Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 8
Effect of eprosartan-based antihypertensive therapy on coronary heart disease risk assessed by Framingham methodology in Canadian patients with diabetes: results of the POWER survey
Authors Petrella R, Gill D, Berrou J
Received 13 December 2014
Accepted for publication 23 January 2015
Published 24 March 2015 Volume 2015:8 Pages 173—180
DOI https://doi.org/10.2147/DMSO.S79221
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ming-Hui Zou
Robert J Petrella,1–3 Dawn P Gill,2,3 Jean-Pascal Berrou4
On behalf of the POWER survey Study Group
1Departments of Family Medicine, Medicine (Cardiology) and Kinesiology, University of Western Ontario, London, ON, Canada; 2Aging, Rehabilitation and Geriatric Care Research Centre, Lawson Health Research Institute, London, ON, Canada; 3Department of Family Medicine and School of Health Studies, University of Western Ontario, London, ON, Canada; 4Abbott Products Operations AG, Allschwil, Switzerland
Objective: As part of the Physicians’ Observational Work on Patient Education According to their Vascular Risk (POWER) survey, we used Framingham methodology to examine the effect of an eprosartan-based regimen on total coronary heart disease (CHD) risk in diabetic patients recruited in Canada.
Methods: Patients with new or uncontrolled hypertension (sitting systolic blood pressure [SBP] >140 mmHg with diastolic blood pressure <110 mmHg) were identified at 335 Canadian primary care practices. Initial treatment consisted of eprosartan 600 mg/day, which was later supplemented with other antihypertensives as required. Outcomes included change in SBP at 6 months (primary objective) and absolute change in the Framingham 10-year CHD risk score (secondary objective).
Results: We identified an intention-to-treat diabetes population of 195 patients. Most diabetic patients were prescribed two or more antihypertensive drugs throughout the survey. Mean reductions in SBP and diastolic blood pressure were 20.8±14.8 mmHg and 9.5±10.7 mmHg, respectively. The overall absolute mean 10-year CHD risk, calculated using Framingham formulae, declined by 2.9±3.5 points (n=49). Average baseline risk was higher in men than women (14.8±8.6 versus 5.6±1.8 points); men also had a larger average risk reduction (4.2±4.3 versus 1.5±1.3 points). The extent of absolute risk reduction also increased with increasing age (trend not statistically significant).
Conclusion: Eprosartan-based therapy substantially reduced arterial blood pressure in our subset of diabetic patients; while there was a slight reduction in Framingham risk, there are indications from our data that both blood pressure control and the wider management of CHD risk in diabetic patients remains suboptimal in Canadian primary care.
Keywords: cardiovascular risk, hypertension, diabetes, eprosartan, Framingham
Introduction
The prevalences of hypertension and type 2 diabetes have increased in recent years;1 these trends will likely have contributed to the burden of morbidity associated with cardiovascular disease.2,3 The importance of the interplay between diabetes and blood pressure in determining risk for cardiovascular disease is reflected in the 2012 recommendations of the Canadian Hypertension Education Program (CHEP),4 which affirmed an arterial blood pressure target of 130/80 mmHg for patients with diabetes plus hypertension, rather than the target of 140/90 mmHg preferred for the generality of patients with high blood pressure.
Canadian advice acknowledges the need for individualized assessment of global cardiovascular risk and identifies a range of instruments that may be used for that purpose, including formulae and tables developed from the Framingham Heart Study.5
The participation of patients and primary care practices in Canada in the Physicians’ Observational Work on Patient Education According to their Vascular Risk (POWER) project enabled us to examine the effect of eprosartan-based therapy (EBT) on systolic blood pressure (SBP) and total coronary heart disease (CHD) risk.6 The present report examines those outcomes in the subset of Canadian patients who had a baseline diagnosis of type 2 diabetes.
Methods
POWER was an open-label, post-marketing surveillance survey of 6 months’ duration that recruited patients from Canada and from 15 other countries in Europe and the Middle and Far East. Cardiovascular risk assessment in Canada was based on Framingham methodology, as described in other reports.6,7
Physicians in Canada collected data for patients who: 1) had newly diagnosed hypertension (mean sitting SBP in the range of 140 to <180 mmHg, plus mean sitting diastolic blood pressure [DBP] <110 mmHg); or 2) had hypertension not adequately controlled by current therapy; or 3) had tolerability problems with other antihypertensive medications. The protocol specified that blood pressure, preferably derived from the mean of two readings, might be measured by whatever methods were regarded locally as reliable, accurate, and reproducible.
The primary in-survey treatment for high blood pressure was eprosartan at its recommended starting dose of 600 mg/day. Additional drugs could be introduced after 1 month if the blood pressure response to monotherapy was judged unsatisfactory. Choice of supplementary drugs was at the unrestricted discretion of individual physicians, though the protocol identified a preference for hydrochlorothiazide 12.5 mg/day where practicable and suitable. Physicians also had complete independence to implement additional measures (lifestyle or pharmacological) to reduce CHD risk in individual patients.
Ethical considerations
The design and conduct of POWER in Canada conformed with prevailing legislation and other requirements pertaining to the conduct of research in humans, and to generally acknowledged principles of good clinical practice. Institutional review board and/or ethics committee review and approval was sought and obtained as required. Informed written consent was obtained for all patients; as part of that process, all participants were advised that they were free to withdraw from the project at any time and for any reason (stated or unstated) without prejudice to their ongoing medical care.
Objectives
The primary endpoint of POWER was the absolute change in SBP in hypertensive patients treated with EBT for 6 months.
Secondary efficacy variables included the absolute change in the 10-year risk of “hard” CHD (ie, myocardial infarction and coronary death) assessed by Framingham® risk scoring from baseline to final visit.
Three complementary approaches were adopted to calculate the 10-year risk of developing “hard” CHD in the Canadian contingent:
- The recorded Framingham risk: physicians’ own Framingham risk estimate.
- The estimated Framingham risk as derived using the Framingham ready reckoner (ie, chart-derived estimates). Risk factors (age, sex, smoking status, SBP, and total and high-density lipoprotein [HDL] cholesterol) were recorded at each visit and Framingham risk was estimated using these data.
- The calculated Framingham risk was derived using formulae, according to the methods described in detail in the Appendix to the work of Wilson et al.8 Risk-factor data were also used for this method.
Statistics
The comparison of blood pressure, laboratory parameters, and Framingham score was performed using variance analysis (in cases of normality) and the Kruskal–Wallis or Wilcoxon tests (in cases of nonnormality) between the segmentation groups of sex and age classes.
Nominal qualitative variables were compared using the chi-squared test and Fisher’s exact test. Ordinal qualitative variables were compared using the Wilcoxon test, and quantitative variables were compared using analysis of variance and the Kruskal–Wallis test. Descriptive statistics were prepared for safety data on all patients who received at least one dose of EBT.
Results
A total of 1,385 patients were recruited at 335 centers in Canada, of whom 234 were identified as having type 2 diabetes at baseline; 195 of these patients were included in the intention-to-treat diabetes population (ITTDP). General demographic and blood pressure data for the overall intention-to-treat cohort (N=1,114) and the ITTDP appear in Table 1 and indicate that the ITTDP was older, heavier, and had higher average body mass index than the Canadian contingent as a whole, and contained a higher proportion of women. The ITTDP also had a noticeably lower total cholesterol:HDL cholesterol ratio than the overall Canadian population.
Baseline SBP was similar at all ages but DBP was substantially higher in younger patients (eg, 91.7±9.3 mmHg at 50–59 years versus 81.5±8.9 mmHg at >70 years; P<0.0001 by the Kruskal–Wallis test). As a result, pulse pressure (PP) increased considerably with age (71.8±12.9 mmHg at >70 years versus 62.5±14.9 mmHg at 50–59 years; P<0.0001 by the Kruskal–Wallis test).
Some 32% of the ITTDP had a record of microalbuminuria, the incidence of which increased nonsignificantly with age. Proteinuria and left ventricular hypertrophy at baseline were recorded in 11%–12% of patients and elevated plasma creatinine in 8.4%. Proteinuria displayed an age-related trend similar to that seen with microalbuminuria, whereas elevated creatinine was largely confined to patients aged >70 years. The percentages of patients with a history of ischemic stroke (P=0.07), transient ischemic attack (P=0.058), or coronary artery disease (P=0.01) increased with age, whereas women were more likely than men to have a history of congestive heart failure (8% versus 2%; P=0.05 by Fisher’s exact test).
Just over a quarter of the patients in the ITTDP (n=55; 28%) were prescribed initial monotherapy to control blood pressure; most patients (n=109; 56%) were given two or more drugs from the outset or had no specific data recorded (n=31; 16%). The proportion of patients receiving monotherapy at the conclusion of the survey was lower than at baseline (20.5% versus 28.2%), whereas the percentage of patients recorded as being prescribed two drugs or more increased to 68.2% and the percentage with no detailed record fell to 11.3% (n=22). Older patients were more likely than younger ones to be on multidrug combination therapy at the start of the study; this trend was less marked by the end of the study owing to an increase in the proportion of younger patients in receipt of polypharmacy.
Blood pressure trends during treatment
Mean baseline blood pressure was 153.4±12.4/86.8±11.3 mmHg; corresponding levels at 6 months were 132.8±13.6/ 77.5±7.5 mmHg. Mean reductions in SBP and DBP over the course of observation were therefore 20.8±14.8 and 9.5±10.7 mmHg, respectively. Mean PP was 66.6±15 mmHg at baseline and 55.4±13.2 mmHg at 6 months, but this average decline of 11.3±15.9 mmHg concealed a strong trend for PP to increase with age, which persisted throughout the survey. Thus, mean PP at baseline was ~10 mmHg higher in patients aged >70 years than in those aged 50–59 years, and similarly higher at 6 months.
Three-quarters (n=147) of the patients in the ITTDP were classified as “responders” to therapy at 6 months according to the following criteria: SBP <130 mmHg or ΔSBP >15 mmHg; or DBP <80 mmHg or ΔDBP >10 mmHg. The target blood pressure of SBP <130 mmHg plus DBP <80 mmHg was attained by 31.3% of patients (n=61) after 6 months.
Risk score trends during treatment
At the start of the study, 131 patients met the theoretical criteria for calculation of Framingham risk, but in practice, only 63 were eligible for assessment. Of the excluded 68 patients, 57 were ineligible owing to non-report of HDL cholesterol data (Figure 1). In light of the large number of ineligible patients, we have excluded “recorded” Framingham risk from our summary of results.
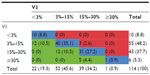
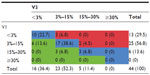
The overall mean Framingham risk score, calculated by formulae, was 10.2±7.7 at baseline, with a marked difference between the average values for men (14.8±8.6) and women (5.6±1.8; P<0.0001 by analysis of variance). The corresponding values after 6 months were: overall mean 7.9±5.7; men 11.5±6.4; women 4.5±1.4 (P<0.0001 for changes from baseline and for comparison of mean scores for men and women at 6 months). The risk distribution for men was less favorable than that for women at baseline and throughout the observation period, but there were no significant intersex differences for shifts in the risk distribution.
There was a marked age-related trend in baseline risk scores and on-treatment changes, as summarized in Table 2. There were no statistically significant differences in shifts in risk distribution stratified by age (data not shown).
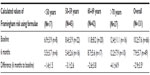  | Table 2 Absolute mean change (± standard deviation) of calculated Framingham coronary heart disease risk using formulae, stratified by age |
Cross-analyses based on chart- or formulae-derived Framingham scores identified a modest net improvement in risk distribution during the study, based on small patient numbers (Tables 3 and 4). By chart-based calculation, the biggest gains were seen in patients aged 50–59 years, whereas by formulae, the proportion of patients with at least one class reduction in Framingham status was highest in those aged >70 years (data not shown).
Additional risk factor observations
Examination of the relative contributions of changes in blood pressure, cholesterol, and smoking status among patients whose overall Framingham-calculated risk decreased (ie, improved) by at least one category during the survey indicated that lower blood pressure was considerably the largest single risk factor alteration associated with the reduction in CHD risk. Thus, a minimum of 66% of patients whose calculated Framingham risk score improved by at least one class had at least a one-category reduction in SBP, compared to an improvement in total cholesterol status in fewer than a quarter of those patients. Smoking rates were constant during the study, with only one patient reporting that they had ceased smoking.
In detail, mean total cholesterol declined from 184.0±40.8 mg/dL at baseline to 172.8±38.3 mg/dL at final visit – an absolute mean change of −13.8 mg/dL – while the total cholesterol:HDL cholesterol ratio changed from 1.6±0.5 to 1.5±0.3. In patients whose Framingham risk score was calculated by chart or formulae, 22.2% of patients registered a relevant decline in total cholesterol. No patient recorded a one-class or better improvement in total cholesterol:HDL cholesterol ratio when Framingham risk score was calculated by the same methods.
Safety findings
Seven suspected adverse drug reactions (SADRs) were recorded for five patients in the safety population of the type 2 diabetes subset (n=224). None of these SADRs were classified as serious or as severe, but six led to the discontinuation of four patients. Included in the discontinuations were two deaths due to myocardial infarctions in male patients aged 57 and 67 years, respectively. These fatalities were not attributed to use of the study drug and were therefore classified as serious and severe adverse events, but not as SADRs.
The seven SADRs consisted of one case each of palpitations, dysphagia, nausea, swelling (of the throat), hyperkalemia, paresthesia, and inefficacy.
Discussion
The principal findings from this exploratory substudy are broadly supportive of the benefits of EBT seen in the larger Canadian cohort of POWER6 and affirm the positive impact of blood pressure control on global CHD risk. Observations in this substudy are perhaps more interesting for the sidelight they shed on the management in Canadian general practice of patients who have both high blood pressure and type 2 diabetes, but the limited numbers of patients, especially for the calculation of Framingham risk, must at all times be kept in mind.
Levels of treatment and control of hypertension in Canada are regarded as being among the best reported from any country.9 However, rates of management and control in patients with hypertension plus diabetes appear to be one conspicuous exception to that opinion; the Ontario Survey on the Prevalence and Control of Hypertension (OSPCH) reported treatment and control of blood pressure to the target of <130/<90 mmHg in only 34.7% of patients with diabetes plus hypertension,9 with the remainder being either uncontrolled (37.4%) or untreated (27.9%). Our own data, in which 31.3% of patients reached that same blood pressure target, suggest that achieving optimal control of blood pressure in patients with diabetes continues to present challenges to Canadian physicians in primary care.
Approximately 17% of patients in the Canadian POWER contingent were diagnosed with both hypertension and diabetes at baseline, almost exactly the same percentage as in the OSPCH. Average blood pressure levels for patients classified as hypertensive were not reported in that study, but we surmise that the baseline levels recorded in our diabetes subset (153.4±12.4/86.8±11.3 mmHg) are indicative of a lack of blood pressure awareness since it seems implausible that patients already known to be hypertensive would remain untreated or, being treated, would be permitted to remain at such levels. The fact that most of the patients in our small cohort were treated with more than one drug indicates awareness among physicians of the need for combination therapy to control blood pressure in patients with diabetes; nevertheless, a fifth of patients received monotherapy only.
We made no investigation of whether doctors’ approaches to treatment of these patients were shaped by the view that attainment of either the 140/90 mmHg target usually specified for nondiabetic hypertensive patients or a reduction in SBP of at least 15 mmHg may be acceptable alternatives to a blood pressure target of <130/<80 mmHg. We have no data on patient adherence or persistence and are thus unable to comment on the contribution (if any) of those factors to the relative lack of success in attaining the blood pressure target of <130/<80 mmHg. The possible persisting contribution of masked hypertension to cardiovascular risk among patients with diabetes is another consideration.10 Nevertheless, examining the matter overall, we are inclined to agree with Liddy et al11 that preventive cardiology in Canadian primary care remains an arena of many missed opportunities. In this context we think it important to acknowledge the influence of other demographic factors operating within the Canadian population, notably the rise in obesity,1 which may have attenuated the response to risk factor intervention.12 The Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration13 provides another valuable perspective on this matter.
The only specified intervention in POWER was against blood pressure; in the context of diabetes, some observations on the EBT regimen used are appropriate. First, the treatment schedule was closely in alignment with CHEP guidance, which emphasizes initial treatment with an angiotensin-receptor blocker and a preference for hydrochlorothiazide as the first add-in drug.14 This is a combination likely to minimize any thiazide-induced hypokalemia and the associated loss of insulin sensitivity. Second, present evidence suggests that a 10 mmHg reduction in SBP is likely to be easier to achieve and more dependable for reducing stroke risk than lowering glycated hemoglobin.15 The efficacy of sartans in stroke risk reduction is documented16–18 but would not feature in the risk estimates from our Framingham instrument, as they did not represent cerebrovascular incidents. Similarly, there would be no representation of any renal benefits of sartan therapy in diabetic patients, as revealed in controlled trials.19–22 To some extent, therefore, the full scale of benefit from blood pressure control may be under-represented in our data.
Some 15%–20% of patients registered a one-class or more improvement in Framingham-calculated risk. Explanations for this modest percentage include ours being an intervention mostly on a single risk factor and the width of the high-risk band in the Framingham distribution.23 This is illustrated by the average risk score change among male patients: a reduction from >15 to ~11 meant that most of these patients started and finished the survey in the highest risk band even though their average absolute 10-year risk declined by >20%.23 All of our Framingham-based calculations were derived from a small sample and must be regarded as exploratory.
Data such as ours suggest that most of the observed reductions in CHD risk may be attributed to the intervention against blood pressure. We have no information about whether and to what extent physicians were motivated to initiate or review other elements of risk-factor modification, and we cannot infer that measures such as cholesterol control (by lifestyle or drugs) were optimal before the start of our survey. Further attention to these other risk factors, including glycated hemoglobin, would be expected to amplify the overall scale of risk reduction.
From this exploratory analysis of a cohort of Canadian patients with hypertension plus diabetes, we conclude that: 1) 6 months of EBT was associated with a substantial reduction in arterial blood pressure; and 2) Framingham instruments could be used successfully in primary care for the initial assessment of risk and to monitor the effect of therapy. However, attainment of blood pressure goals for these high-risk patients was difficult. Our experience is consistent with other reports in that management of diabetic patients with hypertension remains suboptimal in Canadian primary care, and it highlights both the importance of treating to targets and the need for multifactorial intervention.
Acknowledgments
The authors wish to thank the patients and fellow physicians who participated in the POWER survey in Canada. Preparation of this report was assisted by Hughes associates, Unit 103, 94 London Road, Oxford, OX3 9FN, UK. The POWER survey is supported financially by Abbott Products Operations AG, Hegenheimermattweg 127, 4123 Allschwil, Switzerland.
Author contributions
RJP and J-PB made substantial contributions to the conception or design of the project or the acquisition, analysis, or interpretation of data for the project. RJP and DG made substantial contributions to data analysis and interpretation. All named authors contributed to drafting the work or revising it critically for important intellectual content and approved the final version for submission for publication. All named authors undertook to be accountable for all aspects of the work in ensuring that questions relating to the accuracy or integrity of any part of the work were appropriately investigated and resolved.
Disclosure
RJP reports research grants from Pfizer, Astra-Zeneca, Novartis, Abbott, and Sanofi-Aventis, and honoraria from Abbott, Novartis, and Sanofi-Aventis for speaking engagements and symposia participation. J-PB is an employee of Abbott Products Operations AG, Allschwil, Switzerland, the sponsor of the POWER survey. DPG reports no conflicts of interest in this work.
References
Lee DS, Chiu M, Manuel DG, et al. Trends in risk factors for cardiovascular disease in Canada: temporal, socio-demographic and geographic factors. CMAJ. 2009;181(3–4):E55–E66. | |
Campbell NR, Leiter LA, Larochelle P, et al. Hypertension in diabetes: a call to action. Can J Cardiol. 2009;25(5):299–302. | |
Lee D, Goodman SG, Fox KA, et al. Prognostic significance of presenting blood pressure in non-ST-segment elevation acute coronary syndrome in relation to prior history of hypertension. Am Heart J. 2013; 166(4):716–722. | |
Daskalopoulou SS, Khan NA, Quinn RR, et al. The 2012 Canadian hypertension education program recommendations for the management of hypertension: blood pressure measurement, diagnosis, assessment of risk, and therapy. Can J Cardiol. 2012;28(3):270–287. | |
Grover SA, Hemmelgarn B, Joseph L, Milot A, Tremblay G. The role of global risk assessment in hypertension therapy. Can J Cardiol. 2006;22(7):606–613. | |
Petrella RJ, Tremblay G, De Backer G, Gill DP; POWER survey Study Group. Effect of eprosartan-based antihypertensive therapy on coronary heart disease risk assessed by Framingham methodology in Canadian patients: results of the POWER survey. Vasc Health Risk Manag. 2014;10:63–74. | |
De Backer G, Petrella RJ, Goudev AR, Radaideh GA, Rynkiewicz A, Pathak A. Design and methodology of POWER, an open-label observation of the effect of primary care interventions on total cardiovascular risk in patients with hypertension. Fundam Clin Pharmacol. 2013;27(2):210–215. | |
Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97(18):1837–1847. | |
Leenen FH, Dumais J, McInnis NH, et al. Results of the Ontario survey on the prevalence and control of hypertension. CMAJ. 2008;178(11):1441–1449. | |
Andalib A, Akhtari S, Rigal R, et al. Determinants of masked hypertension in hypertensive patients treated in a primary care setting. Intern Med J. 2012;42(3):260–266. | |
Liddy C, Singh J, Hogg W, et al. Quality of cardiovascular disease care in Ontario, Canada: missed opportunities for prevention – a cross sectional study. BMC Cardiovasc Disord. 2012;12:74. | |
Bhan V, Yan RT, Leiter LA, et al. Relation between obesity and the attainment of optimal blood pressure and lipid targets in high vascular risk outpatients. Am J Cardiol. 2010;106(9):1270–1276. | |
Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration (BMI Mediated Effects), Lu Y, Hajifathalian K, et al. Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1.8 million participants. Lancet. 2014;383(9921):970–983. | |
Hypertension Canada. The 2012 Canadian Hypertension Education Program Recommendations (Full Version). Markham (ON):Canadian Hypertension Education Program; 2012. Available from: http://www.hypertension.ca/images/2012_CHEPRecsFullVersion_EN_HCP1000.pdf. Accessed September 11, 2014. | |
Aoki J, Uchino K. Treatment of risk factors to prevent stroke. Neurotherapeutics. 2011;8(3):463–474. | |
Dahlöf B, Devereux RB, Kjeldsen SE, et al. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE):a randomised trial against atenolol. Lancet. 2002;359(9311):995–1003. | |
Schrader J, Lüders S, Kulschewski A, et al. Morbidity and mortality after stroke, eprosartan compared with nitrendipine for secondary prevention: principal results of a prospective randomized controlled study (MOSES). Stroke. 2005;36(6):1218–1226. | |
Blood Pressure Lowering Treatment Trialists’ Collaboration, Turnbull F, Neal B, et al. Blood pressure-dependent and independent effects of agents that inhibit the renin-angiotensin system. J Hypertens. 2007; 25(5):951–958. | |
Pohl MA, Blumenthal S, Cordonnier DJ, et al. Independent and additive impact of blood pressure control and angiotensin II receptor blockade on renal outcomes in the irbesartan diabetic nephropathy trial: clinical implications and limitations. J Am Soc Nephrol. 2005;16(10):3027–3037. | |
Hellemons ME, Persson F, Bakker SJ, et al. Initial angiotensin receptor blockade-induced decrease in albuminuria is associated with long-term renal outcome in type 2 diabetic patients with microalbuminuria: a post hoc analysis of the IRMA-2 trial. Diabetes Care. 2011;34(9):2078–2083. | |
Brenner BM, Cooper ME, de Zeeuw D, et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med. 2001;345(12):861–869. | |
Viberti G, Wheeldon NM; MicroAlbuminuria Reduction With VALsartan (MARVAL) Study Investigators. Microalbuminuria reduction with valsartan in patients with type 2 diabetes mellitus: a blood pressure-independent effect. Circulation. 2002;106(6):672–678. | |
Grundy SM. Primary prevention of coronary heart disease: integrating risk assessment with intervention. Circulation. 1999;100(9):988–998. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.