Back to Journals » Infection and Drug Resistance » Volume 16
Nomogram Prediction Model of Hypernatremia on Mortality in Critically Ill Patients
Authors Qi Z , Lu J , Liu P , Li T, Li A , Duan M
Received 6 September 2022
Accepted for publication 23 December 2022
Published 6 January 2023 Volume 2023:16 Pages 143—153
DOI https://doi.org/10.2147/IDR.S387995
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Zhili Qi,1,* Jiaqi Lu,2,* Pei Liu,1 Tian Li,1 Ang Li,3 Meili Duan1
1Department of Critical Care Medicine, Capital Medical University, Beijing, People’s Republic of China; 2Department of Critical Care Medicine, Beijing Ditan Hospital, Capital Medical University, Beijing, People’s Republic of China; 3Beijing Ditan Hospital, Capital Medical University, Beijing, People’s Republic of China
*These authors contributed equally to the article
Correspondence: Ang Li, Beijing Ditan Hospital, Capital Medical University, Beijing Ditan Hospital 8 Jing Shun East Street, Beijing, People’s Republic of China, Email [email protected] Meili Duan, Department of Critical Care Medicine, Beijing Friendship Hospital, Capital Medical University, No. 95 Yong’an Road, Xicheng District, Beijing, 10005, People’s Republic of China, Email [email protected]
Objective: To investigate the value of hypernatremia in the intensive care unit (ICU) for the risk prediction of mortality in severe patients.
Methods: Clinical data of critically ill patients admitted to the ICU of Beijing Friendship Hospital, were collected for retrospective analysis. Univariate and multivariate logistic regression analyses were employed to analyze the influencing factors. Nomograms predicting the mortality were constructed with R software and validated with repeated sampling.
Results: A total of 442 cases were eligible for this study. Hypernatremia within 48 hours of ICU admission, change in sodium concentration (CNa+) within 48 hours, septic shock, APACHE II score, hyperlactatemia within 48 hours, use of continuous renal replacement therapy (CRRT) within 48 hours, and the use of mechanical ventilation (MV) within 48 hours of ICU admission were all identified as independent risk factors for death within 28 days of ICU admission. These predictors were included in a nomogram of 28-day mortality in severe patients, which was constructed using R software.
Conclusion: The nomogram could predict the individualized risk of 28-day mortality based on the above factors. The model has better discrimination and accuracy and has high clinical application value.
Keywords: intensive care unit, 28 day mortality, serum sodium, hypernatremia
Introduction
Electrolyte imbalance is common in hospitalized patients, especially the elderly,1,2 and is associated with an increased risk of death.3 In addition, abnormal serum sodium concentration is a common electrolyte disorder, and it has been reported that about 30% to 40% of hospitalized patients will have sodium concentration disorder.4,5 More than one-third of patients in intensive care units (ICU) may present with abnormal serum sodium concentrations, which can manifest as hyponatremia or hypernatremia, among others.6,7 Despite large variations in daily sodium and water intake, plasma sodium levels are normally regulated within a small physiological range. When there is an absolute or relative free water deficit in hypernatremia (usually defined as a plasma sodium concentration greater than 145 mmol / L), the brain and kidney responses require that water uptake and excretion be balanced with salt uptake and excretion, which helps restore plasma sodium homeostasis.8 Researches have shown that hypernatremia is common in the ICU setting.9 One study showed that hypernatremia in critically ill patients usually occurs after rather than on admission.10 The hypernatremia seen in hospitalized patients may be either community-acquired hypernatremia as part of the admission diagnosis or hospital-acquired hypernatremia occurring during hospitalization.11 Hypernatremia occurs because the ratio of sodium and water in the blood is changed because the loss of water exceeds the loss of sodium, and the absence of water which may result from reduced intake or excessive loss.12 Therefore, most hypernatremia is thought to be related to hypovolemia. But hypervolemic hypernatremia is rare.13–16 In addition, researchers have also highlighted that patients with severe sepsis who received 0.9% saline resuscitation may acquire hypernatremia at an early stage.17
Due to the significant impact that sodium disturbances have on patient outcomes, there has been a surge in scientific interest in these disorders.18 In fact, sodium level is an important prognostic factor and is included in the ICU scoring system.19 Hypernatremia is an independent predictor of mortality. Based on the presence of hypernatremia in a patient, death is more likely to occur in patients with higher serum sodium concentrations.20,21 Hypernatremia is also associated with increased mortality following bacterial infectious diseases.22 Furthermore, recent research has revealed that even little changes in serum sodium levels are related with a considerable increase in in-hospital mortality.5,23,24
There is some influence of hypernatremia on patient mortality in ICU. The primary objective of this study was to evaluate the value of hypernatremia in the ICU for the risk prediction of mortality in critically ill patients. In turn, to clarify the risks of electrolyte disturbances in critically ill patients in the ICU, early intervention for high-risk patients should be conducted to enhance the quality of patient survival.
Patients and Methods
Patients Information
This retrospective study included a total of 1173 patients who visited the Department of Critical Care Medicine at Beijing Friendship Hospital between January 1, 2018, and December 31, 2018, with only the first admission to the ICU considered if the patients were admitted multiple times during the study period. Exclusion criteria were: 1) Patients’ age < 18 years; 2) Time to ICU admission < 48 hours; 3) Pregnant patients; 4) Recipients who had received a liver and kidney transplant before or those who had received a liver and kidney transplant after admission; 5) Patients with missing clinical data during ICU stay. The study was carried out in accordance with the Declaration of Helsinki. This study was approved by the Professional Committee on bioethics of Beijing Friendship Hospital (No. 2022-P2-083-01). As this study was a study utilizing medical record information obtained from previous clinical experience, we applied for waiver of informed consent, and consent was obtained from the ethics committee. Throughout the study, we respected patient privacy and ensured that data information was not leaked.
Definitions and Diagnostic Criteria
Sepsis is a life-threatening organ dysfunction resulting from a dysregulated response of the organism to infection. Diagnostic criteria: patients with infection or suspected infection and a SOFA score ≥ 2 or a SOFA score changes ≥ 2. Septic shock: in patients with sepsis after adequate fluid resuscitation: 1) Need for vasoactive drugs to maintain map ≥ 65 mmHg; 2) Serum lactate concentration > 2 mmol / L.25 Diagnostic criteria for ICU readmission: if a patient was admitted to the ICU more than once during the study period, only the patient’s first ICU admission was considered relevant. The initial sodium concentration value (Na0) is the first measured value of serum sodium concentration within admission to the ICU. The initial chloride value (CL0) is the first measured value of serum chloride concentration within admission to the ICU. The 48-hour maximum sodium concentration value (Namax) is the maximum sodium concentration value obtained during 48 hours after ICU admission. The 48-hour maximum chloride value (Clmax) is the maximum serum chloride concentration value measured within 48 hours of admission to ICU. Hypernatremia is defined as a sodium concentration greater than 145 mmol / L; Hyponatremia is defined as sodium concentration lower than 135 mmol / L; Normal serum sodium concentrations are 135–145 mmol / L. Hyperchloremia is defined as a serum chloride concentration higher than 110 mmol / L; and Normal serum chloride concentrations are 99–110 mmol / L. Sodium concentration change value (CNa): the difference between the maximum sodium concentration value measured within 48 hours of admission to the ICU minus the difference obtained from the first measured sodium concentration value within the ICU. Chloride concentration change value (CCl): the difference between the maximum serum chloride concentration value measured within 48 hours of admission to the ICU minus the value obtained from the first measured serum chloride concentration within the ICU. Hyperlactatemia is defined as serum lactate values > 2 mmol / L. These criteria are based on the standard values of serum sodium and chloride in the biochemical room at Friendship Hospital.
Data Collection
The study was approved by Beijing Friendship Hospital’s ethics committee and is based on a review of information related to the demographics, clinical characteristics, and laboratory results of critically ill patients admitted to the Beijing Friendship Hospital ICU affiliated with Capital Medical University in 2018. Case Report Form (CRF) was created based on the exclusion criteria and experimental purposes, and the information of eligible research subjects was acquired in accordance with CRF-related content by logging into the medical electronic information system. The information included: patient’s basic information (age, gender), serum chloride - and sodium concentration related indexes (Na0, CL0, Namax, Clmax), underlying diseases (hypertension, diabetes, coronary heart disease, heart failure, liver disease, tumour, hematological diseases), APACHE II score, admission to ICU initial base excess (BE), highest blood lactate within 48 hours of admission to ICU, application of continuous renal replacement therapy (CRRT), mechanical ventilation (MV) and norepinephrine during the initial 48 hours. The outcome measure is 28-day mortality within the ICU.
Predictive Model Construction, Validation, and Evaluation
The data was divided into training and validation sets in a 7:3 ratio, and the modeling process was completed in the training set. Means ± SD was used for continuous variables with a normal distribution, whereas medians and interquartile ranges were used for continuous variables with a skewed distribution. When two independent samples conformed to normal distribution, and homogeneity of variance was assumed, the independent samples t-test was used for difference comparison. The chi-square test or Fisher’s exact test was applied when judging whether there was any difference between the two overall rates and constituent ratios.
To establish a well-calibrated nomogram to predict outcomes, we performed univariate and multivariate logistic regression analyses to screen predictors, in which variables with P < 0.1 in univariate were entered into the multivariate stepwise logistic regression.26 Based on these results, a nomogram prediction model based on independent risk factors was developed using R software. The model was then validated and evaluated. First, the area under the receiver operating characteristic (ROC) curve (AUC) was adopted to analyze the accuracy of the model. Second, repeated sampling validation 1000 times was performed to draw the calibration curve, and the correlation between the calibration curve and the standard curve was verified and evaluated. Finally, clinical impact curve and decision curve analyses were used to determine the model’s clinical validity.
The analysis software for this study was IBM SPSS Statistics 24.0 (IBM Corporation, Armonk, New York, USA) and R version 3.3.3 (The R Foundation for Statistical Computing, Austria, Vienna).
Results
Characteristics of Patients
In this study, we reviewed data from 1221 critically ill patients in the ICU. 779 individuals were not eligible for inclusion and were thus excluded based on the exclusion criteria. Among them, 123 patients were omitted because they were under the age of 18; 492 patients were excluded because they had been in the ICU for less than 48 hours; and 10 pregnancies were excluded. 104 individuals were excluded because they had a kidney or liver transplant; clinical data for two patients were lacking; and 48 patients were readmitted to the ICU. The number of patient cases finally included in the study was 442. The study flow chart is shown in Figure 1, including the training cohort (n = 309) and validation cohort (n = 133). Of these patients, 61 (13.8%) patients died within 28 days. The mortality of 28 days in the training and validation cohorts was 12.3% and 17.3%, respectively. After that, we summarized the demographic and clinical characteristics of the training cohort (Table 1).
 |
Table 1 Patient and Disease Characteristics |
 |
Figure 1 Study design. A total of 443 ICU patients with complete relevant data were enrolled in this study. |
We analyzed a total of 26 clinical variables (Table 1), and analysis of the patients in the 309 training cohort revealed that 182 (58.9%) were male. The age of the patients is 59.5 ± 17.5 years, and although the mean age of the patients in the death group was higher than that in the survival group (61.2 ± 21.3 vs 59.2 ± 17 years), the difference between the two was not statistically significant (P = 0.584). The initial sodium concentration was higher in the death group than in the survival group (140.1 ± 6.5 vs 139.9 ± 5.4 mmol / L), but the difference between the two was not statistically significant (P = 0.860). The initial chloride concentration was lower in the deceased group than in the surviving group (105.5 ± 4.4 vs 106.2 ± 4.8 mmol / L), but the difference was also not statistically significant (P = 0.305). Similarly, the maximum sodium concentration at 48 hours was higher in the death group than in the survival group (143.4 ± 6.3 vs 142.5 ± 4.9 mmol / L), but the difference between the two was not statistically significant (P = 0.431). The maximum chloride concentration at 48 hours was higher in the death group than in the survival group (111.8 ± 6.2 vs 110.3 ± 5 mmol / L), and there was no significant difference between them (P = 0.103). Also, admission to the ICU with initial hypernatremia and hyperchloremia had no effect on patients’ 28-day mortality. On the other hand, the difference of hypernatremia and hyperchloremia within 48h of admission to ICU between the death group and the survival group was statistically significant with P < 0.05. Analysis of the values of sodium concentration as well as chloride concentration change between the survival group and the death group revealed that the values of sodium concentration as well as chloride concentration change in the death group were larger than those in the survival group (4.4 ± 2.9 vs 1.8 ± 3.3 mmol / L) and (6.3 ± 5.1 vs 3.3 ± 4.4 mmol / L), respectively, and the differences were statistically significant with P < 0.001. Other results can be referred to Table 1.
Predictors of Death in Severe Patients
The results of univariate and multivariate logistic regression analyses in the training cohort are shown in Table 2. Selected statistically significant variables were applied to univariate binary logistic regression. The statistically significant variables were then included in a multivariate logistic regression before being included into a predictive model. Univariate analysis revealed that eleven variables were substantially different between the death and survival groups (Table 1): hyperchloremia, hypernatremia, CNa, CCl, Septic shock, APACHE II score, hyperlactatemia, CRRT, MV, and norepinephrine. These variables were further included in the multivariate logistic regression analysis using the forward LR method. As the result, Hyperchloremia, CNa, septic shock, APACHE II score, hyperlactatemia, CRRT, and MV were all identified as independent risk factors for 28-day mortality (Table 2).
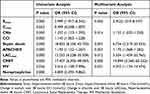 |
Table 2 Univariate and Multivariate Analyses of Predictors for Death |
The results showed that patients with hypernatremia within 48h had a higher risk of 28-day mortality (P = 0.046; OR 2.952, 95% CI 1.019–8.547). Higher values for changes in sodium-ion within 48 hours were associated with higher odds of 28-day death (P = 0.014; OR 1.132, 95% CI 1.025–1.250). Patients who presented with septic shock had a higher risk of death within 28 days than those without septic shock (P = 0.001; OR 6.734, 95% CI 2.219–20.435). As we know, patients with high APACHE II scores are more likely to experience death than those with low scores (P = 0.001; OR 1.170, 95% CI 1.068–1.282). Patients with likewise hyperlactatemia are more likely to die than those without hyperlactatemia (P = 0.012; OR 5.504, 95% CI 1.459–20.765). Patients who use CRRT within 48 h of admission to ICU are more likely to experience death within 28 days than those who do not (P < 0.001; OR 14.894, 95% CI 3.565–62.222). Furthermore, we incorporated it into the prediction model. Similarly, patients who use mechanical ventilation within 48 h of ICU admission are more likely to experience death within 28 days (P = 0.031; or 4.052, 95% CI 1.134–14.474).
Overall, Hypernatremia, CNa, septic shock, APACHE II score, hyperlactatemia, CRRT, and MV can be included in the nomogram as independent risk predictors of 28-day mortality in severe patients by using R software to establish the nomogram (Figure 2).
 |
Figure 2 Nomogram to predict the outcomes of death. |
Determination of Cut-off Values for Predicting Death
Following the establishment of the model, we utilize the area under the receiver operating curve (ROC) (AUC) to assess the model’s accuracy. ROC analysis nomogram was validated internally in the training cohort (Figure 3A) and externally in the validation cohort (Figure 3B). The AUC value of the internal validation ROC curve was 0.9392 (95% CI 0.9053–0.9732); The AUC value of the external validation ROC curve was 0.8289 (95% CI 0.7468–0.9109), indicating that the model had a relatively ideal value. Afterward, R software was utilized to establish the calibration curve to further verify the validity of the model (Figure 4). The calibration of the nomogram was performed internally in the training cohort (Figure 4A) and externally in the validation cohort (Figure 4B). The calibration curve of the model showed a relatively acceptable goodness of fit to the standard ideal curve, which was an ideal situation where the predicted probability of occurrence by the corresponding model was in complete agreement with the actual probability of occurrence. The calibration plot (n = 1000) was drawn using repeated sampling, and the correlation between the calibration and standard curves was verified and evaluated, which further indicated that the model had good fitting validity and high predictive value. Finally, its clinical validity was further evaluated. We used R software to draw clinical impact curves (Figure 5) and decision curves (Figure 6). Most areas of the decision curve of the model were greater than 0, indicating some clinical validity. These results indicated that the model had some predictive value.
 |
Figure 4 Calibration of the nomogram to predict the death in the training dataset (A) and validation dataset (B). |
 |
Figure 6 Decision curve analysis (DCA) for the nomogram in the training dataset (A) and validation dataset (B). |
Discussion
We performed multivariate analyses as well as model building and fit the models in an attempt to identify independent factors predicting mortality. We observed that hypernatremia and CNa were independent risk factors for 28-day mortality in patients hospitalized in the ICU. Mildly elevated sodium concentration levels as well as hypernatremia have previously been shown to place patients at increased risk of death.27–29 Hypernatremia could increase mortality in critical patients independent of comorbidities.10,30–34 A study found that the hospital mortality rate of patients with hospital-acquired hypernatremia was 29%.35 However, it is unclear whether hypernatremia directly reduces survival or whether it is a surrogate marker for more severe disease states.
Hypernatremia is an important factor of morbidity and mortality in patients with neurological disorders. Hypernatremia occurs in 36.9% of severe head injury patients treated in the neurointensive care unit, and it is independently associated with early mortality.36 Hypernatremia is more common in patients with a severe head injury who have central diabetes insipidus and lower admission Glasgow Coma Scale (GCS) scores.37 Patients with spontaneous intracerebral hemorrhage typically have an electrolyte imbalance, and CNa frequently indicates a poor prognosis.38 The early use of osmotic diuretics and loop diuretics, which resulted in a disorder of body water and sodium metabolism, may be the cause of hypernatremia. A retrospective study of 152 ICU patients showed that hypernatremia was an independent risk factor for mortality in ICU patients.39 One study reported a statistically significant sequential relationship between the severity of hypernatremia and the proportion of patients with dementia among hospitalized patients with a mean age of 81 years: mild hypernatremia (146–150 mmol / L) (76%), moderate hypernatremia (151–159 mmol / L) (83%), and severe hypernatremia (≥ 160 mmol / L) (98%).40 In patients with aneurysmal subarachnoid hemorrhage, hypernatremia was associated with increased mortality and a worse prognosis.41 An increase in plasma sodium concentration had also been shown to induce arterial structural remodeling,42 increased arterial oxidative stress,43 collagen deposition, and tube wall thickening with lumen narrowing.44 All of these changes contribute to an increase or maintenance of arterial tone and peripheral vascular total resistance, which causes blood pressure to increase.
In patients with renal system diseases, hypernatremia was also an important factor of morbidity and mortality. The high concentration of sodium in the extracellular space is well recognized to affect cell function, which in turn stimulates inflammatory responses in intestinal, bronchial, and renal epithelial cells.45 Additionally, the kidney plays an important role in regulating body water content, and patients with hypernatremia have a higher incidence of acute kidney injury (AKI).46 Furthermore, patients with hypernatremia had more severe AKI, and the severity of AKI was directly related to a greater risk of mortality.47 Studies have found that the increase of serum creatinine was closely related to the progression of severe hypernatremia.35 At the time of hypernatremia, patients are usually still being treated with normal saline, which may worsen the hypernatremia.12 However, we also recognized that there were many reasons for elevated serum creatinine that might not be explained. In a previous study, our group found that hypernatremia in patients with sepsis was independently related to an increased risk of AKI and might predict AKI.48 Some studies suggested a strong and independent link between hypernatremia, elevated blood sodium levels, and the risk of developing AKI.49 Mendes et al identified pre dialysis hypernatremia as a prognostic indicator of AKI requiring renal replacement therapy.50
Hypernatremia is also common in infectious diseases. One of the complications of COVID-19 is fluid and electrolyte imbalance. The most common of these disorders are hyponatremia, hypernatremia, hypokalemia, hypocalcemia, hypochloremia, hypervolemia, and hypovolemia, which may increase mortality if left untreated.51,52 Hypernatremia was seen in patients with community-acquired pneumonia and was found to be independently linked with death, especially when water loss is corrected with inadequate fluid or relatively hypertonic fluid.53 Burn patients with hypernatremia have a higher mortality rate, and there is evidence that hypernatremia may worsen the burn itself.54 The serum sodium has also been demonstrated to be a reliable and valid predictor of mortality in patients with enterocutaneous fistula worsened by sepsis.55
The study also has some limitations. First, the study is retrospective and the grade of evidence is weak. Second, the study is a single-center study, limiting the generalizability of the findings. Finally, the number of patients included in this study is relatively small (n = 442). Although we have tried our best to control for bias and confounders by using multivariate models, many other known or unknown factors may still exist. Therefore, more experimental studies are required to confirm the current findings.
Conclusions
Our constructed nomogram confirmed that hypernatremia, CNa, septic shock, APACHE II score, hyperlactatemia, CRRT, and MV can be independent risk predictors of 28-day mortality in critically ill patients. Therefore, after building a personalized prediction model, we can intervene in advance for patients who present with large sodium concentration changes. Once high-risk patients are screened, we can intervene in advance.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article or are available from the corresponding author on reasonable request.
Ethics Approval
This study was approved by the Professional Committee on bioethics of Beijing Friendship Hospital (No. 2022-P2-083-01). All methods were carried out in accordance with relevant guidelines and regulations. Professional Committee on bioethics of Beijing Friendship Hospital waived the need to informed consent for this study.
Acknowledgments
The authors would like to thank the database search support provided by Beijing Friendship Hospital affiliated with Capital Medical University.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The study did not receive any specific funding from funding agencies in the public, commercial or non-profit sectors.
Disclosure
The authors declare that there are no conflicts of interest.
References
1. Hawkins RC. Age and gender as risk factors for hyponatremia and hypernatremia. Clin Chim Acta. 2003;337(1–2):169–172. doi:10.1016/j.cccn.2003.08.001
2. Frenkel WN, van den Born BJ, van Munster BC, Korevaar JC, Levi M, de Rooij SE. The association between serum sodium levels at time of admission and mortality and morbidity in acutely admitted elderly patients: a prospective cohort study. J Am Geriatr Soc. 2010;58(11):2227–2228. doi:10.1111/j.1532-5415.2010.03104.x
3. Waikar SS, Mount DB, Curhan GC. Mortality after hospitalization with mild, moderate, and severe hyponatremia. Am J Med. 2009;122(9):857–865. doi:10.1016/j.amjmed.2009.01.027
4. Upadhyay A, Jaber BL, Madias NE. Incidence and prevalence of hyponatremia. Am J Med. 2006;119(7 Suppl 1):S30–35. doi:10.1016/j.amjmed.2006.05.005
5. Sakr Y, Rother S, Ferreira AM, et al. Fluctuations in serum sodium level are associated with an increased risk of death in surgical ICU patients. Crit Care Med. 2013;41(1):133–142. doi:10.1097/CCM.0b013e318265f576
6. Funk GC, Lindner G, Druml W, et al. Incidence and prognosis of dysnatremias present on ICU admission. Intensive Care Med. 2010;36(2):304–311.
7. Darmon M, Diconne E, Souweine B, Ruckly S, Adrie C, Azoulay E. Prognostic consequences of borderline dysnatremia: pay attention to minimal serum sodium change. Crit Care. 2013;17(1):R12.
8. Jones DP. Syndrome of inappropriate secretion of antidiuretic hormone and hyponatremia. Pediatr Rev. 2018;39(1):27–35. doi:10.1542/pir.2016-0165
9. Lindner G, Funk GC. Hypernatremia in critically ill patients. J Crit Care. 2013;28(2):216.e211–220.
10. Darmon M, Timsit JF, Francais A, et al. Association between hypernatraemia acquired in the ICU and mortality: a cohort study. Nephrol Dial Transplant. 2010;25(8):2510–2515.
11. Tsipotis E, Price LL, Jaber BL, Madias NE. Hospital-Associated Hypernatremia Spectrum and Clinical Outcomes in an Unselected Cohort. Am J Med. 2018;131(1):72–82.e71. doi:10.1016/j.amjmed.2017.08.011
12. Sam R, Hart P, Haghighat R, Ing TS. Hypervolemic hypernatremia in patients recovering from acute kidney injury in the intensive care unit. Clin Exp Nephrol. 2012;16(1):136–146. doi:10.1007/s10157-011-0537-7
13. Hooper L, Abdelhamid A, Attreed NJ, et al. Clinical symptoms, signs and tests for identification of impending and current water-loss dehydration in older people. Cochrane Database Syst Rev. 2015;2015(4):Cd009647. doi:10.1002/14651858.CD009647.pub2
14. Sedlacek M, Schoolwerth AC, Remillard BD. Electrolyte disturbances in the intensive care unit. Semin Dial. 2006;19(6):496–501. doi:10.1111/j.1525-139X.2006.00212.x
15. Tinawi M, Bastani B. A mathematical approach to severe hyponatremia and hypernatremia in renal replacement therapies. Semin Dial. 2021;34(1):42–50. doi:10.1111/sdi.12918
16. Sterns RH. Disorders of plasma sodium--causes, consequences, and correction. N Engl J Med. 2015;372(1):55–65. doi:10.1056/NEJMra1404489
17. Shaffer C, Schaefer E. Early intensive care unit-acquired hypernatremia in severe sepsis patients receiving 0.9% saline fluid resuscitation. Acta Anaesthesiol Scand. 2014;58(8):1007–1014. doi:10.1111/aas.12368
18. Wald R, Jaber BL, Price LL, Upadhyay A, Madias NE. Impact of hospital-associated hyponatremia on selected outcomes. Arch Intern Med. 2010;170(3):294–302. doi:10.1001/archinternmed.2009.513
19. Rapsang AG, Shyam DC. Scoring systems in the intensive care unit: a compendium. Indian J Crit Care Med. 2014;18(4):220–228. doi:10.4103/0972-5229.130573
20. O’Donoghue SD, Dulhunty JM, Bandeshe HK, Senthuran S, Gowardman JR. Acquired hypernatraemia is an independent predictor of mortality in critically ill patients. Anaesthesia. 2009;64(5):514–520. doi:10.1111/j.1365-2044.2008.05857.x
21. Chauhan K, Pattharanitima P, Patel N, et al. Rate of Correction of Hypernatremia and Health Outcomes in Critically Ill Patients. Clin J Am Soc Nephrol. 2019;14(5):656–663. doi:10.2215/CJN.10640918
22. Borra SI, Beredo R, Kleinfeld M. Hypernatremia in the aging: causes, manifestations, and outcome. J Natl Med Assoc. 1995;87(3):220–224.
23. Marshall DC, Salciccioli JD, Goodson RJ, et al. The association between sodium fluctuations and mortality in surgical patients requiring intensive care. J Crit Care. 2017;40:63–68.
24. Lombardi G, Ferraro PM, Calvaruso L, Naticchia A, D’Alonzo S, Gambaro G. Sodium fluctuations and mortality in a general hospitalized population. Kidney Blood Press Res. 2019;44(4):604–614. doi:10.1159/000500916
25. Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315(8):801–810. doi:10.1001/jama.2016.0287
26. Rouzier R, Pusztai L, Delaloge S, et al. Nomograms to predict pathologic complete response and metastasis-free survival after preoperative chemotherapy for breast cancer. J Clin Oncol. 2005;23(33):8331–8339. doi:10.1200/JCO.2005.01.2898
27. Annane D, Bellissant E, Bollaert PE, Briegel J, Keh D, Kupfer Y. Corticosteroids for treating sepsis. Cochrane Database Syst Rev. 2015;2015(12):Cd002243. doi:10.1002/14651858.CD002243.pub3
28. Annane D, Bellissant E, Bollaert PE, et al. Corticosteroids for treating sepsis in children and adults. Cochrane Database Syst Rev. 2019;12(12):Cd002243. doi:10.1002/14651858.CD002243.pub4
29. Fang F, Zhang Y, Tang J, et al. Association of corticosteroid treatment with outcomes in adult patients with sepsis: a systematic review and meta-analysis. JAMA Intern Med. 2019;179(2):213–223. doi:10.1001/jamainternmed.2018.5849
30. Lindner G, Funk GC, Lassnigg A, et al. Intensive care-acquired hypernatremia after major cardiothoracic surgery is associated with increased mortality. Intensive Care Med. 2010;36(10):1718–1723. doi:10.1007/s00134-010-1968-4
31. Eckart A, Hausfater P, Amin D, et al. Hyponatremia and activation of vasopressin secretion are both independently associated with 30-day mortality: results of a multicenter, observational study. J Intern Med. 2018;284(3):270–281. doi:10.1111/joim.12764
32. Tzoulis P, Bagkeris E, Bouloux PM. A case-control study of hyponatraemia as an independent risk factor for inpatient mortality. Clin Endocrinol (Oxf). 2014;81(3):401–407. doi:10.1111/cen.12429
33. Corona G, Giuliani C, Parenti G, et al. Moderate hyponatremia is associated with increased risk of mortality: evidence from a meta-analysis. PLoS One. 2013;8(12):e80451. doi:10.1371/journal.pone.0080451
34. Cuesta M, Garrahy A, Slattery D, et al. Mortality rates are lower in SIAD, than in hypervolaemic or hypovolaemic hyponatraemia: results of a prospective observational study. Clin Endocrinol (Oxf). 2017;87(4):400–406. doi:10.1111/cen.13388
35. Ranjan R, Lo SC, Ly S, Krishnananthan V, Lim AKH. Progression to severe hypernatremia in hospitalized general medicine inpatients: an observational study of hospital-acquired hypernatremia. Medicina. 2020;56:7.
36. Vedantam A, Robertson CS, Gopinath SP. Morbidity and mortality associated with hypernatremia in patients with severe traumatic brain injury. Neurosurg Focus. 2017;43(5):E2. doi:10.3171/2017.7.FOCUS17418
37. Li M, Hu YH, Chen G. Hypernatremia severity and the risk of death after traumatic brain injury. Injury. 2013;44(9):1213–1218. doi:10.1016/j.injury.2012.05.021
38. Ryu JH, Walcott BP, Kahle KT, et al. Induced and sustained hypernatremia for the prevention and treatment of cerebral edema following brain injury. Neurocrit Care. 2013;19(2):222–231. doi:10.1007/s12028-013-9824-3
39. Peres LA, Wandeur V, Matsuo T. Predictors of acute kidney injury and mortality in an Intensive Care Unit. J Bras Nefrol. 2015;37(1):38–46. doi:10.5935/0101-2800.20150007
40. De Freitas G, Gudur A, Vela-Ortiz M, Jodelka J, Livert D, Krishnamurthy M. Where there is sodium there may be sepsis. J Community Hosp Intern Med Perspect. 2019;9(4):296–299. doi:10.1080/20009666.2019.1634407
41. Beseoglu K, Etminan N, Steiger HJ, Hänggi D. The relation of early hypernatremia with clinical outcome in patients suffering from aneurysmal subarachnoid hemorrhage. Clin Neurol Neurosurg. 2014;123:164–168.
42. Mulvany MJ. Small artery remodelling in hypertension. Basic Clin Pharmacol Toxicol. 2012;110(1):49–55. doi:10.1111/j.1742-7843.2011.00758.x
43. Touyz RM, Briones AM. Reactive oxygen species and vascular biology: implications in human hypertension. Hypertens Res. 2011;34(1):5–14. doi:10.1038/hr.2010.201
44. Martinez-Lemus LA, Hill MA, Meininger GA. The plastic nature of the vascular wall: a continuum of remodeling events contributing to control of arteriolar diameter and structure. Physiology. 2009;24:45–57.
45. Tabary O, Escotte S, Couetil JP, et al. High susceptibility for cystic fibrosis human airway gland cells to produce IL-8 through the I kappa B kinase alpha pathway in response to extracellular NaCl content. J Immunol. 2000;164(6):3377–3384. doi:10.4049/jimmunol.164.6.3377
46. Chassagne P, Druesne L, Capet C, Ménard JF, Bercoff E. Clinical presentation of hypernatremia in elderly patients: a case control study. J Am Geriatr Soc. 2006;54(8):1225–1230. doi:10.1111/j.1532-5415.2006.00807.x
47. Kellum JA, Lameire N. Diagnosis, evaluation, and management of acute kidney injury: a KDIGO summary (Part 1). Crit Care. 2013;17(1):204. doi:10.1186/cc11454
48. Zhi D, Lin J, Dong L, et al. Risk predictive role of hypernatremia for occurrence of sepsis-induced acute kidney injury. Ann Palliat Med. 2021;10(4):4705–4715. doi:10.21037/apm-21-792
49. Lombardi G, Ferraro PM, Naticchia A, Gambaro G. Serum sodium variability and acute kidney injury: a retrospective observational cohort study on a hospitalized population. Intern Emerg Med. 2021;16(3):617–624. doi:10.1007/s11739-020-02462-5
50. Mendes RS, Soares M, Valente C, Suassuna JH, Rocha E, Maccariello ER. Predialysis hypernatremia is a prognostic marker in acute kidney injury in need of renal replacement therapy. J Crit Care. 2015;30(5):982–987. doi:10.1016/j.jcrc.2015.05.023
51. Zimmer MA, Zink AK, Weißer CW, et al. Hypernatremia-A Manifestation of COVID-19: a Case Series. A a Pract. 2020;14(9):e01295. doi:10.1213/XAA.0000000000001295
52. Pourfridoni M, Abbasnia SM, Shafaei F, Razaviyan J, Heidari-Soureshjani R. Fluid and Electrolyte Disturbances in COVID-19 and Their Complications. Biomed Res Int. 2021;2021:6667047.
53. Krüger S, Ewig S, Giersdorf S, et al. Dysnatremia, vasopressin, atrial natriuretic peptide and mortality in patients with community-acquired pneumonia: results from the German competence network CAPNETZ. Respir Med. 2014;108(11):1696–1705.
54. Namdar T, Siemers F, Stollwerck PL. Increased mortality in hypernatremic burned patients. Ger Med Sci. 2010;8:5185.
55. Wu Y, Ren J, Wang G, et al. Serum Sodium: a Reliable and Validated Predictor for Mortality in Enteric Fistula Patients Complicated with Sepsis. J Invest Surg. 2015;28(3):131–139. doi:10.3109/08941939.2014.957880
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


