Back to Journals » Journal of Pain Research » Volume 9
Nucleoplasty for treating lumbar disk degenerative low back pain: an outcome prediction analysis
Authors Liliang PC, Lu K, Liang CL, Chen YW, Tsai YD, Tu YK
Received 5 July 2016
Accepted for publication 25 August 2016
Published 31 October 2016 Volume 2016:9 Pages 893—898
DOI https://doi.org/10.2147/JPR.S116533
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Michael Schatman
Po-Chou Liliang,1 Kang Lu,1 Cheng-Loong Liang,1 Ya-Wen Chen,2,3 Yu-Duan Tsai,1 Yuan-Kun Tu4
1Department of Neurosurgery, E-Da Hospital, 2Department of Nursing, I-Shou University, 3School of Nursing, Kaohsiung Medical University, 4Department of Orthopedic Surgery, E-Da Hospital, I-Shou University, Kaohsiung, Taiwan
Purpose: Nucleoplasty is a minimally invasive technique that is considered efficacious in alleviating lumbar disk degenerative low back pain (LBP). The efficacy of nucleoplasty and identified variables that can predict pain relief for nucleoplasty was reported.
Patients and methods: Between December 2013 and November 2015, 47 nucleoplasty procedures on 47 lumbar disks in 31 consecutive patients were performed. The outcome was evaluated using a visual analog scale (VAS) score. Improvements of ≥50% in VAS scores were considered substantial pain relief. The variables associated with pain relief after nucleoplasty included: 1) age; 2) sex; 3) body mass index; 4) hyperintensity zone at the rear of the disk; 5) hypointensity of the disk; 6) Modic changes of the end plates; 7) spinal instability pain; and 8) discography results.
Results: Twenty-one patients (67.7%) experienced substantial pain relief. The most common side effects following nucleoplasty were soreness at the needle puncture site (64.5%), numbness in the lower leg (12.9%), and increased intensity of back pain (9.7%). All side effects were transient. Multivariate analysis revealed that the discography results were the most critical predictor for substantial pain relief of nucleoplasty (P=0.03). The sensitivity and specificity of discography were 92.8% and 62.5%, respectively.
Conclusion: Discography results could improve the success rate of nucleoplasty in the treatment of disk degenerative LBP.
Keywords: low back pain, lumbar disk degenerative, nucleoplasty, discography
Introduction
Lumbar disk degenerative low back pain (LBP) has been estimated in ~28%–40% of all types of LBP.1,2 Some patients with disk degenerative LBP improve without requiring intervention. However, some patients develop chronic LBP.3 The conventional treatment for disk degenerative LBP includes rest, narcotic and nonnarcotic analgesia, behavioral management, and physical therapy. Surgical interventions (discectomy and spinal fusion) for patients with small, contained degenerative disks are controversial because the clinical outcomes of the interventions are not favorable.4–6
Several minimally invasive techniques have been developed to treat disk degenerative LBP for several years. Nucleoplasty is a minimally invasive technique that was first approved by the US Food and Drug Administration in 2000.7 Nucleoplasty reduces intradiscal pressure through a patented coblation technology, in which bipolar radiofrequency energy is utilized to ablate and remove disk materials.8 Some preliminary reports support the efficacy of nucleoplasty in lumbar disk degenerative LBP.8–10
However, the optimum candidates for nucleoplasty remain unclear. In this article, the efficacy of nucleoplasty and identified variables that predict substantial pain relief for nucleoplasty in management for lumbar disk degenerative LBP was reported.
Patients and methods
Patients and eligibility
This retrospective study was approved by the E-Da Hospital Institutional Review Board. Because this is a retrospective study, no written informed consent was required from patients according to the Institutional Review Board of E-Da Hospital. Forty seven nucleoplasty procedures on 47 lumbar disks in 31 consecutive patients between December 2013 and November 2015 were performed. Patients with lumbar disk degenerative LBP without radiculopathy were selected to receive nucleoplasty if they had persistent LBP that was refractory to conservative treatment for >3 months. All patients participated in medical history taking, imaging studies (plain radiography, computed tomography, and MRI), and physical examinations to exclude other causes of back pain. The inclusion criteria were as follows: axial back pain with or without radicular pain, failed conservative care of ≥3 months, no neurologic deficit, and disk herniation ≤5 mm. The exclusion criteria were as follows: sequestered or extruded disk herniation, spinal fracture, spondylolisthesis, marked spinal stenosis, progressive neurological deficits, tumor, infection, heavy opioid usage, uncontrolled psychological disorders, litigation, disk height <25% of adjacent level, coagulopathies, and previous spinal surgery on the same level.
Intervention
Nucleoplasty was performed under strict sterile conditions in an operating room. All patients received intravenous sedation prior to the procedure to ensure their comfort. A prophylactic dose of 1 g cefazolin was administered intravenously prior to the procedure. Twenty-two patients received provocative discography to identify the painful disks.11 In the other patients, the therapeutic targets were determined according to the imaging results (high-intensity zone [HIZ] at the rear of the disk, hypointensity of the disk, and Modic changes of the end plates). Standard nucleoplasty procedures, which were described previously,8 were selected for the patients with painful degenerative disks.
A 17-gage needle was introduced via a posterolateral approach toward the identified disk level and advanced into the central portion of the disk under fluoroscopic guidance. A coblation bipolar device (Perc DLG SpineWand connected to ArthroCare System 2000; ArthroCare, Austin, TX, USA) was used in the entire procedure. All patients were observed for 2–4 hours postoperatively for any complications or neurological deficits related to the procedure.
Outcome
After nucleoplasty, the patients were observed for an average period of 10 months (range 4–17 months) in outpatient clinics. Changes in pain were recorded by using a visual analog scale (VAS) ranging from 0 (no pain) to 10 (extremely severe pain). Improvements of ≥50% in VAS scores were considered as substantial pain relief.
Variables
To study variables associated with pain relief after nucleoplasty, the following factors of each patient were observed and analyzed: 1) age; 2) sex; 3) body mass index (BMI); 4) HIZ at the rear of the disk; 5) hypointensity of the disk; 6) Modic changes of the end plates; 7) spinal instability pain; and 8) the discography results. Spinal instability pain is defined as pain that occurs during flexion, extension, and lifting. HIZ at the rear of the disk, hypointensity of the disk, and Modic changes of the end plates (type I and II)12 were observed in the MRI scans. HIZ is defined as a bright white signal in T2W images in the posterior annulus of the disk and represents a tear in the posterior annulus.13 The hypointensity of the disk on T2W images,14,15 resulting in a black disk, is evaluated as a variable associated with the effects of nucleoplasty. Modic end plates of types I and II are typically observed in patients with chronic LBP.16 In the present study, Modic type I and II changes were recorded.
Positive discography is defined as concordant pain reproduction of the examined disk and the absence of pain on provocation of the nearest disk.17,18 Typically, the targets of nucleoplasty were selected on the basis of the discography results. Some nucleoplasty procedures did not provide these results. Nine patients received nucleoplasty without discography data.
Statistical analysis
Patients were grouped based on their substantial pain reduction, with the purpose to identify potential predictors. Data were first subjected to univariate analysis using either chi-square test or Fisher’s exact test, as appropriate, for the variables sex, HIZ at the rear of the disk, hypointensity of the disk, Modic changes of the end plates, spinal instability pain, and the results of discography. The effects of age and BMI on nucleoplasty were determined using the Student’s t-test. Multivariate analysis with stepwise logistic regression was performed to determine the predictive factors for improving the outcomes of nucleoplasty. The findings were considered statistically significant if the P-values were <0.05. Data were analyzed using SPSS 16.0 (SPSS Inc., Chicago, IL, USA).
Results
Table 1 presents the details of clinical characteristics, image findings, results of discography, and effects of nucleoplasty for all subjects. In total, 51 nucleoplasty procedures were performed in 31 patients according to the discography or imaging results: 5 nucleoplasty procedures for L34, 28 procedures for L45, and 18 procedures for L5S1. Twenty-one patients (67.7%) had substantial pain relief (improvements in VAS ≥50%). This series did not include any major complications. The most common side effects following nucleoplasty were as follows: soreness at the needle puncture site (64.5%), new numbness in the lower leg (12.9%), and increased intensity of back pain (9.7%). Soreness, numbness, and back pain subsided in all the patients after 4 weeks.
The results of univariate analysis from the comparison of the substantial pain relief group and poor pain relief group are briefly summarized in Table 2. Age differences were not observed between the groups. Furthermore, sex, BMI, baseline VAS score, Modic changes of the end plates, and spinal instability pain were not associated with substantial pain relief. Patients with HIZ at the rear of the disk (n=24) and hypointensity of the disk (n=27) showed increased rates of substantial pain relief. However, the statistical results were not significant (P=0.17 and P=0.08, respectively). The discography results showed significant associations with substantial pain relief (P=0.01).
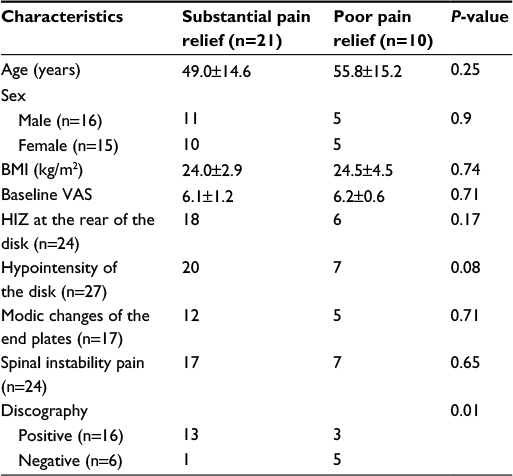  | Table 2 Characteristics of patients with substantial pain relief and those with poor pain relief Abbreviations: BMI, body mass index; VAS, visual analog scale; HIZ, high-intensity zone. |
Furthermore, multivariate analysis with stepwise logistic regression was performed to determine the most critical predictor for substantial pain relief. The analysis revealed that the discography result was the most critical predictor for substantial pain relief after nucleoplasty (P=0.03). The sensitivity and specificity of discography were 92.8% and 62.5%, respectively. The positive predictive value and negative predictive value were 81.3% and 83.3%, respectively.
Discussion
Nucleoplasty is a minimally invasive technique that was approved by the US Food and Drug Administration in 2000.7 Using nucleoplasty, the authors aimed to achieve percutaneous disk decompression through a patented coblation technology, which utilizes the bipolar radiofrequency energy to dissolve the tissue of nucleus pulposus and decrease the intradiscal pressure. The success rate of substantial pain relief post nucleoplasty, which has been reported, varies from 6.3% to 84%.8,10,19,20 Most studies have reported a success rate of >50%. The findings of this study are consistent with those of the previous studies,6,8,10,19,20 with 67.7% substantial pain relief (improvements of ≥50% in VAS scores) at the final follow-up.
Furthermore, in the present study, variables that predict substantial pain relief for nucleoplasty were identified. To date, the optimum candidates for nucleoplasty remain unclear. The predicted values of patients’ characteristics, imaging results, and discography results on nucleoplasty outcomes were interpreted retrospectively. This study reveals that positive discography results are associated with substantial pain relief following nucleoplasty. If the discography results are positive, 81.3% of patients could obtain substantial pain relief. If the discography results are negative, only 16.7% of patients could obtain substantial pain relief. The use of discography results could facilitate target disk selection and improve the success rate of nucleoplasty in the treatment of disk degenerative LBP. A painful disk can be determined if discography is performed properly.21 A true painful disk would respond well to a nucleoplasty procedure. The patients with LBP who failed to respond to nucleoplasty may have pain from other sources, such as sacroiliac joints and facet joints.
Although the predictive value is high in this study, discography has not been routinely used to determine a painful disk for nucleoplasty.8,10 The validity and accuracy of discography for the diagnosis of painful disk is arguable.22,23 A high rate of false-positive results of discography has been reported in asymptomatic participants, patients with chronic pain, patients who had undergone posterior iliac bone graft harvesting procedures, or patients with psychological pathology. Discography is invasive and involves complications such as infection, diskitis,24 allergy to injection material, and bleeding. Some patients refuse discography because of its invasive manner and associated complications. Discography also has some limitations; some subjects had mixed etiologies and some remained undiagnosed after discography.25 However, discography showed high specificity (92.8%) in this study. No patients who received discography in the study showed related complications.
The utilization of imaging studies for the diagnosis of degenerative LBP has increased significantly in recent years; the most critical question is whether this improves patient outcomes. Modic changes of the end plates, hypointensity of the disk, and HIZ at the rear of the disk on MRI are often considered as predictive markers for disk degenerative LBP. In the present study, HIZ at the rear of the disk, hypointensity of the disk, and Modic changes of the end plates did not provide high sensitivity and specificity for the prediction of substantial pain relief after nucleoplasty (Table 3). HIZ at the rear of the disk showed high sensitivity (85.7%) in substantial pain relief; however, its specificity was low (40%). Hypointensity of the disk also had high specificity (95.2%) and low specificity (30%).
Aprill and Bogduk13 described the HIZ as a useful imaging marker of a painful disk (sensitivity 82%; specificity 89%). Schellhas et al26 also reported HIZ as a useful marker in one retrospective study. HIV as a marker of discogenic pain was challenged by some reports,15,27 which stated that sensitivity and specificity of HIZ are not high enough as a useful marker of discogenic pain. The causes are not clear. One explanation may be the various definitions of the HIZ and variability of the gold standard test (provocation discography). Some studies27,28 have also shown various results of the prediction value for Modic changes of the end plates and hypointensity of the disk as a discogenic marker. Therefore, the prediction value of such image markers is not yet established. Image markers for predicting substantial pain relief after nucleoplasty have limited sensitivity and specificity, which may lead to false-positive or false-negative results.
Limitations
This study has several limitations. The present study was a retrospective study with a relatively small sample, which could create a bias. Subjective VAS scores were used in the present study for measuring the outcomes. The chart reviews did not include physical functioning assessments. An objective tool for LBP physical functioning data could improve the outcome measurements. The patients were allowed to receive nucleoplasty despite the absence of discography data or negative discography results. This could decrease the success rate of nucleoplasty.
Conclusion
The pain relief of nucleoplasty for disk degenerative LBP is ~67.7%. The best outcome predictor for nucleoplasty is discography. Discography results could improve the success rate of nucleoplasty for the treatment of disk degenerative LBP primarily because it would enable the determination of a painful disk before nucleoplasty.
Disclosure
The authors report no conflicts of interest in this work.
References
Schwarzer AC, Aprill CN, Derby R, Fortin J, Kine G, Bogduk N. The prevalence and clinical features of internal disc disruption in patients with chronic low back pain. Spine. 1995;20(17):1878–1883. | ||
Zhou YL, Abdi S. Diagnosis and minimally invasive treatment of lumbar discogenic pain – a review of the literature. Clin J Pain. 2006;22(5):468–481. | ||
Peng B, Fu X, Pang X, et al. Prospective clinical study on natural history of discogenic low back pain at 4 years of follow-up. Pain Physician. 2012;15(6):525–532. | ||
Dora C, Schmid MR, Elfering A, Zanetti M, Hodler J, Boos N. Lumbar disk herniation: do MR imaging findings predict recurrence after surgical diskectomy? Radiology. 2005;235(2):562–567. | ||
Mirza SK, Deyo RA. Systematic review of randomized trials comparing lumbar fusion surgery to nonoperative care for treatment of chronic back pain. Spine (Phila Pa 1976). 2007;32(7):816–823. | ||
Robaina-Padrón FJ. [Controversies about instrumented surgery and pain relief in degenerative lumbar spine pain]. Results of scientific evidence. Neurocirugia (Astur). 2007;18(5):406–413. Spanish. | ||
Gerges FJ, Lipsitz SR, Nedeljkovic SS. A systematic review on the effectiveness of the nucleoplasty procedure for discogenic pain. Pain Physician. 2010;13(2):117–132. | ||
Kumar NS, Shah SM, Tan BW, Juned S, Yao K. Discogenic axial back pain: is there a role for nucleoplasty? Asian Spine J. 2013;7(4):314–321. | ||
Singh V, Piryani C, Liao K. Role of percutaneous disc decompression using coblation in managing chronic discogenic low back pain: a prospective, observational study. Pain Physician. 2004;7(4):419–425. | ||
Cincu R, Lorente Fde A, Gomez J, Eiras J, Agrawal A. One decade follow up after nucleoplasty in the management of degenerative disc disease causing low back pain and radiculopathy. Asian J Neurosurg. 2015;10(1):21–25. | ||
Putzier M, Streitparth F, Hartwig T, Perka CF, Hoff EK, Strube P. Can discoblock replace discography for identifying painful degenerated discs? Eur J Radiol. 2013;82(9):1463–1470. | ||
Modic MT, Masaryk TJ, Ross JS, Carter JR. Imaging of degenerative disk disease. Radiology. 1988;168(1):177–186. | ||
Aprill C, Bogduk N. High-Intensity zone: a diagnostic sign of painful lumbar disc on magnetic resonance imaging. Br J Radiol. 1992;65(773):361–369. | ||
Collins CD, Stack JP, O’Connell DJ, et al. The role of discography in lumbar disc disease: a comparative study of magnetic resonance imaging and discography. Clin Radiol. 1990;42(4):252–257. | ||
Weishaupt D, Zanetti M, Hodler J, et al. Painful lumbar disk derangement: relevance of endplate abnormalities at MR imaging. Radiology. 2001;218(2):420–427. | ||
Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR. Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology. 1988;166(1 Pt 1):193–199. | ||
Saboeiro GR. Lumbar discography. Radiol Clin North Am. 2009;47(3):421–433. | ||
Kluner C, Kivelitz D, Rogalla P, Putzier M, Hamm B, Enzweiler C. Percutaneous discography: comparison of low-dose CT, fluoroscopy and MRI in the diagnosis of lumbar disc disruption. Eur Spine J. 2006;15(5):620–626. | ||
Mirzai H, Tekin I, Yaman O, Bursali A. The results of nucleoplasty in patients with lumbar herniated disc: a prospective clinical study of 52 consecutive patients. Spine J. 2007;7(1):88–92; discussion 92–93. | ||
Cohen SP, Williams S, Kurihara C, Griffith S, Larkin TM. Nucleoplasty with or without intradiscal electrothermal therapy (IDET) as a treatment for lumbar herniated disc. J Spinal Disord Tech. 2005;18(suppl):S119–S124. | ||
Wolfer LR, Derby R, Lee JE, Lee SH. Systematic review of lumbar provocation discography in asymptomatic subjects with a meta-analysis of false-positive rates. Pain Physician. 2008;11(4):513–538. | ||
Carragee EJ, Tanner CM, Yang B, Brito JL, Truong T. False-positive findings on lumbar discography. Reliability of subjective concordance assessment during provocative disc injection. Spine. 1999;24(23):2542–2547. | ||
Carragee EJ, Alamin TF, Miller J, Grafe M. Provocative discography in volunteer subjects with mild persistent low back pain. Spine J. 2002;2(1):25–34. | ||
Verrills P, Nowesenitz G, Barnard A. Prevalence and Characteristics of Discogenic Pain in Tertiary Practice: 223 Consecutive Cases Utilizing Lumbar Discography. Pain Med. 2015;16(8):1490–1499. | ||
Osti OL, Fraser RD, Vernon-Roberts B. Discitis after discography. The role of prophylactic antibiotics. J Bone Joint Surg Br. 1990;72(2):271–274. | ||
Schellhas KP, Pollei SR, Gundry CR, Heithoff KB. Lumbar disc high-intensity zone: correlation of magnetic resonance imaging and discography. Spine. 1996;21(1):79–86. | ||
Kang CH, Kim YH, Lee SH, et al. Can magnetic resonance imaging accurately predict concordant pain provocation during provocative disc injection? Skeletal Radiol. 2009;38(9):877–885. | ||
O’Neill C, Kurgansky M, Kaiser J, Lau W. Accuracy of MRI for diagnosis of discogenic pain. Pain Physician. 2008;11(3):311–326. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


