mentioned for ineffective NPC in patient care.
A 30-year-old GP said that
… There is also a lack in the number of nurses and physicians at some working units, which results in work overload on the assigned staff. At this time; since the staff would feel tired, they did not give time for inter-professional communication. The opposite is true for effective inter-professional communication between nurses and physicians on the quality of patient care. (Physician-4)
Supplies of Medical Equipment
Another qualitative study finding showed that the level of accessibility and availability of necessary medical equipment and materials is associated with the level of NPC in patient care.
A 32-year-old pediatrics ward general practitioner (GP) said,
… Whenever physicians ask nurses for any medical equipment or materials, the nurse should give accordingly since most of the time, medical equipment and materials are under the control of nurses. However, if there is a lack of supply of materials, the nurses could not access it, the physicians sometimes became angry with the duty nurses. This could end up with decrement of effective NPC in patient care. (Physician-1)
Hospital Recognition and Management System
A qualitative study finding was also indicated that professionals’ working hospital level of modernization and giving more recognition for those hard workers were another reason explained for the effectiveness or ineffectiveness of NPC in the patient.
A 28 years old pediatrics ward head, general practitioner (GP) said that
… The hospital should give respect and recognition for the professionals as a staff and should take some corrections regarding incentives, work overload, and the like issues accordingly. When one of the staff feels discomfort and tired because of work overload and lack in getting recognition from the hospital, he/she would not take their responsibilities appropriately and this would in turn in affecting the effectiveness of NPC in patient care. (Physician-2)
Again, 31 years old medical ward head nurse said,
… The hospital should be led by professionals which means; those who ever had knowledge and skill regarding health-related issues should be the ones to be in the managerial position. In addition, the hospital managers should be near to hear both the professionals‟ and patients‟ ideas and be refrained from being as a mother for some professionals and as a stepmother for the other professionals. If all these are kept on, the NPC could be effective. (Nurse-1)
Work Performance and Attitude-Related Factors Roles and Responsibilities
Professionals’ level of performing one’s responsibility affects inter-professional communication between nurses and physicians during their patient care was one of the findings from the qualitative part of this study.
28-year-old pediatrics, ward head nurse said,
… Some of the professionals both from Nurses and Physicians had a gap in performing their responsibilities appropriately and even they had also a trend of neglecting one’s duties. At this time, inter-professional conflict maybe happen. Such alike experience could lead to ineffective NPC in patient care and this is primarily affecting the patients’ safety. (Nurse-5)
Another 31-year-old medical ward head nurse said that
… It is highly important to achieve effective NPC where each of us including physicians, is standby to give a priority for patient care since their existence at the working area is because of the patient not for their issues. So, each of the professionals should perform their responsibilities appropriately. (Nurse-1)
Theoretical and Practical Variation at Work
A qualitative study result revealed that some professionals’ experience of different scientific backgrounds and their practice was one of the reasons for the status of NPC inpatient care.
A 30-year-old GP said that
… One of the reasons that may create an ineffective environment for NPC is when some professionals did differently from what they had been learned. For example; if we take some Nurses, when they did an IV line securing for patients, they usually did not follow a correct procedure. As a result, disagreement between the two professionals may happen; this, in turn, could affect the level of NPC. (Physician-4)
Professionals’ Value for Communication
Multi-Disciplinary Round Communication
Findings from the qualitative study of key informants revealed that multi-disciplinary round is one of the most common reasons for the level of improvement of NPC in patient care.
A 34-year-old medical ward head MSc nurse said,
… It is highly important for providing quality of patient care as well as increasing the communication level between different professional groups. It is a type of round, which involves nurses, physicians, and clinical Pharmacists discussing the safety and quality of care. This, in turn, improves the effectiveness of NPC in patient care. (Nurse-3)
The Unfamiliarity of Professionals
Findings from key informants of the qualitative study explained that the unfamiliarity and infrequent contact between Nurses and Physicians could be the reason for ineffective NPC during patient care.
A 28 years old Central ICU head nurse said
… Presence of professionals’ rotation from one unit to the other units, especially nurses and guest specialists and their infrequent contact will lead to coming of the professionals with their early experience of inter-professional communication, which may be a strictly new experience for that unit/institution. So, this could affect the level of NPC in patient care in accordance to professionals’ interaction. (Nurse-2)
Absence of Giving Concern for Communication
Professionals’ value for inter-professional communication was also another reason mentioned by the participants, which affects the levels of NPC in patient care.
A 30-year-old surgical ward head nurse said that
… I think if there is no inter-professional communication, there is no appropriate care. But sometimes professionals did not give value to communication and that is why most nurses do not attend patient rounds with physicians, as well as physicians, do not want to talk with nurses even when they attend the bedside round rather they mostly communicate with medical interns. So, the effectiveness of NPC in patient care would be determined by the professionals’ level of concern for it. (Nurse-6)
Professionals’ Behavior Attributes
Disruptive Behaviors of Professionals
The qualitative study finding also revealed that professionals’ attitudes and behaviors were important reasons that could decide the effectiveness of NPC in patient care.
A 28-year-old Central ICU head, BSc nurse said that
… Not reflecting personal character at a working area by the nurses or physicians. Even if it is reflected the opposite professional should tolerate that one and interpret the situation positively. Finally, it would lead to inter-professional collaboration and effective NPC in patient care. Unless and otherwise, the inter-professional communication level could be disturbed. (Nurse-2)
Again, 32-year-old inpatient medical director GP said that
… Sometimes some doctors order a medication orally even by calling without writing it on the order sheet and when Nurses ask clarification they become agitated. Conversely, some doctors write the medication on the order sheet and leave the room without informing the duty nurses. Thus, when the nurses ask for clarification for that drug they become agitated and sometimes said, ‘Just I have already written it on the order sheet! So, you have to administer as it is ordered.’ All these situations might lead to Nurses’ frustration to talk with Physicians and decrement in the effectiveness of NPC. (Physician-3)
Power of Authority
One of the reasons mentioned by the key informants of the qualitative study that affects NPC was inferiority-superiority complex feelings of professionals.
A 28-year-old pediatrics ward GP said,
… I think one thing for ineffective NPC in patient care is the presence of inter-professional conflict between Nurses and Physicians. This happened when some Physicians feel superiority complex syndrome and in contrast, some Nurses feel inferiority complex syndrome. So, in order to have effective NPC during patient care, both professionals should avoid such feelings rather they should discuss together and do targeting the benefit of patients. (Physician-2)
Discussion
In this study, the overall result showed that the level of NPC in patient care was found to be 53.2%. Increasing in age, getting a lower monthly salary, higher score for work-related attitude, and organizational related factors were the potential predictors of NPC in patient care. The finding of this study is in line with the previous studies conducted on patterns of NPC in patient care in the USA, among nurse–doctor relationships in Rwanda, and the perceived level of practice in NPC at Jimma, Ethiopia.16,28 Therefore, NPC in patient care is attention-seeking a gap in hospitals to achieve the quality of patient care. But it is slightly lower than the result from a study done in Iran.25 This difference may be due to variations in study settings and the nature of the study population. In addition, it may be due to the smaller sample size and the involvement of only Nurses in Iran than this study.
In this study, the increased age of participants was found to be an independent predictor of the level of NPC in patient care. Thus, as the age of nurses and physicians increases, the level of NPC decreased. This finding is consistent with previous studies conducted in Northeastern Japan among doctors,33 and in Turkey among surgeons and anesthetists.37 The current study report is also comparable with a previous research report from Jimma, Ethiopia, which was conducted among nurses and physicians, where older ages were less likely for their good level of communication.28 In contrast, it is not consistent with the study conducted in Iran,25 which showed no difference in perceived level of NPC among different age groups. This difference may be due to the fact that most of the participants of the current study were in younger age groups. It may also be due to differences in study settings, sample size, and professional category of participants.
According to this study, those participants who paid higher monthly salaries had a significant effect on the level of NPC in patient care, whereas those who got the lowest payment were less likely to have good NPC. It was also supported by a study conducted in Jimma, Ethiopia, which found that the increment of monthly salary was the potentially associated factor for the level of NPC.28 This could indicate that relatively better payment for professionals may facilitate a good level of NPC. It may be because of the moral satisfaction of professionals leading their openness to communicate with each other.40 The quantitative part of this study was also identified that a participant’s high score for organizational-related and work attitude-related factors were significantly lowered the level of NPC in patient care. These findings were supported and more explained by the qualitative part of this study as well. These findings are also in line with the previous studies conducted in USA,2 Ethiopia,28 and Turkey,37 which suggested organizational and work attitude-related factors influence the level of NPC in patient care. The possible explanation might be because participants who report as these factors highly affect the level of NPC during patient care could have a lower level of NPC.
The communication level between nurses and physicians in patient care was found to be higher among nurses than physicians. This finding is in line with previous studies conducted in Egypt and USA.41,42 In contrast, it is inconsistent with studies conducted at the University of West Indies and Jimma, Ethiopia28,43 where the communication level was higher among physicians than nurses. This discrepancy may be due to the fact that physicians have better autonomy in their practice in West Indies and Jimma, Ethiopia than the current finding. Again it may be partly due to differences in the professional status, professional roles, and professionals’ perspectives in viewing patients (that is: medical versus psychosocial perspective) of different settings.4,44 In general, the discrepancy in the level of inter-professional communication among nurses and physicians may be the traditional trends that Physicians feel as their role is superior to that of nurses role and this may lead to giving less concern for communication by physicians with that of nurses, and vice versa.
This study also found that a higher level of NPC occurred among ever married than single/unmarried participants. This may be because of the unlimited needs of younger age groups like monetary, love, and enjoying different smart life events, which may conversely affect inter-professional communication during patient care. In addition, younger age group professionals may become busy with their satisfaction and fulfilling of their daily needs.
The qualitative part of this study identified that disruptive behavior of professionals either nurses or physicians or both negligence of one’s duties and responsibilities, level of hospital recognition and management systems, as well as the power of authority where most physicians feel as superiority over nurses were reasons that could determine the level of NPC in patient care. These findings are also supported by previous qualitative studies conducted elsewhere, which indicated disruptive behaviors of professionals, negligence of duties, inequality of nurses and physicians under hospital management were reported as barriers for NPC.16,45 Similarly, the power of authority and personality traits of professionals with divergent attitudes to each other were found to be barriers to good NPC in patient care. This is also supported by studies conducted elsewhere.34,36,45 All these findings may be due to the difference in the professional and educational status of physicians and nurses as well as the difference in perspectives of physicians and nurses in terms of viewing patients. This could lead to a feeling of some nurses being insecure in front of physicians for their opinions and clarifications for what they are going to implement and vice versa.
Performance of non-professional duties, shortage of staff, and professionals’ discrepancy between what they learned and what is being practiced at the Hospital level in the study done in Malaysia were found to be reasons that could affect the level of NPC in patient care.36 Similarly, this study also identified the performance of non-professional duties.
Professionals’ perspectives, theoretical and practical variations of professionals at work were found to be reasons that could affect the level of NPC. If there are professionals’ work overload and inappropriate practice, inter-professional communication among nurses and physicians will be disregarded and this may compromise the quality of patient care.
Physicians’ attitudes towards nurses as well as nurses’ attitudes towards physicians were found to be the independent predictor for the level of NPC in patient care as shown in a study conducted in Belgium.34 The result is consistent with the current study finding, where negative attitudes of professionals towards others were identified as a barrier for the level of NPC in patient care. This may be due to its influence on the attitudes towards one another, and consequently, it affects the forms of communication between the two professionals.
According to studies done by Leary et al in the Northwestern Memorial Hospital and by Chicago and Burns inter-disciplinary patient rounds could determine the level of communication between nurses and physicians.46,47 It is in line with this study where the presence of a multi-disciplinary patient round involving nurses, physicians, and clinical pharmacists is an identified factor that determines the level of NPC during patient care. This may be due to the chance created for the free flow of ideas or opinions about the patient, which in turn, ends up with the effective level of NPC.
The level of availability and accessibility of medical equipment and materials in the working unit is one of the newly identified reasons from the qualitative part of this study that could determine the level of NPC during patient care. Since most of the time, the medical equipment and materials are under the hands of nurses and Physicians should take them as needed. But if there is a limitation in the access or functionality, physicians might become agitated over nurses. This might finally lead to communication disregard between nurses and physicians and withholding of opinions by nurses or physicians during patient care.
Other newly identified reasons that could be independent predictors for the level of NPC in patient care are unfamiliarity of professionals with each other and their low concern for inter-professional communication. Because of infrequent contact between nurses and physicians, they might not get a chance to exchange ideas or opinions about patient care, which consequently affects the communication between them.
Strengths and Limitations
Strengths
The study design was a mixed (quantitative study supplemented with explanatory qualitative part) study design. So, this was important to explore reasons for the level of NPC in patient care which was not addressed by the quantitative part of the study. It also involves both Nurses and Physicians, thus it avoids limiting the conclusions on either of the two professionals.
Limitations
The findings from this study might have been subjected to respondents’ discussion with their colleagues that might result in social desirability bias. It might also be subjected to respondents’ recall bias. Since the study is of the cross-sectional type, it is not possible to explain the causal influence of the examined variables on the level of NPC in patient care.
Conclusions
The overall level of NPC was found to be poor. Increasing in age, being single, being in the professional category of physicians, and getting a lower monthly salary as well as higher score reports for work-related attitudes and organizational related factors were the potential predictors that would decrease the good level of NPC in patient care. The qualitative findings of this study identified four group themes (unattractive working environment/institution, poor work performance and negative attitudes of professionals, unsatisfactory value for communication by professionals, and bad professionals’ personal behavior) as barriers for NPC that result in poor outcomes of NPC in patient care. Therefore, much work is needed to improve the level of NPC in patient care.
Abbreviations
COPD, Cold Out Patient Department; CSA, Central Statistical Agency; DHB, Dire Dawa Health Bureau; DRH, Dilchora Referral Hospital; ETB, Ethiopian birr; EOPD, emergency outpatient department; GPs, general practitioners; HFSUH, Hiwot Fana Specialized University Hospital; HRHB, Harar Regional Health Bureau; IHRERC, Institutional Health Research Ethics Review Committee; IPC, Inter-Professional Collaboration; JH, Jugol Hospital; NPC, Nurse–Physician Communication, OPD, outpatient department, SPLH, Sabian Primary Level Hospital.
Data Sharing Statement
The datasets used for the analysis are available from the first author on reasonable request.
Ethical Approval
Ethical clearance was obtained from the Institutional Health Research Ethics Review Committee (IHRERC) of the College of Health and Medical Sciences, Haramaya University. A support letter was written to all public health facilities where the study was conducted. Informed, voluntary, written and signed consent was obtained from each study participant. Confidentiality of information and privacy of participants were respected and their names were not disclosed to anyone at any time. This study was conducted following the Declaration of Helsinki.
Acknowledgments
The authors thank Haramaya University, College of Health and Medical Sciences, Institutional Health Research Ethics Review Committee coordinating office, School of Nursing and Midwifery, Harari Regional State and Dire-Dawa administration Health Bureaus as well as all the respective hospitals for their unreserved contribution to this research paper, and without them, this work would not be realized.
Author Contributions
All authors have made a significant contribution to the conception, study design, data collection, data analysis, and interpretation of the findings. The authors also took part in writing the manuscript, reviewed the draft, and finally agreed on the journal to which the article has to be published. All authors read and approved the final draft of the manuscript and agreed to be accountable for all contents of the manuscript under any circumstances.
Funding
This study was funded by Haramaya University. The funding organizations had no role in the study design, data collection, data analysis, and writing up of the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Joint Commission. Sentinel event data root causes by event type 2004-2014; 2015. Available from: http://wwwjointcommissionorg/Sentinel_Event_Statistics/defaultaspx(abgerufenam1252015.
2. Tan TC, Zhou H, Kelly M. Nurse–physician communication–an integrated review. J Clin Nurs. 2017;26(23–24):3974–3989. doi:10.1111/jocn.13832
3. House S, Havens D. Nurses’ and physicians’ perceptions of nurse-physician collaboration: a systematic review. J Nurs Admin. 2017;47(3):165–171. doi:10.1097/NNA.0000000000000460
4. Crawford CL, Omery A, Seago JA. The challenges of nurse-physician communication: a review of the evidence. J Nurs Admin. 2012;42(12):548–550. doi:10.1097/NNA.0b013e318274b4c0
5. Yusuf FR, Kumar A, Goodson-Celerin W, et al. Impact of coaching on the nurse-physician dynamic. AACN Adv Crit Care. 2018;29(3):259–267. doi:10.4037/aacnacc2018624
6. Pesko MF, Gerber LM, Peng TR, Press MJ. Home health care: nurse-physician communication, patient severity, and hospital readmission. Health Serv Res. 2018;53(2):1008–1024. doi:10.1111/1475-6773.12667
7. Hammoudi BM, Ismaile S, Abu Yahya O. Factors associated with medication administration errors and why nurses fail to report them. Scand J Caring Sci. 2018;32(3):1038–1046. doi:10.1111/scs.12546
8. Hassan I. Avoiding medication errors through effective communication in the healthcare environment. Movement Health Exer. 2018;7(1):113–126.
9. Wang H-F, Jin J-F, Feng X-Q, et al. Quality improvements in decreasing medication administration errors made by nursing staff in an academic medical center hospital: a trend analysis during the journey to Joint Commission International accreditation and in the post-accreditation era. Ther Clin Risk Manag. 2015;11:393.
10. Müller M, Jürgens J, Redaèlli M, Klingberg K, Hautz WE, Stock S. Impact of the communication and patient hand-off tool SBAR on patient safety: a systematic review. BMJ Open. 2018;8(8):e022202. doi:10.1136/bmjopen-2018-022202
11. Streeton A, Bisbey C, O’Neill C, et al. Improving nurse-physician teamwork: a multidisciplinary collaboration. Medsurg Nurs. 2016;25(1):31.
12. Matzke B, Houston S, Fischer U, Bradshaw MJ. Using a team‐centered approach to evaluate the effectiveness of nurse-physician communications. J Obstetric Gynecol Neonatal Nursi. 2014;43(6):684–694. doi:10.1111/1552-6909.12486
13. Schmalenberg C, Kramer M. Nurse-physician relationships in hospitals: 20 000 nurses tell their story. Crit Care Nurse. 2009;29(1):74–83. doi:10.4037/ccn2009436
14. Brooks AMT. Nurse Physician Disruptive Behavior: Building a Culture of Safety and Quality. 2016.
15. Weldetsadik AY, Gishu T, Tekleab AM, Asfaw YM, Legesse TG, Demas T. Quality of nursing care and nurses’ working environment in Ethiopia: nurses’ and physicians’ perception. Int J Afr Nurs Sci. 2019;10:131–135. doi:10.1016/j.ijans.2019.03.002
16. Mukeshimana M, Asingizwe D. Nurse-doctor relationship in Rwanda: a questionnaire survey. J Nurs Health Sci. 2016;5(4):68–74.
17. Amsalu E, Boru B, Getahun F, Tulu B. Attitudes of nurses and physicians towards nurse-physician collaboration in northwest Ethiopia: a hospital-based cross-sectional study. BMC Nurs. 2014;13(1):1–6. doi:10.1186/s12912-014-0037-7
18. Conover KG, Behrens ME, Usenick EN, Abraham SP, Gillum DR. Factors that contribute to nursing and medical students’ perceptions of the nurse-physician relationship. Int J Studies Nurs. 2019;4(3):1. doi:10.20849/ijsn.v4i3.597
19. Boev C, Xia Y. Nurse-physician collaboration and hospital-acquired infections in critical care. Crit Care Nurse. 2015;35(2):66–72. doi:10.4037/ccn2015809
20. Shaha A. Does CPOE Support Nurse-Physician Communication in the Medication Order Process? A Nursing Perspective. IOS Press; 2014: 149.
21. Renz SM, Carrington JM. Nurse–physician communication in long-term care: a literature review. J Gerontol Nurs. 2016;42(9):30–37. doi:10.3928/00989134-20160615-04
22. De Meester K, Verspuy M, Monsieurs KG, Van Bogaert P. SBAR improves nurse-physician communication and reduces unexpected death: a pre and post-intervention study. Resuscitation. 2013;84(9):1192–1196. doi:10.1016/j.resuscitation.2013.03.016
23. Riegel N. Effects of nurse-physician collaborative rounding. Medsurg Nurs. 2018;27:3.
24. Matthys E, Remmen R, Van Bogaert P. An overview of systematic reviews on the collaboration between physicians and nurses and the impact on patient outcomes: what can we learn in primary care? BMC Fam Pract. 2017;18(1):1–22. doi:10.1186/s12875-017-0698-x
25. Aghamolaei T, Tavafian SS, Hasani L, Moeini B. Nurses’ perception of nurse-physician communication: a questionnaire-based study in Iran. Int J Hosp Res. 2012;1(2):77–84.
26. Ghahramanian A, Rezaei T, Abdullahzadeh F, Sheikhalipour Z, Dianat I. Quality of healthcare services and its relationship with patient safety culture and nurse-physician professional communication. Health Promotion Perspectives. 2017;7(3):168. doi:10.15171/hpp.2017.30
27. Bowles D, McIntosh G, Hemrajani R, et al. Nurse–physician collaboration in an academic medical center: the influence of organizational and individual factors. J Interprof Care. 2016;30(5):655–660. doi:10.1080/13561820.2016.1201464
28. Hailu FB, Kassahun CW, Kerie MW. Perceived nurse-physician communication in patient care and associated factors in public hospitals of Jimma Zone, South West Ethiopia: a cross-sectional study. PLoS One. 2016;11(9):e0162264. doi:10.1371/journal.pone.0162264
29. Falana TD, Afolabi OT, Adebayo AM, Ilesanmi OS. Collaboration between doctors and nurses in a tertiary health facility in southwest Nigeria: implication for effective healthcare delivery. Int J Caring Sci. 2016;9:1.
30. Mohamed ZM, Aboserea MM, El-sayed KA, Mohamed WM. Nurse-physician collaboration and its relation with patient safety. Zagazig Nurs J. 2018;14(2):122–133.
31. Eukubay T, Abate A. Interprofessional collaboration and associated factors among nurses and physicians working at public hospitals in Mekelle city Tigray region, north Ethiopia, 2017. Nurse Care Open Acces J. 2019;6(6):185–192.
32. Population Census Commission. Summary and Statistical Report of the 2007 Population and Housing Census: Population Size by Age and Sex. Addis Ababa: UNFPA; 2008.
33. Minamizono S, Hasegawa H, Hasunuma N, Kaneko Y, Motohashi Y, Inoue Y. Physician’s perceptions of interprofessional collaboration in Clinical Training Hospitals in Northeastern Japan. J Clin Med Res. 2013;5(5):350.
34. Bryon E, Gastmans C, de Casterlé BD. Nurse–physician communication concerning artificial nutrition or hydration (ANH) in patients with dementia: a qualitative study. J Clin Nurs. 2012;21(19pt20):2975–2984. doi:10.1111/j.1365-2702.2011.04029.x
35. Ogbimi RI, Adebamowo CA. Questionnaire survey of working relationships between nurses and doctors in University Teaching Hospitals in Southern Nigeria. BMC Nurs. 2006;5(1):2. doi:10.1186/1472-6955-5-2
36. Amudha P, Hamidah H, Annamma K, Ananth N. Effective communication between nurses and doctors: barriers as perceived by nurses. J Nurs Care. 2018;7(03):1–6.
37. Önler E, Yildiz T, Bahar S. Evaluation of the communication skills of operating room staff. J Interprofessional Educ Pract. 2018;10:44–46. doi:10.1016/j.xjep.2017.11.004
38. Sidibe I. Perceptions of Effective and Ineffective Nurse–Physician Communication in Hospitals: What are the Existing Themes at UC Davis Medical Center? Davis: University of California; 2013.
39. Vaismoradi M, Turunen H, Bondas T. Content analysis and thematic analysis: implications for conducting a qualitative descriptive study. Nurs Health Sci. 2013;15(3):398–405. doi:10.1111/nhs.12048
40. Saif NI, Saleh AS. Psychological empowerment and job satisfaction in Jordanian hospitals. Int J Humanities Soc Sci. 2013;3(16):250–257.
41. Elithy A, Harmina MK, Elbialy GG. Nurses and physicians perceptions of their inter-professional relationships at Alexandria Main University Hospital. J Am Sci. 2011;7(12):750–757.
42. Nair DM, Fitzpatrick JJ, McNulty R, Click ER, Glembocki MM. Frequency of nurse-physician collaborative behaviors in an acute care hospital. J Interprof Care. 2012;26(2):115–120. doi:10.3109/13561820.2011.637647
43. Chang L, Harding H, Tennant I, et al. Interdisciplinary communication in the intensive care unit at the University Hospital of the West Indies. West Ind Med J. 2010;59(6):656.
44. Quan SD, Morra D, Lau FY, et al. Perceptions of urgency: defining the gap between what physicians and nurses perceive to be an urgent issue. Int J Med Inform. 2013;82(5):378–386. doi:10.1016/j.ijmedinf.2012.11.010
45. Nakhaee S, Nasiri A. Inter-professional relationships issues among Iranian nurses and physicians: a qualitative study. Iran J Nurs Midwifery Res. 2017;22(1):8. doi:10.4103/1735-9066.202076
46. O’Leary KJ, Thompson JA, Landler MP, et al. Patterns of nurse-physician communication and agreement on the plan of care. BMJ Qual Saf. 2010;19(3):195–199. doi:10.1136/qshc.2008.030221
47. Burns K. Nurse-physician rounds: a collaborative approach to improving communication, efficiencies, and perception of care. Medsurg Nurs. 2011;20(4):194.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



