Back to Journals » Journal of Pain Research » Volume 14
Nurse-Administered Analgesic Treatment in Italian Emergency Medical Services: A Nationwide Survey
Authors Imbriaco G , Rondelli R, Maroni F, Mazzolani S, Sasso S, Sebastiani S , Samolsky Dekel BG
Received 27 January 2021
Accepted for publication 11 May 2021
Published 16 June 2021 Volume 2021:14 Pages 1827—1835
DOI https://doi.org/10.2147/JPR.S303998
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Salimah H Meghani
Guglielmo Imbriaco,1,2 Riccardo Rondelli,3 Federica Maroni,2,4 Selene Mazzolani,2,5 Silvia Sasso,2,6 Stefano Sebastiani,2,7 Boaz Gedaliahu Samolsky Dekel2,7,8
1Centrale Operativa 118 Emilia Est, Maggiore Hospital Carlo Alberto Pizzardi, Bologna, Italy; 2Critical Care Nursing Master Course, University of Bologna, Bologna, Italy; 3Intensive Care Unit, Maggiore Hospital Carlo Alberto Pizzardi, Bologna, Italy; 4Emergency Department, Bufalini Hospital, Cesena, Italy; 5Intensive Care Unit, Infermi Hospital, Faenza, Italy; 6Surgical Unit, State Hospital, San Marino, San Marino Republic; 7IRCCS Azienda Ospedaliero-Universitaria di Bologna, Bologna, Italy; 8Department of Medical and Surgical Sciences (DIMEC), University of Bologna, Bologna, Italy
Correspondence: Guglielmo Imbriaco
Centrale Operativa 118 Emilia Est, Ospedale Maggiore Carlo Alberto Pizzardi, Bologna, Largo Nigrisoli 2, Bologna, 40133, Italy
Tel +39 051 6478868
Fax +39 051 6478866
Email [email protected]
Background: Acute pain is common among patients requiring assistance from prehospital emergency medical services (EMS). Nonetheless, the undertreatment of pain in this context remains a frequent phenomenon. Timely and effective analgesia is a crucial feature in emergency medicine. To ensure analgesia provision, prehospital paramedics and nurses can administer analgesics via standard operating protocols or under a physician’s remote supervision. Information about such protocols in Italian EMS is lacking.
Objective: Evaluation of the availability of nurse’s standard analgesia protocols in Italy’s prehospital EMS settings.
Methods: A cross-sectional online survey involved all 74 Italian emergency medical dispatch centres (EMDCs). Aside from descriptive statistics, we used χ2-analysis and Spearman-rank correlation to look for associations between geographical areas’ dependence upon independent variable categories and their correlations.
Results: Of all the 74 Italian EMDCs, 70 (94.6%) completed the survey, covering 100 provinces out of a total of 107 (93.5%). Operating nurses’ prehospital analgesia protocols are available in 46 provinces (46.0%). The availability of prehospital analgesia protocols is more extended in northern Italy EMDCs (n=30, 66.7%) than in central Italy (n=9, 42.8%) and southern Italy and islands (n=7, 20.6%). Morphine (76.1% for medical patients and 95.7% for trauma) and paracetamol (89.1% for both) are the most common drugs included in the prehospital analgesia protocols.
Conclusion: Despite international consensus on the necessity, efficacy, and safety of nurses’ prehospital analgesia provision, nurse-administered analgesia protocols are available in less than half of Italian provinces, with substantial differences between northern, central, and southern areas. These results indirectly indicate potential undertreatment of prehospital pain in Italy and yield practice improvements.
Keywords: nurses, pain management, analgesia, pain relief, prehospital emergency care, emergency medical services
Introduction
A timely and effective analgesia treatment represents a key feature in emergency medicine.1,2 Pain assessment and treatment should be routine tasks for EMS providers caring for medical or trauma patients, even those not requiring hospitalization. In the prehospital settings, adequate analgesia makes patients’ transportation issues more feasible, efficient, and tolerable. Moreover, analgesia can prevent physiological and psychological hazards (ie, tachycardia, blood hypertension, anxiety, and stress), increasing patient safety, compliance, and satisfaction.3,4 Pain relief provision involves ethical and legal aspects; it denotes a sensible and civilized society.5
Acute pain is a common symptom in patients requiring assistance from prehospital emergency medical services (EMS). In the literature, 10% to 42% of prehospital patients experience moderate to severe pain;6–8 pain prevalence may reach 67% among trauma patients.9 In 1989 Wilson and Pendleton defined pain undertreatment at any emergency setting as “oligo-analgesia”.10 Oligo-analgesia remains a common phenomenon in the prehospital emergency setting. Indeed, only 20–40% of patients who require ambulance or helicopter emergency medical service (HEMS) receive pharmacological pain treatment.11–13
Conditions for administering analgesic treatment depend on several factors such as provider experience and training, but mainly on the EMS organization.14 In many countries, pharmacological treatments, notably opioids, can only be administered by physicians. To overcome this limit, different strategies allowing analgesics to be administered by emergency medical technicians, paramedics and nurses, have been developed. Standard operating protocols and physician teleconsultation ensure access to analgesic treatment for a larger number of patients.14–16
Through a nationwide survey, we sought to assess the availability and applicability of nurses’ standard analgesia protocols in Italy’s prehospital EMS settings. The gathered data may depict prehospital analgesia treatment’s existing standards and uncover caveats and limitations that may yield practice improvements.
Methods
Study Design and Setting
This nationwide cross-sectional, observational, and descriptive study investigates quantitatively the availability of nurse-administered analgesia in the Italian prehospital emergency setting. This research is part of a dissertation project from the Critical Care Nursing Master course (Director Prof. B. Samolsky Dekel) at the University of Bologna, Italy.
Italian territory has a total area of 301,340 km2 (116,350 square miles) and a population of roughly 60 million people with a density of 201.3/km2 (521.4/square mile). The Italian Republic’s constituent entities are its 107 provinces, which are an intermediate level between a municipality and the 20 Italian regions. For convenience, provinces are grouped in three macro areas (North, Centre, South and Islands). Several small provincial Emergency-Medical-Dispatch-Centres (EMDCs) have recently merged into large-area EMDCs managing EMS on a broader territory, including several provinces or an entire region. All 74 Italian (EMDCs) of the 107 Italian provinces were involved in this survey.
Procedures and Instruments
A scientific panel (SP) of four clinicians and EMS nurses developed the survey. Following literature reviews and recommendations, EMS prehospital pain-treatment essential domains were identified and adapted to create the survey.1,14,17 Hence, the developed survey was presented to five other EMS nurses with prehospital pain treatment experience to assess its face/content validity, adequacy of grammar, wording, and items. For the final survey’s version, the SP resolved by consensus emerged divergences/suggestions. The final version of the questionnaire is available as supplementary material (Supplementary 1).
Between September and October 2017, nurse coordinators of all Italian EMDCs were contacted by phone to introduce the survey’s objectives and were asked to adhere. Three researchers carried out data collection; each of them followed one of Italy’s three geographical areas (North, Centre, South and Islands). An online survey using GoogleDocs® (copyright 2019 Google™, Mountain View, California) was sent to the coordinators. In the case of the impossibility of online compilation, the questionnaire was completed during a telephone interview. Telephone interviews were conducted by reading the survey’s questions following the on-line form. If ever, interview bias is minimal as the survey’s items are limited in length, comprehensible, and mostly require closed answers and thus fit for a telephone interview. Failure to reply after a second attempt resulted in data being archived as “not reported.”
Category variables included in this study are: (1) Italian geographical area (North, Centre, South and Islands), participating provinces, and EMDCs; (2) presence of nurse-staffed ambulances (yes/no); (3) availability of nurse-administered analgesia protocols (yes/no); (4) presence of differentiated protocols for medical and trauma patients (yes/no); (5) analgesic drugs authorized in protocols (generic names).
Ethics
The research meets all applicable standards with regard to the ethics of experimentation and research integrity. Informed consent to participation in the study was obtained from each nurse coordinator before questionnaire submission, clearly explaining that the aspects investigated were related to nursing protocols and procedures and that no sensitive data related to patients were to be collected. Consent was collected and stored in an electronic database, together with the collected data.
Data Presentation and Statistical Analysis
Categorical data for the entire survey and split by geographical areas are reported as absolute numbers and percentages. The available number of analgesic drugs is reported as the median and range. The geographical areas dependence upon independent variable categories (number of nurses-equipped ambulances, availability of analgesia protocols, differentiated analgesia protocols, analgesia drugs, and the number of optional analgesia drugs for medical and trauma patients) is determined using χ2-analysis. When appropriate, the post hoc analyses results (calculated p-values – Bonferroni method – for adjusted residuals) are reported as cell contribution for the reported association (the most influent two). Spearman-rank correlation analysis is used to assess the correlation between area classes and drug items; when statistically significant an absolute Rho value between 0.2 and 0.4 is considered as mild; 0.41–0.7 as moderate and 0.71–1.0 as strong correlation. Statistical significance was defined as P < 0.05. When appropriate, P < 0.01 are reported.
Results
Table 1 describes the rate of the Italian territory, provinces, and EMDCs that participated in the survey. Of the 74 Italian EMDCs, 94.6% (n=70), covering 93.5% (n=100) of the 107 national provinces, completed the survey. The EMDCs participation rate within the three Italian geographical areas (North, Centre, and South and Islands) was between 92.8% (South and Islands) and 96.5% (North).
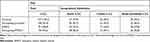 |
Table 1 Distribution of the Survey’s Participating Provinces and EMDCs |
Nurses-equipped ambulances were reported in 94 (94%) of the 100 national screened provinces; their rate was over 90% in each of the three geographical areas considered. The rate of nurses-equipped ambulances, availability of analgesia protocols, and the protocols’ differentiation between medical and trauma patients are detailed in Table 2.
 |
Table 2 Percentage of Nurse-Administered Analgesia Protocols |
The rate of provinces with analgesia protocols for ambulance nurses was 46% (n=46). The latter rate implies that more than half of the Italian ambulance-nurses cannot administer analgesia drugs in prehospital settings. The rate of the Italian provinces with analgesia protocols varies across the national territory. In particular, such protocols are available in two-thirds (66.7%) of the provinces of the Northern area, in less than half (42.8%) and roughly one-fifth (20.6%) of the provinces of the Centre and the South and Islands areas, respectively. Differentiated analgesia protocols for trauma and medical patients were reported only in 22 (22.0%) of the Italian provinces. Low rate of such differentiated analgesia protocols was reported within the South and Islands provinces (8.8%).
Table 3 reports the drugs’ rates included in the nurse-administered analgesia-protocols, split by medical and trauma patients. In particular, for medical and trauma patients, respectively, paracetamol (89.1%) and morphine (76.1–95.7%) are the most common drugs, followed by nonsteroidal anti-inflammatory drugs (NSAIDs) (65.2–43.5%), and fentanyl (39.1–63.0%).
 |
Table 3 Rates of Drugs Included in Nurse-Administered Analgesia Protocols |
Within the three geographical areas, drug availability for analgesia protocols shows notable variability. For medical patients, paracetamol is available in over 90% of the protocols in the North and the Centre and in 70% in the South and Islands area; morphine is available in 83% of the protocols in the North area and roughly in 60% of the other two areas; NSAIDs are available only in a third of the protocols in the Centre area against higher rate in the South and Islands (86%), and in the North (70%); fentanyl is present only in one protocol in the Centre and roughly in 45% in the other two areas. For trauma patients, paracetamol and morphine are available in over 86% of the protocols of all areas, in particular 100% in North and Centre; fentanyl is present in 86% and 63% of the protocols in the South and Islands and North areas, respectively, and only in one protocol of the Centre area; NSAIDs are present in 57%, 22%, and 14% of the protocols in the North, Centre, and South and Islands areas, respectively. Some protocols provide more than one pharmacological option, mainly based on pain score or possible allergies. In all protocols, the analgesic drugs’ administration route is parenteral. Only in seven cases (15.2%), all in the North area, the possibility of intranasal administration was reported.
The overall median number of analgesic drugs available for each analgesia protocol is two for medical patients and three for trauma patients (range 1 to 5). The rates of drugs available in the nurse-administered analgesia protocols, also split by geographical areas and by patients’ groups, are detailed in Table 4.
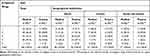 |
Table 4 Rates of Drugs Available in Nurse-Administered Analgesia Protocols |
Table 5 reports the results of the association analyses (χ2-analysis) between geographical areas and independent variables. It also reports the post-hoc analysis results as cell contribution for the reported association. Firstly, significant associations were found between the geographical areas and the variables availability of analgesia protocols, and the number of optional analgesia drugs for medical patients (χ2-analysis, p < 0.01). In particular, post-hoc analyses show that the South and Islands area is associated with no availability of analgesia protocols, followed by the North area’s association with protocols availability. Further, the North area is associated with a combination of three optional drugs for medical patients. Interestingly, the South and Island area is associated with low proportions of morphine and paracetamol availability for both medical and trauma patients and of NSAIDs for trauma patients. In contrast, the North area is associated with high paracetamol availability proportions for both medical and trauma patients and of morphine and fentanyl for medical patients.
 |
Table 5 Association Analyses Between Geographical Areas and Independent Variables |
Table 6 reports the Spearman-rank correlation analyses (absolute Rho and p values) between area classes and drug items. All drugs’ correlations were significant, for both medical and trauma patients, except for NSAIDs. In particular, the correlation between geographical areas and analgesic drugs was mild (Rho range from 0.21 to 0.40). A more substantial yet moderate correlation (Rho range from 0.50 to 0.60) was found between morphine, paracetamol, and fentanyl for both medical and trauma patients. These results imply that available analgesia drugs are roughly similar in all areas’ protocols and that morphine, paracetamol, and fentanyl combinations are frequent.
 |
Table 6 Correlation Analyses Between Area Classes and Drug Items |
Discussion
EMS Organization and Nurse-Administered Analgesia in Italy
In a nationwide survey involving 94.6% of the Italian EMDCs and covering 93.5% of the national provinces, we found that nurse-equipped ambulances are present in 94% of the screened provinces with a rate of over 90% in each of the three geographical areas considered. Nonetheless, only 46% reported analgesia protocols for ambulance nurses, and only 22% reported differentiated analgesia protocols for medical and trauma patients. Analgesia drugs included morphine, paracetamol, NSAIDs and fentanyl. We found substantial variability between geographical areas regarding protocols and analgesic drug availability with low rates in the South and Islands area against relatively high rates in the North area.
To our knowledge, this survey is the most recent analysis on nurse-administered pain treatments in the prehospital EMS setting in Italy and has obtained answers from the majority of the EMDCs present on the national territory. Italian EMS are managed on a provincial basis, with significant organizational differences across the country and particularly on the different role of health care professionals. The most widespread organizational model of prehospital EMS in Italy relies on a dual-response system to grant an increasing level of emergency care, with Basic Life Support (BLS) ambulances, staffed with professional or volunteer rescuers, or nurse-staffed ambulances, with a higher level of assistance, and physician units (medical cars, ambulances or helicopters) required in support for the most critical patients. Although the possibility of administering drugs and other life-saving treatments by ambulance nurses under the authorization of EMS head physician has been guaranteed by law since 1992, procedures and protocols have been developed in the Italian territory in a fragmented and heterogeneous way. Across the 107 Italian provinces it is possible to find EMS with nurses trained and authorized for complete Advanced Life Support (ALS) manoeuvres, while other services do not employ nurses or permit nurses to perform only BLS. Italian intersociety recommendations on pain management in the emergency setting, published in 2015, recommend to manage pain in the prehospital emergency setting with an interdisciplinary approach based on clinical protocols, adequate analgesics supply, and dedicated training for EMS professionals.17 In 2010, a national survey described the availability of analgesic (strong or weak opioids and other drugs) on board of physician-staffed ambulances in Italy; authors considered the availability of analgesics as an indirect indicator of treatment. Results showed the absence of analgesic drugs in 10.6% of physician-staffed ambulances and a substantial difference in the diffusion of strong opioids, widely available in Northern Italy rather than in Central and Southern Italy and Islands (morphine 96% vs 79% vs 44% and fentanyl 84% vs 39% vs 26%). The authors hypothesized that this geographical variability between the different Italian areas could be related to cultural and religious factors and to different approaches of the physicians to pain treatment.5 Even if these results are related only to physician-staffed ambulances, the geographical differences in analgesic availability (and particularly opioids) can be considered comparable to our findings of nurse-administered analgesia protocols, more widespread in Northern Italy than in the Centre and South and Islands. In 2009 another survey tried to describe advanced nursing tasks in the prehospital setting: the percentage of responses from Italian EMDCs was 87.2%, corresponding to a territorial coverage of 89 provinces (83.2%). Nurse-staffed ambulances were available in 53% of the provinces and only 29% of them had pain treatment protocols.18,31 Compared to 2009, our survey reports an increase in the presence of nurses on board of emergency ambulances (94%) and in the percentage of provinces where nurses can administer analgesic drugs through a physician prescribed procedure (46%), with the least presence in the South and Islands area (20.6%). Nevertheless, it is necessary to consider that in more than half of Italian provinces, with consistent differences between the three geographical areas, patients suffering from pain may receive delayed analgesia, having to wait for a physician-staffed unit, or do not receive any treatment. The cause of this disparity between the areas of the North compared with the Centre and South of Italy is probably due to a different organizational setting of the emergency services. Outdated organizational EMS models, based on the presence of volunteer ambulance associations and a physician as the only health care professional, have been consolidated in the last 20 years. Another aspect to consider is that 94% of Italian EMS are equipped with nurse-staffed ambulances but only in half of them nurses are allowed to administer analgesia. This failure to use a specialized and versatile professional resource such as the nurse represents a waste of resources within the complex and interdisciplinary EMS system.
Advantages of Nurse-Administered Analgesia in the Emergency Setting
In recent years, the impact of nurse-initiated analgesia protocols in the emergency department has been widely investigated, demonstrating efficacy and safety. Conversely, the topic of nurse-led analgesia in the EMS setting has been poorly investigated.19–21 Nurse-initiated treatments before the physician’s intervention, authorized by policies or protocols, represent an important strategy to provide timely and effective pain management. In most cases, nurses are the first health care providers to take care of patients in the emergency setting, both in-hospital and pre-hospital, and they are in an optimal position to ensure an early treatment for pain and other symptoms.22 Nurse-administered analgesia is based on a defined treatment algorithm requiring a pain evaluation and the administration of a fixed dose or a weight dependant dose of drug. Usually, the option between an opioid or another drug depends on pain score. A recent systematic review analysing pre-hospital pain management guidelines reported that the majority of actual guidelines recommend paracetamol as the medication of choice for the treatment of mild pain and fentanyl and morphine for severe pain.23
To maximize patient safety, some EMS provide single-drug protocols with dosing restrictions, but with the risk of suboptimal analgesia.23 Another option comes from teleconsultation, transmitting vital signs, communications or videos to a physician; telemedically delegated analgesia led to an optimal pain relief, without severe adverse events related to analgesic drugs.14–16,23,24 Opioids, ketamine, and NSAIDs are reported to provide safe and optimal analgesia for acute pain in the prehospital setting.25 Safety of opioid-based protocols is ensured by vital signs monitoring, the availability of antidotes (naloxone), bag mask ventilation, and providers’ expertise in emergency procedures.26 Moreover, even if opioid related complications, such as nausea, vomiting, hypoxia and hypotension, are reported as very low, a two-tier emergency system guarantees medical support in case of adverse events or unmanageable pain.7,27–30
International experiences from other European countries such as Switzerland, Germany, and Denmark, as well as Australia and the United States, reported that paramedic or nurse analgesia projects are safe and effective, and could optimize treatment for a wider range of patients, particularly in rural and remote prehospital environments.4,16,24 A retrospective analysis evaluating analgesia administered by physicians and paramedics in over 20,000 prehospital missions in Switzerland showed that both groups achieved sufficient pain relief (76% vs 77%, p 0.82) but while physicians treated 776 patients, paramedics administered analgesia to 15,293, a number twenty times larger.31
Literature findings report that prehospital analgesia has a high profile of efficacy and safety and indicate the need for Italian EMS to improve an appropriate usage of a standard orders protocol system for ambulance nurses. The principal aim should be to extend the capability for an intermediate or advanced level of emergency care to a wider number of patients, not only limited to pain treatment. The advanced competencies acquired through dedicated training and specialized education (eg, Critical Care Nursing Master or ALS courses), make nurses a valuable resource able to guarantee an equal level of emergency care to a wider range of citizens.
Study Limitations
Although the overall response rate to our survey was very high, Italian EMS are experiencing a period of important dynamic changes and thus our survey should be considered as a snapshot of the Italian situation at the moment of the survey. Nonetheless, results are important as a benchmark condition to be compared in future similar surveys. The number of the survey’s items was limited in order to deliver a feasible and concise questionnaire. Future surveys should include additional items regarding the protocols’ implementation way (standardized prescription protocols, telemedicine consultations or authorization advice by telephone with EMDC physicians), which pain evaluation tools are used, indications for each analgesic, analgesic dose, and analgesia administration routes. For a more complete analysis of this topic, it is also advisable to invest in additional aspects such as adverse event monitoring and educational programs for prehospital pain management. Continuous monitoring of the development and deployment of nursing protocols in the Italian prehospital setting would be appropriate.
Conclusions
Recognition, assessment, and treatment of pain should be considered mandatory for every health care professional for clinical, legal, and ethical reasons. Despite the demonstrated efficacy and safety reported by international experiences, nurse-administered prehospital analgesia protocols are available in less than half of Italian provinces, with substantial differences between Northern, Central, and Southern areas. These results indirectly indicate potential undertreatment of prehospital pain in Italy and yield practice improvements.
Ethical Statement
The research meets all applicable standards with regard to the ethics of experimentation and research integrity. Ethical Committee approval is not required at our institution for this type of research, not involving patient-related data.
Author Contributions
All authors made a significant contribution to the conception, study design, execution, acquisition of data, analysis, and interpretation of data. All authors took part in drafting and critically reviewing the article; gave final approval of the version to be published; have agreed to submit it to the current journal; and agreed to be responsible for all aspects of the work.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Disclosure
The authors declare no conflicts of interest.
References
1. Gausche-Hill M, Brown KM, Oliver ZJ, et al. An evidence-based guideline for prehospital analgesia in trauma. Prehosp Emerg Care. 2014;18(SUPPL.1):25–34. doi:10.3109/10903127.2013.844873
2. Ariès P, Montelescaut E, Pessey F, Des Déserts MD, Giacardi C. Pre-hospital emergency medicine: pain control. Lancet. 2016;387(10020):747. doi:10.1016/S0140-6736(16)00325-1
3. Thomas SH, Shewakramani S. Prehospital trauma analgesia. J Emerg Med. 2008;35(1):47–57. doi:10.1016/j.jemermed.2007.05.041
4. Lenssen N, Krockauer A, Beckers SK, et al. Quality of analgesia in physician-operated telemedical prehospital emergency care is comparable to physician-based prehospital care - a retrospective longitudinal study. Sci Rep. 2017;7(1):1–10. doi:10.1038/s41598-017-01437-5
5. Marinangeli F, Narducci C, Ursini ML, et al. Acute pain and availability of analgesia in the prehospital emergency setting in Italy: a problem to be solved. Pain Pract. 2009;9(4):282–288. doi:10.1111/j.1533-2500.2009.00277.x
6. Jennings PA, Cameron P, Bernard S. Epidemiology of prehospital pain: an opportunity for improvement. Emerg Med J. 2011;28(6):530–531. doi:10.1136/emj.2010.098954
7. Friesgaard KD, Riddervold IS, Kirkegaard H, Christensen EF, Nikolajsen L. Acute pain in the prehospital setting: a register-based study of 41.241 patients. Scand J Trauma Resusc Emerg Med. 2018;26(1):1–10. doi:10.1186/s13049-018-0521-2
8. Galinski M, Ruscev M, Gonzalez G, et al. Prevalence and management of acute pain in prehospital emergency medicine. Prehosp Emerg Care. 2010;14(3):334–339. doi:10.3109/10903121003760218
9. Albrecht E, Taffe P, Yersin B, Schoettker P, Decosterd I, Hugli O. Undertreatment of acute pain (oligoanalgesia) and medical practice variation in prehospital analgesia of adult trauma patients: a 10 year retrospective study. Br J Anaesth. 2013;110(1):96–106. doi:10.1093/bja/aes355
10. Borland ML, Jacobs I, Rogers IR. Options in prehospital analgesia. Emerg Med. 2002;14(1):77–84. doi:10.1046/j.1442-2026.2002.00288.x
11. Xia AD, Dickerson SL, Watson A, Nokela M, Colman S, Szende A. Evaluation of pain relief treatment and timelines in emergency care in six European countries and Australia. Open Access Emerg Med. 2019;11:229–240. doi:10.2147/oaem.s214396
12. Scholten AC, Berben SAA, Westmaas AH, et al. Pain management in trauma patients in (pre)hospital based emergency care: current practice versus new guideline. Injury. 2015;46(5):798–806. doi:10.1016/j.injury.2014.10.045
13. Spilman SK, Lechtenberg GT, Hahn KD, et al. Is pain really undertreated? Challenges of addressing pain in trauma patients during prehospital transport and trauma resuscitation. Injury. 2016;47(9):2018–2024. doi:10.1016/j.injury.2016.03.012
14. Kontinen V. Pain outside of the hospital: what is the situation in pre-hospital care, and how could it be improved? Scand J Pain. 2015;8:35–36. doi:10.1016/j.sjpain.2015.05.001
15. Brown KM, Hirshon JM, Alcorta R, et al. The implementation and evaluation of an evidence-based statewide prehospital pain management protocol developed using the national prehospital evidence-based guideline model process for emergency medical services. Prehosp Emerg Care. 2014;18(SUPPL.1):45–51. doi:10.3109/10903127.2013.831510
16. Brokmann JC, Rossaint R, Hirsch F, et al. Analgesia by telemedically supported paramedics compared with physician-administered analgesia: a prospective, interventional, multicentre trial. Eur J Pain. 2016;20(7):1176–1184. doi:10.1002/ejp.843
17. Savoia G, Coluzzi F, Maria CDI, Ambrosio F, Della Corte F. Italian intersociety recommendations on pain management in the emergency setting. Minerva Anestesiol. 2015;81(2):205–225.
18. Imbriaco G, Mostardini M, Erbacci M, et al. Analisi delle competenze infermieristiche nei servizi di emergenza preospedaliera: i risultati di un’indagine multicentrica Italiana. Scenario. 2010;27(4):35–42.
19. Varndell W, Fry M, Elliott D. Quality and impact of nurse-initiated analgesia in the emergency department: a systematic review. Int Emerg Nurs. 2018;40:46–53. doi:10.1016/j.ienj.2018.05.003
20. Pierik JG, Berben SA, IJzerman MJ, et al. A nurse-initiated pain protocol in the ED improves pain treatment in patients with acute musculoskeletal pain. Int Emerg Nurs. 2016;27:3–10. doi:10.1016/j.ienj.2016.02.001
21. Douma MJ, Drake CA, O’Dochartaigh D, Smith KE. A pragmatic randomized evaluation of a nurse-initiated protocol to improve timeliness of care in an urban emergency department. Ann Emerg Med. 2016;68(5):546–552. doi:10.1016/j.annemergmed.2016.06.019
22. Varndell W, Fry M, Elliott D. Pain assessment and interventions by nurses in the emergency department: a national survey. J Clin Nurs. 2020;29(13–14):2352–2362. doi:10.1111/jocn.15247
23. Yousefifard M, Askarian-Amiri S, Madani Neishaboori A, Sadeghi M, Saberian P, Baratloo A. Pre-hospital pain management; a systematic review of proposed guidelines. Arch Acad Emerg Med. 2019;7(1):e55.
24. Scharonow M, Alberding T, Oltmanns W, Weilbach C. Project for the introduction of prehospital analgesia with fentanyl and morphine administered by specially trained paramedics in a rural service area in Germany. J Pain Res. 2017;10:2595–2599. doi:10.2147/JPR.S151077
25. Sobieraj DM, Martinez BK, Miao B, et al. Comparative effectiveness of analgesics to reduce acute pain in the prehospital setting. Prehosp Emerg Care. 2019:1–12. doi:10.1080/10903127.2019.1657213
26. Häske D, Böttiger BW, Bouillon B, et al. Analgesia in patients with trauma in emergency medicine-a systematic review and meta-analysis. Dtsch Arztebl Int. 2017;114(46):785–792. doi:10.3238/arztebl.2017.0785
27. Friesgaard KD, Nikolajsen L, Giebner M, et al. Efficacy and safety of intravenous fentanyl administered by ambulance personnel. Acta Anaesthesiol Scand. 2016;60(4):537–543. doi:10.1111/aas.12662
28. Kanowitz A, Dunn TM, Kanowitz EM, Dunn WW, VanBuskirk K. Safety and effectiveness of fentanyl administration for prehospital pain management. Prehosp Emerg Care. 2006;10(1):1–7. doi:10.1080/10903120500373264
29. Soriya GC, McVaney KE, Liao MM, et al. Safety of prehospital intravenous fentanyl for adult trauma patients. J Trauma Acute Care Surg. 2012;72(3):755–759. doi:10.1097/TA.0b013e31823c4444
30. Friesgaard KD, Kirkegaard H, Rasmussen CH, Giebner M, Christensen EF, Nikolajsen L. Prehospital intravenous fentanyl administered by ambulance personnel: a cluster-randomised comparison of two treatment protocols. Scand J Trauma Resusc Emerg Med. 2019;27:1. doi:10.1186/s13049-019-0588-4
31. Kiavialaitis GE, Müller S, Braun J, et al. Clinical practice of pre-hospital analgesia: an observational study of 20978 missions in Switzerland. Am J Emerg Med. 2020;38(11):2318–2323. doi:10.1016/j.ajem.2019.10.033
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
