Back to Journals » Open Access Rheumatology: Research and Reviews » Volume 12
Neurological Manifestations in Familial Mediterranean Fever: a Genotype-Phenotype Correlation Study
Authors Salehzadeh F , Azami A, Motezarre M, Nematdoust Haghi R , Ahmadabadi F
Received 14 November 2019
Accepted for publication 4 January 2020
Published 15 January 2020 Volume 2020:12 Pages 15—19
DOI https://doi.org/10.2147/OARRR.S238649
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Chuan-Ju Liu
Farhad Salehzadeh, 1 Ahad Azami, 2 Maryam Motezarre, 1 Roghayeh Nematdoust Haghi, 1 Farzad Ahmadabadi 1
1Pediatric Department, Bouali Children’s Hospital, Ardabil University of Medical Sciences (ARUMS), Ardabil, Iran; 2Internal Medicine Department, Imam Khomeini Hospital, Ardabil University of Medical Sciences (ARUMS), Ardabil, Iran
Correspondence: Farzad Ahmadabadi
Pediatric Neurology, Pediatric Department, Bouali Children’s Hospital, Ardabil University of Medical Sciences (ARUMS), Ardabil, Iran
Email [email protected]
Background and Aims: Familial Mediterranean Fever (FMF) is a periodic auto-inflammatory disease with an autosomal recessive hereditary pattern. The aim of this study is to explain the spectrum of possible neurological manifestations and its genotype-phenotype correlation in patients with familial Mediterranean fever.
Methods: In this case series study, data of 311 FMF patients at the FMF Registration Center in Iran (http://www.fmfiran.ir/) was studied. Patient’s information was entered into a researcher designed questionnaire. Data were analyzed by SPSS software.
Results: The mean age of the 181 male and 130 female patients was 23.01 years, ranging from 3– 78 years old. Twelve common MEFV gene analyses were performed in 311 patients, with mutated results in 187 (60.1%) patients. The most common neurological manifestations were headache in 47.26%; 64.1% of those were persistent and 35.9% had a recurrent nature. Other neurological manifestations were vertigo (83 patients, 26.7%), paresthesia (72 patients, 23.2%), tremor (53 patients, 17%), disorientation (40 patients, 12.9%), breath-holding (23 patients, 7.4%), migraine (19 patients, 6.1%), syncope (8 patients, 2.6%), epilepsy (7 patients, 2.3%), febrile seizure (4 patients, 1%), and ataxia (5 patients, 1.6%). There were no cases of stroke or metabolic disorders among these patients.
Conclusion: The prevalence of epilepsy among FMF patients was significantly higher than the general population. FMF patients with negative results for MEFV gene mutations had significant frequency of headache, paresthesia, breath-holding, and ataxia.
Keywords: familial mediterranean fever, MEFV gene, epilepsy, migraine, headache, breathe holding, paresthesia
Introduction
Familial Mediterranean fever (FMF) is a hereditary auto-inflammatory disease with autosomal recessive inheritance. FMF is characterized by recurrent fever and inflammation of serous membranes, leading to abdominal pain, chest pain, and joint inflammation, and its classic feature includes self-limiting periods of fever and serositis.1
Clinical manifestations of the disease usually occur during the first decade of life in more than 80% of patients, and in 90% of the patients the disease began before 20 years of age.2,3 FMF is common among Mediterranean populations (Jews, Arabs, Turks, and Armenians).1 The highest prevalence of the disease among the “Sephardic Jews” and the Armenians has been reported. In the Middle East its prevalence is one in 100–2,000 people, according to different studies.3
The disease frequency in young age groups is low.4 Males are slightly more involved than females, with a prevalence rate of 1.5–2-times.5 The Mediterranean fever gene (MEFV), the causative agent of FMF, is located on the short arm (p) of chromosome 16 at position 13.3 (16p 13.3) and encode a protein called pyrin (or marenostrin) which suppresses the inflammatory response.6,7
Two MEFV gene mutations confirms the genetically diagnosis of FMF. Moreover, with regards to genotype-phenotype correlation, some data reported that patients carrying heterozygous mutations showed a more severe disease when compared both to subjects carrying homozygous and compound heterozygous mutations.8
Patients carrying MEFV mutations can also display aspecific clinical manifestations as well as significant changes in disease behavior over time.
Although FMF is a polyserositis disease, there is also central nervous system (CNS) involvement and many neurological associated symptoms. Aseptic meningitis, headache, demyelinating lesions, and pseudo tumor cerebri have been reported in patients with FMF. The neurological manifestations of disease are listed in Table 1, including persistent and/or episodic symptoms associated with febrile attacks.9
 |
Table 1 Neurological Manifestation in FMF |
It is not included following four distinct types of musculoskeletal pain (myalgia) syndrome as known neuromuscular involvement of FMF: as a constitutional symptom, as an additional type of FMF, exertion leg pain, and protracted febrile myalgia syndrome.13,14
Recently, FMF has been reported as a common auto-inflammatory disease from the northwest of Iran, with its own phenotype genotype features. The most common MEFV gene mutations in FMF patients are M694V (20.9%), V726A (12.7%), E148Q (10.7%), M680I (10.3%), and M694I (2.1%), respectively,15,16 whilst 25% of the healthy and general population in this area showed different MEFV gene alleles, as follows: E148Q (18.3%), P396S (3.1%), V726A (2.2%), features in heterozygote form.17
The aim of this study is to assess the clinical findings of FMF patients who presented with neurological findings due to CNS involvement. This study explains common neurological symptoms in these patients, which, based on some reports, have different frequencies and presentation compared with the general population regarding their MEFV gene mutations and phenotype-genotype correlations.
Materials and Methods
This is a case series study. The data of 311 FMF undercontrolled patients, who were diagnosed based on Tel-Hashomer criteria at the rheumatologic clinic and FMF Registration Center (http://www.fmfiran.ir), were collected.
Demographic information of patients, such as age, race, gender, and their neurological findings, which have been confirmed by adult or pediatric neurologist, were collected. Blood samples were screened for the 12 common pathogenic variants (E148Q, P369S, F479L, I692del, M680I (G/C), M680I (G/A), M694V, M694I, K695R, V726A, A 744S, and R 761H) according to manufacturer’s instructions (FMF Strip Assay, Vienna lab, Vienna, Austria).
The study is complaint with the Helsinki Declaration and was approved by the local Ethics Committee under number IR.ARUMS. REC.1396.95. Written Informed consent was obtained from all the participants and/or their parents.
Statistical Analysis
Analysis was mainly descriptive, calculating mean and frequency derivatives using SPSS version 20.
A 2-sided P-value<0.05 was considered statistically significant.
Results
Demographic Findings
This study included 181 (58.2%) males and 130 (41.8%) females (M/F=1.4). The mean age of the patients was 23.01±15.5 years. The youngest patient was 2 years old and the oldest one was 78 years old. The mean age of the male and female patients was 23.87 and 21.82 years, respectively.
Neurologic Findings
The neurological manifestations among the patients showed headache as the most common symptom in 147 (47.26%) patients, 64.1% of them had persistent ache, 35.9% recurrent headache, 6.1% showed classic migraine, and 10% had tension and cluster type headaches.
Other neurological manifestations were vertigo (83, 26.7%), paresthesia (72, 23.2%), tremor (53, 17%), disorientation (40, 12.9%), breath-holding (23, 7.4%), migraine (19, 6.1%), syncope (8, 2.6%), epilepsy (7, 2.3%), ataxia (5, 1.6%), and febrile seizure (4, 1.2%).
There were no stroke or metabolic disorders among patients. One female patient suffered from a MS-like disorder.
Genetic Findings
As shown in Table 2, two groups of FMF patients with positive (12 common pathogenic variants alleles) and negative results for MEFV gene mutations had significantly different frequencies of headache, paresthesia, breath-holding, and ataxia. These manifestations were significantly higher than patients without mutations.
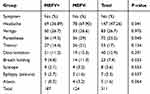 |
Table 2 Neurological Manifestations of Patients Regarding MEFV Results |
Regarding seizures, although theirfrequency was higher than patients with MEFV mutations, this differences is not meaningful (P=0.537).
Discussion
Gedalia and Zamir18 reported that, out of 101 children with FMF, 13 children (12.9%) had headache during acute fever attacks. In the Uluduz et al19 study, 32.9% of FMF patients had tension headache. A severe type of headache in the form of FMF-like recurring meningitis has also been reported by Feld et al.20 Our study showed that the prevalence of headache in FMF patients is 47.26% and it is significantly more common in MEFV allele’s negative patients.
A recent study by Canpolat et al21 of 22 children with FMF showed neurological findings included headache in 16 patients (72.7%), epilepsy in six patients (27.3%), pseudotumor cerebri in two patients (9.1%), multiple sclerosis in one patient (4.5%), and tremor in one patient (4.5%). The most common MEFV gene mutation in these patients was M694V (40.9%).
Three Israeli FMF patients with seizure were reported in 1993, which was the first report of seizure and FMF association.18 In general, our recent data has not shown a strong relationship between FMF and epilepsy. The prevalence of the epilepsy in FMF patients is 2.3%, however, in comparison with the prevalence of epilepsy in the general population of the Mediterranean region, 0.4–1.2%22 it seems, this is interestingly twice the rate of the general population.
The frequency of febrile seizure (FS) in the general population is estimated between 2–5%,23 while, in our study, the frequency of FS in FMF patients was lower than the normal range, although Comak et al24 showed children with FMF had a higher rate of FS than the general population. These contradictory results consider multiple factors in the pathogenesis of FS such as environmental and ethnic backgrounds.
There was not any case of metabolic disorders among our patients. In the Kiykim et al25 study in 174 FMF patients, only two cases of fatty acid oxidation deficiency were observed.
The relationship between FMF and stroke has not been completely studied and it is limited to a case report in children. Seven cases of stroke were reported in 3,034 patients with FMF in Kalyoncu et al's9 study. Although these patients also had other risk factors, this indicates a high prevalence compared to the general population rates (0.2% vs 0.005–0.015 in adults older than 50 years), whether FMF can be considered as a risk factor for stroke is still to be answered; however, some associated disease with FMF, particularly systemic vasculitis, may involve CNS and presents CNS vascular disorders such as stroke and ischemia.26
There have been some case reports about the coexistence of familial Mediterranean fever and posterior reversible leukoencephalopathy (PRES);9 however there was, not any co-existence of stork and PRES in our study.
The frequency of breath holding as an autonomic dysfunction in this study was 7.4%, which is higher than the general population (4–5%).27 In this study, 23.2% of patients had paresthesia, which was similar to the result of Salehzadeh et al15 report 22%, whereas in Kalyoncu et al's9 work from 18 patients with FMF who had neurological symptoms, 11.1% had paresthesia.
An interesting study by Witt et al28 showed that the sign and symptoms of autonomic dysfunction are more prevalent in FMF patients than in age- and gender-matched healthy controls.
Of these, 35.9% had recurrent headache and 6.1% showed classic migraine, whilst in the study of Uluduz et al,19 29.5% of FMF patients had migraine. On the basis of MEFV gene alleles, headache as a general symptom was meaningfully more common in MEFV negative patients.
In our study, 26.7% had vertigo and there is not any difference in frequency of vertigo between MEFV gene negative and positive patients.
The other neurological manifestations such as tremor (17%), disorientation (12.9%), and syncope (2.6%) showed a similar frequency between MEFV gene negative and positive patients.
Ataxia has been shown in 1.6% of patients, and meaningfully it was more common in MEFV gene negative patients.
The high frequency of four common neurologic symptoms in FMF patients (headache, paresthesia, breath holding, and ataxia) with negative MEFV gene mutations could be emphasized the partial protection and or modifying role of this mutation in appearance of these symptoms.
One patient in our study had multiple sclerosis (MS) like disorder with M694V heterozygous pattern. Although it has been shown that MS is more common in FMF than in the general population,29 however; it does not have any effect on the course of the disease.30
There was no case of recurrent meningitis, known as mollaret meningitis,31 among these patients.
The main limitation of this study is that the patients were evaluated retrospectively, and we did not separate pediatric from adult patients.
Conclusion
The frequency of seizure among FMF patients is significantly higher than the general population. Headache, paresthesia, breath holding, and ataxia are more common in the MEFV gene mutations negative group.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Author Contributions
F.S. and A.A. work at the rheumatology clinic and planned the study and diagnosed the FMF patients. F.A. worked on the neurologic manifestations of patients and wrote the final copy. R.N.wrote the draft copy of the manuscript. M.M. collected all data for the manuscript. All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Shohat M, Halpern GJ. Familial mediterranean fever—a review. Genet Med. 2011;13(6):487–498. doi:10.1097/GIM.0b013e3182060456
2. Fietta O. Auto inflammatory disease: the hereditary periodic fever syndromes. Acta Biomed. 2004;75(2):92–99.
3. Ben-Chetrit E, Levy M. Familial mediterranean fever. Lancet. 1998;351(9103):659–664. doi:10.1016/S0140-6736(97)09408-7
4. Aringer M. Periodic fever syndromes—a clinical overview. Acta Med Austriaca. 2004;31(1):8–12.
5. Meyerhoff J. Familial mediterranean fever: report of a large family, review of the literature, and discussion of the frequency of amyloidosis. Medicine. 1980;59(1):66–77. doi:10.1097/00005792-198001000-00004
6. Ting JP, Kastner DL, Hoffman HM. CAT- ERPILLERs, pyrin and hereditary immune - logical disorders. Nat Rev Immunol. 2006;6(3):183–195. doi:10.1038/nri1788
7. Savic S, Dickie LJ, Battellino M, McDer- mott MF. Familial mediterranean fever and related periodic fever syndromes/autoinflammatory diseases. Curr Opin Rheumatol. 2012;24(1):103–112. doi:10.1097/BOR.0b013e32834dd2d5
8. Procopio V, Manti S, Bianco G, Conti G, Romeo A. Genotype-phenotype correlation in FMF patients: a “non classic” recessive autosomal or “atypical” dominant autosomal inheritance? Gene. 2018;641:279–286. doi:10.1016/j.gene.2017.10.068
9. Kalyoncu U, Eker A, Oguz KK, et al. Familial mediterranean v fever and central nervous system involvement: a case series. Medicine (Baltimore). 2010;89(2):75–84. doi:10.1097/MD.0b013e3181d5dca7
10. Collard M, Sellal F, Hirsch E, Mutschler V, Marescoux C. Recurrent aseptic meningitis in periodic disease or mollaret’s meningitis? Rev Neurol. 1991;147:403–405.
11. Vilaseca J, Tor J, Guardia J, Bacardi R. Periodic menin- gitis and familial mediterranean fever. Arch Intern Med. 1982;142(2):378–379.
12. Gokalp HZ, Baskaya MK, Aydin V. Pseudotumor cerebri with familial mediterranean fever. Clin Neurol Neurosurg. 1992;94:261–263. doi:10.1016/0303-8467(92)90101-8
13. Langevitz P, Zemer D, Livneh A, Shemer J, Pras M. Protracted febrile myalgia in patients with familial mediterranean fever. J Rheumatol. 1994;21:1708–1709.
14. Sidi G, Shinar Y, Livneh A, et al. Protracted febrile myalgia of familial mediterranean fever. mutation analysis and clinical correlations. Scand J Rheumatol. 2000;29:174–176. doi:10.1080/030097400750002058
15. Salehzadeh F, Emami D, Zolfegari AA, et al. Familial mediterranean fever in northwest of Iran (Ardabil): the first global report from Iran. Turk J Pediatr. 2008;50(1):40–44.
16. Salehzadeh F. Familial mediterranean fever in Iran: a report from FMF registration center. Int J Rheumatol. 2015;2015:1–6. doi:10.1155/2015/912137
17. Salehzadeh F, Sharghi F, Motayayagheni A, et al. MEFV gene variant alleles in normal population of Northwest of Iran, which is near to mediterranean sea. Genet Res Int. 2019;2019. doi:10.1155/2019/6418759
18. Gedalia A, Zamir S. Neurologic manifestations in familial mediterranean fever. Pediatr Neurol. 1993;9(4):301–302. doi:10.1016/0887-8994(93)90068-N
19. Uluduz D, Tavsanli ME, Uygunoglu U, et al. Primary headaches in pediatric patients with chronic rheumatic disease. Brain Dev. 2014;36(10):884–891. doi:10.1016/j.braindev.2014.01.009
20. Feld O, Yahalom G, Livneh A. Neurologic and other systemic manifestations in FMF: published and own experience. Best Pract Clin Rheumatol. 2012;26(1):119–133. doi:10.1016/j.berh.2012.01.004
21. Canpolat M, Gumus H, Gunduz Z, et al. Neurological manifestations in familial mediterranean fever: results of 22 children from a reference center in Kayseri, an Urban Area in Central Anatolia, Turkey. Neuropediatrics. 2017;48(2):79–85. doi:10.1055/s-0036-1593374
22. Bulletin of World Health Organization. Epilepsy in the WHO Eastern Mediterranean Region Bridging the Gap. 2010:11–12
23. Patel N, Ram D, Swiderska N, et al. Febrile seizure. BMJ. 2015;351:1–7. doi:10.1136/bmj.h4240
24. Çomak E, Tüfekçi Ö, Kılıçbay F. Febrile seizures in children with familial mediterranean fever: coincidence or association? Eur J Paediatr Neurol. 2015;19(5):572–576. doi:10.1016/j.ejpn.2015.05.004
25. Kiykim E, Aktuglu-Zeybek A, Barut K, et al. Screening for inherited metabolic disorders in patients with familial mediterranean fever. Pediatr Rheumatol Online J. 2015;13(11):97. doi:10.1186/1546-0096-13-S1-P97
26. Abbara S, Grateau G, Ducharme-Bénard S, Saadoun D, Georgin-Lavialle S. Association of vasculitis and familial mediterranean fever. Front Immunol. 2019;10:763. doi:10.3389/fimmu.2019.00763
27. Leung AKC, Leung AAM, Wong AHC. Breath-holding spells in pediatrics: a narrative review of the current evidence. Curr Pediatr Rev. 2019;15(1):22–29. doi:10.2174/1573396314666181113094047
28. Witt M, Valda K, Moog P, et al. AB1033 evidence for autonomic dysfunction in Familial Mediterranean Fever(FMF): results from a prospective controlled study including the compass-31 questionnaire. Ann Rheum Dis. 2015;74:1243. doi:10.1136/annrheumdis-2015-eular.5750
29. Yahalom G
30. Siva A, Tutuncu M, Uygunoglu U, et al. Does Co-morbidity with familial mediterranean fever change the course of multiple sclerosis? Neurology. 2018;90(15 Supplement):
31. Ginsberg L. Difficult and recurrent meningitis. J Neurol Neurosurg Psychiatry. 2004;75(SupplI):i16–i21. doi:10.1136/nip.2003.034272
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
