Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 15
Novel versus Traditional Inspiratory Muscle Training Regimens as Home-Based, Stand-Alone Therapies in COPD: Protocol for a Randomized Controlled Trial
Authors Formiga MF , Dosbaba F , Hartman M , Batalik L , Plutinsky M, Brat K , Ludka O, Cahalin LP
Received 5 June 2020
Accepted for publication 11 August 2020
Published 11 September 2020 Volume 2020:15 Pages 2147—2155
DOI https://doi.org/10.2147/COPD.S266234
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Magno F Formiga,1 Filip Dosbaba,2 Martin Hartman,2 Ladislav Batalik,2 Marek Plutinsky,3,4 Kristian Brat,3,4 Ondrej Ludka,4 Lawrence P Cahalin5
1Departamento de Fisioterapia, Universidade Estadual da Paraíba, Campina Grande, PB, Brazil; 2Department of Rehabilitation, University Hospital Brno, Brno, Czech Republic; 3Department of Respiratory Diseases, University Hospital Brno, Brno, Czech Republic; 4Faculty of Medicine, Masaryk University, Brno, Czech Republic; 5Department of Physical Therapy, University of Miami – Miller School of Medicine, Coral Gables, FL, USA
Correspondence: Filip Dosbaba; Ladislav Batalik
Department of Rehabilitation, University Hospital Brno, Jihlavska 20, Brno 62500, Czech Republic
Email [email protected]; [email protected]
Background: Subjects with COPD frequently develop considerable weakness and deconditioning of the inspiratory musculature, which can be corrected with inspiratory muscle training (IMT). While rehabilitation centers may be able to provide IMT as part of the rather complex management of COPD, there is currently a lack of rehabilitation services in the Czech Republic. Remote IMT may then benefit subjects with COPD who are unable to attend or do not have access to rehabilitation programs. We aim at evaluating the utility of the test of incremental respiratory endurance (TIRE) as an at-home IMT method in subjects with COPD, while comparing the effectiveness of this novel training approach to the outcomes of traditional, threshold loading IMT protocols.
Methods/Design: This prospective, randomized controlled trial will comprise 8 weeks of at-home IMT sessions with remote supervision followed by 4 months of unsupervised, independent IMT. Eligible subjects will be randomly assigned to one of the following three distinct home-based IMT protocols: (1) TIRE, (2) Threshold loading, and (3) Sham training. Subjects allocated to the TIRE group will train once daily using an advanced IMT electronic system (PrO2), while the other two groups will receive threshold devices. Study outcomes will include measures of inspiratory muscle strength and endurance, pulmonary function, COPD-specific symptomatology, functional exercise capacity, surrogate markers of mortality risk, mental health status and health-related quality of life.
Discussion: While we acknowledge the value of threshold loading IMT protocols, we believe that the TIRE training method has the potential to provide additional clinical benefits in COPD given its sophisticated remote tracking system and ability to modulate all aspects of muscular performance, including not only strength but also endurance, power and work capacity, allowing users to achieve considerably higher inspiratory pressures throughout the full range of inspiration when compared to other more traditionally used IMT methods.
Keywords: chronic obstructive pulmonary disease, pulmonary rehabilitation, telemedicine, quality of life, inspiratory muscle training, test of incremental respiratory endurance
Introduction
Chronic obstructive pulmonary disease (COPD) is a highly prevalent and complex disease characterized by a progressive decline in lung function, which is not fully reversible.1 The prevalence of COPD is increasing worldwide, with high rates of mortality and morbidity impacting the quality of life of affected subjects.2 Despite optimal bronchodilator therapy, many patients suffer from intolerance of physical exercise and dyspnea of a multifactorial nature.3 In the Czech Republic, approximately 800,000 people are estimated to have COPD (7–8% of the country’s entire population).4
Pulmonary rehabilitation represents one of the most important and effective therapies in COPD. It is aimed at restoring function and has been shown to increase exercise tolerance, reduce dyspnea and improve quality of life in participants.5 While pulmonary rehabilitation is a central component in the rather complex management of COPD, there is currently a lack of centers able to provide appropriate rehabilitation services in the Czech Republic. Therefore, a great discrepancy between the theoretical need and the actual availability of these programs exists.2,6 The reasons for the absence of such outpatient programs in the Czech Republic include the lack of both experience and interest of health insurance companies in the context of secondary prevention programs, as well as unavailability of an adequate number of healthcare facilities specialized in the management of chronic respiratory conditions.6 In the United States (US), adherence to pulmonary rehabilitation is extremely low among subjects with COPD, despite all its benefits.7 This can be explained in part by the fact that pulmonary rehabilitation programs are typically hospital-based, which limits accessibility. Travel and transport issues have been cited as being the most common obstacles for program attendance.7,8 Home-based therapies like inspiratory muscle training (IMT) are then a promising approach found to yield beneficial effects on exercise capacity and exertional dyspnea in subjects with COPD.9
The Test of Incremental Respiratory Endurance (TIRE) is a novel method to assess the inspiratory musculature of subjects diagnosed with COPD. The TIRE has recently been validated for use in this population, providing reliable measures of maximal inspiratory pressure (MIP), sustained maximal inspiratory pressure (SMIP) and inspiratory duration (ID).10 The same method can be used as a more comprehensive IMT regimen which has not been fully examined in COPD.11
IMT has been shown to produce significant clinical benefits in obstructive lung disease.12 The positive effects of IMT in COPD make it an attractive therapy due to its easy applicability. Optimizing IMT methods to elicit the most functional improvements in COPD is therefore of significant importance.13 Traditional threshold loading IMT has important limitations, which are a limited workload (a maximal resistance of −41 cmH2O or less in such devices) and a limited inspiratory duration. By its nature, the TIRE promises to be a more efficient training tool because it allows patients to achieve considerably higher inspiratory pressures (up to −300 cmH2O) throughout the full range of inspiration, as shown in Figure 1, adapted from Cahalin et al.14
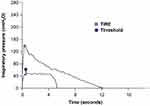 |
Figure 1 Comparison of the maximal inspiratory effort slopes obtained via the TIRE method and traditional inspiratory muscle assessment utilizing a threshold device. |
The main objective of this trial is to fully evaluate the utility of the TIRE as an IMT method in subjects with COPD, while comparing the effectiveness of this novel training approach to the outcomes of traditional, threshold loading IMT protocols. We hypothesize that, as a home-based stand-alone rehabilitative therapy, TIRE might be superior to traditional IMT in improving inspiratory muscle performance and COPD-related outcomes.
Methods/Design
Study Design
The intended study will include two treatment groups and one sham intervention group in a 1:1:1 ratio. All subjects will undergo a certain type of IMT regardless of group assignment, which will be performed via two different devices. The study will be conducted in cooperation with the Rehabilitation Department and the Department of Respiratory Diseases of University Hospital Brno. The trial will comprise an 8-week at-home training period with remote supervision followed by 4 months of unsupervised, independent respiratory training. The study will be prospective, controlled, and randomized. The patients will be assigned 1:1:1 using a computerized random allocation sequence, which will be done through the use of opaque, sealed and numbered envelopes. This process will be administrated by a skilled, independent expert at the hospital center. They will also collect and store informed consents, questionnaires and other trial information. Electronic data will be stored in the hospital’s private cloud and backed up to a flash drive. All data will be processed and backed up according to the currently valid General Data Protection Regulations. Although some healthcare providers will need to be informed about their patient’s group assignment, subjects will be asked not to disclose their group assignment to the physician performing initial and final examinations, who will be blinded. The overall training regimen and data collection time points are shown in Figure 2.
 |
Figure 2 Outline of study design. Subjects are assigned to one of three home-based inspiratory muscle training groups and expected to train for 8 weeks. |
All subjects will be recruited from the outpatient services of the Department of Respiratory Diseases at the University Hospital Brno. Subjects are expected to meet the following criteria: (a) subjects over the age of 40 with a clinical and functional diagnosis of COPD according to the Global Initiative of Chronic Obstructive Lung Disease (GOLD) guidelines – stages I to IV, (b) evidence of inspiratory muscle weakness, defined as a MIP ≤ 80 cmH2O and a SMIP ≤ 427 PTU (pressure time units),15 (c) ability to operate a computer, tablet or smartphone independently and follow the training instructions, (d) clinical stability with no history of infections or exacerbation of respiratory symptoms for at least two months prior to study enrollment, and (e) non-participation in exercise programs in the past 12 months. The above criteria for inspiratory muscle weakness were chosen based upon a previous study by our research group, which found a SMIP value of 427 PTU to be equivalent to the MIP cut-off value of 80 cmH2O for stratification of clinically important inspiratory muscle impairment proposed by the ATS/ERS statement on respiratory muscle testing.15,16
We will exclude subjects with history of lung surgery, lung cancer, as well as individuals with any diagnosed cognitive (ie, Mini Mental State Examination score <24), orthopedic, neurological or neuromuscular disorders that might prevent them from appropriately performing the required physical tests and/or completing the study questionnaires. Subjects will not be excluded based upon their current bronchodilator regimen. If subjects experience acute exacerbations or respiratory infections during the training period, they will be examined by a pneumologist who will decide whether the participant should continue with the training or not. In the event that losses to follow-up or dropouts are observed, we will perform an intention-to-treat analysis.
Data will be collected in the following order: a) spirometry and body plethysmography, b) walking test, c) questionnaires, and d) inspiratory muscle performance via the TIRE. Subjects will be randomly divided into groups and familiarized with the proposed training regimens and their respective devices.
Training Description
Eligible subjects will be randomly assigned to one of the following three distinct home-based IMT protocols: (1) TIRE, (2) Traditional (Threshold loading IMT), and (3) Sham (ie, Low Resistance). All subjects will undergo 8 weeks of daily unsupervised IMT using either a PrO2 device (Design Net, Smithfield, USA) or Threshold device at home. Table 1 presents a summary of the distinctive training characteristics per study group. All training modalities require the subjects to be seated and wearing a nose clip while performing the required breaths. Subjects will be instructed on their respective training procedures and complete their first training session in the presence of a research team member upon enrollment. Regardless of training method, subjects will be instructed to fill in diary cards at the end of each training session, in which they document how many breaths they were able to perform. This information will be later used for compliance assessment. They will be also provided with user guides developed by our research team with detailed instructions regarding equipment set-up, training protocol and contact information. In addition, subjects will receive weekly phone calls from week 0 to week 8 to encourage compliance and adherence to the study protocol, to address any subject questions or concerns, and to collect information regarding their current symptomatology (Figure 2).
 |
Table 1 Proposed Training Characteristics per Study Group |
Group 1 – TIRE IMT
The TIRE training regimen will involve the use of a tablet provided to assigned subjects with the training software installed and a PrO2 device through which they will train. The software allows subjects to track their inspiratory muscle performance via real-time graphic representations of their efforts as training progresses. Training will consist of six levels (A-F) with six inspirations at each level for up to 36 breaths per session. Pre-set recovery times between breaths decrease as subjects advance each level from 60 seconds at level A to 50, 40, 30, 20 and 10 seconds at levels B to F, respectively. TIRE data will be stored in the tablet and automatically synced to account on cloud-based online platform for subsequent interrogation and data retrieval. Each participant will get his or her own login and password to account. The research team will have access to the accounts of all subjects. This feature makes the TIRE system a powerful resource to ensure compliance and remotely track adherence to study protocol.
Before every training session, subjects will be required to complete one maximal and sustained inspiratory effort from which the training is based on for that day. This effort will be recorded on the software and visually redrawn on the tablet screen to a training template set at 50% of the entire effort. Subjects will be required to match or exceed the on-screen training template for their efforts to be considered successful, achieving pressures of at least 90% of the redrawn MIP and area under the curve (ie, SMIP). Although the achievement of the 50% pre-set training template is sufficient to allow for training continuation, subjects are instructed to perform maximal maneuvers from RV to TLC, not only matching but exceeding the effort requirement whenever possible. After each successful breath, a countdown clock will be trigged, and the subject will have to wait to perform the next breath following the pre-set recovery time for that level. If at least 90% of the redrawn MIP and SMIP are not achieved, the subject will receive a prompt that they had failed to generate the required pressures and will be automatically provided with two options: either terminate or continue the training. Subjects will be instructed to terminate the session in case of two consecutive failed inspiratory efforts. It is important to note that subjects will be instructed not to expire into the device. They will only use the device when prompted by the software to inspire at which time they will place the mouthpiece of the device in their mouth and perform the required sustained inspiratory effort.
Group 2 – Threshold IMT
Subjects assigned to the threshold loading training regimen will receive a traditionally used Threshold inspiratory muscle trainer (Threshold IMT; Philips Respironics, USA). This device features a one-way spring-loaded valve at one end and a mouthpiece on the other through which subjects will be required to breathe in hard enough to overcome the resistance provided by the spring-loaded valve, allowing correct inspiration to happen. In other words, air flow is blocked until subjects generate sufficient inspiratory pressure to exceed the device pre-set pressure in cmH2O. The resistance will be set using the device’s adjustable pressure setting which is fixed at 50% of the subject’s MIP at the time of enrollment. The resistance will be readjusted as needed at week 4 to still reflect 50% of their inspiratory muscle strength at that time. Subjects will be coached to perform up to 36 breaths daily using the device. They will be also instructed to complete the training session within a 30-minute period.
Group 3 – Sham IMT (Low Resistance)
The Sham (Low Resistance) training regimen will use the same methods described above for the threshold loading IMT, except for the amount of resistance applied within the device. Subjects will receive a Threshold which has been set to its minimal resistance, which is 9 cmH2O. Again, subjects will be instructed to perform up to 36 breaths daily using the device within a 30-minute period.
Outcome Measures
Key outcome measures in the trial will be assessed at baseline and 8 weeks post training start date at the University Hospital Brno. TIRE and COPD Assessment Test data will also be collected during the second study visit. Data collection per study visit will take approximately 90 minutes.
The primary outcome measure will be SMIP, which will be obtained along with MIP and ID in every subject using the PrO2 device, an electronic pressure manometer which utilizes wireless technology to connect to a tablet containing the TIRE software.15 The software provides the user with a real-time graphic representation as they perform the required inspiratory maneuver, as shown in Figure 3. The PrO2 has a 2 mm leak which provides a set resistance to inspiratory flow and avoids glottal closure during maximal inspiratory effort. Subjects will be instructed to exhale completely and then forcefully breathe in through the device generating as much pressure as possible within 1 to 2 seconds of inspiration and continue to inhale deeply for as long as possible. SMIP will be measured from residual volume (RV) to total lung capacity (TLC) and represents the area under the curve in PTU, while MIP will be recorded in cmH2O and represents the highest pressure generated during inspiration from RV. ID will document the total duration of full inspiration per trial in seconds. A single assessment session will consist of 3 to 5 sequential trials with rest intervals of 60 seconds between efforts. The greatest SMIP will be used to identify the best of the repeated trials within the session, providing the MIP and SMIP values to be documented and used for study purposes. All inspiratory maneuvers will be performed with the subjects seated in a chair and wearing nose clips according to American Thoracic Society (ATS) standards on respiratory muscle testing.16
Other key outcome measures will include pulmonary function tests which comprise post-bronchodilator spirometry using SpiroScout® and whole-body plethysmography using the PowerCube® Body+ (Ganshorn, Niederlauer, Germany) following European Respiratory Society - ERS/ATS standards,17 providing measures of forced expiratory volume in the first second (FEV1), forced vital capacity (FVC), inspiratory capacity (IC), RV and TLC, obtained 15–20 min after 400µg salbutamol will administered via a metered dose inhaler through a spacer. Functional exercise capacity will be determined using the six-minute walk test (6MWT), which will be performed as recommended by ERS/ATS guidelines.18 The severity of dyspnea, mental health status and health-related quality of life of the subjects will be assessed via the modified Medical Research Council (mMRC) dyspnea scale, the Hospital Anxiety and Depression scale (HADS) and the St. George’s Respiratory Questionnaire, respectively.19–21 The impact of disease-specific symptoms on the health status of the subjects will be quantified by the CAT,22 while comorbidity burden will be assessed using the Charlson Comorbidity Index.23 The BODE index will be also calculated and will serve as a surrogate marker of mortality risk in COPD.24 The above scales, questionnaires and indices will use point-based grading systems with higher total scores indicating more severe conditions. Occurrence of adverse events and reasons for early termination of trial will be evaluated.
Data regarding medications and past medical history will be extracted from each individual’s electronic medical record. A full tobacco history will be obtained at baseline, with subjects being asked to report the total number of years smoked, average number of cigarettes smoked per day, and current smoking status. Finally, subjects will be provided with a 5-item self-completed questionnaire developed by our research team that will measure their satisfaction with the intervention they received and the study in general. The items will be presented in the form of statements to which subjects will be asked to respond using a 1–5 Likert scale (“strongly agree”, “agree”, “not sure”, “disagree”, and “strongly disagree”).
Sample Size
We performed a power analysis based on the report of previous studies on TIRE measures. Normative TIRE data yielded effect sizes ranging between 0.50–1.00 when comparing SMIP to different age groups.25 A meta-analysis for inspiratory muscle strength demonstrated a significant summary effect size of 0.68 (95% CI 0.54–0.82; p = 0.001) for MIP.26 Thus, we believe that an effect size of about 0.75 is a good estimate. We examined the number of subjects necessary to achieve such an effect size using Portney & Watkins test and concluded that the sample size needed for our statistical analyses is of at least 12 subjects in each of the three groups with 2 degrees of freedom and a power of 0.9 with an alpha level of 0.05. Subjects that are eventually excluded or decide to drop out will be replaced with new enrollees to ensure completion of at least 12 subjects per group.
Statistical Analysis
Baseline characteristics of the study sample will be analyzed and summarized using descriptive statistics. Differences in recorded variables between the three groups at baseline, and after four and eight weeks of training will be analyzed by a mixed-design analysis of variance and multiple linear regressions. Training compliance information will be expressed as a percentage. Statistical significance will be set at an alpha-level of 0.05. All analyses will be performed with IBM SPSS Statistics 24 (Armonk, New York, USA 10,504–1722) and Statistica 12 (TIBCO Software, INC Palo Alto, US).
Trial Status
This study will be performed in accordance with the World Medical Association Declaration of Helsinki and was approved by the Ethical Committee of the University Hospital Brno, Czech Republic. This trial follows the SPIRIT 2013 checklist standards of reporting trials and is registered at ClinicalTrials.gov with identifier: NCT04415788.
Discussion
Patients with COPD commonly develop significant deterioration in exercise capacity in association with weakness and deconditioning of the respiratory muscles. Particular impairment has been described in inspiratory muscle performance reflected by decreases in MIP.27,28 Whereas inspiratory muscle function in COPD has mostly been described in terms of inspiratory muscle strength, the day-to-day relevance of measures like MIP is debatable. In fact, studies suggest greater clinical, perceptive, functional, psychological and prognostic values in the assessment of single-breath work capacity when compared to the evaluation of inspiratory muscle strength alone in COPD.15,29,30 Besides the traditionally studied measure of MIP, the TIRE provides values of single-breath work capacity such as SMIP and ID, allowing for a more profound assessment of the musculature involved with inspiration. Moreover, the TIRE can serve as a novel training method likely to result in better clinical outcomes in the COPD population.
While we acknowledge the value of traditional IMT protocols, which use Threshold devices, we believe that the TIRE training has the potential to provide added clinical benefits since it is able to modulate all aspects of muscular performance, including strength, endurance and work capacity. The real-time biofeedback and a training template that encourages the generation of higher pressures throughout the entire inspiration are also unique and superior features of the TIRE training, which facilitate a more controlled breathing pattern and possibly improved gas exchange during and post-training.
Additionally, we will be able to remotely and electronically track training compliance of the subjects assigned to the TIRE protocol, a distinct and important characteristic of this training approach that might allow us to reliably assess the subject’s adherence to study protocol, unlike the other groups whose training compliance will be self-reported. We believe that more accurate conclusions as to changes observed in clinical outcomes from baseline can be drawn when actual compliance is accounted for; therefore, the TIRE device and software is a promising tool.
Whereas other inspiratory flow resistive loading (IRFL) techniques and devices exist, from simple dial-based equipment such as the Pflex (Philips Respironics, the Netherlands) to more sophisticated electronic instruments like the POWERbreathe (POWERbreathe International Ltd, United Kingdom), the TIRE method implemented via the PrO2 device is novel as it provides original features not available in other training approaches. The TIRE offers the possibility of assessing and training the unique SMIP, which can be defined as single-breath inspiratory work capacity, reflecting the ability of the inspiratory muscles to maintain force over time through a great resistive load imposed by a fixed 2 mm inspiratory orifice.10,15 Other distinctive characteristic of the TIRE is its modern remote tracking system and cloud-based online platform, making the PrO2 an attractive alternative to devices such as the POWERbreathe which are currently unable to remotely interrogate and retrieve data as training happens. Finally, due to its fixed flow resistive load, the TIRE allows subjects to produce considerably higher pressures for longer periods of time (ie, total duration of inspiration can exceed 10 seconds), possibly resulting in greater improvements in inspiratory muscle endurance and work capacity.
Remote alternatives to traditional rehabilitation programs are important for subjects with COPD who are unable (or not willing) to attend such services. In 2015, the ERS/ATS published a political statement in which they commit to the promotion and expansion of home-based pulmonary rehabilitation.31 Meta-analyses have shown that telerehabilitation technologies are of great importance in managing COPD as they can improve respiratory muscle pressures, functional lung capacity and the quality of life of those who are treated remotely.32,33 Several telemedicine benefits have been reported following the rehabilitation of patients with other diseases.34
In conclusion, the main objective of this study will be to fully evaluate the utility of TIRE as an at-home inspiratory muscle training method in subjects with COPD, while comparing the effectiveness of this novel training approach to the outcomes of more traditional IMT protocols. We hypothesize that, as a home-based stand-alone rehabilitative therapy, TIRE will be superior to traditional, threshold loading IMT in improving measures of inspiratory muscle performance, pulmonary function, dyspnea, functional exercise capacity, overall and mental health, health-related quality of life and surrogate markers of mortality risk in COPD. We expect to publish the findings of this investigation in due course.
Abbreviations
ATS, American Thoracic Society; CAT, COPD assessment test; COPD, chronic obstructive pulmonary disease; ERS, European Respiratory Society; FEV1, forced expiratory volume in the first second; FVC, forced vital capacity; GOLD, Global Initiative of Chronic Obstructive Lung Disease; HADS, Hospital Anxiety and Depression Scale; IC, inspiratory capacity; ID, inspiratory duration; IMT, inspiratory muscle training; MIP, maximal inspiratory pressure; mMRC, modified Medical Research Council; N, sample size; PTU, pressure time units; RV, residual volume; SMIP, sustained maximal inspiratory pressure; TIRE, test of incremental respiratory endurance; TLC, total lung capacity; US, United States; 6MWT, six-minute walk test.
Ethics Approval and Consent to Participate
This study is approved by The Ethical Committee University Hospital Brno, Czech Republic (Reference number: 01-020420/EK). Subjects will sign a written informed consent prior to enrolment.
Disclosure
Marek Plutinsky reports personal fees from Boehringer Ingelheim, Berlin Chemie, and CSL Behring, outside the submitted work. The authors report no other potential conflicts of interest in this work.
References
1. Figueiredo RI, Azambuja AM, Cureau F, Sbruzzi G. Inspiratory muscle training in COPD. Respir Care. 2020;65:
2. Singh D, Agusti A, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: the GOLD science committee report 2019. Eur Respir J. 2019;53:1900164. doi:10.1183/13993003.00164-2019
3. Sundh J, Ekström M. Persistent disabling breathlessness in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2016;11:2805–2812. doi:10.2147/COPD.S119992
4. Institute of Health Information and Statistics of the Czech Republic. Health statistics annual of the Czech Republic 2017. (Ústav zdravotnických informací a statistiky ČR. Zdravotnická ročenka České republiky 2017). Available from: http://www.uzis.cz/publikace/zdravotnicka-rocenka-ceske-republiky-2017
.
5. McCarthy B, Casey D, Devane D, Murphy K, Murphy E, Lacasse Y. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2015;2:CD003793. doi:10.1002/14651858.CD003793.pub3
6. Spruit MA, Pitta F, Garvey C, et al. Differences in content and organisational aspects of pulmonary rehabilitation programmes. Eur Respir J. 2014;43:1326–1337. doi:10.1183/09031936.00145613
7. Bhatt SP. It’s time to rehabilitate pulmonary rehabilitation. Ann Am Thorac Soc. 2019;16(1):55–57. doi:10.1513/AnnalsATS.201809-641ED
8. Keating A, Lee A, Holland AE. What prevents people with chronic obstructive pulmonary disease from attending pulmonary rehabilitation? A systematic review. Chron Respir Dis. 2011;8:89–99. doi:10.1177/1479972310393756
9. Bavarsad MB, Shariati A, Eidani E, Latifi M. The effect of home-based inspiratory muscle training on exercise capacity, exertional dyspnea and pulmonary function in COPD patients. Iran J Nurs Midwifery Res. 2015;20(5):613–618. doi:10.4103/1735-9066.164588
10. Formiga MF, Roach KE, Vital I, et al. Reliability and validity of the test of incremental respiratory endurance measures of inspiratory muscle performance in COPD. Int J Chron Obstruct Pulmon Dis. 2018;13:1569–1576. doi:10.2147/COPD.S160512
11. Cahalin LP, Arena R. Novel methods of inspiratory muscle training via the Test of Incremental Respiratory Endurance (TIRE). Exerc Sport Sci Rev. 2015;43:84–92. doi:10.1249/JES.0000000000000042
12. Beaumont M, Forget P, Couturaud F, Reychler G. Effects of inspiratory muscle training in COPD patients: a systematic review and meta-analysis. Clin Respir J. 2018;12:2178–2188. doi:10.1111/crj.12905
13. Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188:13–64. doi:10.1164/rccm.201309-1634ST
14. Cahalin LP, Arena R, Guazzi M, et al. Inspiratory muscle training in heart disease and heart failure: a review of the literature with a focus on method of training and outcomes. Expert Rev Cardiovasc Ther. 2013;11:161–177. doi:10.1586/erc.12.191
15. Formiga MF, Vital I, Urdaneta G, Campos MA, Cahalin LP. Beyond inspiratory muscle strength: clinical utility of single-breath work capacity assessment in veterans with COPD. Respir Med. 2019;147:13–18. doi:10.1016/j.rmed.2018.12.012
16. American Thoracic Society. ATS/ERS statement on respiratory muscle testing. Am J Respir Crit Care Med. 2002;166:518–624. doi:10.1164/rccm.166.4.518
17. Miller MR, Hankinson JA, Brusascoet TS, et al. Standardisation of spirometry. Eur Respir J. 2005;26:319–338. doi:10.1183/09031936.05.00034805
18. Holland AE, Spruit MA, Troosters T, et al. An official European Respiratory Society/American Thoracic Society technical standard: field walking tests in chronic respiratory disease. Eur Respir J. 2014;44:1428–1446. doi:10.1183/09031936.00150314
19. Barr JT, Schumacher GE, Freeman S, LeMoine M, Bakst AW, Jones PW. American translation, modification, and validation of the St. George’s Respiratory Questionnaire. Clin Ther. 2000;22:1121–1145. doi:10.1016/S0149-2918(00)80089-2
20. Hajiro T, Nishimura K, Tsukino M, Ikeda A, Koyama H, Izumi T. Analysis of clinical methods used to evaluate dyspnea in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998;158:1185–1189. doi:10.1164/ajrccm.158.4.9802091
21. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi:10.1111/j.1600-0447.1983.tb09716.x
22. Jones PW, Harding G, Berry P, Wiklund I, Chen WH, Leidy K. Development and first validation of the COPD assessment test. Eur Respir J. 2009;34:648–654. doi:10.1183/09031936.00102509
23. Charlson ME, Pompei P, Ales KL, McKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi:10.1016/0021-9681(87)90171-8
24. Celli BR, Cote CG, Marin JM, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med. 2004;350:1005–1012. doi:10.1056/NEJMoa021322
25. Cahalin LP, Garcia C, Denis TS, et al. Normative values for the test of incremental respiratory endurance (TIRE). Am J Respir Crit Care Med. 2016;193:A6363–A6363.
26. Gosselink R, De Vos J, van den Heuvel SP, Segers J, Decramer M, Kwakkei G. Impact of inspiratory muscle training in patients with COPD: what is the evidence? Eur Respir J. 2011;37(2):416–425. doi:10.1183/09031936.00031810
27. Couillard A, Prefaut C. From muscle disuse to myopathy in COPD: potential contribution of oxidative stress. Eur Respir J. 2005;26:703–719. doi:10.1183/09031936.05.00139904
28. Gosselink R. Breathing techniques in patients with chronic obstructive pulmonary disease (COPD). Chron Respir Dis. 2004;1:163–172. doi:10.1191/1479972304cd020rs
29. Formiga MF, Vital I, Urdaneta G, Balestrini K, Cahalin LP, Campos MA. The BODE index and inspiratory muscle performance in COPD: clinical findings and implications. SAGE Open Med. 2018;6:2050312118819015. doi:10.1177/2050312118819015
30. Formiga MF, Vital I, Urdaneta G, et al. Higher serum levels of systemic inflammatory markers are linked to greater inspiratory muscle dysfunction in COPD. Clin Respir J. 2019;13:247–255. doi:10.1111/crj.13006
31. Dong J, Li Z, Luo L, et al. Efficacy of pulmonary rehabilitation in improving the quality of life for patients with chronic obstructive pulmonary disease: evidence based on nineteen randomized controlled trials – a systematic review and meta-analysis. Int J Surg. 2020;73:78–86. doi:10.1016/j.ijsu.2019.11.033
32. Weitong L, Yalou P, Aifeng M, Zhi X, Xu G. Effectiveness of pulmonary rehabilitation in elderly patients with COPD: a systematic review and meta‐analysis of randomized controlled trials. Int J Nurs Pract. 2019;25:e12745. doi:10.1111/ijn.12745
33. Hong Y, Lee SH. Effectiveness of tele-monitoring by patient severity and intervention type in chronic obstructive pulmonary disease patients: a systematic review and meta-analysis. Int J Nurs Stud. 2019;92:1–15. doi:10.1016/j.ijnurstu.2018.12.006
34. Batalik L, Filakova K, Batalikova K, Dosbaba F. Remotely monitored telerehabilitation for cardiac patients: a review of the current situation. World J Clin Cases. 2020;8(10):1818–1831. doi:10.12998/wjcc.v8.i10.1818
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.