Back to Journals » Local and Regional Anesthesia » Volume 13
Novice and Expert Anesthesiologists’ Eye-Tracking Metrics During Simulated Epidural Block: A Preliminary, Brief Observational Report
Authors Capogna E , Salvi F , Delvino L, Di Giacinto A , Velardo M
Received 15 June 2020
Accepted for publication 6 August 2020
Published 21 August 2020 Volume 2020:13 Pages 105—109
DOI https://doi.org/10.2147/LRA.S267879
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Stefan Wirz
Emanuele Capogna,1 Francesco Salvi,1 Lorena Delvino,2 Andrea Di Giacinto,2 Matteo Velardo1
1EESOA Maternal Neonatal Simulation Center, European School of Obstetric Anesthesia, Rome, Italy; 2SrLabs, Milan, Italy
Correspondence: Emanuele Capogna
EESOA Maternal Neonatal Simulation Center, European School of Obstetric Anesthesia, Via Giulia di Gallese 15, Rome 00151, Italy
Email [email protected]
Introduction: Eye tracking is the process of measuring an individual’s eye movements to register their attentional behavior by using a device called an eye-tracker. Studies conducted using eye-tracking techniques have demonstrated a number of differences in eye movement parameters and patterns between experts and novices. The aim of this preliminary study was to evaluate if there are any differences in eye-tracking metrics between novice and expert anesthesiologists during the performance of an epidural block using an epidural simulator.
Methods: Seven experts and seven novices who gave their consent to this preliminary study were asked to perform an epidural technique using an epidural simulator while wearing a pair of Tobii Pro glasses. Number of fixations, fixation duration, heat maps and scan-paths were examined by Tobii Pro Lab Software. Duration of the procedure was also recorded.
Results: The observation of the attentional heat map and gaze plot showed different gaze dispersion between experts and novices. The mean total duration of fixations during needle insertion and advancement and catheter introduction was lower in experts than trainees (respectively, 0.18 vs 3.56 sec; P< 0.05 and 0.73 vs 2.48 sec; P< 0.05). The mean fixation count was greater in experts vs trainees (5 vs 2; P< 0.05). The mean duration of the epidural procedure was 104.16 (41) (trainees) vs 65.3 (32.6) seconds (experts) (P< 0.05). Expert anesthesiologists spent more time fixating a more specific target location (eg, the point of the epidural needle rather than the syringe’s barrel) whilst novices split their attention between tracking their tools and the target location.
Discussion: Eye tracking may have interesting implications for the creation of assessment programs, which distinguish skill level through the use of gaze behavior, and may be a promising tool for monitoring training progress towards the development of expertise.
Keywords: simulation, epidural technique, eye tracking
Introduction
Epidural block is a complex procedure and requires cognitive skills, such as the knowledge of the anatomy and of the procedure, along with psychomotor skills, such as those required to perform the technique, one of the most difficult to master in anesthesia.1
Eye tracking is the process of measuring an individual’s eye movements, using a device called an eye-tracker, to register his attentional behavior while performing a task. By recording the direction of a user’s gaze and relationship to an area of interest (AOI), eye‐tracking technology provides an objective tool for measuring visual patterns. It has been used in psychology, in psycholinguistics, marketing, as an input device for human-computer interaction, and in product design, and, most recently, also in some fields of medicine and nursing, for both training and assessment.2
For procedural and visual‐based tasks, eye tracking holds great promise as a tool for monitoring training progress towards the development of expertise in medicine. For example, experienced surgeons spend more time concentrating on target location whilst novices split their attention between tracking their tools, the operative site, the sterile field and target location.3
The aim of this preliminary, observational study was to evaluate if there are any differences in eye-tracking metrics between novice and expert anesthesiologists during the performance of the epidural block using an epidural simulator.
Methods
Ethical approval was requested and was waived by the Research Ethics Committee because they deemed it unnecessary due to the nature of the study, as no patients were involved, the participants were volunteers, all their data were completely anonymized, and all the investigators had no conflict of interest since they were not involved in any teaching program of the University to which the trainees belonged. This decision was in agreement with the eligibility of this study for exemption according to US Federal Human Subject Regulations-Protection of Human Subjects. Each participant gave written informed consent and privacy, confidentiality and anonymity were fully guaranteed by the EESOA Research Board.
We enrolled 7 novice trainees and 7 expert anesthesiologists with more than 15 years experience in epidural techniques who were asked to perform the epidural procedure using a standardized epidural simulator, while wearing the eye-tracking glasses.
For this study, we used a commercially available Tobii Pro Glasses 50 Hz wearable wireless eye tracker (Figure 1). This system can measure eye movements using cameras integrated into the eyeglasses which record the corneal reflection of infrared lighting to track pupil position, mapping the subject’s focus of attention on video recordings of the subject’s field of vision (gaze).
 |
Figure 1 The Tobii Pro Glasses 50 Hz wearable wireless eye tracker. |
All the eye-tracked epidural procedures were recorded immediately after accurate individual calibration, during which the participant, after wearing the glasses unit, focused on the center of the calibration target.
All the eye-tracking video-recordings were stored and analyzed by using a Tobii Pro Lab Software. We selected six areas of interest (AOI), to define regions of a displayed stimulus, and to extract metrics specifically for those regions. The areas were the following: 1) point of the epidural needle at its insertion into the skin; 2) shaft of the epidural needle; 3) hub of the needle; 4) barrel of the syringe; 5) plunger of the syringe; 6) other fields of view (Figure 2).
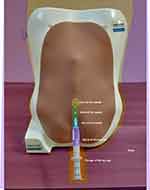 |
Figure 2 Areas of interest (AOI). |
We also divided the epidural procedure into two phases: (1) needle insertion and its advancement and (2) epidural catheter introduction and its advancement.
The number and duration of fixations for each area of interest and for each phase were examined.
Fixations are represented as discrete samples of almost stable points where the eye is looking. Their duration is the elapsed time between the start of the first fixation on the AOI until the end of the last fixation on the AOI.
Eye-tracking metrics were mapped as gaze plots and heat maps. Gaze plots show the location, order, and time spent looking at locations on the stimulus. Time spent looking, most commonly expressed as fixation duration, is shown by the diameter of the fixation circles. The longer the look, the larger the circle.
Heat maps show how looking is distributed over the stimulus and can effectively reveal the focus of visual attention.
For the purpose of the study, we used a validated, modified version of a commercially available epidural simulator (P61, 3B Scientific) which can realistically reproduce the anatomical features of the layers the needle must pass through to reach the epidural space.4
The total duration of the procedure was defined as the length of time between the insertion of the epidural needle into the skin of the simulator and the introduction of the catheter into the epidural space.
An unpaired T-test was used to evaluate the differences between the variables observed between the trainees and the experts.
Results
All the participants completed their task. Observation of the attentional heat map and the gaze plot showed different gaze dispersion between experts and novices (Figure 3). Expert anesthesiologists spent more time fixating a more specific target location (eg: the point of the epidural needle rather than the syringe’s barrel) whilst novices split their attention between tracking their tools and the target location.
 |
Figure 3 Gaze behavior. Typical novice’s (A) and expert’s (B) gaze plots and novice’s (C) and expert’s (D) heatmap. |
Results are shown in Table 1. The mean total duration of fixations during needle insertion and advancement and catheter introduction was lower in experts than trainees (respectively, P<0.05 and P<0.05). During the insertion of the epidural catheter the mean fixation count was greater in experts vs trainees (P<0.05). The mean duration of the epidural procedure was greater with trainees. (P<0.05).
 |
Table 1 Eye-Tracking Metrics. Values are Given as Mean (SD) |
Discussion
It is commonly believed that there is a difference in the cognitive and motor skills of physicians depending on how experienced they are. Eye-tracking methodology has been used to identify gaze control parameters that differentiate novices from experts but, to the best of our knowledge, this is the first eye-tracking study on an anesthesia technical skill. Our results are consistent with that obtained in a surgical setting,2,5,6 which showed that experienced surgeons spent more time fixating on a target location, whereas novice surgeons fragmented their attention between tracking their tools and the target site. These findings are however in contrast to those of another study7 where experts were found to take much longer to complete the simulated surgical procedure compared to novices and were also found to make more errors. This was, however, most likely due to the experts being less experienced with the virtual reality trainer simulator than their novice colleagues. In our case, such a bias would have been highly unlikely, since both the groups had never previously used the epidural simulator and the environmental conditions of epidural simulation were very realistic without the need to use virtual reality.
In our simulation study, the expert anesthesiologists had an overall shorter duration of fixations during the epidural procedure, and spent more time fixating a more specific target location such as the point of the epidural needle rather than the syringe’s barrel, whilst novices split their attention between tracking their tools and the target location.
The ability of eye tracking to identify such a difference in gazing during the epidural procedure supports the idea that gaze behavior differences found between experts and novices may be fundamental in helping to guide the future in the development of training and assessment programs.
When comparing gaze behavior between expert and novice users, experts make more careful observations, have a deeper cognitive processing and demonstrate less anticipation, together with more local processing and engagement with the task than novices.8 Indeed, experts make more careful observations and have deeper cognitive load of the stimulus, and this suggests that they focus more on the details.8
We recognize that the limitations of our study are its observational nature and the relatively small sample involved, and certainly, further work is required to fully explore the applications of eye-tracking and gaze behavior in this anesthesia setting. However, we believe that our preliminary results could lay the groundwork for the potential use of gaze patterns as an early warning system to novice-type gaze behavior, thereby reducing clinical errors.
Recent papers focused on learning and safety during the execution of neuraxial techniques by studying applied forces using devices which detect the pressure variations.9,10
Gaze behavior also focus on learning and safety, since it could be used not only to create assessment tools and training programs for clinicians, but also to improve technique with a shortened learning curve. A replay of the eye movements of experts, superimposed on the screen showing the visualization, could be used to model the eye movements of novices. In this way, novices may learn on what and in which order to focus.
In summary, this preliminary research has demonstrated different gaze patterns between experts, who spent more time fixating a more specific target location, and trainees, who split their attention between tracking their tools and other different areas, when performing a simulated epidural technique.
Data Sharing Statement
The data used to support the findings of this study are available from the corresponding author upon request.
Acknowledgment
We thank prof G Capogna (Director of EESOA Maternal Neonatal Simulation Center) for his assistance and for comments on the manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
LD is Marketing Analysis Solutions Manager and AD is Chief Technology Officer of SrLabs. The authors report no other potential conflicts of interest for this work.
References
1. Konrad C, Schüpfer G, Wietlisbach M, Gerber H. Learning manual skills in anesthesiology: is there a recommended number of cases for anesthetic procedures? Anesth Analg. 1998;86(3):
2. Tien T, Pucher PH, Sodergren MH, Sriskandarajah K, Yang GZ, Darzi A. Eye tracking for skills assessment and training: a systematic review. J Surg Research. 2014;191(1):
3. Khan RS, Tien G, Atkins MS, Zheng B, Panton ON, Meneghetti AT. Analysis of eye gaze: do novice surgeons look at the same location as expert surgeons during a laparoscopic operation? Surg Endoscopy. 2012;26(12):
4. Capogna G, Coccoluto A, Capogna E, Del Vecchio A. Objective evaluation of a new epidural simulator by the compuflo® epidural instrument. Anesth Res Pract. 2018;2018:4710263. doi:10.1155/2018/4710263
5. Wilson M, McGrath J, Vine S, Brewer J, Defriend D, Masters R. Psychomotor control in a virtual laparoscopic surgery training environment: gaze control parameters differentiate novices from experts. Surg Endosc. 2010;24(10):
6. Harvey A, Vickers JN, Snelgrove R, Scott MF, Morrison S. Expert surgeon’s quiet eye and slowing down: expertise differences in performance and quiet eye duration during identification and dissection of the recurrent laryngeal nerve. Am J Surg. 2014;207(2):
7. Zheng B, Tien G, Atkins SM, et al. Surgeon’s vigilance in the operating room. Am J Surg. 2011;201(5):
8. Gegenfurtner A, Lehtinen E, Säljö R. Expertise differences in the comprehension of visualizations: a meta-analysis of eye-tracking research in professional domains. Ed Psychol Rev. 2011;23(4):523–552. doi:10.1007/s10648-011-9174-7
9. Tesei M, Saccomandi P, Massaroni C, et al. A cost-effective, non-invasive system for pressure monitoring during epidural needle insertion: design, development and bench tests. Conf Proc IEEE Eng Med Biol Soc. 2016;2016:194–197. doi:10.1109/EMBC.2016.7590673
10. Carassiti M, Mattei A, Quarta R, et al. A new pressure guided management tool for epidural space detection: feasibility assessment on a simulator. Artif Organs. 2017;41(12):E320–E325. doi:10.1111/aor.13007
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
