Back to Journals » Journal of Inflammation Research » Volume 16
Neutrophil-to-Lymphocyte Ratio (NLR) and Platelet-to-Lymphocyte Ratio (PLR) Can Predict Spontaneous Preterm Birth?
Authors Yuce E
Received 26 March 2023
Accepted for publication 31 May 2023
Published 8 June 2023 Volume 2023:16 Pages 2423—2429
DOI https://doi.org/10.2147/JIR.S414305
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Monika Sharma
Ebru Yuce1,2
1Department of Gynecology and Obstetrics, Yuksek Ihtisas University, Faculty of Medicine, Ankara, Turkey; 2Department of Gynecology and Obstetrics, Liv Hospital, Ankara, Turkey
Correspondence: Ebru Yuce, Department of Gynecology and Obstetrics, Yuksek Ihtisas University, Faculty of Medicine, Kavaklidere, Bestekar Cd No: 8, Cankaya, Ankara, 06680, Turkey, Tel +905327135990, Email [email protected]
Purpose: To investigate the role of neutrophil to lymphocyte ratio (NLR) and platelet to lymphocyte ratio (PLR) in the prediction of spontaneous preterm birth.
Patients and Methods: Data was retrospectively collected from hospital record between February 2018 and November 2022. Pregnant women (n = 78) with a single pregnancy between 24 and 34 weeks of gestation, presented with labor pain, and had regular uterine contractions (threatened preterm labor – TPL) were included. Patients delivered within the first week after TPL were included in group 1 (n = 40) and who delivered after in group 2 (n = 38). Two groups were investigated for NLR and PLR values.
Results: The median cervical length among women who gave birth within a week was significantly lower (24.5 versus 30.0 p < 0.001). The median neutrophil-to-lymphocyte ratio among women who gave birth within a week was significantly higher (6.4 versus 4.5 p < 0.001). The median platelet-to-lymphocyte ratio among women who gave birth within a week was significantly higher (151 versus 131 p < 0.001). The cut-off values to predict preterm birth were > 5 for NLR (sensitivity: 90%, specificity: 92.1%), > 139 for PLR (sensitivity: 97.5%, specificity: 100%).
Conclusion: NLR and PLR values predict spontaneous preterm birth with high sensitivity and specificity. By predicting preterm birth, the pregnancy process can be managed sensitively and smoothly.
Keywords: neutrophil-lymphocyte ratio, NLR, platelet-lymphocyte ratio, PLR, preterm birth, prediction
Introduction
Premature birth is an important public health problem due to its high frequency and serious consequences. If it is detected and treated at an early stage by screening, the benefit of treatment increases and the economic burden of preterm births decreases. The mechanism of preterm birth is not fully understood and therefore there is no effective internationally accepted treatment. Screening methods were mainly based on the previous obstetric history of the pregnant woman. About half of preterm births occur in the first pregnancy and in pregnant women without known risk factors. Most of the tests we use to predict preterm birth do not have sufficient sensitivity, specificity and positive predictive value to identify high-risk pregnant women.
Preterm birth is a significant cause of morbidity and mortality in infants. Respiratory distress syndrome, bronchopulmonary dysplasia, patent ductus arteriosus, necrotizing enterocolitis, hyperbilirubinemia, intraventricular hemorrhage, neonatal sepsis and retinopathy may develop in preterm infants due to organ immaturity. Although there had been important advances in the prognosis of low-birth-weight babies with the establishment of neonatal intensive care facilities in recent years, prediction of preterm labor and reduction in preterm birth rates have not been achieved.1–4
The successful prediction of preterm birth is difficult given the interactions between numerous risk factors. Preterm birth may occur due to multifactorial causes, which make identification of the exact etiology difficult. Identification of methods to predict preterm birth has particular importance regarding the individual, economical, and health implications of the situation and different markers have been used to predict preterm labor.5–7
Parameters that has been prioritized by many articles in recent years are neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) that are calculated from complete blood count. The literature data suggests that preterm labor and particularly preterm premature rupture of membranes (PPROM) might be associated with subtle infections,8 and a previous study that evaluated the association between inflammation and preterm births reported that chorioamnionitis may result in placental inflammation and can be predicted by NLR in these patients.9 However, these findings have not been completely evaluated and need further investigation in different populations. In this study, we aimed to determine whether these simply calculated parameters, which are indicators of immune response capacity and subclinical inflammation, have clinical utility in the prediction of spontaneous preterm birth.
Materials and Methods
The data used in the study were collected retrospectively from the database of our hospital between February 2018 and November 2022. The study was conducted under the principles of the Declaration of Helsinki. Local Ethics committee of Yuksek Ihtisas University approved the study protocol. Patient consent to review their medical records was not required by the committee since unidentified data was used, and no confidential information was obtained from retrospective data collection (approval number: 2023–03-06, approval date: 05/18/2023).
Pregnant women (n = 78) with a single pregnancy between 24 and 34 weeks of gestation, presenting with labor pain, and having regular uterine contractions (threatened preterm labor – TPL) were included in the study. Patients who delivered within the first week after diagnosis of TPL were included in group 1 and those who delivered later than 1 week were included in group 2. Two groups were investigated for NLR and PLR values.
The NLR and PLR values of all patients were obtained from laboratory tests taken at the time of first admission, without antibiotic prophylaxis and betamethasone dose for lung maturation. NLR was defined as the absolute neutrophil count divided by the absolute lymphocyte count, while PLR was defined as the absolute platelet count divided by the absolute lymphocyte count.
PPROM, placenta previa totalis, abruptio placenta, multiple pregnancy, assisted reproductive technologies (ART) conceptions, presence of vaginal bleeding, vasculitis, presence of connective tissue disease (Ehler Danlos, Marfan Syndrome, etc.), fetal distress, intrauterine ex fetus, gross fetal anomaly, polyhydramnios, presence of inflammatory diseases, hematological disorders, malignancies, liver disease, history of autoimmune disease, gestational diabetes mellitus and preeclampsia and pregnant women with acute or chronic infections were excluded from the study.
Statistical Analyses
Continuous variables were expressed as Median (interquartile range). Kolmogorov–Smirnov test was used to determine whether variables were normally distributed. Mann Whitney U-test was used to compare continuous variables between groups. Binary logistic regression analysis was performed to determine the variables for predicting delivery time. The receiver operating characteristic (ROC) curve was constructed and the area under the curve (AUC) was calculated to estimate the predictive power of the cervical length, neutrophil-to-lymphocyte ratio, and platelet-to-lymphocyte ratio score for predicting delivery time. The sensitivity and specificity values were calculated. Statistical analysis of the data was performed with SPSS.25 and MedCalc12. A value of p < 0.05 was considered statistically significant.
Power Analysis
The sample size was calculated based on the NLR values reported previously for the PPROM patients in different studies.8,10 However, the literature data suggested these values in a wide range, and we estimated the projected NLR values using the data from previous studies, and internal results from other studies conducted at our department, as 6.3±4.9 for premature birth group, and 3.6±2.1 for controls. The required sample size was calculated using G*Power 3.1 software,11 assuming Type-I error of 5%, and Type-II error of 0.80. Accordingly, we found that a total of 70 participants was needed, and with inclusion of 10% non-response rate, we estimated the total sample size as 78 patients.
Results
The neutrophils (/mm3) were significantly higher (p < 0.001), lymphocytes were significantly lower (p < 0.001), platelets were similar but statistically different (p = 0.022) among women who gave birth within a week (n = 40) compared to women who have not given birth within a week (n = 38). However, gestational weeks (p = 0.075), age (p = 0.0425), gravida (p = 0.863), parity (p = 0.093) and hemoglobin (p = 0.386) levels were not significantly different between among women who gave birth within a week and women who have not given birth within a week (Table 1).
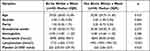 |
Table 1 Comparison of Age, Gravida, Parity, Gestational Weeks, Hemoglobin, Neutrophils (/mm3), Lymphocytes (/mm3) and Platelet (x1000/ mm3) Among Groups |
As seen Table 2, the median cervical length among women who gave birth within a week was significantly lower than women who have not given birth within a week (24.5 versus 30.0, p < 0.001). However, the median neutrophil-to-lymphocyte ratio among women who gave birth within a week was significantly higher than women who have not given birth within a week (6.4 versus 4.5, p < 0.001). The median platelet-to-lymphocyte ratio among women who gave birth within a week was significantly higher than women who have not given birth within a week (151 versus 131, p < 0.001).
 |
Table 2 Comparison of Cervical Length, Neutrophil-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio Among Groups |
Logistic Regression Analyses
According to results of logistic regression analyses, the cervical length (B = −1.026, OR = 0.358, 95% CI 0.231–0.556, p < 0.001), neutrophil-to-lymphocyte ratio (B = 2.291, OR = 9.887, 95% CI 4.140–23.614, p < 0.001), and platelet-to-lymphocyte ratio (B = 0.229, OR = 1.257, 95% CI 1.157–1.367, p < 0.001) were significantly related to delivery time (Table 3).
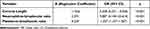 |
Table 3 Logistic Analysis Results for Cervical Length, Neutrophil-to-Lymphocyte Ratio, and Platelet-to-Lymphocyte Ratio |
ROC Analysis
The optimal cut-off value of cervical length for predicting delivery time was ≤25, with sensitivity of 90% (CI = 76.3–97.2) and specificity of 97.4% (CI = 86.2–99.9) (Table 4 and Figure 1). The optimal cut-off value of neutrophil-to-lymphocyte ratio for predicting delivery time was >5, with sensitivity of 90% (CI = 76.3–97.2) and specificity of 92.11% (CI = 78.6–98.3) (Table 4 and Figure 2). The optimal cut-off value for platelet-to-lymphocyte ratio was >139 with sensitivity of 97.5% (CI = 86.8–99.9) and specificity of 100% (CI = 90.7–100) (Table 4 and Figure 3).
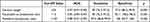 |
Table 4 ROC Analysis Results for Cervical Length, Neutrophil-to-Lymphocyte Ratio, and Platelet-to-Lymphocyte Ratio |
 |
Figure 1 Receiver operating characteristic curve analysis for cervical length. |
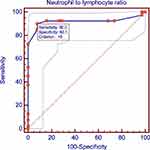 |
Figure 2 Receiver operating characteristic curve analysis for neutrophil-to-lymphocyte ratio. |
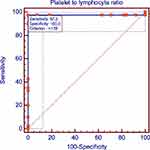 |
Figure 3 Receiver operating characteristic curve analysis for platelet-to-lymphocyte ratio. |
Discussion
Although various factors are blamed in the pathogenesis of preterm birth, inflammation and inflammatory processes are important causes of preterm birth.12 In our research, neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio were found significantly higher in women with TPL who delivered within a week. These results suggest that the severity of inflammation and the time to delivery are inversely proportional.
Levels of lymphocytes and neutrophils which are leukocyte subtypes show changes in systemic inflammatory events. NLR and PLR have been shown to have prognostic and predictive values in many pregnancy-related or non-pregnancy-related studies.13–16 High NLR values in intrahepatic cholestasis,17 hyperemesis gravidarum18 and preeclampsia19 have been reported. In addition, it has been shown that NLR values are higher in spontaneous preterm labor and PPROM and are useful in the prediction of preterm labor.20 On the other hand, PLR values have different patterns in pregnancy. Since it is a valuable indicator of inflammation and thrombosis, its levels may change in PPROM or preeclampsia, but not affected in amniotic fluid disorders especially in the normal amniotic fluid in PPROM.8,21 It is reported that, the value of complete blood count parameters were related in predicting preterm delivery.22 Among those parameters. NLR. PLR, and lymphocyte-to-monocyte ratio might have prognostic significance since they can represent chronic low-grade inflammation. In our study, the number of lymphocytes was found to be significantly lower in those who were born within 1 week. We think that this result is related to the decreased lymphocyte count in chronic inflammation, as in other indices.
In a recent study similar to ours, NLR and PLR values were investigated in the prediction of preterm labor in pregnant women hospitalized due to the threat of preterm birth. The authors found that; NLR, RDW, WBC, and absolute neutrophil cell count are positively associated with birth within 1 week of diagnosis of TPL.23 Additionally, PLR values were also investigated in addition to this study and logistic regression analysis and ROC analysis were also included, in our study. Neutrophil-to-lymphocyte ratio was related for predicting delivery with sensitivity of %90 and %92 specificity. Similarly, the platelet-to-lymphocyte ratio had %97.5 sensitivity and %100 specificity, for birth prediction.
In our study, we found that NLR and PLR values predict preterm birth with high sensitivity and specificity, and we think that our findings will contribute to the literature, systematic reviews and meta-analyses. By predicting preterm birth, the pregnancy process can be managed sensitively and smoothly. We hope that with the increase in the knowledge about its pathophysiology and the use of new techniques, better points will be reached in the estimation of preterm birth. With regard to this perspective, novel methods are being investigated and contemporary approaches are being reported in the literature. In one of these studies, Della Rosa et al established a generalized methodology to build an evidence-based holistic model based on their results from analysis of 174 identified intrauterine and extrauterine factors, and reported that placenta previa, pregnancy-induced hypertension, antibiotics, cervix length, physical exercise, fetal growth, maternal anxiety, preeclampsia, and antihypertensive use were the parameters in their most informative and parsimonious model.24
Besides the significance of NLR and PLR found, there are several limitations in this study to be considered in interpretation of the results. First, this is a retrospective study, and our results should be confirmed in randomized prospective studies. Second, although the sample size was calculated to achieve adequate study power, our findings may not reflect the situation in different populations or demographic subgroups with different prevalence of preterm births, and studies in larger cohorts are needed to replicate these results.
Conclusions
This study showed that NLR and PLR are promising biomarkers that can be used to predict preterm birth. Although the high sensitivity and specificity of these parameters suggest that they are successful in preterm labor prediction, these results should be confirmed in prospective studies.
Disclosure
The author reports no conflicts of interest in this work.
References
1. Vogel JP, Chawanpaiboon S, Moller AB, Watananirun K, Bonet M, Lumbiganon P. The global epidemiology of preterm birth. Best Pract Res Clin Obstet Gynaecol. 2018;52:3–12. doi:10.1016/j.bpobgyn.2018.04.003
2. da Fonseca EB, Damião R, Moreira DA. Preterm birth prevention. Best Pract Res Clin Obstet Gynaecol. 2020;69:40–49. doi:10.1016/j.bpobgyn.2020.09.003
3. Griggs KM, Hrelic DA, Williams N, McEwen-Campbell M, Cypher R. Preterm labor and birth: a clinical review. MCN Am J Matern Child Nurs. 2020;45(6):328–337. doi:10.1097/nmc.0000000000000656
4. Laudanski P, Lemancewicz A, Kuc P, et al. Chemokines profiling of patients with preterm birth. Mediators Inflamm. 2014;2014:185758. doi:10.1155/2014/185758
5. Suff N, Story L, Shennan A. The prediction of preterm delivery: what is new? Semin Fetal Neonatal Med. 2019;24(1):27–32. doi:10.1016/j.siny.2018.09.006
6. Oskovi Kaplan ZA, Ozgu-Erdinc AS. Prediction of preterm birth: maternal characteristics, ultrasound markers, and biomarkers: an updated overview. J Pregnancy. 2018;2018:8367571. doi:10.1155/2018/8367571
7. Daskalakis G, Theodora M, Antsaklis P, et al. Assessment of uterocervical angle width as a predictive factor of preterm birth: a systematic review of the literature. Biomed Res Int. 2018;2018:1837478. doi:10.1155/2018/1837478
8. Esercan A, Demir I. Neutrophil/lymphocyte and platelet/lymphocyte ratio in preterm premature rupture of membranes. Cureus. 2023. doi:10.7759/cureus.38664
9. Cappelletti M, Della Bella S, Ferrazzi E, Mavilio D, Divanovic S. Inflammation and preterm birth. J Leukoc Biol. 2016;99(1):67–78. doi:10.1189/jlb.3MR0615-272RR
10. Uçkan K, Başkıran Y, Çeleğen İ. Association of subclinical markers of inflammation with preterm premature rupture of membranes and adverse neonatal results: a case control study. Arch Gynecol Obstet. 2022;306(6):2063–2068. doi:10.1007/s00404-022-06756-1
11. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175–191. doi:10.3758/bf03193146
12. Vakili S, Torabinavid P, Tabrizi R, Shojazadeh A, Asadi N, Hessami K. The association of inflammatory biomarker of neutrophil-to-lymphocyte ratio with spontaneous preterm delivery: a systematic review and meta-analysis. Mediators Inflamm. 2021;2021:6668381. doi:10.1155/2021/6668381
13. Ying HQ, Deng QW, He BS, et al. The prognostic value of preoperative NLR, d-NLR, PLR and LMR for predicting clinical outcome in surgical colorectal cancer patients. Med Oncol. 2014;31(12):305. doi:10.1007/s12032-014-0305-0
14. Sari I, Sunbul M, Mammadov C, et al. Relation of neutrophil-to-lymphocyte and platelet-to-lymphocyte ratio with coronary artery disease severity in patients undergoing coronary angiography. Kardiol Pol. 2015;73(12):1310–1316. doi:10.5603/KP.a2015.0098
15. Seckin KD, Karslı MF, Yucel B, et al. The utility of tumor markers and neutrophil lymphocyte ratio in patients with an intraoperative diagnosis of mucinous borderline ovarian tumor. Eur J Obstet Gynecol Reprod Biol. 2016;196:60–63. doi:10.1016/j.ejogrb.2015.10.025
16. Kumtepe Y, Dündar O, Cetinkaya K, Ingeç M. Preeclampsia and eclampsia incidence in the eastern Anatolia region of Turkey: the effects of high altitude. J Turk Ger Gynecol Assoc. 2011;12(1):26–30. doi:10.5152/jtgga.2011.06
17. Kirbas A, Biberoglu E, Daglar K, et al. Neutrophil-to-lymphocyte ratio as a diagnostic marker of intrahepatic cholestasis of pregnancy. Eur J Obstet Gynecol Reprod Biol. 2014;180:12–15. doi:10.1016/j.ejogrb.2014.05.042
18. Kurt RK, Güler A, Silfeler DB, Ozçil MD, Karateke A, Hakverdi AU. Relation of inflammatory markers with both presence and severity of hyperemesis gravidarum. Ginekol Pol. 2014;85(8):589–593. doi:10.17772/gp/1776
19. Kurtoglu E, Kokcu A, Celik H, Tosun M, Malatyalioglu E. May ratio of neutrophil to lymphocyte be useful in predicting the risk of developing preeclampsia? A pilot study. J Matern Fetal Neonatal Med. 2015;28(1):97–99. doi:10.3109/14767058.2014.905910
20. Toprak E, Bozkurt M, Dinçgez Çakmak B, et al. Platelet-to-lymphocyte ratio: a new inflammatory marker for the diagnosis of preterm premature rupture of membranes. J Turk Ger Gynecol Assoc. 2017;18(3):122–126. doi:10.4274/jtgga.2017.0028
21. Scheurer M, Zhou X, Du Y, et al. Prognostic value of PLR in various cancers: a meta-analysis. PLoS One. 2014;9(6). doi:10.1371/journal.pone.0101119
22. Daglar HK, Kirbas A, Kaya B, Kilincoglu F. The value of complete blood count parameters in predicting preterm delivery. Eur Rev Med Pharmacol Sci. 2016;20(5):801–805.
23. Tolunay HE, Elci E. Importance of haemogram parameters for prediction of the time of birth in women diagnosed with threatened preterm labour. J Int Med Res. 2020;48(4):300060520918432. doi:10.1177/0300060520918432
24. Della Rosa PA, Miglioli C, Caglioni M, et al. A hierarchical procedure to select intrauterine and extrauterine factors for methodological validation of preterm birth risk estimation. BMC Pregnancy Childbirth. 2021;21(1). doi:10.1186/s12884-021-03654-3
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
