Back to Journals » Pediatric Health, Medicine and Therapeutics » Volume 11
Newborn Care Practices and Associated Factors Among Lactating Mothers at Home in the Rural Districts of Gedeo Zone, Southern Ethiopia
Received 29 September 2019
Accepted for publication 25 January 2020
Published 11 February 2020 Volume 2020:11 Pages 47—54
DOI https://doi.org/10.2147/PHMT.S232860
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Roosy Aulakh
Abebe Alemu,1 Akine Eshete2
1Department of Midwifery, College of Medicine and Health Sciences, Wachemo University, Hossana, Ethiopia; 2Department of Public Health, College of Medicine and Health Sciences, Dilla University, Dilla, Ethiopia
Correspondence: Abebe Alemu
Department of Midwifery, College of Medicine and Health Sciences, Wachemo University, PO. Box: 667, Hossana, Ethiopia
Tel +251 913672730
Email [email protected]
Introduction: Globally, approximately three million neonates die in the first month of life. Neonatal mortality is a public problem in low and middle-income counties. Home-based good newborn care practice by lactating mothers is vital to improve newborns’ health. In Ethiopia, home-based cultural newborn care practice among lactating mothers is very common, in contrast to standard essential newborn care practice. Thus, this study aimed to assess home-based newborn care practices among lactating mothers and associated factors in rural districts of Gedeo Zone, Southern Ethiopia, in 2018.
Methods: A community-based cross-sectional study was conducted in the rural districts of Gedeo Zone, Southern Ethiopia. A single population formula was used to determine the sample size, and 834 lactating mothers were enrolled in the study. Multistage sampling techniques were used to select study participants. Data were collected using a pre-tested interviewer-administered structured questionnaire and analyzed by SPSS version 22 software (IBM Corporation, Armonk, NY, USA). To determine associated factors with good newborn care practice among lactating mothers, the odds ratio with 95% confidence interval was used.
Results: The level of good newborn care practice among lactating mothers at home was 24.1% with 95% CI: 2.5– 9.7. The factors significantly associated were maternal education (adjusted OR=2.6; 95% CI: 1.8– 3.9), maternal employment (adjusted OR=2.1; 95% CI: 1.4– 3.1), pregnancy intention (adjusted OR=1.7, 95% CI: 1.2– 2.2), antenatal care visit (adjusted OR=5.7, 95% CI 3.9– 7.9), and birth interval (adjusted OR=1.9, 95% CI: 1.3– 2.8).
Conclusion: The level of good newborn care practices among lactating mothers at home was found to be low. Thus, advancing women’s education and employment in the community, and providing quality prenatal care are suggested to scale up good newborn care practice among lactating mothers at home. Additionally, an observational study might be needed to identify further associated factors.
Keywords: newborn care practice, lactating mothers, home, Ethiopia
Background
Globally, approximately three million babies die in the first month of life; one million of these newborns die on the first day of life, which makes up 40% of the under-five mortality. The Ethiopian government implemented the “Health Extension Program” to improve health care at the community level through transfer of knowledge and skill to the household.1–3
According to the World Health Organization (WHO) findings on trends in child and maternal mortality, despite falling under-five mortality, there has been very little change in the neonatal mortality rate (NMR). The NMR fell from 36 per 1000 live births in 1990 to 19 in 2015, and the number of neonatal deaths declined from 5.1 million to 2.7 million.4–6
Ethiopia has achieved its Millennium Development Goal-4 targets, but newborn deaths have declined more slowly. In spite of many efforts applied by the government and other partner organizations, a sluggish decline has been achieved in the NMR.7 The NMR (per 1000 live births) was 61 in 1990 and 28 in 2015. A survey at the household level revealed that the neonatal mortality ratio was 27 per 1000 live births, which accounts for 308 neonatal deaths.3–8
Neonatal mortality is becoming progressively a public problem. The essential newborn care interventions have been applied to reduce under-five children deaths, but do not yet completely address the causes of the under-five children's deaths.2,5,9
According to the Ethiopian Demographic Health Survey 2014, newborns who received postnatal care within the first two days of birth are only 12%.10 The literature revealed that socioeconomic, demographic characteristics, good newborn care, and cultural practices were important determinants of neonatal mortality.11–13
Practicing effective interventions can avert neonatal mortality and quality care during the pre-pregnancy, antenatal, intrapartum, and postnatal period is vital to ensure the reduction of neonatal mortality.14,15 Good newborn care practices are one of the strategies to improve newborn health.16,17 For all newborns, clean delivery and cord care, thermal protection, early and exclusive breastfeeding, and immunization are recommended by the WHO.18–20
In low and middle-income countries, there were different cultural newborn care practices at home which are in contrast to WHO recommendations. Culturally sensitive newborn care practice is important to assure the quality of service and well-being of newborns.20,21
The literature findings have shown that newborn care practices were associated with maternal age, maternal education, parity, antenatal care visit, place of delivery, mothers’ cultural practices, maternal decision-making, and knowledge on newborn danger signs.22–25 In low and middle-income countries, studies have shown that home-based newborn care intervention can prevent 30–60% of newborn deaths, particularly in high mortality settings. Home-based good newborn care practice may improve the survival of the newborn.16,26–29
In Ethiopia, there are different home-based cultural newborn care practices among lactating mothers in contrast to WHO recommendations. However, little was known on home-based newborn care practices (exclusive breastfeeding, cord care, colostrum use, and baby bath) among lactating mothers and associated factors in the study area. Determining the level of good newborn care practice and associated factors among lactating mothers at home is important to complement essential newborn care practices and improve newborn survival. Thus, this study aimed to assess the level of good newborn care practice and associated factors among lactating mothers at home in the rural districts of Gedeo Zone, Southern Ethiopia, 2018.
Methods
Study Setting
The study was conducted in Gedeo Zone which is found in the Southern Nations and Nationalities of Peoples (SNNP) regional state of Ethiopia, and the zone has six rural districts. According to the 2007 census of Central Statistical Agency of Ethiopia report, the zone has a total population of 847,434, of whom 424,742 are men and 422,692 women.
Study Design, and Period
A community-based cross-sectional study was conducted among lactating mothers who have a baby of age less than or equal to six months in the rural districts of Gedeo Zone, Southern Ethiopia from April, 15 to May 15, 2018.
Source Population
All lactating mothers in the study area during data collection.
Study Population
All selected lactating mothers in the study area during data collection.
Sample Size Determination
The sample size was determined using a single population formula by considering: (p=55.6%) prevalence of newborn care practice among postnatal mothers, in Udupi District (30); 95% confidence interval, 5% margin of error and considering design effect=2, and non-response rate of 10%. Finally, the total sample size was 834.
Sampling Technique
A multistage sampling technique was used to select and enroll a total of 834 lactating mothers with babies aged less than six months in Gedeo Zone, Southern Ethiopia. In Gedeo Zone, there are six rural districts. Three rural districts were selected by a simple random method and, then, from each rural district, six kebeles were selected randomly. The sample size was distributed proportionally to the selected kebeles. The study participants were framed from registration books of health extension workers in the corresponding kebeles. Study participants were selected by simple random sampling techniques at the household level.
Data Collection Tool and Quality Assurance
Data were collected using a pre-tested interviewer-administered structured questionnaire. The questionnaire was adopted from related literature28,29 and translated into the local language. It contains socio-demographic information, obstetrics characteristics, and newborn care practice. The instrument validity was assured by applying validity criteria and reliability assured by the stability of responses of participants under similar situations. Data were collected by nine Diploma Nurses. To assure data quality, training was given for data collectors. The principal investigators were supervised and cheeked the questionnaires for completeness daily.
Ethics Statement
Ethical approval was obtained from the Research and Ethics Review Committee of the College of Health Sciences, Dilla University. A formal letter was obtained from Zonal and District Health Bureaus. The participants were informed about the purpose, procedures, and benefits of the study. Written informed consent was obtained from the participants. The information obtained was kept anonymous, thereby ensuring confidentiality. The study participants were ensured that refusal or withdrawal from the study would not put at risk their access to care.
Data Analysis
Data were entered into Epi-INFO version 7 software and exported to Statistical Package for Social Science (SPSS) version 22 software (IBM Corporation, Armonk, NY, USA) for analysis. Descriptive statistics were done and the results presented using tables. Bivariable and multivariable logistic regression analyses were used to determine the association of the independent variables with the outcome variable. Explanatory variables with p<0.25 on bivariate logistic regression analyses were booked into the multivariable logistic regression model. The degree of association between independent and dependent variables was assessed using odds ratio with 95% confidence interval. Finally, variables with p<0.05 on the multivariable logistic regression analysis model were declared statistically significant with the outcome variable. The model fitness was checked using Pearson’s chi-square with a value of 4.341 and significance of 0.037.
Inclusion and Exclusion Criteria
Mothers who have a baby age less than or equal to six months were included and those mothers who were too critically ill to practice newborn care were excluded.
Operational Definitions and Descriptions
Good newborn care practice among lactating mothers at the household level during the postnatal period was operationalized using four newborn care practices. These four components are adopted from essential newborn practice standards. These four components were selected because of their practicality by lactating mothers at home irrespective of the place of delivery [Table 1].
 |
Table 1 Operational Definition and Description of Explanatory Variables |
Study Variables
The dependent variable in this study was newborn care practice among lactating mothers and the independent variables were categorized as respondents’ socio-demographic characteristics, obstetrics characteristics, and newborn care practices.
Results
All study participants responded to the questionnaires, which made a response rate of 100%. The mean age of respondents was 28.6 (±4.8) years. Four hundred and nighty-five (59.4%) respondents cannot read and write, and six hundred and thirty-six (76.3%) were non-employed [Table 2].
 |
Table 2 Socio-Demographic Characteristics of Respondents in the Rural Districts of Gedeo Zone, Southern Ethiopia, 2018 [n=834] |
Respondents’ Obstetric Characteristics
From the respondents, six hundred and forty-six (77.5%) lactating mothers had an antenatal care (ANC) visit, but only one hundred and thirty-one (20.3%) of the mothers had booked their first ANC visit within first 16 weeks of pregnancy. Regarding the pregnancy plan, two hundred and thirty-one (27.7%) pregnancies were unplanned among study participants. Three hundred and seven (42.8%) of the mothers had their last birth by a birth interval of less than two years [Table 3].
 |
Table 3 Obstetric Characteristics of Respondents in the Rural Districts of Gedeo Zone, Southern Ethiopia, 2018 [n=834] |
Home-Based Newborn Care Practices Among Lactating Mothers
The prevalence of good newborn care practice among lactating mothers at home was 24.1% with 95% CI: 2.5–9.7. Four newborn cares of exclusive breastfeeding, colostrum using, baby bathing, and cord care were used to determine the level of newborn care practice among the lactating mothers at home. These four practices can be practiced by lactating mothers to all newborns at home to support newborn well-being irrespective of the place of delivery.
For each newborn care practice by mothers at home, the standard practice was scored “1”; but practice that diverges from the standard practice was scored “0”. The mothers who had practiced all newborn care as standard newborn care were categorized as good newborn care practice; but mothers who had not practiced were categorized as poor newborn care at home.
Four hundred and seventy-seven (57.2%) lactating mothers have practiced exclusive breastfeeding and one hundred and eighteen (14.1%) mothers gave colostrum for their newborn. Concerning newborn bathing, two hundred and fifty-two (30.2%) of the babies had a bath within the first 24 hrs of delivery [Table 4].
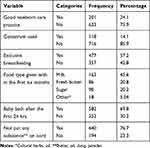 |
Table 4 Newborn Care Practices Among Lactating Mothers at Home in the Rural Districts of Gedeo Zone, Southern Ethiopia, 2018 [n=834] |
Factors Associated with Newborn Care Practices Among Lactating Mothers
Multivariable logistic regression analysis revealed that good newborn care practice was significantly associated with maternal education, employment, pregnancy plan, birth interval, and antenatal care.
Maternal education: educated mothers were 2.6 times higher (adjusted OR=2.6; 95% CI: 1.8–3.9) compared with non-educated mothers to have good newborn care practices.
Maternal employment: employed mothers were 2.1 times higher (adjusted OR=2.1; 95% CI: 1.4–3.1) compared with non-employed mothers to have good newborn care practice.
Antenatal care: mothers who had antenatal care follow-up were 5.7 times higher (adjusted OR=5.7, 95% CI: 3.9–7.9) compared with mothers who did not have antenatal care follow-up to have good newborn care practice.
Pregnancy intention: mothers who had planned pregnancy were 1.7 times higher (adjusted OR=1.7; 95% CI: 1.2–2.2) compared with mothers who had unplanned pregnancy to have good newborn care practice.
Birth interval: mothers who had birth interval greater than or equal to three years were 1.9 times higher (adjusted OR=1.9; 95% CI: 1.3–2.8) compared with mothers who had birth interval less than three years to have good newborn care practice [Table 5].
 |
Table 5 Factors Associated with Good Newborn Care Practice Among Lactating Mothers in Rural Districts Gedeo Zone, Southern Ethiopia, 2018 [n=834] |
Discussion
In this study, the prevalence of good newborn care practice among lactating mothers was 24.1% (95% CI: 2.5–9.7) in rural districts of Gedeo Zone, Southern Ethiopia. The finding of this study was lower as compared to previous studies in Northwest Ethiopia;11,27 however, the finding is higher than studyies conducted previously.22,30–33 This finding discrepancy might be due to the differences in socioeconomic status of mothers, study participants, and scoring parameters used to level good newborn practices.
In this study, maternal educational status was significantly associated with good newborn care practice among lactating mothers at home. The finding of this study was comparable with Ethiopian Demographic Health Survey results7 and other studies conducted in Tigray, Ethiopia, Uganda, Ghana, and India.25,28,30–36 This findings consistency might be due to educating women being a community and political concern in developing and developed countries in comparable commitment. Women's education is a universal agenda to be implemented as a prospective countries program and is playing a great role to have good newborn care practice among lactating mothers.
Maternal employment was a significantly associated factor with good newborn care among lactating mothers. This finding corresponds with study findings in Tigray and North Ethiopia.31,34 This might be that maternal employment helps mothers to improve their status in the community which means it empowers mothers to access education, health service care, decision-making, and economic independence. This directly and indirectly contributes to mothers having good newborn care at home.
Antenatal care follow-up was found to be a significantly associated factor for good newborn care practice among lactating mothers in this study. This study result corresponds with previously conducted studies in Ethiopia, Northern Ghana, and Nepal.11,22,33,34 However, a community-based study conducted in Uganda showed that antenatal care follow-up was not significantly associated with good newborn care among lactating mothers at home.25
These findings inconsistencies might be due to the difference in study participants, socio-demographic characteristics, and period.
Planned pregnancy was found to be a significantly associated factor with good newborn care practice among lactating mothers in the study area. This result is consistent with the previous studies' findings.24,25 When pregnancy is planned, the socioeconomic situation of mothers will be good and that may create an opportunity for mothers to access a good health service.
In this study, the birth interval was found to be a significantly associated factor with good newborn care practice among lactating mothers. This result was similar to a study done on cultural newborn practice among mothers in Indonesia;21 however, other studies revealed that the birth interval was not significantly associated with good newborn care practice in Uganda and Sri Lanka.24,37 Consequently, the difference in results might be due to differences in socio-demographic characteristics and health service utilization among study participants.
The study findings have programmatic implications meaning that providing good newborn care was expected from health professionals as per the World Health Organization recommendation. But, this study finding infers that to assure quality newborn care services, home-based good newborn care practice by lactating mothers was suggested. Thus, the findings of the study give the clue to develop the program to link institution-based service to home-based newborn care practices to sustain good newborn care as per the standard.
Strength and Limitation of the Study
As a strength, the study was one of the few studies conducted to assess newborn care among lactating mothers at home. The study also tried to show home-based newborn care practice by lactating mothers which might support the standard newborn care practice continuum.
The study also has limitations that should be considered while interpreting the findings. We used only four standard practices to determine the level of “good newborn care practice” that could be practiced by lactating mothers at home. The study was conducted at a point in time but it could be better to do an observational study to identify associated factors at the household level.
Conclusion
The prevalence of good newborn care practice among lactating mothers was found to be low. Improving women's education, employment, antenatal care follow-up, and family planning service is recommended to assure good newborn care practices among lactating mothers.
Abbreviations
ANC, antenatal care; BF, breastfeeding; EDHS, Ethiopian demographic and health survey; LBW, low birth weight; NMR, neonatal mortality rate; PMR, perinatal mortality rate; PROM, prolonged rupture of membranes; SNNPR, South Nations Nationalities Peoples; UNICEF, United Nation Children’s Fund; WHO, World Health Organization.
Ethics Statement
The study was conducted in accordance with the Declaration of Helsinki.
Data Sharing Statement
All relevant data are within the manuscript.
Acknowledgment
We would like to thank all our study respondents and supervisors for their contributions.
Disclosure
All authors declare that they have no competing interests.
References
1. Commission AU. 2014 Status Report on Maternal, Newborn & Child Health; 2014.
2. Dhaded SM, Somannavar MS, Vernekar SS, et al. Neonatal mortality and coverage of essential newborn interventions 2010–2013: a prospective, population-based study from low-middle income countries. Reprod Health. 2015;12 Suppl 2(2):S6.
3. MCEE-WHO Methods and Data Sources for Child Causes of Death 2000–2015; 2016 February.
4. WHO. Trends in maternal mortality: 1990 to 2013. Estimates by WHO,UNICEF, UNFPA, The World Bank and the United Nations Population Division. World Heal Organ [Internet]; 2014;56. Available from: http://apps.who.int/iris/bitstream/10665/112682/2/9789241507226_eng.pdf?ua=1.
5. You D, Hug L, Ejdemyr S, et al. Global, regional and national levels and trends in under fine mortality between 1990 and 2015: UN inter-Agency group. Lancet. 2015;386:2275–2286. doi:10.1016/S0140-6736(15)00120-8
6. Darmstadt GL, Shiffman J, Lawn JE. Advancing the newborn and stillbirth global agenda: priorities for the next decade. Arch Dis Child. 2015;100(Suppl 1):S13–S18. doi:10.1136/archdischild-2013-305557
7. ICF CSA (CSA) [Ethiopia] and. Ethiopia Demographic and Health Survey 2016: Key Indicators Report; 2016.
8. OECD. Health at a Glance 2011: OECD Indicators. OECD Publishing; 2011.
9. Lawn JE, Blencowe H, Oza S. Every newborn: progress, priorities, and potential beyond survival. Lancet. 2014;384(9938):189–2015. doi:10.1016/S0140-6736(14)60496-7
10. Central Statistical Agency. 2014 Ethiopia Mini Demographic and Health Survey (EMDHS); 2014 August:111.
11. Tegene T, Andargie G, Nega A, Yimam K. Newborn care practice and associated factors among mothers who gave birth within one year in Mandura District, Northwest Ethiopia Clinics in Mother and Child Health. Clin Mother Child Health. 2015;12(1):1–7.
12. Amolo L, Irimu G, Njai D. Knowledge of postnatal mothers on essential newborn care practices at the Kenyatta National Hospital: a cross sectional study. Pan Afr Med J. 2017;28(97). doi:10.11604/pamj.2017.28.97.13785
13. Asif M, Vishnu Bhat EM. Knowledge attitude and practice of neonatal care among postnatal mothers. J Curr Pediatr. 2010;14(2):147–152.
14. Mekonnen Y, Tensou B, Telake DS, et al. Neonatal mortality in Ethiopia: trends and determinants. BMC Public Health. 2013;13(483). doi:10.1186/1471-2458-13-483
15. Postnatal Care for Mothers and Newborns Highlights from the World Health Organization 2013 Guidelines; 2015 March:1–8.
16. World Health Organization/United Nations Childrens Fund. WHO/UNICEF Joint Statement: Home Visits for the Newborn Child: A Strategy to Improve Survival. WHO Libr. 1–8. 2009.
17. Mangham-Jefferies L, Pitt C, Cousens S, Mills A, Schellenberg J. Cost-effectiveness of strategies to improve the utilization and provision of maternal and newborn health care in low-income and lower-middle-income countries: a systematic review. BMC Pregnancy Childbirth. 2014;14(1):1–23. doi:10.1186/1471-2393-14-243
18. The World Health Organisation, Report P. Every newborn progress report. World Heal Organ (2015) EVERY NEWBORN Prog Rep MAY 2015 [Internet]; 2015 May. Available from: www.everynewborn.orgwww.everynewborn.org.
19. WHO. Postnatal care of the mother and newborn 2013. World Heal Organ [Internet]; 2013;1–72. Available from: http://apps.who.int/iris/bitstream/10665/97603/1/9789241506649_eng.pdf.
20. Temmerman M, Khosia R, Bhutta ZA, Bustreo F. Are we on the threshold of change towards a new global strategy for women’s, children’s and adolescents’ health. BMJ. 2015;351.
21. Sutan R, Berkat S. Does cultural practice affects neonatal survival- a case control study among low birth weight babies in Aceh Province, Indonesia. BMC Pregnancy Childbirth. 2014;14:1–13.
22. Saaka M, Iddrisu M. Patterns and determinants of essential newborn care practices in rural areas of Northern Ghana. Int J Popul Res. 2014;2014:1–10. doi:10.1155/2014/404387
23. Nalwadda CK, Waiswa P, Guwatudde D, Kerber K, Peterson S, Kiguli J. As soon as the umbilical cord gets off, the child ceases to be called a newborn”: sociocultural beliefs and newborn referral in rural Uganda. Glob Health Action. 2015;1:1–10.
24. Waiswa P, Peterson S, Tomson G, et al. Poor newborn care practices - a population based survey in eastern Uganda. BMC Pregnancy Childbirth. 2010;10(9). doi:10.1186/1471-2393-10-9
25. Ayiasi RM, Kasasa S, Criel B, Orach CG, Kolsteren P. Is antenatal care preparing mothers to care for their newborns? A community-based cross-sectional study among lactating women in Masindi, Uganda. BMC Pregnancy Childbirth. 2014;14(1):1–11. (). doi:10.1186/1471-2393-14-1
26. Darmstadt GL, Choi Y, Arifeen SE, et al. Evaluation of a cluster-randomized controlled trial of a package of community-based maternal and newborn interventions in Mirzapur, Bangladesh. PloS one. 2010;5(3).
27. Lassi ZS, Haider BA, Bhutta ZA. Community-based intervention packages for reducing maternal and neonatal morbidity and mortality and improving neonatal outcomes. Cochrane Database Syst Rev. 2010;11(11):CD007754.
28. Sitrin D, Guenther T, Waiswa P, et al. Improving newborn care practices through home visits: lessons from Malawi, Nepal, Bangladesh, and Uganda. Glob Health Action. 2015;8(1):1–12. doi:10.3402/gha.v8.23963
29. Callaghan-Koru JA, Seifu A, Tholandi M, et al. Newborn care practices at home and in health facilities in 4 regions of Ethiopia. BMC Pediatr. 2013;13:198. doi:10.1186/1471-2431-13-198
30. Castalino F, Nayak BS, Souza DA. Knowledge and practices of postnatal mothers on newborn care in tertiary care hospital of udupi district. Nitte Univ J Heal Sci. 2014;4(2):98–101.
31. Berhe M, Medhaniye AA, Kahsay G, Birhane E, Abay M. Essential neonatal care utilization and associated factors among mothers in public health facilities of Aksum Town, North Ethiopia, 2016. PLoS One. 2017;12(4):1–11. doi:10.1371/journal.pone.0175902
32. Sinha LN, Kaur P, Gupta R, Dalpath S, Goyal V, Murhekar M. Newborn care practices and home-based postnatal newborn care programme – Mewat, Haryana, India, 2013. West Pacific Surveill Response. 2014;5(3):22–29. doi:10.5365/wpsar.2014.5.1.006
33. Kebede A. Knowledge, practice and associated factors of newborn care among postnatal mothers at health centers, Bahir Dar City, Northwestern Ethiopia, 2016. BMC Res Notes. 2019;12(483). doi:10.1186/s13104-019-4501-z
34. Misgna HG, Gebru HB, Birhanu MM. Knowledge, practice and associated factors of essential newborn care at home among mothers in Gulomekada District, Eastern Tigray, Ethiopia, 2014. BMC Pregnancy Childbirth. 2016;16(1):1–8. doi:10.1186/s12884-016-0931-y
35. Mandal M, Ghosh A. Evaluation of awareness of neonatal care practices among postnatal mothers in a tertiary care hospital. Clin Obstet Gynecol Reprod Med. 2016;2. doi:10.15761/COGRM.1000159.
36. Sharafi R, Esmaeeli H. Knowledge assessment of neonatal care among postnatal mothers. Iran J Neonatol. 2013;4(1):28–31.
37. Dayaratne N, de Silva G. Knowledge on newborn care among postnatal mothers of term babies with birth weights 2.5 kg or more at the De Soysa Hospital for Women, Colombo and associated factors. Sri Lanka J. Child Heal. 2016;45(4):271–275. doi:10.4038/sljch.v45i4.8184
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
