Back to Journals » Vascular Health and Risk Management » Volume 12
Noninvasive FFR derived from coronary CT angiography in the management of coronary artery disease: technology and clinical update
Authors Nakanishi R, Budoff M
Received 18 September 2015
Accepted for publication 29 February 2016
Published 22 June 2016 Volume 2016:12 Pages 269—278
DOI https://doi.org/10.2147/VHRM.S79632
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Daniel Duprez
Rine Nakanishi, Mathew J Budoff
Los Angeles Biomedical Research Institute, Harbor-UCLA Medical Center, Torrance, CA, USA
Abstract: After a decade of clinical use of coronary computed tomographic angiography (CCTA) to evaluate the anatomic severity of coronary artery disease, new methods of deriving functional information from CCTA have been developed. These methods utilize the anatomic information provided by CCTA in conjunction with computational fluid dynamics to calculate fractional flow reserve (FFR) values from CCTA image data sets. Computed tomography-derived FFR (CT-FFR) enables the identification of lesion-specific drop noninvasively. A three-dimensional CT-FFR modeling technique, which provides FFR values throughout the coronary tree (HeartFlow FFRCT analysis), has been validated against measured FFR and is now approved by the US Food and Drug Administration for clinical use. This technique requires off-site supercomputer analysis. More recently, a one-dimensional computational analysis technique (Siemens cFFR), which can be performed on on-site workstations, has been developed and is currently under investigation. This article reviews CT-FFR technology and clinical evidence for its use in stable patients with suspected coronary artery disease.
Keywords: fractional flow reserve, coronary computed tomographic angiography, FFRCT, cFFR
Introduction
Fractional flow reserve (FFR) is considered as one of the diagnostic methods for guiding decision making to identify patients who would benefit from revascularization.1–4 Current guidelines serve FFR as a class IIa recommendation for treatment decisions for coronary revascularization or medical care.5,6
Noninvasive diagnostic modalities are used in individuals with suspected coronary artery disease (CAD) to identify patients who should undergo invasive coronary angiography (ICA). This conceptual scheme, in terms of diagnostic decision making for suspected CAD, is widely accepted and used in clinical settings7 to reduce medical costs and avoid the risks of ICA. However, a recent study of the National Cardiovascular Data Registry (NCDR) with respect to the clinical impact of noninvasive imaging tests on the use of ICA demonstrated a low diagnostic yield of noninvasive tests to detect significant CAD in patients undergoing ICA. Of the 661,063 patients undergoing elective ICA, 64% of them had prior noninvasive testing (78% were stress single photon emission computed tomography-myocardial perfusion image [SPECT-MPI], 20% other stress testing, and 2% underwent coronary computed tomographic angiography [CCTA]) prior to ICA.8 While 81% of patients showed abnormal noninvasive findings before ICA, only 45% of patients had obstructive CAD with >50% stenosis by ICA.8 Similarly, in a recent European multicenter study designed to assess the relative accuracy of commonly used noninvasive imaging tests, significant CAD was found in only 29% of patients at ICA, with significant CAD defined as ≥70% stenosis in a major coronary artery, ≥50% stenosis in a left main trunk, or the presence of invasive FFR ≥0.80 with an intermediate lesion (30%–70% stenosis).9 This low diagnostic yield of noninvasive functional test raises suspicion on the results of diagnostic tests among physicians.
Clinical need for CT-derived FFR
CCTA is a useful, noninvasive modality to assess patients with suspected CAD and can reliably identify the presence or absence of CAD. To date, numerous multicenter studies have demonstrated the high diagnostic yield of CCTA to identify CAD stenosis by ICA.10–12 However, coronary stenosis severity does not always correlate well with the functional severity of CAD detected by invasive FFR, with poor correlation between anatomical and functional significance of coronary lesions. In the FAME study, Tonino et al13 found that 20% showed FFR >0.80 among 70%–90% of severe ICA stenoses and 65% had FFR >0.80 among 50%–69% of moderate ICA stenosis. This observation was also shown in a study of 79 patients undergoing CCTA, in which the diagnostic accuracy of ≥50% anatomical stenosis to identify invasive FFR ≤0.8 was only 49%.14 In a recent large study of 2,986 patients by Toth et al,15 quantitative coronary angiography was used to assess angiographic diameter stenosis (DS), and FFR was used to evaluate lesion-specific drop. The concordance between DS ≥50% and FFR ≤0.80 was a modest 64%.15 A higher cutoff value of DS ≥70% did not improve the diagnostic performance for the determination of FFR ≤0.8 compared to DS ≥50%.15 In a study of 99 symptomatic patients undergoing both CCTA and ICA with FFR, quantitative CCTA stenosis also showed only modest correlation between DS% and invasive FFR with R2=0.429.16
Although numerous studies have shown the prognostic value of anatomical stenosis by CCTA,17,18 this misclassification may influence the treatment decision making among patients with suspected CAD and future risks. In a study of 81 patients who underwent both ICA with FFR and CCTA, when invasive FFR ≤0.75 was considered appropriate for revascularization decision making, 30% of patients failed to undergo appropriate revascularization by CCTA guidance due to lack of evidence of functional significance or inappropriate deferral compared to FFR guidance.19 Thus, based on these issues, we may need a new approach after CCTA performance to more accurately identify patients who would benefit from revascularization.
FFR derived from CCTA images is emerging as a novel noninvasive method to evaluate lesion-specific drop of CAD. CT-derived FFR is calculated by processing the same images used for evaluating coronary arteries under resting conditions. The significance of coronary lesions at hyperemic flow condition can be estimated by computational flow modeling, and no adenosine is required. Thus, CT-derived FFR estimates virtual hyperemia for the calculation. Hence, additional image acquisition, radiation exposure, or pharmacological stress during CCTA scanning are not necessary for the computation of FFR from coronary CT.
Currently, there are two methods for calculating FFR from CCTA. The first involves three-dimensional (3D) modeling of the entire coronary tree with computation of FFR values throughout the coronary tree. This is a computationally demanding process and requires off-site supercomputer analysis. Such analysis is known as FFRCT and is available as a web-based service provided by HeartFlow, Inc. (Redwood City, California, USA). FFRCT was approved for clinical use by the US Food and Drug Administration (FDA) in late 2014. A simplified one-dimensional (1D) analysis (cFFR) that can be performed at on-site workstations has been developed by Siemens Healthcare (Forchheim, Germany) but is not yet commercially available. A number of studies have been conducted and reported using the two methods in the past several years.
Technology for CT-derived FFR
The technology for calculating FFR from CCTA involves three main elements: 1) anatomical modeling of coronary arteries, 2) physiological modeling of blood flow, and 3) solution of the governing equations of blood flow on a computer using numerical methods.20 The scientific basis for 3D modeling of FFR has been described in detail by Taylor et al.20 FFRCT analysis involves off-site processing using an FDA-regulated image analysis process and parallel supercomputers. The scientific basis of the 1D analysis is described in the previous study.21 The specific methods utilized in the cFFR technology are described in a study by Itu et al.22
3D modeling: Anatomical models of coronary artery and left ventricular mass derived from CCTA images enable calculation of blood flow in coronary arteries since coronary blood flow under resting conditions is proportional to myocardial mass.23 Left ventricular mass is easily measured with volumetric imaging of the heart; however, scanning the whole heart is essential. The segmentation and 3D modeling of coronary arteries are the most time-consuming processes for calculating FFRCT since these processes are likely to be affected by image quality. Of note, for the 3D method of calculating FFRCT, all available vessels with adequate size including side branches, which are not considered part of the AHA 17 segment coronary model, provide more accurate computations of blood flow distribution. The total resting blood flow computed from the left ventricular myocardial mass and the number and size of the branches in the 3D coronary model are used to estimate coronary blood flow for each vessel. To solve for coronary blood flow, velocity, and pressure, the 3D finite element method is used for FFRCT. The 3D model details the lumen boundary, captures the three components of velocity vectors, and directly accounts for pressure gradients across the stenosis rather than assuming them from idealized loss models as in the 1D method.20
1D modeling: Reduced order models and 1D processing of the image data have been proposed as a method that could be used by physicians or technologists using an on-site workstation.20,24 While this method can facilitate rapid computation of blood flow, this is done by making significant broad assumptions related to how blood flows through arteries. Specifically, the 1D model calculates cFFR using only the cross-sectional area of the vessels, a single axial component of velocity with an assumed profile function, and requires empirical stenosis loss models.25,26
During the measurement of invasive FFR, adenosine is administered to cause maximum coronary hyperemia, thus allowing the evaluation of lesion-causing drop in coronary arteries. For both the 3D and 1D computational analyses of FFR, adenosine administration is not required during CCTA scanning, which is performed under resting conditions. For computation of FFR, the resting microcirculatory resistance is reduced in the computational model to simulate the maximum hyperemic response. Because healthy and diseased vessels adapt to the amount of flow they carry, microcirculatory resistance can be modeled since vessel resistance is inversely proportional to the coronary lumen area of the feeding coronary vessels.27,28
Diagnostic accuracy of CT-derived FFR compared to measured FFR
During the past several years, numerous studies examining the diagnostic performance of both 3D FFRCT and 1D cFFR compared to invasive FFR as the reference standard have been reported.24,29–34
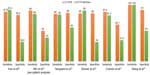
The diagnostic performance of FFRCT and cFFR is summarized in Table 1. Overall, good correlations of both FFRCT and cFFR to invasive FFR were demonstrated ranging between 0.63 and 0.82. All studies have demonstrated that FFRCT and cFFR showed high discrimination in predicting lesion-causing drop by invasive FFR, with area under the curve (AUC) ranging from 0.81 to 0.92.24,29–34 Importantly, compared to CCTA stenosis alone, FFRCT and cFFR improved specificity, while showing similar sensitivity (Figure 1). This evidence may solve the issue of a high false-positive rate by CCTA stenosis alone and potentially reduce unnecessary ICA rates.
  | Table 1 Diagnostic performance of CT-derived FFR |
The diagnostic performance of 3D FFRCT using invasively measured FFR as the reference standard has been evaluated in three prospective, multicenter clinical trials, including >600 patients with blinded core-lab analysis of 1,050 vessels.29–31 Each of these trials (DISCOVER-FLOW, DeFACTO, and NXT) demonstrated high diagnostic performance of FFRCT with significant improvement in diagnostic accuracy and specificity compared to CCTA alone. The most recent NXT study, utilized the latest, updated HeartFlow Analysis software, which has now been cleared for clinical use by the FDA. High CT image quality, in accordance with SCCT guidelines,35 was required, and nitroglycerin was administered in >99% of patients. The determination of CCTA stenosis was by site read in order to best reflect the “real-word” scenario.36 The per-patient diagnostic accuracy of FFRCT was significantly higher for FFRCT (81%) than for CCTA (53%, P<0.001). This was primarily due to a much higher specificity for FFRCT (79%) compared to CT angiography (34%, P<0.001). Sensitivity was similarly high for both FFRCT (86%) and CCTA (94%, P=ns). The correlation between FFRCT and invasive FFR was higher compared to the previous studies, with a lower SD (0.074 in the NXT vs 0.116 in the DISCOVER-FLOW) (Figure 2A).
  | Figure 2 Bland-Altman Plot of FFR and FFR derived from CT. |
The studies evaluating 1D cFFR have thus far been single-center, retrospective studies including 219 patients with 324 vessels. However, the correlations between cFFR and invasive FFR are similarly good, ranging from 0.59 to 0.75 with an SD of 0.13 (Figure 2B). The most recent study by Coenen et al24 included 106 patients with 189 lesions and showed improved discrimination of hemodynamic ischemia for cFFR compared to CCTA stenosis alone (AUC by receiver-operating characteristic curve analysis 0.833 vs 0.642).
Instantaneous wave-free ratio is a novel method to determine the lesion-specific pressure drop in coronary arteries and may be an alternative to FFR.37 However, no studies examining the relation of CT-derived FFR and instantaneous wave-free ratio have been reported.
Diagnostic accuracy of CT-derived FFR in intermediate stenosis
Intermediate degrees of stenosis (30%–70%) present the greatest challenge in the diagnosis of CAD. Since hemodynamically significant lesions are occasionally observed in intermediate lesions with <70% stenosis,13 the use of invasive FFR is recommended to evaluate the function of intermediate coronary lesions as a class IIa indication.6 However, given the relatively lower prevalence of lesion-specific pressure drop caused by intermediate stenosis compared to that of severe stenosis in the FAME study,13 CT-derived FFR would be of great use for assessing the functional significance of intermediate lesions to avoid unnecessary ICA and help in treatment decision making. Table 2 provides a summary of the studies of FFRCT and cFFR. Similar to the overall diagnostic accuracy of CT-derived FFR, all studies demonstrated high diagnostic performance for intermediate stenosis, with the highest accuracy and specificity for FFRCT.24,31,38,39
  | Table 2 Diagnostic performance of CT-derived FFR for intermediate stenosis |
Diagnostic accuracy of CT-derived FFR vs transluminal attenuation gradient
Transluminal attenuation gradient (TAG) is a potential method for noninvasive determination of lesion-specific ischemia by CCTA and is calculated as the slope of the linear regression produced by the luminal contrast attenuation from the ostium to the distal coronary vessel.40 TAG is an easily measured parameter; however, none of the studies have shown superior diagnostic performance of TAG compared to CT-derived FFR for the determination of lesion-specific drop as defined by invasive FFR.34,41,42 Yoon et al41 investigated 53 patients who underwent both 64 slice CCTA and ICA with FFR. AUC demonstrated higher discrimination of lesion-specific ischemia for FFRCT than that for TAG (0.94 vs 0.63, P<0.001). Similarly, our group has demonstrated this relationship in a larger cohort of 103 patients undergoing various detector CCTAs with broad Z-axis coverage (64–320 slice CTs).42 In a substudy of the DISCOVER-FLOW and DeFACTO studies, we found that the AUC for FFRCT had a greater discrimination of lesion-specific drop compared to TAG (0.79 vs 0.50, P<0.001), CCTA stenosis alone (vs 0.62, P=0.0004), and the combination of TAG and CCTA stenosis (vs 0.63, P=0.004).42 These findings remained consistent in a subanalysis when used with different cutoff values for TAG or in a subgroup with larger detector CCTAs (>64 slice CTs). Wang et al34 have also shown that the diagnostic performance of TAG was only modest compared to cFFR (AUC: 0.67 vs 0.91) in a study of 32 patients. A possible explanation for these findings is that TAG assesses coronary blood flow under resting conditions and not during hyperemic conditions that is simulated for the computation of FFRCT and is induced with adenosine during invasive FFR. Another possibility may be that FFRCT is not affected by the various detector CCTAs with broad Z-axis coverage that influences the degree of TAG. In this regard, the cutoff value of TAG is not uniform and relies on the CCTA detectors.42 In contrast, the threshold for FFR-derived CT is always unique, similar to invasive FFR.
Image quality and diagnostic accuracy of CT-derived FFR
Maintaining good image quality and adequate patient preparation for CCTA scanning is essential to provide high diagnostic accuracy for assessment of coronary stenosis severity. Current image acquisition guidelines have helped in reducing technical image errors, providing improved image quality for assessing CAD. However, despite recent advanced technologies, previous investigations have shown that 2.9%–4.2% of segments were still excluded from analyses due to unsatisfactory image quality.43,44 Image quality may similarly affect diagnostic performance of CT-derived FFR since visualization and detection of lumen boundaries and left ventricular mass are imperative for computation of CT-derived FFR. In fact, as shown in Table 3, 10%–13% of cases in the aforementioned studies did not meet the criteria for assessing CCTA images or calculating CT-derived FFR due to suboptimal image quality.24,30,31
  | Table 3 Image quality and CT-derived FFR |
In a substudy of DeFACTO, Leipsic et al45 explored the relationship between image quality and patient preparation before CT to the diagnostic performance of FFRCT. They found that misalignment artifact reduced accuracy (56.0% vs 71.0%, P=0.03) and sensitivity (43.0% vs 86.0%, P=0.001) of FFRCT, whereas coronary motion or increased coronary artery calcium (CAC) did not affect diagnostic performance. A potential explanation may be that severe misalignment artifact can cause inaccurate modeling of the lumen boundary from the proximal to the distal portion of the coronary arteries, which is required for modeling fluid dynamics. Of interest, although premedication with beta-blocker and nitroglycerin within 30 minutes of CCTA scanning did not improve overall diagnostic accuracy of FFRCT, these medications increased specificity (51.0% vs 66.0%, P=0.03). The influence of beta-blocker or heart rates for the computation of FFRCT relies on the scanner’s temporal resolution.
A substudy of the DISCOVER-FLOW study showed that FFRCT had superior diagnostic accuracy compared to CCTA stenosis across the spectrum of image quality, including potential artifacts such as coronary motion, misalignment, image noise, blooming artifact, and signal-to-noise ratio.46
CAC and diagnostic accuracy of CT-derived FFR
Severe CAC can cause blooming artifacts that can interfere with interpretation of CT coronary stenosis. CCTA studies with heavily calcified plaque often have reduced specificity and a lower diagnostic accuracy. Several studies have shown that a high CAC score of ≥400 or 600 results in a reduced specificity ranging between 35% and 48%.47,48 Recent publications suggest that CT-derived FFR does not seem to be affected by high calcification with maintenance of a high diagnostic accuracy, sensitivity, and specificity.31,45,49 In a subanalysis of the NXT trial, among patients with CAC score ≥400, the accuracy, sensitivity, and specificity of FFRCT for the determination of lesion-causing pressure drop were 75% (95% CI: 62%–84%), 88% (95% CI: 64%–97%), and 69% (95% CI: 54%–81%), which were higher than those of CCTA with 44% (95% CI: 31%–56%), 94% (95% CI: 79%–100%), and 23% (95% CI: 11%–37%), respectively.31 Subsequent to this study, Nørgaard et al demonstrated that the diagnostic performance of FFRCT did not diminish at higher levels of coronary calcification. FFRCT showed superior diagnostic accuracy compared to CCTA stenosis alone in a wide range of CAC values.49 Of importance, among patients in the highest quartile of CAC scores, ranging between 416 and 3,599, FFRCT provided a twofold or threefold greater diagnostic specificity for the discrimination of lesion-specific drop compared to CCTA stenosis alone.49 High diagnostic performance of FFRCT was similarly reported in a wide range CAC scores in a subanalysis of DeFACTO (P>0.05).45 The relative immunity of 3D FFRCT to high vessel calcification may be due to the detailed segmentation of the entire coronary tree and the inclusion of physiologic modeling in addition to anatomic modeling. The performance of 1D cFFR analysis in calcified vessels has not been reported. Coenen et al24 eliminated ten patients having an extremely high CAC score with >2,000 in their study, whereas the other studies did not address any criteria to exclude patients due to their baseline CAC scores.30,31 However, the mean CAC in the studies for cFFR was around 550, which is higher than the mean CAC ranging between 300 and 400 in the studies for FFRCT (Table 3), and cFFR showed a high diagnostic accuracy as noted. The further studies examining the diagnostic accuracy of cFFR among patients with high CAC will be needed.
Image quality and processing time
CT image quality affects not only the diagnostic performance of computed FFR but also the processing time of CT-derived FFR. Image quality primarily influences coronary artery segmentation and creation of the anatomical coronary model, which is the most time-consuming process.
Prior studies have shown that the processing time for 1D cFFR analysis was <2 hours per case (Table 3). Coenen et al24 reported that 30 minutes to 2 hours were required for coronary segmentation and modeling, and 5–10 minutes were needed for computation of 1D cFFR. Other studies using 1D cFFR reported similar processing times of 37–52 minutes per patient.32,33 This approach may be more practical in a busy clinical practice for managing patient care and <1–2 hours for getting the results of CT-derived FFR may be practical, especially to evaluate subjects with acute chest pain in emergency department.
In contrast, 3D FFRCT analysis required ~4 hours for processing and calculation of FFRCT.29,31 Introduction of semiautomated and automated processes and inclusion of machine learning algorithms have improved processing times for 3D FFRCT analysis such that processing times of 1–2 hours can be anticipated in the near future.
Predicting therapeutic benefit and planning revascularization strategy
The most exciting potential benefit of CT-derived FFR compared to other noninvasive functional tests may be its ability to both plan and simulate coronary intervention and forecast the benefit of revascularization. Kim et al have recently revealed the utility of FFRCT for “virtual coronary stenting”, in which the preoperative anatomic computational model is modified to eliminate one or more stenosis, thus simulating the anatomic changes due to stenting. The pressure, flow, and FFRCT are then recomputed to show the predicted therapeutic benefit that can be expected from revascularization.50 This novel method may improve preinterventional treatment planning and reduce procedure time, contrast use, and radiation exposure as well as downstream procedures such as serial FFR or intravenous ultrasound measurements during coronary intervention, especially in patients with complex lesions.
The clinical utility of CT-derived FFR
The clinical utility of FFRCT in helping to guide decision making in symptomatic patients with suspected CAD has been evaluated in the prospective, multicenter “Prospective LongitudinAl Trial of FFRCT: Outcome and Resource IMpacts (PLATFORM)” Study.51 In this study of 584 patients with suspected CAD, patients referred directly for ICA or for noninvasive testing were compared to similar patients evaluated with CT angiography and FFRCT. This study demonstrated that among patients with planned ICA, 73% had no significant coronary obstruction (<50% stenosis) by coronary angiography. By comparison, only 12% of patients evaluated using an FFRCT-guided strategy went on to have an ICA that showed no significant coronary obstruction, a reduction of 83%. In 61% of patients, the use of an FFRCT-guided strategy resulted in the cancelation of the planned coronary angiogram. Despite excluding subjects who did not calculate FFRCT due to lack of obstruct CAD on CCTA, FFRCT still canceled ICA among 35% of patients. In addition, despite the difference in the number of patients who required ICA, the rates of revascularization procedures, such as stenting or CABG, were similar in patients evaluated by ICA (31.6%) and patients evaluated by FFRCT (28.5%). Importantly, no clinical adverse events were reported among patients whose physicians chose to cancel ICA based on the FFRCT result.
This study demonstrated that by using FFRCT, physicians may be able to efficiently triage patients to the most appropriate care and reduce the use of ICA. This highlights the potential clinical utility of FFRCT in guiding treatment decisions in patients with stable CAD; however, several clinical questions remain to be addressed. In the PLATFORM, the relative magnitudes of false positives of FFRCT were seen in FFRCT group of the planned ICA arm. Positive predictive value of FFRCT was modest with 68.4%, which is in line with the previous diagnostic studies for CT-derived FFR, ranging between 61% and 75% (Table 1).24,29–32,34, Although this rate is still lower than the rate of nonobstructive CAD by ICA being found after other noninvasive tests,52 this would be controversial to select inappropriate ICA candidates. Another concern may be that the data regarding the contemporary workflow for the subjects with a “gray-zone” CT-derived FFR, similar to that by invasive FFR, are still lacking,53 whereas the PLATFORM showed no clinical adverse events among patients who canceled ICA because FFRCT did not reach the threshold of FFRCT <0.80.
Since there has been to date no study done to focus upon the workflow of CT-derived FFR to confirm the feasibility of this emerging technique in real-world clinical practice, more plenty data with respect to the contemporary clinical experience with CT-derived FFR in real-world patients would be required.
The cost implications of CT-derived FFR
The cFFR may not add additional cost over that of CCTA since this technique is calculated on the workstation at a local site. This approach may provide lower medical costs compared to the combination of CCTA with other noninvasive modalities for the assessment of inconclusive coronary lesions, where the functional assessment is needed.
Compared with cFFR, cost-effectiveness plays a key role for the practical utility of FFRCT, since the result of the calculation is provided by the off-site service. Despite the technique being commercially approved in the USA and Europe, the Medicare cost for FFRCT has not been established yet. Owing to this issue, a few studies explored the economic value of FFRCT over the ICA strategy.54–56 In a substudy of 96 patients enrolled from DISCOVER-FLOW, the FFRCT strategy saved a 30% of medical cost to identify patients who need coronary intervention when compared to that of the ICA by visual assessment with PCI, resulting in a 12% reduction in clinical outcomes at 1 year. Another subanalysis from the NXT trial similarly demonstrated that the CCTA-FFRCT strategy reduced 32% of medical costs and resulted in 19% lower clinical outcomes compared to the ICA-visual strategy at 1 year in Japan.55
A recent substudy of the aforementioned PLATFORM tested several cost weights of FFRCT and explored the cost-effectiveness and quality of life of FFRCT during a follow-up of 90 days.56 When the cost for FFRCT is set at seven times the weight of CCTA cost, FFRCT demonstrated a 20% reduction of medical costs compared to the usual care among patients who were enrolled in the planned invasive group. FFRCT demonstrated a significant cost benefit until up to a 20-fold higher cost of CCTA. In contrast, when FFRCT cost is weighted one-half cost of CCTA, FFRCT costs higher than usual care among patients who were enrolled in the planned noninvasive group ($2,766 vs $2,137, P=0.02). However, the quality of life was improved in the FFRCT group compared to the usual care group.
Conclusion
Computational analysis of FFR from CCTA imaging data allows noninvasive assessment of lesion-specific drop. This combined anatomic and functional assessment can accurately identify patients who have lesion-causing pressure drop in coronary arteries. This new noninvasive method may be an alternative to invasive ICA with FFR in helping to guide patient care. However, we would need more data on how to fit the emerging technique into a “real-world” clinical practice to guide decision making for patient care in the coming years.
Disclosure
The authors report no conflicts of interest in this work.
References
Pijls NH, van Schaardenburgh P, Manoharan G, et al. Percutaneous coronary intervention of functionally nonsignificant stenosis: 5-year follow-up of the defer study. J Am Coll Cardiol. 2007;49:2105–2111. | |
Pijls NH, Fearon WF, Tonino PA, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention in patients with multivessel coronary artery disease:2-year follow-up of the fame (fractional flow reserve versus angiography for multivessel evaluation) study. J Am Coll Cardiol. 2010;56:177–184. | |
De Bruyne B, Pijls NH, Kalesan B, et al. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med. 2012;367:991–1001. | |
De Bruyne B, Fearon WF, Pijls NH, et al; FAME 2 Trial Investigators. Fractional flow reserve-guided PCI for stable coronary artery disease. N Engl J Med. 2014;371:1208–1217. | |
Windecker S, Kolh P, Alfonso F, et al. 2014 ESC/EACTS guidelines on myocardial revascularization:the task force on myocardial revascularization of the European society of cardiology (ESC) and the European association for cardio-thoracic surgery (EACTS)developed with the special contribution of the European association of percutaneous cardiovascular interventions (EAPCI). Eur Heart J. 2014;35:2541–2619. | |
Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention:a report of the American college of cardiology foundation/American heart association task force on practice guidelines and the society for cardiovascular angiography and interventions. Circulation. 2011;124:e574–e651. | |
Montalescot G, Sechtem U, Achenbach S, et al. 2013 ESC guidelines on the management of stable coronary artery disease:the task force on the management of stable coronary artery disease of the European society of cardiology. Eur Heart J. 2013;34:2949–3003. | |
Patel MR, Dai D, Hernandez AF, et al. Prevalence and predictors of nonobstructive coronary artery disease identified with coronary angiography in contemporary clinical practice. Am Heart J. 2014;167:846 e2.–852.e2. | |
Neglia D, Rovai D, Caselli C, et al; EVINCI Study Investigators. Detection of significant coronary artery disease by noninvasive anatomical and functional imaging. Circ Cardiovasc Imaging. 2015;8:e002179. | |
Budoff MJ, Dowe D, Jollis JG, et al. Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease:results from the prospective multicenter accuracy (assessment by coronary computed tomographic angiography of individuals undergoing invasive coronary angiography) trial. J Am Coll Cardiol. 2008;52:1724–1732. | |
Meijboom WB, Meijs MF, Schuijf JD, et al. Diagnostic accuracy of 64-slice computed tomography coronary angiography:a prospective, multicenter, multivendor study. J Am Coll Cardiol. 2008;52:2135–2144. | |
Miller JM, Rochitte CE, Dewey M, et al. Diagnostic performance of coronary angiography by 64-row ct. N Engl J Med. 2008;359:2324–2336. | |
Tonino PA, Fearon WF, De Bruyne B, et al. Angiographic versus functional severity of coronary artery stenoses in the fame study fractional flow reserve versus angiography in multivessel evaluation. J Am Coll Cardiol. 2010;55:2816–2821. | |
Meijboom WB, Van Mieghem CA, van Pelt N, et al. Comprehensive assessment of coronary artery stenoses:computed tomography coronary angiography versus conventional coronary angiography and correlation with fractional flow reserve in patients with stable angina. J Am Coll Cardiol. 2008;52:636–643. | |
Toth G, Hamilos M, Pyxaras S, et al. Evolving concepts of angiogram:fractional flow reserve discordances in 4000 coronary stenoses. Eur Heart J. 2014;35:2831–2838. | |
Rossi A, Papadopoulou SL, Pugliese F, et al. Quantitative computed tomographic coronary angiography: does it predict functionally significant coronary stenoses? Circ Cardiovasc Imaging. 2014;7:43–51. | |
Min JK, Shaw LJ, Devereux RB, et al. Prognostic value of multidetector coronary computed tomographic angiography for prediction of all-cause mortality. J Am Coll Cardiol. 2007;50:1161–1170. | |
Min JK, Dunning A, Lin FY, et al. Age- and sex-related differences in all-cause mortality risk based on coronary computed tomography angiography findings results from the international multicenter confirm (coronary CT angiography evaluation for clinical outcomes:an international multicenter registry) of 23,854 patients without known coronary artery disease. J Am Coll Cardiol. 2011;58:849–860. | |
Sarno G, Decraemer I, Vanhoenacker PK, et al. On the inappropriateness of noninvasive multidetector computed tomography coronary angiography to trigger coronary revascularization:a comparison with invasive angiography. JACC Cardiovasc Interv. 2009;2:550–557. | |
Taylor CA, Fonte TA, Min JK. Computational fluid dynamics applied to cardiac computed tomography for noninvasive quantification of fractional flow reserve:scientific basis. J Am Coll Cardiol. 2013;61:2233–2241. | |
Stergiopulos N, Young DF, Rogge TR. Computer simulation of arterial flow with applications to arterial and aortic stenoses. J Biomech. 1992;25:1477–1488. | |
Itu L, Sharma P, Mihalef V, et al. A patient-specific reduced-order model for coronary circulation. Proc IEEE Int Symp Biomed Imaging. 2012; 832–835. | |
Choy JS, Kassab GS. Scaling of myocardial mass to flow and morphometry of coronary arteries. J Appl Physiol. 1985;2008(104):1281–1286. | |
Coenen A, Lubbers MM, Kurata A, et al. Fractional flow reserve computed from noninvasive CT angiography data:diagnostic performance of an on-site clinician-operated computational fluid dynamics algorithm. Radiology. 2015;274:674–683. | |
Olufsen MS. Structured tree outflow condition for blood flow in larger systemic arteries. Am J Physiol. 1999;276:H257–H268. | |
Smith NP, Pullan AJ, Hunter PJ. Generation of an anatomically based geometric coronary model. Ann Biomed Eng. 2000;28:14–25. | |
Seiler C, Kirkeeide RL, Gould KL. Measurement from arteriograms of regional myocardial bed size distal to any point in the coronary vascular tree for assessing anatomic area at risk. J Am Coll Cardiol. 1993;21:783–797. | |
Sharma P, Itu L, Zheng X, et al. A framework for personalization of coronary flow computations during rest and hyperemia. Conf Proc IEEE Eng Med Biol Soc. 2012;2012:6665–6668. | |
Koo BK, Erglis A, Doh JH, et al. Diagnosis of ischemia-causing coronary stenoses by noninvasive fractional flow reserve computed from coronary computed tomographic angiograms. Results from the prospective multicenter discover-flow (diagnosis of ischemia-causing stenoses obtained via noninvasive fractional flow reserve) study. J Am Coll Cardiol. 2011;58:1989–1997. | |
Min JK, Leipsic J, Pencina MJ, et al. Diagnostic accuracy of fractional flow reserve from anatomic CT angiography. JAMA. 2012;308:1237–1245. | |
Nørgaard BL, Leipsic J, Gaur S, et al; NXT Trial Study Group. Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease:the NXT trial (analysis of coronary blood flow using CT angiography: next steps). J Am Coll Cardiol. 2014;63:1145–1155. | |
Renker M, Schoepf UJ, Wang R, et al. Comparison of diagnostic value of a novel noninvasive coronary computed tomography angiography method versus standard coronary angiography for assessing fractional flow reserve. Am J Cardiol. 2014;114:1303–1308. | |
Baumann S, Wang R, Schoepf UJ, et al. Coronary CT angiography-derived fractional flow reserve correlated with invasive fractional flow reserve measurements – initial experience with a novel physician-driven algorithm. Eur Radiol. 2015;25:1201–1207. | |
Wang R, Renker M, Schoepf UJ, et al. Diagnostic value of quantitative stenosis predictors with coronary CT angiography compared to invasive fractional flow reserve. Eur J Radiol. 2015;84:1509–1515. | |
Leipsic J, Abbara S, Achenbach S, et al. SCCT guidelines for the interpretation and reporting of coronary CT angiography:a report of the society of cardiovascular computed tomography guidelines committee. J Cardiovasc Comput Tomogr. 2014;8:342–358. | |
Gaur S, Achenbach S, Leipsic J, et al. Rationale and design of the heartflownxt (heartflow analysis of coronary blood flow using CT angiography:next steps) study. J Cardiovasc Comput Tomogr. 2013;7:279–288. | |
Jeremias A, Maehara A, Généreux P, et al. Multicenter core laboratory comparison of the instantaneous wave-free ratio and resting pd/pa with fractional flow reserve:the resolve study. J Am Coll Cardiol. 2014;63:1253–1261. | |
Min JK, Koo BK, Erglis A, et al. Usefulness of noninvasive fractional flow reserve computed from coronary computed tomographic angiograms for intermediate stenoses confirmed by quantitative coronary angiography. Am J Cardiol. 2012;110:971–976. | |
Nakazato R, Park HB, Berman DS, et al. Noninvasive fractional flow reserve derived from computed tomography angiography for coronary lesions of intermediate stenosis severity:results from the defacto study. Circ Cardiovasc Imaging. 2013;6:881–889. | |
Steigner ML, Mitsouras D, Whitmore AG, et al. Iodinated contrast opacification gradients in normal coronary arteries imaged with prospectively ECG-gated single heart beat 320-detector row computed tomography. Circ Cardiovasc Imaging. 2010;3:179–186. | |
Yoon YE, Choi JH, Kim JH, et al. Noninvasive diagnosis of ischemia-causing coronary stenosis using CT angiography:diagnostic value of transluminal attenuation gradient and fractional flow reserve computed from coronary CT angiography compared to invasively measured fractional flow reserve. JACC Cardiovasc Imaging. 2012;5:1088–1096. | |
Nakanishi R, Matsumoto S, Alani A, et al. Diagnostic performance of transluminal attenuation gradient and fractional flow reserve by coronary computed tomographic angiography (FFRCT) compared to invasive FFR:a sub-group analysis from the discover-flow and defacto studies. Int J Cardiovasc Imaging. 2015;31:1251–1259. | |
Puchner SB, Liu T, Mayrhofer T, et al. High-risk plaque detected on coronary CT angiography predicts acute coronary syndromes independent of significant stenosis in acute chest pain: results from the Romicat-II trial. J Am Coll Cardiol. 2014;64:684–692. | |
Hamon M, Biondi-Zoccai GG, Malagutti P, et al. Diagnostic performance of multislice spiral computed tomography of coronary arteries as compared with conventional invasive coronary angiography: a meta-analysis. J Am Coll Cardiol. 2006;48:1896–1910. | |
Leipsic J, Yang TH, Thompson A, et al. CT angiography (CTA) and diagnostic performance of noninvasive fractional flow reserve:results from the determination of fractional flow reserve by anatomic CTA (defacto) study. AJR Am J Roentgenol. 2014;202:989–994. | |
Min JK, Koo BK, Erglis A, et al. Effect of image quality on diagnostic accuracy of noninvasive fractional flow reserve:results from the prospective multicenter international discover-flow study. J Cardiovasc Comput Tomogr. 2012;6:191–199. | |
Arbab-Zadeh A, Miller JM, Rochitte CE, et al. Diagnostic accuracy of computed tomography coronary angiography according to pre-test probability of coronary artery disease and severity of coronary arterial calcification. the core-64 (coronary artery evaluation using 64-row multidetector computed tomography angiography) international multicenter study. J Am Coll Cardiol. 2012;59:379–387. | |
Abdulla J, Pedersen KS, Budoff M, Kofoed KF. Influence of coronary calcification on the diagnostic accuracy of 64-slice computed tomography coronary angiography:a systematic review and meta-analysis. Int J Cardiovasc Imaging. 2012;28:943–953. | |
Nørgaard BL, Gaur S, Leipsic J, et al. Influence of coronary calcification on the diagnostic performance of CT angiography derived FFR in coronary artery disease:a substudy of the NXT trial. JACC Cardiovasc Imaging. 2015;9:1045–1055. | |
Kim KH, Doh JH, Koo BK, et al. A novel noninvasive technology for treatment planning using virtual coronary stenting and computed tomography-derived computed fractional flow reserve. JACC Cardiovasc Interv. 2014;7:72–78. | |
Douglas PS, Pontone G, Hlatky MA, et al. Clinical outcomes of fractional flow reserve by computed tomographic angiography-guided diagnostic strategies vs. Usual care in patients with suspected coronary artery disease:the prospective longitudinal trial of FFRCT: outcome and resource impacts study. Eur Heart J. 2015;36:3359–3367. | |
Patel MR, Peterson ED, Dai D, et al. Low diagnostic yield of elective coronary angiography. N Engl J Med. 2010;362:886–895. | |
Petraco R, Sen S, Nijjer S, et al. Fractional flow reserve-guided revascularization:practical implications of a diagnostic gray zone and measurement variability on clinical decisions. JACC Cardiovasc Interv. 2013;6:222–225. | |
Hlatky MA, Saxena A, Koo BK, Erglis A, Zarins CK, Min JK. Projected costs and consequences of computed tomography-determined fractional flow reserve. Clinical Cardiol. 2013;36:743–748. | |
Kimura T, Shiomi H, Kuribayashi S, et al. Cost analysis of non-invasive fractional flow reserve derived from coronary computed tomographic angiography in Japan. Cardiovasc Interv Ther. 2015;30:38–44. | |
Hlatky MA, De Bruyne B, Pontone G, et al; PLATFORM Investigators. Quality-of-life and economic outcomes of assessing fractional flow reserve with computed tomography angiography: platform. J Am Coll Cardiol. 2015;66:2315–2323. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.