Back to Journals » Journal of Inflammation Research » Volume 15
Neutrophil Ratio of White Blood Cells as a Prognostic Predictor of Clostridioides difficile Infection
Authors Lee CC , Lee JC, Chiu CW, Tsai PJ , Ko WC , Hung YP
Received 13 December 2021
Accepted for publication 11 March 2022
Published 19 March 2022 Volume 2022:15 Pages 1943—1951
DOI https://doi.org/10.2147/JIR.S353814
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Monika Sharma
Ching-Chi Lee,1,2,* Jen-Chieh Lee,2,* Chun-Wei Chiu,3 Pei-Jane Tsai,4– 6 Wen-Chien Ko,2,7 Yuan-Pin Hung2,3,7
1Clinical Medicine Research Center, National Cheng Kung University Hospital, College of Medicine, National Cheng Kung University, Tainan, 704, Taiwan; 2Department of Internal Medicine, National Cheng Kung University Hospital, College of Medicine, National Cheng Kung University, Tainan, 704, Taiwan; 3Department of Internal Medicine, Tainan Hospital, Ministry of Health and Welfare, Tainan, 700, Taiwan; 4Department of Medical Laboratory Science and Biotechnology, College of Medicine, National Cheng Kung University, Tainan, 704, Taiwan; 5Department of Pathology, National Cheng Kung University Hospital, College of Medicine, National Cheng Kung University, Tainan, Taiwan; 6Centers of Infectious Disease and Signaling Research, National Cheng Kung University, Tainan, Taiwan; 7Department of Medicine, College of Medicine, National Cheng Kung University, Tainan, 704, Taiwan
*These authors contributed equally to this work
Correspondence: Yuan-Pin Hung, Department of Internal Medicine, Tainan Hospital, Ministry of Health and Welfare, Tainan, 700, Taiwan, Email [email protected] Wen-Chien Ko, Department of Medicine, College of Medicine, National Cheng Kung University, Tainan, 704, Taiwan, Email [email protected]
Introduction: A leukocyte count ≥ 15,000 cells/mL and serum creatinine of > 1.5 mg/dL have been reported as two important predictors of severe CDI. However, the association of the differential ratios of blood leukocytes, and the prognosis of Clostridioides difficile infection (CDI) is not clear.
Materials and Methods: A clinical study was conducted at medical wards of Tainan Hospital, Ministry of Health and Welfare in southern Taiwan between January 2013 and April 2020. Hospitalized adults (aged ≥ 20 years) with hospital-onset CDI (ie, symptom onset after at least 48 hours of admission) were included.
Results: A total of 235 adults with an average age of 75.7 years and female predominance (51.5%), including 146 (62%) adults with non-severe CDI and 87 (38%) severe CDI, were included for analysis. Patients with severe CDI had a higher crude in-hospital mortality rate than patients with non-severe CDI (35.6% vs 18.5%, P = 0.005). Multivariate analysis revealed no association between a leukocyte count > 15,000 cell/mL at the onset of CDI and in-hospital mortality (odds ratio [OR] 1.66, P = 0.21). In contrast, a neutrophil ratio > 75% (OR 2.65, P = 0.02), serum creatinine > 1.5 mg/L (OR 3.42, P = 0.03), and CDI caused by isolates harboring the tcdC gene (OR 3.54, P = 0.02) were independently associated with in-hospital mortality. Patients with a neutrophil ratio > 85%, 80– 85%, or 75– 80% of serum leukocytes had a higher mortality rate (34.8%, 30.3%, or 34.4%, respectively) than patients with a neutrophil ratio of 70– 75% or ≤ 75% (12.5% or 13.9%, respectively).
Conclusion: Serum creatinine > 1.5 mg/L, a high neutrophil ratio of blood leukocytes (> 75%), and the causative C. difficile harboring the tcdC gene was independent prognostic predictors in hospitalized adults with CDI.
Keywords: Clostridioides difficile, leukocyte, differential ratio, neutrophil, prognosis, mortality
Introduction
Clostridioides difficile infection (CDI) is a common community-acquired or health care-associated intestinal infection that has variable clinical presentations ranging from mild diarrhea, pseudomembranous colitis, and toxic megacolon to death.1 Host immunity is associated with the disease severity of CDI.1,2 For host immunity, leukocytes or white blood cells (WBCs) are a heterogeneous group of nucleated cells found in the circulation, with a normal range of 4000 and 10,000 per microliter in blood.3 Leukocytosis in CDI patients, especially leukocyte counts ≥ 15,000 cells/mL, is an important predictor of poor clinical outcome, including treatment failure, prolonged hospitalization, and mortality.4,5 Therefore, a leukocyte count ≥ 15,000 cells/mL and serum creatinine of > 1.5 mg/dL are two important predictors of severe CDI, according to the clinical guidelines issued by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA) in 2017.6 These guidelines recommended oral vancomycin for non-severe and severe CDI and metronidazole as an alternative choice for non-severe CDI.6
Neutrophils, accounting for 60–70% of serum leukocytes, are the first cells recruited at the site of infection. Neutrophils attack, ingest, and digest microorganisms by producing reactive oxygen species.7 Neutrophils play an important role in acute inflammatory settings, especially acute bacterial infections.7 During CDI, neutrophils are the major defense cells that infiltrate affected intestinal tissue and participate in pathogen clearance. Therefore, neutrophilic infiltration in the gut is an important process in CDI.8 A clinical study of 600 cases of CDI showed that a neutrophil-lymphocyte ratio within two days of CDI diagnosis predicted mortality and intensive care unit (ICU) transfer.9 In contrast, another retrospective study found that increasing neutrophil count was linked to a higher likelihood of the resolution of CDI in 44 neutropenic patients.10 An increase in eosinophils and lymphocytes, two other important subpopulations of leukocytes, was associated with milder CDI severity.9,11 As there were variations in the subpopulations of leukocytes among the CDI patients with at least one comorbidity and polypharmacy, total leukocyte count may not be a perfect indicator of disease severity. The association of differential ratios of blood leukocytes, especially neutrophils, and the outcomes of CDI was analyzed in this study.
Materials and Methods
Study Protocol
A clinical study was performed in the medical wards of the Tainan Hospital, Ministry of Health and Welfare, a regional hospital in southern Taiwan between January 2013 and April 2020. The institutional review board of National Cheng Kung University Hospital, Taiwan approved this study (approval number: B-ER-103-098). Because of a retrospective review of medical records of hospitalized patients, incapability of obtaining informed consent, and no specific ethical concern and minimal safety risk, the study was allowed to waive informed consent in compliance with the Declaration of Helsinki from the legally authorized representatives. Patient data confidentiality was cautiously maintained. Hospitalized adults (aged ≥ 20 years) with hospital-onset CDI (ie, symptom onset at least 48 hours after admission) were included. Patients with underlying hematological malignancy or cytotoxic chemotherapy for solid tumors in the previous three months were excluded. CDI was diagnosed as the presence of unexplained diarrhea and a positive result of glutamate dehydrogenase (GDH) and toxin A/B using an enzyme immunoassay (EIA) (Abbott, Santa Clara, USA) in fecal samples or the detection of tcdB-carrying C. difficile isolates in stool culture.12 Diarrhea was defined as at least three unformed bowel movements per day for at least two days. Fecal samples were sent for C. difficile cultures in cycloserine-cefoxitin-fructose agar (CCFA) plates at the discretion of attending physicians, which were incubated anaerobically for 24 to 48 hours.13 A multiplex polymerase chain reaction (PCR) was used to detect tcdA, tcdB, cdtA, cdtB, and tcdC deletions in C. difficile isolates, as described previously.14
Collection of Clinical Data
Clinical data, including sex, age, nasogastric tube use, underlying diseases, and laboratory data, were collected from electronic medical records using a predetermined record form. Medications, including antibiotics, proton pump inhibitors, histamine H2-receptor antagonists, or steroids, prescribed within one month before the onset of CDI or during hospitalization were recorded. The place of CDI onset, such as wards or intensive care units (ICUs), was recorded. Chronic kidney disease (CKD) was defined as an estimated glomerular filtration rate (eGFR) of < 60 mL/min/1.73 m2 for at least three months.15 Leukocyte counts and differential ratios within two days after CDI onset were recorded. Leukocyte counts and differential ratios were analyzed using a Sysmex XN-1000™ Hematology Analyzer (Sysmex@, Canada). Colonization or infection of vancomycin-resistant enterococci (VRE) during hospitalization was recorded based on medical charts.
Disease Severity and Outcome of CDI
The disease severity of CDI was graded based on the Clinical Practice Guidelines of IDSA and SHEA issued in 2017 (13). Briefly, patients with a leukocyte count of ≥ 15,000 or serum creatinine > 1.5 mg/dL were considered to have severe infection, whereas patients who lack these criteria had non-severe infections.6 The duration of hospitalization preceding CDI was the period from admission to CDI onset, and only the first CDI episode was included. The following modified definition of treatment success was used: the resolution of diarrhea within six days of antimicrobial therapy, without the need to change the therapeutic regimen, and survival at the end of antimicrobial therapy.16 The appearance of relapsing diarrhea in combination with the detection of C. difficile toxin or tcdB-carrying C. difficile in unformed stools at least three weeks following initial treatment success was defined as having recurrent CDI.16
Statistical analysis was performed using statistical software (IBM SPSS, version 22.0). Continuous data are expressed as the means ± standard deviations. The χ2 or Fisher’s test was used for categorical variables, and Student’s t-test was used for continuous variables. A two-tailed P value of < 0.05 was considered statistically significant. The Bonferroni correction was applied for multiple comparisons. Variables with a P value < 0.15 in univariate analysis were selected for multivariate analysis, which was performed using the Hosmer–Lemeshow test for goodness of fit in the logistic regression model.
Results
A total of 235 patients were included in the study, including 146 (62%) patients with non-severe CDI and 87 (38%) patients with severe CDI, as shown in Figure 1. Their average age was 75.7 years, and females predominated and accounted for 51.5% (n=121) of 235 participants (Table 1). One hundred forty-six patients with severe CDI had a higher crude in-hospital mortality rate than 87 patients with non-severe CDI (35.6% vs 18.5%, P = 0.005). The mean duration (± standard deviation) from onset of CDI to in-hospital mortality was 18.0 (± 11.8) days and 23.5 (± 9.8) days for patients with severe and non-severe CDI, respectively (P = 0.06; Figure 1). One hundred seventy-seven surviving patients were more likely to be male (52.5% vs 36.2%, P = 0.04) and less likely to have prior penicillin exposure within one month before CDI onset (9.6% vs 19.0%, P = 0.06) than 58 fatal patients. There were no differences in comorbidities, medication exposure, concurrent antibiotic use, VRE colonization during hospitalization, or ICU-onset CDI between the survivors and fatal patients (Table 1 and Supplement Table 1). None of the patients in the present study experienced VRE infection during hospitalization.
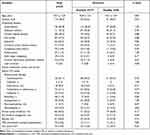 |
Table 1 Underlying Diseases and Prior Medications in Hospitalized Adults with Clostridioides Difficile Infection (CDI) Stratified by the in-Hospital Outcome |
 |
Figure 1 The mortality of patients with Clostridioides difficile infection (CDI) was stratified according to the severity grading of IDSA/SHEA. Notes: *Severe CDI: blood leukocyte ≥ 15,000 cells/mL or serum creatinine > 1.5 mg/dL; non-severe CDI: blood leukocyte ≤ 15,000 cells/mL and serum creatinine < 1.5 mg/dL, according to the IDSA/ SHEA criteria6. |
The laboratory data revealed that fatal patients had a higher blood leukocyte count (13.5 ± 7.8 vs 11.6 ± 6.6 x 1000 cells/mL, P = 0.06) and neutrophil ratio (79.6% vs 74.1%, P = 0.005) but a lower monocyte (5.7% vs 6.6%, P = 0.03) and lymphocyte (12.3% vs 15.8%, P = 0.02) ratio than surviving patients (Table 2). There was no difference in the neutrophil/lymphocyte ratio between the two groups. Because the average neutrophil ratio of 235 included patients was 75.4%, they were further divided into two groups, patients with neutrophil ratios ≤ 75% and > 75%. Fatal patients more often had a neutrophil ratio of > 75% (75.9% vs 49.2%, P < 0.001) and serum creatinine > 1.5 mg/L (19.3% vs 9.0%, P = 0.06), were infected by C. difficile harboring the tcdC gene (22.0% vs 8.5%, P = 0.03), and were treated with oral vancomycin (8.6% vs 2.3%, P = 0.04) than survivors (Table 2).
 |
Table 2 Laboratory Characteristics and Antimicrobial Therapy in Patients with Clostridioides Difficile Infection (CDI) Stratified by the in-Hospital Outcome |
Multivariate analyses revealed that only two variables, serum creatinine and C. difficile with tcdC deletion, were independently associated with in-hospital mortality when the blood leukocyte count parameter was entered in the logistic regression model (Table 3). However, three variables (a neutrophil ratio > 75%, serum creatinine > 1.5 mg/L, and C. difficile harboring the tcdC gene) were independently related to a fatal outcome when the neutrophil ratio was considered (Table 3). Notably, there were no differences between patients with a neutrophil ratio > 75% and ≤ 75% in age, sex, underlying disease, or CDI caused by an isolate harboring the tcdC gene (Table 4). Patients with a neutrophil ratio > 75% more often had a leukocyte count ≥ 15,000 cells/mL (38.2% vs 11.5%, P < 0.001) than patients with a neutrophil ratio ≤ 75%.
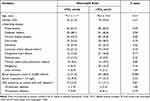 |
Table 4 Clinical and Microbiological Characteristics in Patients with Clostridioides Difficile Infection (CDI) Stratified by a Neutrophil Ratio ≤ 75% or > 75% |
To further confirm the association between the neutrophil ratio and in-hospital mortality, the 235 patients were stratified by the neutrophil ratio (Figure 2). Patients with a neutrophil ratio > 85%, 80–85%, or 75–80% had a relatively higher mortality rate (34.8%, 30.3%, or 34.4%, respectively) than patients with a neutrophil ratio of 70–75% or < 70% (12.5% or 13.9%, respectively), but the difference was not statistically significant (P = 0.06, by Fisher’s test). However, there was no correlation between the treatment success rate or recurrence rate and the neutrophil ratio.
Discussion
Although the IDSA/SHEA guidelines refer to two host variables, leukocytosis (leukocyte count ≥ 15,000 cells/mL) and serum creatinine > 1.5 mg/dL, as surrogate markers of severe CDI disease, our study found that the neutrophil ratio of blood leukocytes better predicted the risk of in-hospital prognosis in hospitalized adults with CDI. A neutrophil ratio > 75% provided a better correlation with in-hospital mortality than a blood leukocyte count ≥ 15,000 cells/mL. However, the clinical significance of neutrophil count in neutropenic patients is different, since in a small cohort of neutropenic patients the increase of absolute neutrophil count was linked to increased likelihood of resolution of CDI.10 Therefore, the clinical implications of leukocytosis and impaired renal function as outcome indicators of CDI require detailed evaluation of clinical complexity of the care receipts.
The decrease in monocyte or lymphocyte ratio was not significantly associated with in-hospital mortality in our adult patients with CDI. Neutrophils provide important innate immunity against CDI.17–19 During CDI, inflammatory cytokines, such as C-X-C motif chemokine ligand 1, granulocyte-macrophage colony-stimulating factor, and interleukin-23, recruit neutrophils to the colon mucosa.17–19 Lack of intestinal neutrophil and eosinophil recruitment in aged mice during severe CDI was accompanied by a simultaneous increase in circulating neutrophils and eosinophils in blood.18 Therefore, an increase in circulating neutrophils in blood may be associated with decreased innate immunity in the colon mucosa and more severe CDI. Increasing neutrophil count in neutropenic patients was associated with an increased chance of CDI resolution.10 However, an exaggerated inflammatory response during CDI results in host tissue damage, which is associated with worse patient outcomes.20 Notably, type-2 immune response activation, with a hallmark of an increase in eosinophils and decrease in neutrophils, was proposed as a novel prognostic marker for CDI.11,20 Eosinopenia or undetectable eosinophil count at admission correlates with increased mortality in hospitalized patients,11,21 although this correlation is not evident in the present study.
CDI due to C. difficile strains with 18-bp (primarily RT027 complex) or 39-bp (mainly RT078 complex) tcdC deletion was linked to a higher in-hospital mortality rate in patients with CDI in our study. Increased production of toxins A and B via tcdC deletion, a negative regulator of toxin production, may be a hallmark of hypervirulent C. difficile strains.22 C. difficile strains with 18-bp and 39-bp deletions were reported in Asia23,24 and Taiwan.1,24 However, the clinical importance of C. difficile harboring the tcdC gene was challenged recently.23,25 C. difficile strains with 18-bp or 39-bp tcdC deletion were common in Singapore but were not associated with more severe diseases.23 Tschudin-Sutter et al reported that two microbiological characteristics of C. difficile, the presence of tcdC deletion or binary toxin, did not predict CDI severity. Another phenotypic characteristic of toxigenic C. difficile strains, the growth rate measured using microcalorimetry, inversely correlated with disease severity.25 A multicenter study in the United Kingdom showed that C. difficile hypervirulent ribotypes, including 18-bp and 39-bp tcdC deletions, had no mortality or recurrence impact in multivariate analyses.26 In contrast, CDI due to the RT078 complex was associated with in-hospital mortality in patients with hematological malignancy in our multicenter study in Taiwan.1 The present study supports the prognostic impact of clinical C. difficile strains with 18-bp or 39-bp tcdC deletion in hospitalized adults. The controversy of the clinical impact of C. difficile harboring different tcdC genes from different countries or areas warrants further evaluations of the interference from strain diversity or host heterogeneity.
There were some limitations in this study. First, it was performed in a regional hospital, and the results may not be applicable to medical centers or hospitals in other areas. Second, the study included a limited number of patients and clinical isolates without molecular typing data, although tcdC deletion was a microbiological characteristic related to clinical prognosis. Third, other factors affecting in-hospital mortality, such as the general condition of the included patients, causal relationship of CDI and mortality, concurrent or superimposed infections, or complications of underlying medical illness, were not considered in this study. Last, we arbitrarily used a breakpoint of neutrophil ratio (75%) according to the average neutrophil ratio in our population, and this breakpoint may not be suitable for other clinical settings.
In conclusion, a higher neutrophil ratio of blood leukocytes was independently associated with crude in-hospital mortality among adults with CDI, suggestive of the prognostic significance of the extent of systemic inflammatory response.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The present study was supported by research grants from the Ministry of Science and Technology, Taiwan (MOST 108-2321-B-006-004, 108-2320-B-006-043-MY3, 109-2314-B-006- 089-MY3, 110-2320-B-006-024, and 110-2314-B-675-001), Ministry of Health and Welfare, Taiwan (MOHW 110-TDU-B-211-124003), and National Cheng Kung University Hospital, Tainan, Taiwan (NCKUH-11004029).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Hung YP, Tsai CS, Tsai BY, et al. Clostridioides difficile infection in patients with hematological malignancy: a multicenter study in Taiwan. J Microbiol Immunol Infect. 2021;54:1101–1110.
2. Lai YH, Tsai BY, Hsu CY, et al. The role of toll-like receptor-2 in Clostridioides difficile infection: evidence from a mouse model and clinical patients. Front Immunol. 2021;12:691039.
3. Blumenreich MS. The white blood cell and differential count. In: Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. Boston; 1990.
4. Bauer MP, Hensgens MP, Miller MA, et al. Renal failure and leukocytosis are predictors of a complicated course of Clostridium difficile infection if measured on day of diagnosis. Clin Infect Dis. 2012;55(Suppl 2):S149–53.
5. Reigadas E, Alcala L, Marin M, Martin A, Bouza E. Clinical, immunological and microbiological predictors of poor outcome in Clostridium difficile infection. Diagn Microbiol Infect Dis. 2017;88:330–334.
6. McDonald LC, Gerding DN, Johnson S, et al. Clinical practice guidelines for Clostridium difficile infection in adults and children: 2017 Update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis. 2018;66:987–994.
7. Tahir N, Zahra F. Neutrophilia. Treasure Island (FL): StatPearls; 2021.
8. Jose S, Madan R. Neutrophil-mediated inflammation in the pathogenesis of Clostridium difficile infections. Anaerobe. 2016;41:85–90.
9. Haddad FG, Zaidan J, Polavarapu A, et al. An insight into Clostridium difficile infection: a single-center retrospective case-control study. Z Gastroenterol. 2019;57:1183–1195.
10. Tieu JD, Schmidt SA, Miller JL, et al. Clostridium difficile treatment in neutropenic patients: clinical outcomes of metronidazole, vancomycin, combinations, and switch therapy. J Oncol Pharm Pract. 2019;25:520–528.
11. Kulaylat AS, Buonomo EL, Scully KW, et al. Development and validation of a prediction model for mortality and adverse outcomes among patients with peripheral eosinopenia on admission for Clostridium difficile infection. JAMA Surg. 2018;153:1127–1133.
12. Loo VG, Bourgault AM, Poirier L, et al. Host and pathogen factors for Clostridium difficile infection and colonization. N Engl J Med. 2011;365:1693–1703.
13. Lee CC, Lee JC, Chiu CW, Tsai PJ, Ko WC, Hung YP. Clinical significance of toxigenic Clostridioides difficile growth in stool cultures during the era of nonculture methods for the diagnosis of C. difficile infection. Microbiol Spectr. 2021;1:e0079921.
14. Hung YP, Cia CT, Tsai BY, et al. The first case of severe Clostridium difficile ribotype 027 infection in Taiwan. J Infect. 2015;70:98–101.
15. Levey AS, Eckardt KU, Tsukamoto Y, et al. Definition and classification of chronic kidney disease: a position statement from Kidney Disease: improving Global Outcomes (KDIGO). Kidney Int. 2005;67:2089–2100.
16. Zar FA, Bakkanagari SR, Moorthi KM, Davis MB. A comparison of vancomycin and metronidazole for the treatment of Clostridium difficile-associated diarrhea, stratified by disease severity. Clin Infect Dis. 2007;45:302–307.
17. McDermott AJ, Falkowski NR, McDonald RA, Pandit CR, Young VB, Huffnagle GB. Interleukin-23 (IL-23), independent of IL-17 and IL-22, drives neutrophil recruitment and innate inflammation during Clostridium difficile colitis in mice. Immunology. 2016;147:114–124.
18. Abernathy-Close L, Dieterle MG, Vendrov KC, Bergin IL, Rao K, Young VB. Aging dampens the intestinal innate immune response during severe Clostridioides difficile infection and is associated with altered cytokine levels and granulocyte mobilization. Infect Immun. 2020;88:e00960–19.
19. McDermott AJ, Frank CR, Falkowski NR, McDonald RA, Young VB, Huffnagle GB. Role of GM-CSF in the inflammatory cytokine network that regulates neutrophil influx into the colonic mucosa during Clostridium difficile infection in mice. Gut Microbes. 2014;5:476–484.
20. Donlan A, Petri WA. The inflammasome and type-2 immunity in Clostridium difficile infection. Clin Colon Rectal Surg. 2020;33:67–72.
21. Carlson TJ, Endres BT, Le Pham J, et al. Eosinopenia and binary toxin increase mortality in hospitalized patients with Clostridioides difficile infection. Open Forum Infect Dis. 2020;7:ofz552.
22. Kelly CP, LaMont JT. Clostridium difficile–more difficult than ever. N Engl J Med. 2008;359:1932–1940.
23. Verdoorn BP, Orenstein R, Rosenblatt JE, et al. High prevalence of tcdC deletion-carrying Clostridium difficile and lack of association with disease severity. Diagn Microbiol Infect Dis. 2010;66:24–28.
24. Hung YP, Tsai PJ, Lee YT, et al. Nationwide surveillance of ribotypes and antimicrobial susceptibilities of toxigenic Clostridium difficile isolates with an emphasis on reduced doxycycline and tigecycline susceptibilities among ribotype 078 lineage isolates in Taiwan. Infect Drug Resist. 2018;11:1197–1203.
25. Tschudin-Sutter S, Braissant O, Erb S, et al. Growth patterns of Clostridium difficile - correlations with strains, binary toxin and disease severity: a prospective cohort study. PLoS One. 2016;11:e0161711.
26. Martin JSH, Eyre DW, Fawley WN, et al. Patient and strain characteristics associated with Clostridium difficile transmission and adverse outcomes. Clin Infect Dis. 2018;67:1379–1387.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


