Back to Journals » Patient Preference and Adherence » Volume 11
New insights into frequency and contents of fear of cancer progression/recurrence (FOP/FCR) in outpatients with colorectal carcinoma (CRC) receiving oral capecitabine: a pilot study at a comprehensive cancer center
Authors Hefner J, Berberich S, Lanvers E, Sanning M, Steimer A, Kunzmann V
Received 28 May 2017
Accepted for publication 25 July 2017
Published 14 November 2017 Volume 2017:11 Pages 1907—1914
DOI https://doi.org/10.2147/PPA.S142784
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Jochen Hefner,1 Sara Berberich,2 Elena Lanvers,3 Maria Sanning,2 Ann-Kathrin Steimer,2 Volker Kunzmann4
1Section of Psychosomatic Medicine, Department of Internal Medicine II, University of Wuerzburg, 2Faculty of Medicine, University of Wuerzburg, Bavaria, 3Children’s Hospital of the City of Cologne, North Rhine-Westphalia, 4Section of Clinical Oncology, Department of Internal Medicine II, University of Wuerzburg, Bavaria, Germany
Background: Fear of cancer progression/recurrence (FOP/FCR) is considered one of the most prevalent sources of distress in cancer survivors and associated with lower quality of life and functional impairment. Detailed measures of FOP/FCR are needed because little is known about the knowledge of FOP/FCR, its associations with the patient–doctor relationship, and the rate of adequate therapy. Colorectal cancer (CRC) is one of the most prevalent cancer entities, and oral capecitabine is widely prescribed as treatment. Therefore, we initiated a pilot study to expand the literature on FOP/FCR in CRC outpatients receiving capecitabine and to generate hypotheses for future investigations.
Methods: This study included 58 patients treated at a comprehensive cancer center. FOP/FCR was assessed with the Fear of Progression Questionnaire (FOP-Q-SF). Satisfaction with the relationships with doctors was assessed with the Patient–Doctor Relationship Questionnaire-9 (PRDQ-9). Levels of side effects were rated by the patients on a visual analog scale. Clinical data were extracted from the charts.
Results: A total of 19 out of 58 patients (36%) suffered from FOP/FCR according to our assessment. Levels of FOP/FCR seemed to be mostly moderate to high. Only four out of the 19 distressed patients (21%) were treated accordingly. Typical side effects of oncological treatment were associated with higher FOP/FCR. Satisfaction with doctor–patient relationships was not associated with FOP/FCR. Regarding single items of FOP/FCR, three out of the five most prevalent fears were associated with close relatives.
Discussion: FOP/FCR occurred frequently in more than one in three patients, but was mostly untreated in this sample of consecutive outpatients with CRC receiving oral capecitabine. In detail, most fears were related to family and friends. In addition to an unmet need of patients, our data indicate sources of distress not considered thus far. If replicated in larger studies, results may help to inform intervention development and improve patient care.
Keywords: oral anticancer drugs, colorectal cancer, fear of progression, screening for distress, comprehensive management
Introduction
Colorectal cancer (CRC) represents one of the most prevalent cancer entities in western countries. In the USA, CRC is the third most common cancer entity affecting patients of both genders with an estimated number of 135,000 new cases each year.1 In Germany, CRC constitutes the second and third most prevalent cancer entity in women and men, respectively. About 27,270 German women and 33,370 German men were diagnosed with CRC in 2013.2 During the last decades, the survival time of CRC patients could be substantially prolonged so that today, almost two-thirds of CRC survivors live more than 5 years after their first diagnosis.3 The majority of CRC patients undergo surgery. In case of the tumor having invaded the bowel wall deeply or having metastasized to lymphatic nodes, broadly active chemotherapy is administered to most patients despite advantages regarding targeted or immune therapies.1 In fact, chemotherapy protocols based on 5-fluorouracil (5-FU; F. Hoffmann-La Roche AG, Basel, Switzerland) are expected to constitute the backbone of drug treatment for patients with CRC for the upcoming years.4–6 Usually administered intravenously, 5-FU leads to a range of side effects typical for drugs acting non-specifically on fast growing cells.7 With the prodrug capecitabine (Xeloda®; F. Hoffmann-La Roche AG) converting predominantly to 5-FU within tumors, not only the spectrum but also the magnitude of side effects could be reduced. Furthermore, capecitabine can be conveniently administered orally and thus stands in contrast to many other drugs for cancer chemotherapy.7 However, despite these fundamental research progresses made on the somatic side, still much less is known about psychological distress in patients with CRC receiving oral capecitabine, especially in the form of fear of cancer recurrence (FCR). Fear of cancer progression/recurrence (FOP/FCR) is described as “fear, worry or concern about cancer returning or progressing”8,9 and is considered one of the most prevalent sources of distress in cancer survivors.10,11 It associates with lower quality of life and higher levels of anxiety and depression and also with functional impairment.11–15 A recent publication of secondary analyses within a large-scale CRC survey with nearly 11,000 patients revealed that about one half was distressed by FOP/FCR.16 Furthermore, associations were found between FOP/FCR and younger age, female gender, use of chemotherapy, shorter time after treatment, and maladaptive health behaviors.16 In another study with about 900 patients, van de Wal et al concluded that factors like emotional well-being or quality of life might play a greater role for developing or not developing FOP/FCR than demographic or medical factors.17 In a qualitative approach, Mutsaers et al have recently revealed that “feeling alone” seems to be a feature of FOP/FCR in a sample of patients with mixed cancer types.18 On the other hand, the feeling of being understood by relevant people may help to adapt to FOP/FCR.10,19–21 From several publications, it is known that a close, trustworthy relationship between patient and doctor allowing open communication helps to alleviate fear and distress.22,23 These results inspired us to launch a pilot study on FOP/FCR in outpatients with CRC receiving oral capecitabine. Our interest focused on the prevalence and contents of FOP/FCR and further on the associations made with the perceived quality of doctor–patient relationships. We chose a real-world setting at an outpatient clinic of a comprehensive cancer center and in its associated clinics and doctors’ offices in order to get a first impression of the respective daily routine.
Materials and methods
Design
A prospective and descriptive design was adopted for this explorative study. The data set used in this study was part of a broader scientific approach where CRC outpatients receiving oral capecitabine were screened for distress, doctor–patient relationships, and adherence (Hefner et al, in preparation). In this article, we introduce a corresponding subgroup analysis.
Setting and ethical issues
All participants were recruited from the comprehensive cancer center of the Medizinische Klinik und Poliklinik II of the University of Wuerzburg. About 4,000 oncological outpatients are treated at this facility every year by multidisciplinary teams consisting of specialists of hematology/oncology and psychosomatic medicine at the local cancer outpatient clinic, the associated outpatient clinics, and the doctors’ offices in Wuerzburg, Kitzingen, Lohr, and Schweinfurt (all located about 30 km away).
Patient study requirements comprised documented CRC and treatment with oral capecitabine. Major exclusion criteria included age under 18 years, need of inpatient treatment, obvious intellectual impairment, and insufficient knowledge of the German language. All subjects were informed about the aims of the study and gave written informed consent before enrollment. After consenting, the participants were asked to complete their questionnaires. All patients were briefed about the psycho-oncological support program provided by the hospital. Patient assessments had a mean duration of 15 minutes and were performed in a separate room at the outpatient clinic in order to provide privacy and confidentiality. The study was approved by the Ethics Committee for Medical Research in Wuerzburg, Germany, in accordance with the Declaration of Helsinki.
Measures
Sociodemographic data
Sociodemographic data including age, gender, marital status, and education were obtained using an established questionnaire.24
Fear of cancer progression/recurrence
FOP/FCR was assessed by the 12-item short form of the Fear of Progression Questionnaire (FOP-Q-SF).25,26 The FOP-Q-SF is a reliable instrument to measure fear of progression in chronically ill patients.25,26 The FOP-Q-SF shows high internal consistency (Crohnbach’s α=0.87) and has been used in different cancer settings before to assess levels and content of FOP/FCR.27,28
The 12 items of the FOP-Q-SF comprise four scales of the original FOP-Q: affective reactions, partnership/family, occupation, and loss of autonomy.25,26,29 Levels of fear are assessed on a 5-point Likert scale ranging from 1 (never) to 5 (very often) and summed up with higher values indicating higher levels of FOP.25 We used a sum score of 34 as a cutoff point for existing FOP/FCR.29–31 Levels of FOP/FCR were labeled as “moderate” if patients ticked off 4 or 5 in at least 50% of all items. Levels of FOP/FCR were considered as “high” if patients ticked off these numbers in at least 75% of all items.32,33
The topic of treatment costs was not dealt with in this questionnaire because of the full monetary treatment coverage by the German health care system and hence remained disregarded.
Patient–doctor relationship
The 9-item Patient-Doctor Relationship Questionnaire-9 (PDRQ-9) is utilized to assess the patients’ perception of their relationship with the doctor.34 Core items of the PDRQ-9 are perceptions of a trustworthy, communicative relationship with an effective and helpful health professional.34 Answers are rated using a 5-point scale ranging from 1 (not at all) to 5 (totally). Higher scores express higher satisfaction.34 The instrument was validated in a primary care sample and a representative cross-sectional German population study.35,36 The internal reliability (Crohnbach’s α) of the total score was 0.95.36
Clinical data
Medical history as well as initial tumor staging and treatment modalities (adjuvant/palliative regimen, mono/combination therapy, time since treatment initiation) were assessed from the charts derived from the outpatient clinic database.
The patients’ specifications about current psychotherapeutic or psychopharmacological treatments were assessed. Furthermore, patients rated the current level of common side effects of capecitabine (diarrhea, fatigue, nausea, vomiting, fever or infection, hand-foot syndrome, and mucositis) on a visual analog scale (VAS 0–100).
Statistical analysis
The data were registered and analyzed using the Statistical Package for Social Sciences (SPSS for Windows, German version 22). All tests of significance were two-tailed, p-values of <0.05 were considered statistically significant.
For descriptive analysis, data are given here with mean values (M) and standard deviation (SD). Since the data did not follow a normal distribution, Spearman’s rank correlation was used when examining two independent metric variables. For tests of significance, mean differences of continuous variables among two subgroups were examined by the Mann–Whitney U test for independent samples. To examine the relationship between two independent categorical variables, Fisher’s exact test was performed.
Results
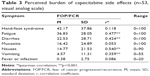
The sociodemographic and medical characteristics of the 53 patients analyzed are given in Tables 1 and 2. Mean age was 66 years, and 24% of the participants were female. Most patients were married (68%) and had been educated in main schools (64%) (Table 1). The most frequent treatment modality of capecitabine was an adjuvant regimen (64%). The remaining one third (36%) of the patients received capecitabine as a palliative treatment. The drug was most often used as a single agent (68%). In about one third (32%) of the cases, capecitabine was combined with other anticancer drugs. The mean time since the CRC diagnosis accounted for 14 months, and the mean time since the onset of capecitabine treatment amounted to 5 months (Table 2). The highest burden of current side effects resulted from hand-food syndrome (VAS 42), fatigue (VAS 37), and diarrhea (VAS 23) (Table 3).
FOP/FCR scores
The mean score of FOP/FCR within the total sample amounted to 31.00±9.00. Correlations between sociodemographic variables and FOP/FCR were not statistically significant (Table 4).
  | Table 4 FOP-Q-SF single-item responses and sum score (n=53) |
In regard to clinical variables, FOP/FCR was significantly correlated with the side effects fatigue (r(53) =0.0477, p<0.001), diarrhea (r(53) =0.424, p<0.001), nausea (r(53) =0.540, p<0.001), and vomiting (r(53) =0.359, p<0.001). Although the burden of hand-foot syndrome was rated highest, this side effect was not significantly correlated with FOP/FCR. Mucositis and fever or infection were not much pronounced and also not significantly correlated with FOP/FCR (Table 3).
Furthermore, the FOP/FCR sum score was not significantly associated with time elapsed since the first CRC diagnosis or time elapsed since the onset of treatment with oral capecitabine. The FOP/FCR sum score in our sample was not associated with the type of capecitabine regimen (ie, adjuvant or palliative), or monotherapy, or combination therapy, respectively (Table 2).
Prevalence and levels of FOP/FCR
By applying the sum score of 34 as a cutoff value for a present FOP/FCR, 19 out of 53 patients (36%) were classified as distressed by FOP/FCR. Regarding FOP/FCR levels, 11 patients (21%) suffered from moderate levels of fear, whereas five patients (9%) suffered from high levels of FOP/FCR. Only four out of 19 patients classified as distressed (21%) received corresponding support in the form of psychotherapy or psychopharmacological treatment. One patient received a combination of both treatment modalities. Two other patients received psychotherapy or psychopharmacotherapy without being distressed according to the FOP-Q-SF.
FOP/FCR single-item analyses
The item no 11 “Worrying about what will happen to the family if something should happen to me” comprised the most pronounced fear (2.98±1.17) overall (Table 4). The relevance of actual fear about the course of disease ranked only in the fourth place (2.85±1.06), whereas three out of the five most prevalent items concerned relationships. As expected, the fear of side effects was among the top five items (2.91±1.81) as well. However, concerns regarding close relatives and friends were rated higher, too (Table 4).
PDRQ-9 scores
The sum score of the PDRQ-9 in our sample was 39.92±5.97 (Table 5). To our surprise, FOP/FCR was not associated with the assessment of patient–doctor relationships.
  | Table 5 PDRQ-9 single-item responses and sum score (n=53) |
Discussion
In the present sample of outpatients with CRC, we found that 36% out of 19 patients could be classified as distressed with FOP/FCR. Furthermore, most of these distressed patients (16 out of 19; 84%) stated moderate to high levels of FOP/FCR according to our screening method. Hence, we are able to support the above-mentioned findings that FOP/FCR is well prevalent in patients with CRC.16,37 But does it also represent an unmet need as has been repeatedly suggested in the literature?11,38–40 Only four of the 19 patients distressed by FOP/FCR (21%) received corresponding support in terms of psychotherapy or psychopharmacological treatment, and only one patient was treated with a combination of both, an approach considered adequate as an initial treatment for patients with moderate to severe major depressive disorder.41 Assuming that the prevailing distress had first appeared with the cancer diagnosis and considering further a mean time of 14 months since that diagnosis, even the other three patients who did receive support may have been undertreated according to the respective guidelines.41 Another possible explanation for the infrequent utilization is offered by recent reports indicating that only a part of distressed patients express a need for support.42,43 Unlike in other reports, most of our patients were males; and it is well known from other cancer entities that men are less likely to seek cancer support services.44,45 Therefore, we cannot rule out the possibility that psychosocial support had been initially offered but was turned down. On the other hand, all four patients receiving psycho-oncological support in our study were males. Only future studies including larger populations may reveal if the low rate of adequate psycho-oncological support indicates a lack of detection, a low rate of utilization or rather a male idiosyncrasy. Age, another sociodemographic variable, was not significantly associated with FOP/FCR in our sample. The strong correlations of FOP/FCR with younger age in prior reports on CRC and other cancer entities were assumedly linked with the care for young children or worries about the economic future in this stage of life.10,11 We can rule out these factors with near certainty in our sample, because mean age was 66 years with 81% of the patients having already retired and therefore being financially covered by social systems. There were no other significant correlations between sociodemographic variables and FOP/FCR in our sample. As expected, levels of FOP/FCR were significantly associated with typical side effects. We can only speculate why hand-foot syndrome was unrelated to FOP/FCR. Our patients might have been very well informed about how to deal with this side effect of capecitabine, one of the most prevalent ones.46 Furthermore, the hand-foot syndrome is, contrary to the other side effects, visible and treatable by the patients themselves.46 It is even thinkable that patients perceive this distinct side effect as a sign of an antitumor effect just like patients with graft-versus-host disease after allogenic stem cell transplantation often do.47 To answer these questions, more in-depth questioning in larger samples is surely required. We found no other associations of FOP/FCR with medical variables in our sample, a finding in line with prior reports.11 Contrary to our assumption, FOP/FCR was not associated with patients’ satisfaction regarding their relationships with their doctors, assessed with the PDRQ-9. In contrast, three out of five of the most prevalent fears were related to close relatives or friends. We consider this one of the major and rather unexpected findings of our pilot study. The latter, however, shows several limitations. The number of patients included is small despite the considerable size of our institution. As the single units of our comprehensive cancer center started to cooperate only recently, we may have not reached all qualified patients. Furthermore, we chose an opt-in strategy to address our patients. In detail, the questionnaires were introduced during a follow-up appointment at the respective outpatient clinic or doctor’s office. Patients were free to fill in the questionnaires during their visit. Due to organizational reasons, we could not obtain data on dropouts. But as more distressed patients tend not to fill in the questionnaires, the prevalence of FOP/FCR may be even higher than found here.11 Another limitation of the study is the cross-sectional design: older patients seem to be more resilient regarding FOP/FCR in such a way that it subsides more rapidly with time.48 Furthermore, levels of FOP/FCR are higher when triggered, for instance during control visits or checkups.37 With a mean of 5 months since the start of treatment and a mean age of 66 years in our population, FOP/FCR may have declined quickly in the course of disease and treatment. Though unconfirmed, we got the notion that FOP/FCR may be persistent as described in other reports.10,11,15,37 Our respective opinion as professional psycho-oncologists is based on the fact that FOP/FCR is obviously not adequately treated in most patients. This consideration leads to more general limitations of FOP/FCR studies. The construct of FOP/FCR is not incorporated in current diagnostic manuals such as ICD-10 or DSM-IV. Neither does a common definition of the construct exist nor cutoffs for clinical FOP/FCR relevance.11,37,48,49 With a growing number of cancer survivors every year, the need to cover this common ground is urgent. This observation holds especially true for the scientific community, where differences in definitions and measurement lead to results almost impossible to compare.11,48 For health care professionals screening for FOP/FCR, we aim at underlining the need of a focus on close personal relationships in CRC patients. To our opinion, the FoP-Q-SF is a valuable tool to provide this additional information. Unfortunately, validated versions are available only in German and Dutch.25,26,50
Assessing the patient–doctor relationship with the PDRQ-9 has its shortcomings, too. Our screening may have emphasized trust insufficiently, which seems to emerge as a major factor influencing worries and fears in cancer patients.22 As communication skills or deficits affect levels of distress one way or the other, a more focused approach on communication styles and techniques may have led to different findings.51
Support from family and friends may also transpire to be a two-sided matter: on the one hand, it may indeed help to alleviate psychological adjustment, but it may be perceived as a burden on the other hand, particularly when experienced as unhelpful and not understanding.18,52 Our patients worried about their loved ones. A somatic reason for this worry seems unlikely due to the absence of diagnosis of Lynch syndrome or Hereditary Non-Polyposis Colorectal Cancer (HNPCC), which both can pose a threat to lineal descendants due to genetic inheritance. However, on an emotional level, caregivers and friends may suffer even more from FOP/FCR than the patients.53 We did not investigate the levels of distress in personal surroundings, which in turn may have affected our patients.13,54,55 Hence, we suggest focusing more on communication styles of doctors and on levels of trust put in them as well as an enrollment of close relatives and friends in future studies of FOP/FCR in order to close a gap in the current literature on FOP/FCR in CRC survivors.14,22,51
Conclusion
To sum up, we show for the first time that FOP/FCR is considerably prevalent in a population of predominantly elder male outpatients with CRC receiving oral capecitabine. Due to a low rate of respective supportive treatment, these findings represent a substantial unmet need. Most distressing fears in our sample referred to relationships with family and friends. Relationships to medical professionals in our sample according to our assessment tool were far less relevant than originally thought.
Screening for FOP/FCR with elaborated questionnaires may help to initiate a tailored interdisciplinary management for CRC patients and relatives alike. The effectiveness of tailored interventions should be investigated in future studies.
Acknowledgments
Göbel E of Hospital of Kitzingen, Germany; Haas J and Schoettker B of Medical Office of Hematology-Oncology, Wuerzburg, Germany; Hupp E of Hospital of Lohr, Germany; and Reinel H of MVZ of Leopoldia Hospital, Schweinfurt, Germany cared for study patients.
Author contributions
All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
American Cancer Society. Cancer Facts & Figures 2016. Atlanta; 2017. Available from: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2016/cancer-facts-and-figures-2016.pdf. Accessed August 1, 2017. | ||
Robert Koch Institut. Krebsdaten; 2015. Available from: http://www.krebsdaten.de/Krebs/DE/Content/Krebsarten/Darmkrebs/darmkrebs_node.html. Accessed August 1, 2017. | ||
El-Shami K, Oeffinger KC, Erb NL, et al. American Cancer Society colorectal cancer survivorship care guidelines. CA Cancer J Clin. 2015;65(6):428–455. | ||
Carrillo E, Navarro SA, Ramirez A, et al. 5-Fluorouracil derivatives: a patent review (2012–2014). Expert Opin Ther Pat. 2015;25(10):1131–1144. | ||
Weinberg BA, Marshall JL, Hartley M, Salem ME. A paradigm shift from one-size-fits-all to tailor-made therapy for metastatic colorectal cancer. Clin Adv Hematol Oncol. 2016;14(2):116–128. | ||
McQuade RM, Stojanovska V, Bornstein JC, Nurgali K. Colorectal cancer chemotherapy: the evolution of treatment and new approaches. Curr Med Chem. 2017;24(15):1537–1557. | ||
Twelves C. Vision of the future: capecitabine. Oncologist. 2001;6(Suppl 4):35–39. | ||
Vickberg SM. The Concerns About Recurrence Scale (CARS): a systematic measure of women’s fears about the possibility of breast cancer recurrence. Ann Behav Med. 2003;25(1):16–24. | ||
Lebel S, Ozakinci G, Humphris G, et al. From normal response to clinical problem: definition and clinical features of fear of cancer recurrence. Support Care Cancer. 2016;24(8):3265–3268. | ||
Simonelli LE, Siegel SD, Duffy NM. Fear of cancer recurrence: a theoretical review and its relevance for clinical presentation and management. Psychooncology. 2016 Epub Jun 1. | ||
Simard S, Thewes B, Humphris G, et al. Fear of cancer recurrence in adult cancer survivors: a systematic review of quantitative studies. J Cancer Surviv. 2013;7(3):300–322. | ||
Llewellyn CD, Weinman J, McGurk M, Humphris G. Can we predict which head and neck cancer survivors develop fears of recurrence? J Psychosom Res. 2008;65(6):525–532. | ||
Mellon S, Northouse LL, Weiss LK. A population-based study of the quality of life of cancer survivors and their family caregivers. Cancer Nurs. 2006;29(2):120–131; quiz 132–133. | ||
Crist JV, Grunfeld EA. Factors reported to influence fear of recurrence in cancer patients: a systematic review. Psychooncology. 2013;22(5):978–986. | ||
Koch L, Jansen L, Brenner H, Arndt V. Fear of recurrence and disease progression in long-term (≥5 years) cancer survivors – a systematic review of quantitative studies. Psychooncology. 2013;22(1):1–11. | ||
Fisher A, Beeken RJ, Heinrich M, Williams K, Wardle J. Health behaviours and fear of cancer recurrence in 10 969 colorectal cancer (CRC) patients. Psychooncology. 2016;25(12):1434–1440. | ||
van de Wal M, van de Poll-Franse L, Prins J, Gielissen M. Does fear of cancer recurrence differ between cancer types? A study from the population-based PROFILES registry. Psychooncology. 2016;25(7):772–778. | ||
Mutsaers B, Jones G, Rutkowski N, et al. When fear of cancer recurrence becomes a clinical issue: a qualitative analysis of features associated with clinical fear of cancer recurrence. Support Care Cancer. 2016;24(10):4207–4218. | ||
Myers SB, Manne SL, Kissane DW, et al. Social-cognitive processes associated with fear of recurrence among women newly diagnosed with gynecological cancers. Gynecol Oncol. 2013;128(1):120–127. | ||
Janz NK, Hawley ST, Mujahid MS, et al. Correlates of worry about recurrence in a multiethnic population-based sample of women with breast cancer. Cancer. 2011;117(9):1827–1836. | ||
Liu Y, Perez M, Schootman M, Aft RL, Gillanders WE, Jeffe DB. Correlates of fear of cancer recurrence in women with ductal carcinoma in situ and early invasive breast cancer. Breast Cancer Res Treat. 2011;130(1):165–173. | ||
Hillen MA, de Haes HC, Smets EM. Cancer patients’ trust in their physician-a review. Psychooncology. 2011;20(3):227–241. | ||
Lehmann C, Koch U, Mehnert A. [Impact of the doctor-patient-communication on distress and utilization of psychosocial services among cancer patients. A review of the current literature]. Psychother Psychosom Med Psychol. 2009;59(7):e3–e27. German. | ||
Deck R, Röckelein E. Zur Erhebung soziodemographischer und sozialmedizinischer Indikatoren in den rehabilitationswissenschaftlichen Forschungsverbünden. DRV-Schriften. 1999;16:84–102. | ||
Herschbach P, Berg P, Dankert A, et al. Fear of progression in chronic diseases: psychometric properties of the Fear of Progression Questionnaire. J Psychosom Res. 2005;58(6):505–511. | ||
Mehnert A, Herschbach P, Berg P, Henrich G, Koch U. Fear of progression in breast cancer patients – validation of the short form of the Fear of Progression Questionnaire (FoP-Q-SF). Z Psychosom Med Psychother. 2006;52(3):274–288. | ||
Herschbach P, Dinkel A. Fear of progression. Recent Results Cancer Res. 2014;197:11–29. | ||
Mehnert A, Koch U, Sundermann C, Dinkel A. Predictors of fear of recurrence in patients one year after cancer rehabilitation: a prospective study. Acta Oncol. 2013;52(6):1102–1109. | ||
Koch L, Bertram H, Eberle A, et al. Fear of recurrence in long-term breast cancer survivors-still an issue. Results on prevalence, determinants, and the association with quality of life and depression from the cancer survivorship – a multi-regional population-based study. Psychooncology. 2014;23(5):547–554. | ||
Sarkar S, Sautier L, Schilling G, Bokemeyer C, Koch U, Mehnert A. Anxiety and fear of cancer recurrence and its association with supportive care needs and health-care service utilization in cancer patients. J Cancer Surviv. 2015;9(4):567–575. | ||
Hinz A, Mehnert A, Ernst J, Herschbach P, Schulte T. Fear of progression in patients 6 months after cancer rehabilitation – a validation study of the fear of progression questionnaire FoP-Q-12. Support Care Cancer. 2015;23(6):1579–1587. | ||
Mehnert A, Berg P, Henrich G, Herschbach P. Fear of cancer progression and cancer-related intrusive cognitions in breast cancer survivors. Psychooncology. 2009;18(12):1273–1280. | ||
Koch-Gallenkamp L, Bertram H, Eberle A, et al. Fear of recurrence in long-term cancer survivors – Do cancer type, sex, time since diagnosis, and social support matter? Health Psychol. 2016;35(12):1329–1333. | ||
Van der Feltz-Cornelis CM, Van Oppen P, Van Marwijk HW, De Beurs E, Van Dyck R. A patient-doctor relationship questionnaire (PDRQ-9) in primary care: development and psychometric evaluation. Gen Hosp Psychiatry. 2004;26(2):115–120. | ||
Porcerelli JH, Murdoch W, Morris P, Fowler S. The Patient-Doctor Relationship Questionnaire (PDRQ-9) in primary care: a validity study. J Clin Psychol Med Settings. 2014;21(3):291–296. | ||
Zenger M, Schaefert R, van der Feltz-Cornelis C, Brahler E, Hauser W. Validation of the Patient-Doctor-Relationship Questionnaire (PDRQ-9) in a representative cross-sectional German population survey. PLoS One. 2014;9(3):e91964. | ||
Custers JA, Gielissen MF, Janssen SH, de Wilt JH, Prins JB. Fear of cancer recurrence in colorectal cancer survivors. Support Care Cancer. 2016;24(2):555–562. | ||
Santin O, Murray L, Prue G, Gavin A, Gormley G, Donnelly M. Self-reported psychosocial needs and health-related quality of life of colorectal cancer survivors. Eur J Oncol Nurs. 2015;19(4):336–342. | ||
Thewes B, Brebach R, Dzidowska M, Rhodes P, Sharpe L, Butow P. Current approaches to managing fear of cancer recurrence; a descriptive survey of psychosocial and clinical health professionals. Psychooncology. 2014;23(4):390–396. | ||
Armes J, Crowe M, Colbourne L, et al. Patients’ supportive care needs beyond the end of cancer treatment: a prospective, longitudinal survey. J Clin Oncol. 2009;27(36):6172–6179. | ||
Gelenberg AJ, Freeman MP, Markowitz JC, et al. Practice Guideline for the Treatment of Patients with Major Depressive Disorder; 2010. Available from: https://psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/mdd.pdf. Accessed August 1, 2017. | ||
Faller H, Weis J, Koch U, et al. Perceived need for psychosocial support depending on emotional distress and mental comorbidity in men and women with cancer. J Psychosom Res. 2016;81:24–30. | ||
Faller H, Weis J, Koch U, et al. Utilization of professional psychological care in a large German sample of cancer patients. Psychooncology. 2017;26(4):537–543. | ||
McDowell ME, Occhipinti S, Ferguson M, Chambers SK. Prospective predictors of psychosocial support service use after cancer. Psychooncology. 2011;20(7):788–791. | ||
Dunn J, Ng SK, Holland J, et al. Trajectories of psychological distress after colorectal cancer. Psychooncology. 2013;22(8):1759–1765. | ||
Murugan K, Ostwal V, Carvalho MD, et al. Self-identification and management of hand-foot syndrome (HFS): effect of a structured teaching program on patients receiving capecitabine-based chemotherapy for colon cancer. Support Care Cancer. 2016;24(6):2575–2581. | ||
Zhang P, Chen BJ, Chao NJ. Prevention of GVHD without losing GVL effect: windows of opportunity. Immunol Res. 2011;49(1–3):49–55. | ||
Mosher CE, Winger JG, Given BA, Helft PR, O’Neil BH. Mental health outcomes during colorectal cancer survivorship: a review of the literature. Psychooncology. 2016;25(11):1261–1270. | ||
Simard S, Savard J. Screening and comorbidity of clinical levels of fear of cancer recurrence. J Cancer Surviv. 2015;9(3):481–491. | ||
Kwakkenbos L, van den Hoogen FH, Custers J, et al. Validity of the Fear of Progression Questionnaire – Short Form in patients with systemic sclerosis. Arthritis Care Res (Hoboken). 2012;64(6):930–934. | ||
van Vliet LM, Epstein AS. Current state of the art and science of patient-clinician communication in progressive disease: patients’ need to know and need to feel known. J Clin Oncol. 2014;32(31):3474–3478. | ||
Mellon S, Kershaw TS, Northouse LL, Freeman-Gibb L. A family-based model to predict fear of recurrence for cancer survivors and their caregivers. Psychooncology. 2007;16(3):214–223. | ||
Cohee AA, Adams RN, Johns SA. Long-term fear of recurrence in young breast cancer survivors and partners. Psychooncology. 2017;26(1):22–28. | ||
Bigatti SM, Steiner JL, Makinabakan N, Hernandez AM, Johnston E, Storniolo AM. Matched and mismatched cognitive appraisals in patients with breast cancer and their partners: implications for psychological distress. Psychooncology. 2012;21(11):1229–1236. | ||
Segrin C, Badger T, Sieger A, Meek P, Lopez AM. Interpersonal well-being and mental health among male partners of women with breast cancer. Issues Ment Health Nurs. 2006;27(4):371–389. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.