Back to Journals » International Journal of General Medicine » Volume 14
Neutrophil Gelatinase-Associated Lipocalin Contributes to Increased Risk of Cardiovascular Death After Acute Coronary Syndrome
Authors Liu H , Wan X, Shi Y, Huang F, Shu H, Huang R, Gu L
Received 7 July 2021
Accepted for publication 5 August 2021
Published 27 August 2021 Volume 2021:14 Pages 4887—4895
DOI https://doi.org/10.2147/IJGM.S328022
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Huogen Liu, Xin Wan, Yundi Shi, Fengming Huang, Hailin Shu, Rijin Huang, Ling Gu
Department of Critical Care Medicine, Mindong Hospital Affiliated to Fujian Medical University, Fu’an City, Fujian Province, 355000, People’s Republic of China
Correspondence: Ling Gu
Department of Critical Care Medicine, Mindong Hospital Affiliated to Fujian Medical University, No. 89 Heshan Road, Fu’an City, Fujian Province, 355000, People’s Republic of China
Email [email protected]
Background: Neutrophil gelatinase-associated lipocalin (NGAL) has been suggested to reflect early renal dysfunction. We investigated the predictive significance of serum NGAL in predicting cardiovascular (CV) death in an old-age population with coronary heart disease (CHD).
Methods: In total, 633 CHD patients with a stable clinical condition were enrolled. The measurements of serum NGAL and other laboratory indices were performed within 24 hours after admission. Adjusted analysis was used to assess relationships between serum NGAL and CV death during the 10-year follow-up period.
Results: Multivariate logistic regression analysis demonstrated that elevated NGAL levels were related to a higher prevalence of CV disease history [quartile 4, 2.41 (1.60– 4.59), P-trend < 0.001]. The Kaplan–Meier curve indicated that patients with high NGAL levels tended to have a higher rate of CV death than patients with low NGAL levels. A multivariate Cox model suggested that increased levels of NGAL were independently linked with elevated risk of CV death (HR=2.62, 95% CI 1.51– 4.96, P< 0.001) during the 10-year follow-up period, after adjusting for related confounding factors using sensitivity analysis. Furthermore, the receiver operating characteristics (ROC) curve demonstrated that serum NGAL (AUC=0.917, 95% CI 0.895– 0.940, P< 0.001) had an ideal predictive value in predicting CV death.
Conclusion: Serum levels of NGAL were elevated in patients with CHD and may be a new parameter that could independently predict CV death in these patients, which may strengthen its potential application in clinical practice.
Keywords: neutrophil gelatinase-associated lipocalin, cardiovascular death, ischemic heart disease
Introduction
Coronary heart disease (CHD), the result of long-term myocardial ischemia caused by coronary atherosclerosis, can develop into myocardial infarction (MI) and heart failure (HF),1,2 which bring about serious medical and economic burdens and can be life-threatening for these patients.3 Although the prognosis of patients with CHD has been greatly improved by enhanced medical treatment, and many risk factors, such as hypertension and diabetes mellitus and its related pathogenesis, including inflammation and oxidative stress, have been fully confirmed in previous studies,4–7 CHD-related mortality remains high.8 Therefore, finding valuable indicators for predicting deaths from CHD is necessary.
Neutrophil gelatinase-associated lipocalin (NGAL) is a glycoprotein with a molecular weight of 25 kDa, which was originally obtained from human neutrophils.9,10 It can be synthesized in the bone marrow and stored in specific granules of mature neutrophils,11 as well as being produced in a variety of cell types, including endothelial cells, hepatic cells, cardiomyocytes, renal cells and neurons.12–15 Reports have shown that NGAL can be rapidly released as a result of damage to the kidney tubules, and was identified as a biomarker for early kidney injury in vivo.16,17 Considering the pathological features, studies have demonstrated that elevated NGAL can be regarded a biomarker for detecting renal failure in patients with HF.14,18 Another study has suggested an association between elevated NGAL and a high risk of mortality in HF patients with or without renal dysfunction.19 An animal study showed that NGAL is overexpressed in compensatory cardiomyocytes after MI and the overexpression persists at least for 1 month.14 Researchers have also observed that NGAL expression is elevated in isolated cardiomyocytes from rat heart after inflammatory stimuli, including endothelin-1, interleukin-1β and tumor necrosis factor-α (TNF-α).14,20,21 Importantly, some studies have reported that NGAL is involved in inflammation-related cardiac injury.14,22,23
Up to now, however, few studies have investigated the correlation between NGAL and CV death in CHD patients. Against the above research background, our study was the first to evaluate whether serum NGAL can predict CV death in CHD patients during a 10-year follow-up period.
Materials and Methods
Baseline Evaluations
Our study included 633 patients with CHD (MI and angina pectoris) who were hospitalized at the Cardiovascular Medicine Department of the Affiliated Mindong Hospital of Fujian Medical University owing to acute coronary syndrome (ACS) from October 2005 to December 2010. These included patients who had undergone echocardiographic evaluation and standardized treatment during hospitalization. The diagnostic criteria for CHD include:24 1) typical angina pectoris or MI without evidence of severe aortic stenosis, insufficiency, cardiomyopathy and others; 2) electrocardiogram (ECG) showing MI or a positive ECG exercise test, excluding other causes (various heart diseases, significant anemia, obstructive emphysema, autonomic nerve dysfunction, application of digitalis, electrolyte disorder and other); 3) patients over 40 years old with heart enlargement, HF and dysfunction of papillary muscles, which cannot be explained by myocardial disease or other reasons, and who have two of the following three items: hypertension, hypercholesterolemia or diabetes.25 These included CHD patients who had been clinically stable for more than 6 months and had not experienced serious illness requiring hospitalization before this admission. In total, 153 of all included patients had a history of cardiovascular disease (CVD), including essential hypertension (n=141) and stroke (n=12). All clinical features after admission (baseline data) were collected from these patients’ medical records. Patients with chronic kidney disease (n=13), serious liver diseases (n=6), neoplastic diseases (n=7) or other diseases (n=5) were excluded from this cohort study. According to Declaration of Helsinki guidelines, the Ethics Committee of the Affiliated Mindong Hospital of Fujian Medical University approved this prospective study and all included patients gave their written informed consent.
Follow-Up
All CHD patients were contacted by telephone four times each month until the occurrence of CV death during the 10-year follow-up period. The death event was defined as death caused by MI, acute HF or exacerbation of chronic HF, stroke, sudden cardiac death or arrhythmia. Our reliable and continuous surveillance system can ensure adequate collection of CV death. For the purpose of this study, as long as one of these events occurred, the patient’s follow-up was completed. If the current status of these patients was uncertain, referring cardiologists and/or general practitioners were contacted and invited to identify the patient’s condition. Fifteen CHD patients were lost to follow-up.
Laboratory Measurements
A fasting venous blood specimen was obtained from all included CHD patients on the first morning after admission. The samples were measured for brain natriuretic peptide (BNP), serum fasting blood glucose (FBG), serum urea nitrogen (BUN), hemoglobin (Hb), albumin (ALB), serum creatinine (SCr) and high-sensitivity C-reactive protein (hs-CRP) by an automated blood counter (Sysmex XE5000; Emilio de Azevedo Campos, Porto, Portugal). Low-density lipoprotein cholesterol (LDL), total cholesterol (TC), high-density lipoprotein cholesterol (HDL) and triglycerides (TG) were measured using the Siemens ADVIA 2400 automatic biochemistry analyzer (Siemens AG). Serum NGAL levels in the blood samples were measured by a rapid, point-of-care fluorescence detection immunoassay using the Triage meter (Biosite, Quilaban, Lisboa, Portugal).
Statistical Analyses
The Kolmogorov–Smirnov test combined with Q-Q plots was used to assess data normality. Data with a non-normal distribution were analyzed by the Mann–Whitney U-test, normally distributed data by the independent t-test and categorical variables by the chi-squared test.
First, to test whether serum NGAL might be associated with CVD history on admission, a corrected logical regression model was performed with serum NGAL as the independent variable and CVD history as the dependent variable. Confounding factors were corrected as follows: Model 1: Adjusted for age, gender and body mass index (BMI). Model 2: Adjusted for age, gender, BMI, smoker, drinker, exercise regularly, diabetes mellitus, blood pressure (BP), preserved left ventricular ejection fraction (LVEF) and medications. Model 3: Adjusted for age, gender, BMI, smoker, drinker, exercise regularly, diabetes mellitus, BP, preserved LVEF, medications and laboratory measurements. Second, the free rate of CV death was constructed by the Kaplan–Meier method. We further analyzed the association between serum NGAL and CV death using a corrected Cox regression model. The corrected model was used to confirm independent risk factors for CV death. Factors with P values less than 0.05 analyzed by univariate analysis were entered into the multivariate analysis. We also adjusted for confounding factors associated with CVD, even if they were not significantly associated with outcomes in the univariate analysis.
In addition, the predictive value of serum NGAL for CV death was determined using receiver operating characteristics (ROC) curves, and the area under the curve (AUC), 95% confidence intervals, sensitivity and specificity were calculated. All of the analyses were performed using SPSS 26.0 and P≤0.05 was considered statistically significant.
Results
Clinical Characteristics of the Patients with CHD After Admission
All clinical data on the included patients with CHD are described in Table 1. The serum median NGAL level in these patients was 102.5 ng/mL. Based on the serum median, all subjects were classified into two subgroups [patients with high serum NGAL (≥102.5 ng/mL) and low serum NGAL (<102.5 ng/mL)]. Compared with CHD patients with low NGAL levels, CHD patients with high serum NGAL levels had a higher CV mortality and higher prevalence of CVD history on admission (all P<0.05). They tended to be smokers or drinkers, and tended to have higher BMI, systolic BP and diastolic BP, a higher rate of diabetes mellitus and a lower rate of preserved LVEF (all P<0.05). With regard to laboratory measurements, CHD patients with high NGAL levels tended to have higher levels of FBG, LDL, TG, TC, hs-CRP, SCr and BUN, and lower levels of Hb and ALB (all P<0.05).
 |
Table 1 Clinical Characteristics of the Patients with CHD After Admission |
Elevated NGAL Levels Were Associated with Higher Prevalence of CVD History on Admission in Patients with CHD
To confirm the correlation of CVD history with serum NGAL in CHD patients, logistic regression of the correction models was used, as shown in Table 2. Model 1 demonstrated that elevated NGAL levels were linked with a higher prevalence of CVD history when age, gender and BMI were adjusted [quartile 4, 2.46 (1.65–4.67), P-trend <0.001]. The results of Model 2 were changed little and statistically significant when further adjustments for smoker, drinker, exercise regularly, diabetes mellitus, BP, preserved LVEF and medications were made [quartile 4, 2.43 (1.63–4.63), P-trend <0.001]. The results of Model 3 were similar to Model 2 when continuing to add serum indices into Model 2 [quartile 4, 2.41 (1.60–4.59), P-trend <0.001].
 |
Table 2 Logistic Regression Analysis for the Association Between Serum NGAL Levels and CVD History on Admission in Patients with CHD |
Elevated NGAL Levels Suggested an Independent Association with CV Death in Patients with CHD by Sensitivity Analysis, Using “CVD History” as a Covariate
CV deaths in CHD patients were determined from inclusion to the end of a follow-up of 10 years. In total, 51 patients with CHD died; 43 of these deaths were due to CV outcomes and the remaining eight deaths were caused by non-CV factors. The CV deaths resulted from MI (n=14), acute HF or exacerbation of chronic HF (n=12), stroke (n=8), arrhythmia (n=5) and sudden cardiac death (n=4). Kaplan–Meier analysis indicated that CHD patients with high NGAL levels (≥102.5 ng/mL) tended to have a higher rate of CV death than CHD patients with lower NGAL (P<0.001) (Figure 1).
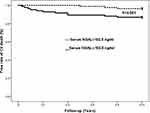 |
Figure 1 Kaplan–Meier analysis of CV mortality according to median levels of serum NGAL in patients with CHD. |
Furthermore, the predictors for CV death were assessed by Cox regression analysis. Our univariate analysis suggested that NGAL, BMI, smoker, CVD history, diabetes mellitus, SCr, TG, TC and LDL were significantly related to increased CV mortality (Table 3). Importantly, the multivariate analysis suggested that elevated NGAL levels were independently linked with increased CV mortality (HR=2.62, 95% CI 1.51–4.96, P<0.001) after adjusting for age, gender, BMI, smoker, drinker, diabetes mellitus, BP, preserved LVEF and laboratory measurements. In addition, we used a stratified analysis to investigate the correlation of serum NGAL with CV mortality in patients with MI and angina pectoris. The multivariate Cox model indicated that elevated NGAL levels were still linked with higher CV mortality in patients with MI [2.76 (1.73–5.47), P<0.001, Model 3] and in patients with angina pectoris [2.40 (1.22–4.21), P<0.001, Model 3] (Table 4). The HR value was higher in patients with MI than in patients with angina pectoris.
 |
Table 4 Association Between Serum NGAL Levels and CV Mortality During the Follow-Up of 10 Years in Patients with CHD by Stratified Analysis |
Serum NGAL Had a Good Predictive Value for Predicting CV Death During Follow-Up in Patients with CHD
To further evaluate the predictive value of NGAL in predicting CV death in patients with CHD, the ROC curve was plotted (Figure 2). We observed that serum NGAL (AUC=0.917, 95% CI 0.895–0.940, P<0.001) had an ideal predictive value in predicting CV death.
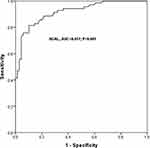 |
Figure 2 Predictive value of serum NGAL in predicting CV death in patients with CHD. |
Discussion
As far as we know, this is the first cohort study evaluating associations between serum concentrations of NGAL and CV death in CHD patients. We observed that serum NGAL is an independent predictor for CV death in patients with CHD.
The association of NGAL with CVD has been investigated in previous clinical studies and basic experiments. A clinical study showed that patients with chronic HF and MI had higher levels of NGAL compared with healthy subjects.14 Furthermore, elevated NGAL levels were significantly related to higher New York Heart Association (NYHA) classification.14 Some other studies also suggested raised NGAL levels in patients with CVD.22,23 NGAL was further found to have a prognostic value in HF patients and higher serum level of NGAL were associated with an increased risk of death.19 Importantly, elevated NGAL levels in these HF patients may reflect renal dysfunction because renal dysfunction is often observed in HF patients and can cause increased NGAL levels.26 Expression of NGAL was significantly higher in the non-ischemic area than the ischemic area in a rat model with HF caused by MI.14 Another study found that NGAL exists in atherosclerotic plaques in humans, where macrophages colocalized with NGAL.27 It also found that NGAL expression was significantly elevated in the heart and aorta of MI mice.27 In a prospective cohort study, higher serum NGAL at baseline contributed to higher risks of all-cause mortality and adverse cardiac events in a general population.28 The association of increased NGAL levels with risk of CV events was also reported in a large elderly population.29 Moreover, one study reported that among patients with ACS, elevated NGAL levels were associated with adverse outcomes.30 These previous findings are consistent with our results, that elevated serum NGAL levels and NGAL expression in tissues are associated with adverse CV events. However, differently from the previous studies, our results were based on corrected renal function so that abnormal renal function did not affect the independent association between serum NGAL and CV events in patients with CHD.
In basic experiments, the association of NGAL with cardiac function has also been investigated in NGAL−/− mice.31 A potential function is that NGAL is involved in the recruitment process of inflammatory cells in heart transplantation. Research demonstrated that a remarkably reduced number of infiltrating granulocytes was observed in NGAL+/+ recipients from transplanted NGAL−/− hearts.32,33 Another study also showed that NGAL can promote cardiomyocyte apoptosis directly, which can contribute to the remodeling process of underlying CVD conditions, including MI and HF.34 Based on the previous research on mechanisms, NGAL is significantly involved in the inflammatory reactions in the heart, causing inflammatory damage to cardiomyocytes. Similarly, with NGAL as a marker of this state, elevated hs-CRP is a marker of higher inflammatory burden.35 The mechanism of inflammatory damage may be partly responsible for the increased NGAL associated with CV death in patients with CHD.
The present study has several remarkable strengths. To begin with, this longitudinal cohort study was performed with a long-term follow-up of 10 years and sufficient clinical information was obtained. We ensured that major CV deaths occurred during our follow-up period to avoid outcome bias due to insufficient follow-up time. Our study is the first to demonstrate that elevated NGAL levels are associated with increased CV mortality and might be considered as a predictor for CV death in CHD patients, although previous studies have shown that NGAL was related to CVD. Furthermore, major confounding factors associated with NGAL and CVD were adjusted for the independent association, ensuring the reliability of our results. Of course, our research also has several unavoidable limitations. First, previous studies have shown that NGAL is a marker of early renal injury. Whether the relationship between NGAL and CHD death is caused by CHD or renal function has not been fully analyzed, although SCr, an important marker of renal function, was corrected in our regression model. Second, sufficient correction of confounding factors may also lead to overfitting of the correction model, which can make the results of the study slightly inconsistent with the actual results. Third, serum NGAL measurement was performed only once in all included patients at baseline. Other variables that may affect serum NGAL levels are unknown. A single serum test may not fully represent the real level of NGAL in these patients, thus leading to some bias in our results.
Conclusions
Serum NGAL levels are elevated and have a significant association with CV death in patients with CHD. The significant predictive value of elevated NGAL levels may be linked to a higher degree of inflammatory reactions in CHD patients because NGAL expression in a healthy general population was linked with all inflammatory markers.
Funding
This work was supported by Medical Innovation Projects of Fujian Province’s Health and Scientific Research Talent Training Project (grant no. 2019-CXB-25).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Darby SC, Ewertz M, Mcgale P, et al. Risk of ischemic heart disease in women after radiotherapy for breast cancer. N Engl J Med. 2013;368(11):987–998. doi:10.1056/NEJMoa1209825
2. Kaplan H, Thompson RC, Trumble BC, et al. Coronary atherosclerosis in indigenous South American Tsimane: a cross-sectional cohort study. Lancet. 2017;389(10080):1730–1739. doi:10.1016/S0140-6736(17)30752-3
3. Yan R, Li W, Yin L, et al. Cardiovascular diseases and risk‐factor burden in urban and rural communities in high‐, middle‐, and low‐income regions of China: a large community‐based epidemiological study. J Am Heart Assoc Cardiovasc Cerebrovasc Dis. 2017;6(2):e004445.
4. Zannad F, Anker SD, Byra WM, et al. Rivaroxaban in patients with heart failure, sinus rhythm, and coronary disease. N Engl J Med. 2018;379(14):1332–1342. doi:10.1056/NEJMoa1808848
5. Balsan G, Pellanda LC, Sausen G, et al. Effect of yerba mate and green tea on paraoxonase and leptin levels in patients affected by overweight or obesity and dyslipidemia: a randomized clinical trial. Nutr J. 2019;18(1):5. doi:10.1186/s12937-018-0426-y
6. Lin QY, Lang PP, Zhang YL, et al. Pharmacological blockage of ICAM-1 improves angiotensin II-induced cardiac remodeling by inhibiting adhesion of LFA-1+ monocytes. Am J Physiol Heart Circ Physiol. 2019;317(6):H1301–H1311. doi:10.1152/ajpheart.00566.2019
7. Kibel A, Lukinac AM, Dambic V, et al. Oxidative stress in ischemic heart disease. Oxid Med Cell Longev. 2020;2020(1):1–30. doi:10.1155/2020/6627144
8. Moran AE. Temporal trends in ischemic heart disease mortality in 21 world regions, 1980 to 2010. Circulation. 2014;129(14):1483–1492. doi:10.1161/CIRCULATIONAHA.113.004042
9. Kjeldsen L, Cowland JB, Borregaard N. Human neutrophil gelatinase-associated lipocalin and homologous proteins in rat and mouse. Biochim Biophys Acta. 2000;1482(1):272–283. doi:10.1016/S0167-4838(00)00152-7
10. Lippi G, Meschi T, Nouvenne A, et al. Neutrophil gelatinase-associated lipocalin in cancer. Adv Clin Chem. 2014;64:179–219.
11. Langelueddecke C, Roussa E, Fenton RA, et al. Lipocalin-2 (24p3/neutrophil gelatinase-associated lipocalin (NGAL)) receptor is expressed in distal nephron and mediates protein endocytosis. J Biol Chem. 2012;287(1):159–169. doi:10.1074/jbc.M111.308296
12. Han M, Li Y, Liu M, et al. Renal neutrophil gelatinase associated lipocalin expression in lipopolysaccharide-induced acute kidney injury in the rat. BMC Nephrol. 2012;13:1.
13. Krizanac M, Mass Sanchez PB, Weiskirchen R, et al. A scoping review on Lipocalin-2 and Its role in non-alcoholic steatohepatitis and Hepatocellular carcinoma. Int J Mol Sci. 2021;22(6):2865. doi:10.3390/ijms22062865
14. Vandekerckhove L, Vermeulen Z, Liu ZZ, et al. Neuregulin-1 attenuates development of nephropathy in a type 1 diabetes mouse model with high cardiovascular risk. Am J Physiol Endocrinol Metab. 2016;310(7):E495–504. doi:10.1152/ajpendo.00432.2015
15. Ferreira AC, Dá Mesquita S, Sousa JC, et al. From the periphery to the brain: lipocalin-2, a friend or foe? Prog Neurobiol. 2015;131:120–136. doi:10.1016/j.pneurobio.2015.06.005
16. Ronco C, Bellomo R, Kellum JA. Acute kidney injury. Lancet. 2019;394(10212):1949–1964. doi:10.1016/S0140-6736(19)32563-2
17. Maisel AS, Wettersten N, van Veldhuisen DJ, et al. Neutrophil gelatinase-associated lipocalin for acute kidney injury during acute heart failure hospitalizations: the AKINESIS study. J Am Coll Cardiol. 2016;68(13):1420–1431. doi:10.1016/j.jacc.2016.06.055
18. Mortara A, Bonadies M, Mazzetti S, et al. Neutrophil gelatinase-associated lipocalin predicts worsening of renal function in acute heart failure: methodological and clinical issues. J Cardiovasc Med. 2013;14:9. doi:10.2459/JCM.0b013e3283629ca6
19. Deursen VV, Damman K, Voors AA, et al. Prognostic value of plasma neutrophil gelatinase-associated lipocalin for mortality in patients with heart failure. Circ Heart Fail. 2013;7:1.
20. Jha MK, Jeon S, Jin M, et al. The pivotal role played by lipocalin-2 in chronic inflammatory pain. Exp Neurol. 2014;254:41–53. doi:10.1016/j.expneurol.2014.01.009
21. Czapski GA, Zhao Y, Lukiw WJ, et al. Acute systemic inflammatory response alters transcription profile of genes related to immune response and Ca2+ homeostasis in hippocampus; relevance to neurodegenerative disorders. Int J Mol Sci. 2020;21(21):7838. doi:10.3390/ijms21217838
22. van Deursen VM, Damman K, Voors AA, et al. Prognostic value of plasma neutrophil gelatinase-associated lipocalin for mortality in patients with heart failure. Circ Heart Fail. 2014;7(1):35–42. doi:10.1161/CIRCHEARTFAILURE.113.000242
23. Damman K, Veldhuisen DV, Navis G, et al. Urinary neutrophil gelatinase associated lipocalin (NGAL), a marker of tubular damage, is increased in patients with chronic heart failure. Eur J Heart Fail. 2014;10(10):997–1000. doi:10.1016/j.ejheart.2008.07.001
24. Gerych PR. Comorbid IHD in patients with COPD: definition, risk factors, diagnostic criteria. Galician Med J. 2014;21(4):38–42.
25. Demirel F, Rasoul S, Elvan A, et al. Impact of out-of-hospital cardiac arrest due to ventricular fibrillation in patients with ST-elevation myocardial infarction admitted for primary percutaneous coronary intervention: impact of ventricular fibrillation in STEMI patients. Eur Heart J Acute Cardiovasc Care. 2015;4(1):16–23. doi:10.1177/2048872614547448
26. Berardinis BD, Gaggin HK, Magrini L, et al. Comparison between admission natriuretic peptides, NGAL and sST2 testing for the prediction of worsening renal function in patients with acutely decompensated heart failure. Clin Chem Lab Med. 2015;53(4):613–621.
27. Vafadarnejad E, Rizzo G, Krampert L, et al. Dynamics of cardiac neutrophil diversity in murine myocardial infarction. Circ Res. 2020;127(9):e232–e249. doi:10.1161/CIRCRESAHA.120.317200
28. Lindberg S, Jensen JS, Mogelvang R, et al. Plasma neutrophil gelatinase-associated lipocalinin in the general population: association with inflammation and prognosis. Arterioscler Thromb Vasc Biol. 2014;34(9):2135–2142. doi:10.1161/ATVBAHA.114.303950
29. Daniels L, Barrett-Connor E, Clopton P, et al. Plasma neutrophil gelatinase–associated lipocalin is independently associated with cardiovascular disease and mortality in community-dwelling older adults. J Am College Cardiol. 2012;59(12):1101–1109. doi:10.1016/j.jacc.2011.11.046
30. Rozenfeld KL, Zahler D, Shtark M, et al. Elevated neutrophil gelatinase-associated lipocalin for the assessment of structural versus functional renal damage among ST-segment elevation myocardial infarction patients. Blood Purif. 2020;49(5):560–566. doi:10.1159/000506175
31. Yang B, Fan P, Xu A, et al. Improved functional recovery to I/R injury in hearts from lipocalin-2 deficiency mice: restoration of mitochondrial function and phospholipids remodeling. Am J Transl Res. 2012;4(1):60–71.
32. Aigner F, Maier HT, Schwelberger HG, et al. Lipocalin-2 regulates the inflammatory response during ischemia and reperfusion of the transplanted heart. Am J Transplant. 2007;7(4):779–788. doi:10.1111/j.1600-6143.2006.01723.x
33. Schroll A, Eller K, Feistritzer C, et al. Lipocalin-2 ameliorates granulocyte functionality. Eur J Immunol. 2012;42(12):3346–3357. doi:10.1002/eji.201142351
34. Xu G, Ahn J, Chang S, et al. Lipocalin-2 induces cardiomyocyte apoptosis by increasing intracellular iron accumulation. J Biol Chem. 2012;287(7):4808. doi:10.1074/jbc.M111.275719
35. Menees SB, Powell C, Kurlander J, et al. A meta-analysis of the utility of C-reactive protein, erythrocyte sedimentation rate, fecal calprotectin, and fecal lactoferrin to exclude inflammatory bowel disease in adults with IBS. Am J Gastroenterol. 2015;110(3):444–54.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

